Optical Microscopy as a Tool for Assessing Parenteral Nutrition Solution Stability: A Proof of Concept
Abstract
:1. Introduction
2. Results
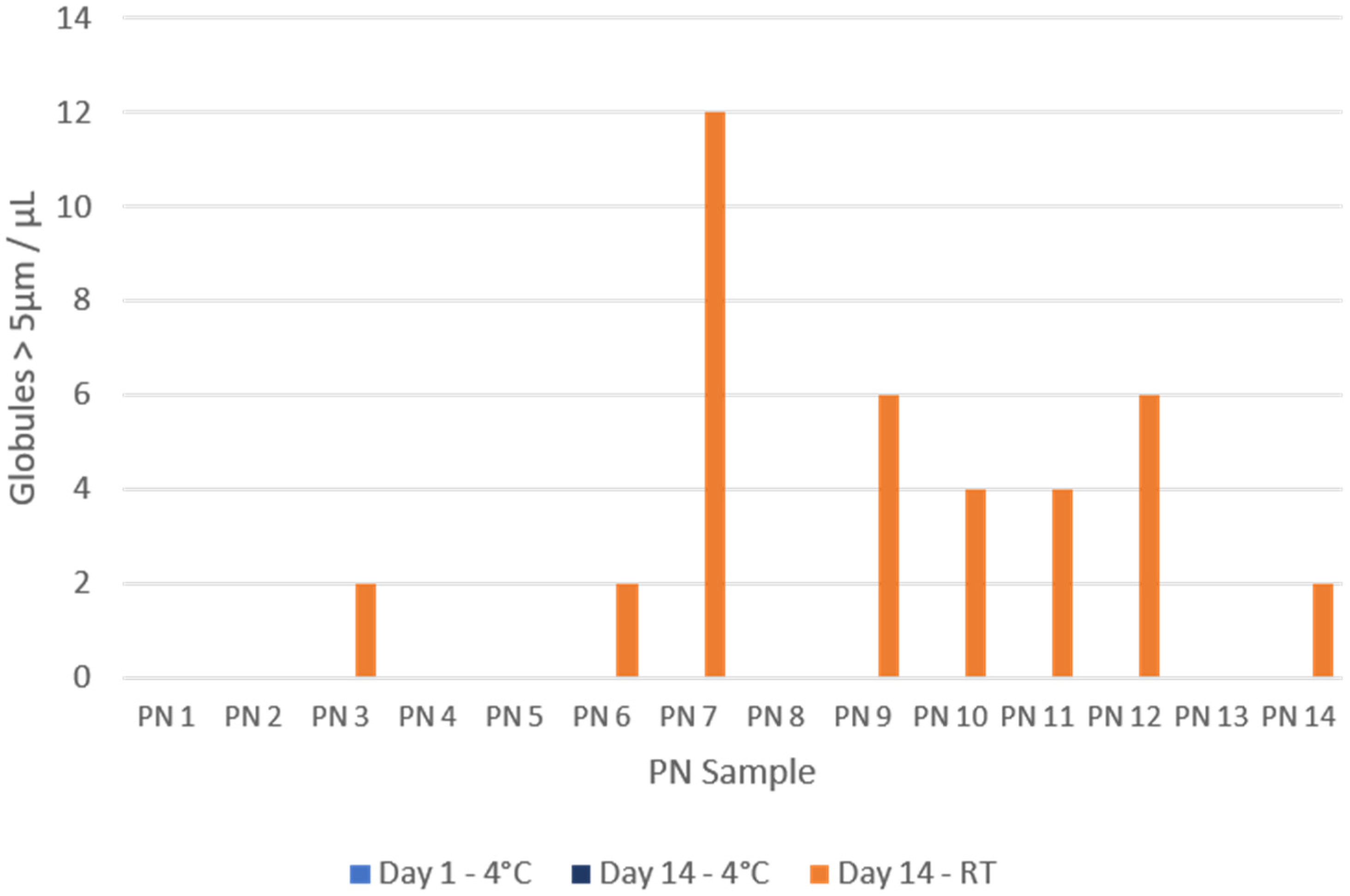
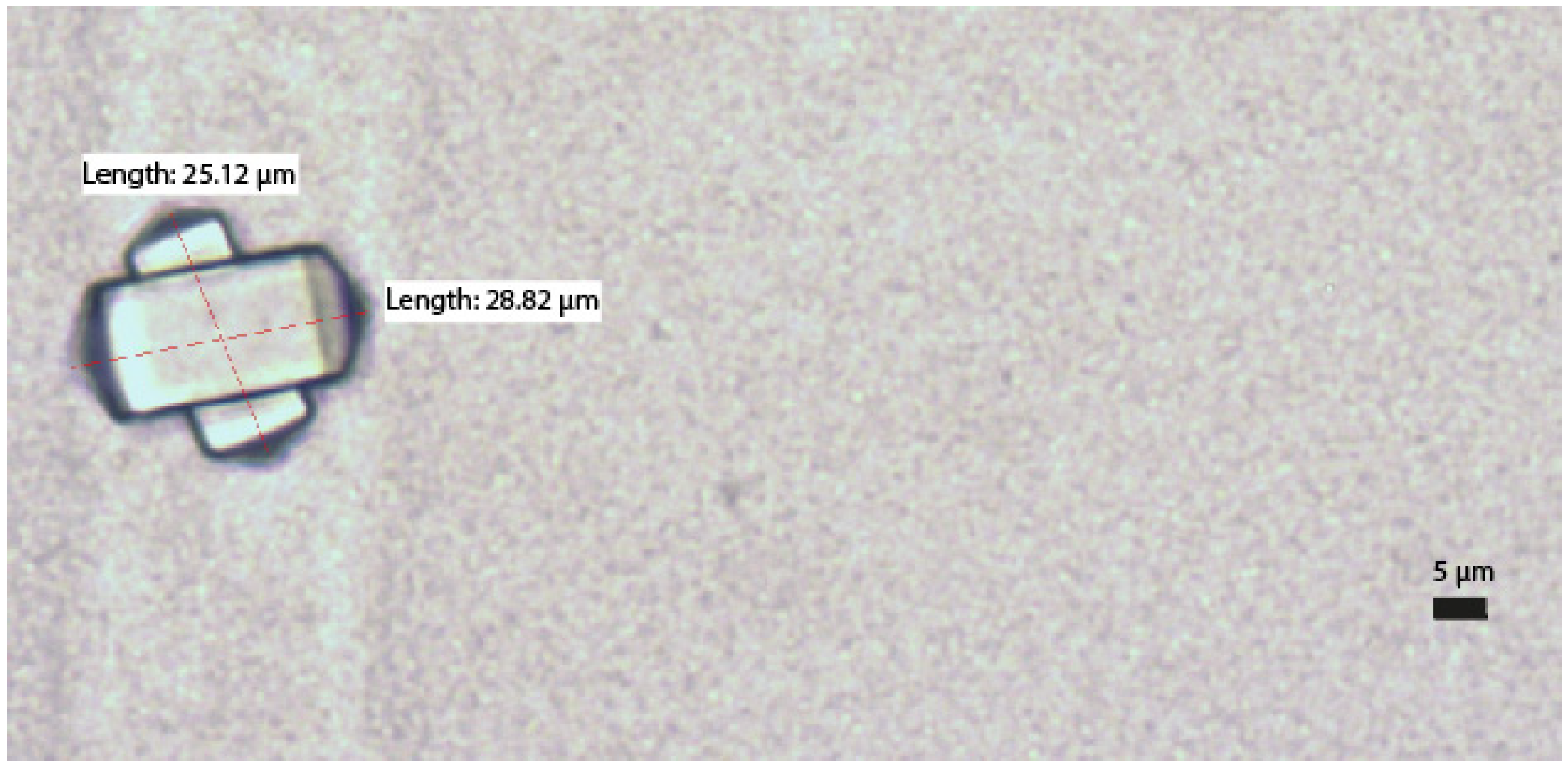
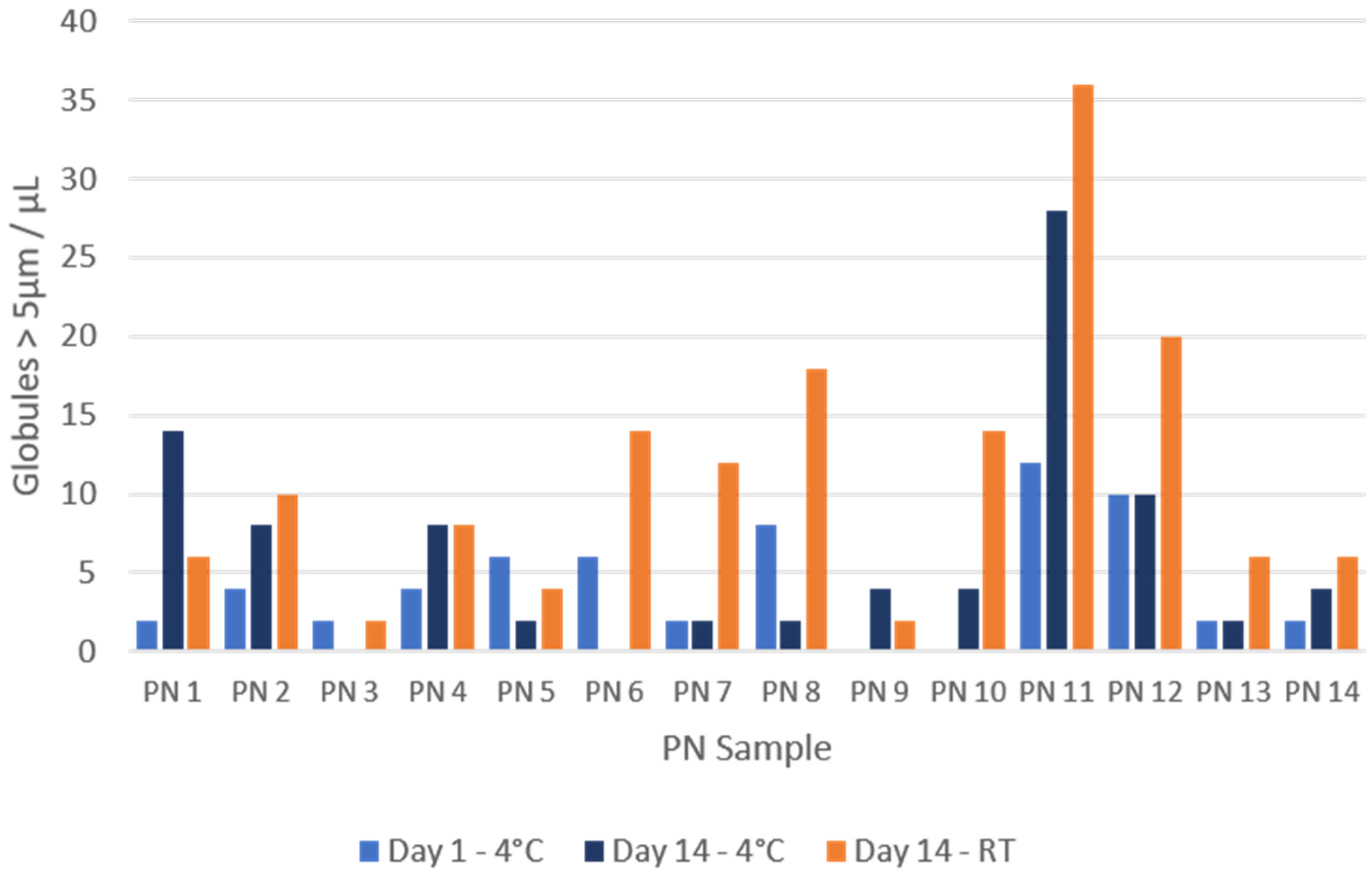
2.1. Precipitate Formation
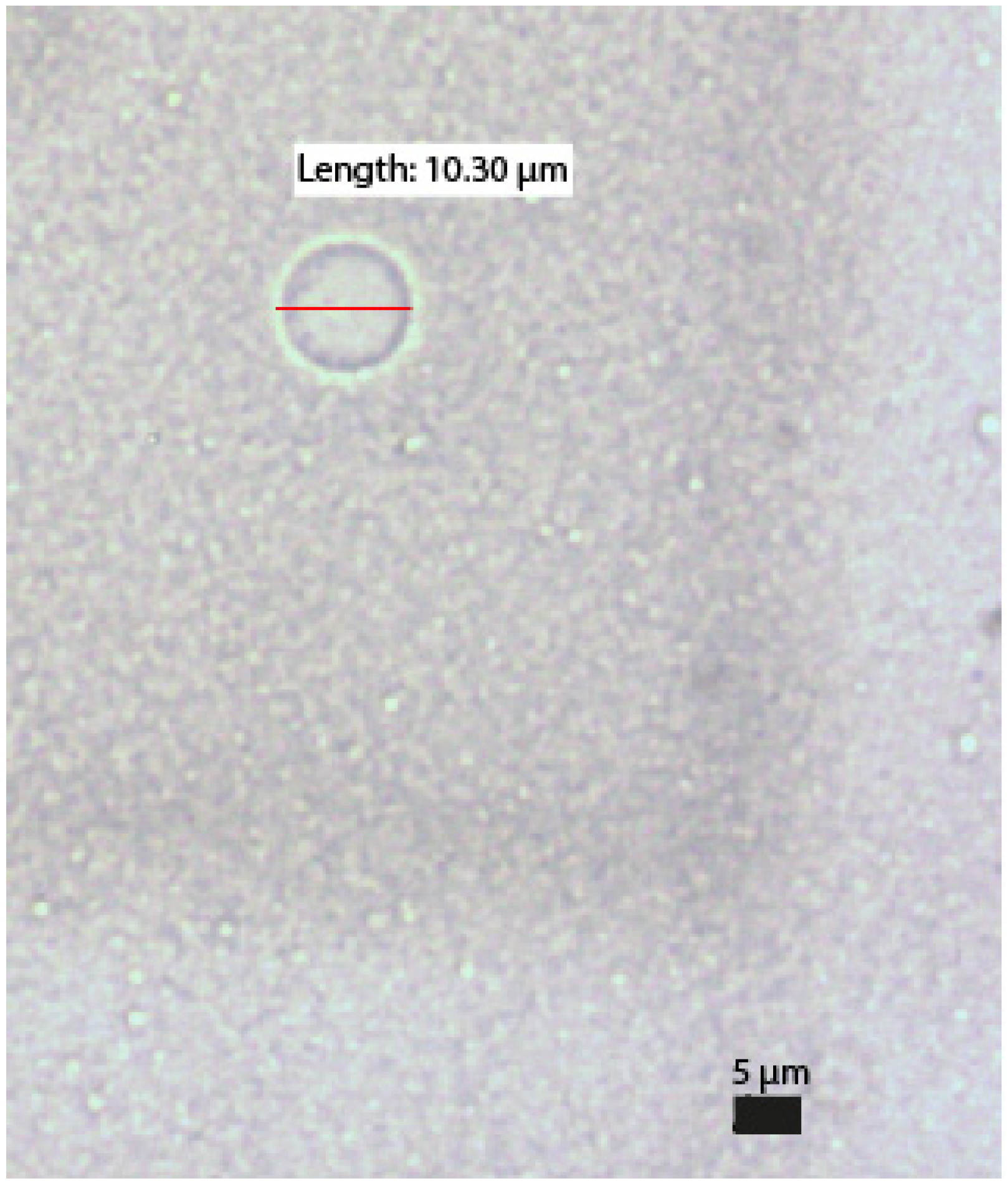
2.2. Globule Size
3. Discussion
4. Materials and Methods
4.1. Sample Preparation
4.2. Optical Microscopy
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Thibault, R.; Abbasoglu, O.; Ioannou, E.; Meija, L.; Ottens-Oussoren, K.; Pichard, C.; Rothenberg, E.; Rubin, D.; Siljamäki-Ojansuu, U.; Vaillant, M.-F.; et al. ESPEN Guideline on Hospital Nutrition. Clin. Nutr. 2021, 40, 5684–5709. [Google Scholar] [CrossRef] [PubMed]
- Boullata, J.I.; Berlana, D.; Pietka, M.; Klek, S.; Martindale, R. Use of Intravenous Lipid Emulsions with Parenteral Nutrition: Practical Handling Aspects. JPEN J. Parenter. Enteral Nutr. 2020, 44 (Suppl. 1), S74–S81. [Google Scholar] [CrossRef] [PubMed]
- Driscoll, D.F. Quality, stability and safety of lipid emulsions. Clin. Nutr. 2007, 2 (Suppl. 3), 11–15. [Google Scholar]
- Mckinnon, B.T. FDA Safety Alert: Hazards of Precipitation Associated with Parenteral Nutrition. Nutr. Clin. Pract. 1996, 11, 59–65. [Google Scholar] [CrossRef]
- Driscoll, D.F.; Nehne, J.; Peterss, H.; Klütsch, K.; Bistrian, B.R.; Niemann, W. Physicochemical Stability of Intravenous Lipid Emulsions as All-in-One Admixtures Intended for the Very Young. Clin. Nutr. 2003, 22, 489–495. [Google Scholar] [CrossRef] [PubMed]
- Driscoll, D.F.; Thoma, A.; Franke, R.; Klütsch, K.; Nehne, J.; Bistrian, B.R. Lipid Globule Size in Total Nutrient Admixtures Prepared in Three-Chamber Plastic Bags. Am. J. Health Syst. Pharm. 2009, 66, 649–656. [Google Scholar] [CrossRef]
- Joy, J.; Silvestri, A.P.; Franke, R.; Bistrian, B.R.; Nehne, J.; Newton, D.W.; Driscoll, D.F. Calcium and Phosphate Compatibility in Low-Osmolarity Parenteral Nutrition Admixtures Intended for Peripheral Vein Administration. JPEN J. Parenter. Enter. Nutr. 2010, 34, 46–54. [Google Scholar] [CrossRef]
- de Oliveira Ribeiro, D.; Lobo, B.W.; Volpato, N.M.; da Veiga, V.F.; Cabral, L.M.; de Sousa, V.P. Influence of the Calcium Concentration in the Presence of Organic Phosphorus on the Physicochemical Compatibility and Stability of All-in-One Admixtures for Neonatal Use. Nutr. J. 2009, 8, 51. [Google Scholar] [CrossRef]
- Parikh, M.J.; Dumas, G.; Silvestri, A.; Bistrian, B.R.; Driscoll, D.F. Physical Compatibility of Neonatal Total Parenteral Nutrient Admixtures Containing Organic Calcium and Inorganic Phosphate Salts. Am. J. Health Syst. Pharm. 2005, 62, 1177–1183. [Google Scholar] [CrossRef]
- Maruyama, H.; Saito, J.; Nagai, M.; Mochizuki, M.; Ishikawa, Y.; Ito, Y. Maximization of Calcium and Phosphate in Neonatal Total Parenteral Nutrition. Pediatr. Int. 2018, 60, 634–638. [Google Scholar] [CrossRef]
- Singh, H.; Dumas, G.J.; Silvestri, A.P.; Young, S.; Martin, C.R.; Bistrian, B.R.; Driscoll, D.F. Physical Compatibility of Neonatal Total Parenteral Nutrition Admixtures Containing Organic Calcium and Inorganic Phosphate Salts in a Simulated Infusion at 37 °C. Pediatr. Crit. Care Med. 2009, 10, 213–216. [Google Scholar] [CrossRef] [PubMed]
- Allwood, M.C.; Kearney, M.C.J. Compatibility and Stability of Additives in Parenteral Nutrition Admixtures. Nutrition 1998, 14, 697–706. [Google Scholar] [CrossRef] [PubMed]
- Cardona Pera, D.; Cervera Peris, M.; Fernández Arévalo, M.; Gomis Muñoz, P.; Martínez Tutor, M.J.; Piñeiro Corrales, G.; Rodríguez Penín, I.; Vázquez Polo, A. Consenso Español Sobre La Preparación de Mezclas Nutrientes Parenterales. Farm. Hosp. 2009, 76, 81–107. [Google Scholar]
- MacKay, M.; Anderson, C. Physical Compatibility of Sodium Glycerophosphate and Calcium Gluconate in Pediatric Parenteral Nutrition Solutions. JPEN J. Parenter. Enter. Nutr. 2015, 39, 725–728. [Google Scholar] [CrossRef] [PubMed]
- Anderson, C.; MacKay, M. Physical Compatibility of Calcium Chloride and Sodium Glycerophosphate in Pediatric Parenteral Nutrition Solutions. JPEN J. Parenter. Enter. Nutr. 2016, 40, 1166–1169. [Google Scholar] [CrossRef]
- Raupp, P.; Kries, R.V.; Pfahl, H.-G.; Manz, F. Glycero- vs. Glucose-Phosphate in Parenteral Nutrition of Premature Infants: A Comparative in Vitro Evaluation of Calcium/Phosphorus Compatibility. JPEN J. Parenter. Enter. Nutr. 1991, 15, 469–473. [Google Scholar] [CrossRef]
- Bouchoud, L.; Fonzo-Christe, C.; Sadeghipour, F.; Bonnabry, P. Maximizing Calcium and Phosphate Content in Neonatal Parenteral Nutrition Solutions Using Organic Calcium and Phosphate Salts. JPEN J. Parenter. Enter. Nutr. 2010, 34, 542–545. [Google Scholar] [CrossRef]
- Chaieb D., S.; Chaumeil, J.C.; Jebnoun, S.; Khrouf, N.; Hedhili, A.; Sfar, S. Effect of the Intravenous Lipid Emulsions on the Availability of Calcium When Using Organic Phosphate in TPN Admixtures. Pharm. Res. 2008, 25, 2545. [Google Scholar] [CrossRef]
- Athanasiou, C.; Hatziantoniou, S.; Skouroliakou, M.; Markantonis-Kyroudis, S. Assessment of the Physicochemical Stability of All-in-One Parenteral Emulsions for Neonates According to USP Specifications. JPEN J. Parenter. Enter. Nutr. 2014, 38, 867–872. [Google Scholar] [CrossRef]
- Foinard, A.; Perez, M.; Barthélémy, C.; Lannoy, D.; Flamein, F.; Storme, L.; Addad, A.; Bout, M.-A.; Décaudin, B.; Odou, P. In Vitro Assessment of Interaction Between Amino Acids and Copper in Neonatal Parenteral Nutrition. JPEN J. Parenter. Enter. Nutr. 2016, 40, 827–834. [Google Scholar] [CrossRef]
- USP-NF. General Chapter, (729) Globule Size Distribution in Lipid Injectable Emulsions; USP-NF: Rockville, MD, USA, 2023; [Revised 2023]. [Google Scholar] [CrossRef]
- Skouroliakou, M.; Matthaiou, C.; Chiou, A.; Panagiotakos, D.; Gounaris, A.; Nunn, T.; Andrikopoulos, N. Physicochemical Stability of Parenteral Nutrition Supplied as All-in-One for Neonates. JPEN J. Parenter. Enter. Nutr. 2008, 32, 201–209. [Google Scholar] [CrossRef] [PubMed]
- Driscoll, D.F. Stability and Compatibility Assessment Techniques for Total Parenteral Nutrition Admixtures: Setting the Bar According to Pharmacopeial Standards. Curr. Opin. Clin. Nutr. Metab. Care 2005, 8, 297–303. [Google Scholar] [CrossRef] [PubMed]
- Liviskie, C.J.; Lange, S.A.; McPherson, C.C. Precipitation of Heparin Products with Calcium Gluconate: The Activity of Inactive Ingredients. J. Pediatr. Pharmacol. Ther. 2017, 22, 314–315. [Google Scholar] [CrossRef] [PubMed]
- Akers, M.J.; Schrank, G.D.; Russell, S. Particulate Evaluation of Parenteral Nutrition Solutions by Electronic Particle Counting and Scanning Electron Microscopy. Am. J. Hosp. Pharm. 1981, 38, 1304–1307. [Google Scholar] [CrossRef]
- Janů, M.; Brodská, H.; Vecka, M.; Masteiková, R.; Kotrlíková, E.; Lažauskas, R.; Pečiūra, R.; Bernatonienė, J. Comparison of Long-Term Stability of Parenteral All-in-One Admixtures Containing New Lipid Emulsions Prepared Under Hospital Pharmacy Conditions. Medicina 2011, 47, 46. [Google Scholar] [CrossRef]
- Watrobska-Swietlikowska, D. Compatibility of Maximum Inorganic and Organic Calcium and Phosphate Content in Neonatal Parenteral Solutions. Sci. Rep. 2019, 9, 10525. [Google Scholar] [CrossRef]
- Driscoll, D.F.; Nehne, J.; Peterss, H.; Klutsch, K.; Bistrian, B.R.; Niemann, W. Physical Assessments of Lipid Injectable Emulsions via Microscopy: A Comparison to Methods Proposed in United States Pharmacopeia Chapter 729. Int. J. Pharm. Compd. 2006, 10, 309–315. [Google Scholar]
- EDQM Council of Europe. Pharmaceutical Technical Procedures Chapter, (2.9.37) Optical Microscopy; European Pharmacopeia 11.0; EDQM Council of Europe: Strasbourg, France, 2023; [Revised 2024]; Available online: https://pheur.edqm.eu/home (accessed on 23 September 2024).
- Driscoll, D.F.; Ling, P.-R.; Quist, W.C.; Bistrian, B.R. Pathological Consequences from the Infusion of Unstable Lipid Emulsion Admixtures in Guinea Pigs. Clin. Nutr. Edinb. Scotl. 2005, 24, 105–113. [Google Scholar] [CrossRef]
- Gerard-Boncompain, M.; Claudel, J.P.; Gaussorgues, P.; Salord, F.; Sirodot, M.; Chevallier, M.; Robert, D. Hepatic Cytolytic and Cholestatic Changes Related to a Change of Lipid Emulsions in Four Long-Term Parenteral Nutrition Patients With Short Bowel. JPEN J. Parenter. Enter. Nutr. 1992, 16, 78–83. [Google Scholar] [CrossRef]
- Toce, S.S.; Keenan, W.J. Lipid Intolerance in Newborns Is Associated with Hepatic Dysfunction but Not Infection. Arch. Pediatr. Adolesc. Med. 1995, 149, 1249–1253. [Google Scholar] [CrossRef]
- Driscoll, D.F.; Parikh, M.; Silvestri, A.P.; Klütsch, K.; Bistrian, B.R.; Nehne, J. Establishing a Stability Window for Medium- and Long-Chain-Triglyceride Lipid-Based Total Nutrient Admixtures Using USP Standards. Am. J. Health Syst. Pharm. 2006, 63, 2135–2143. [Google Scholar] [CrossRef]
- Driscoll, D.F.; Silvestri, A.P.; Nehne, J.; Klütsch, K.; Bistrian, B.R.; Niemann, W. Physicochemical Stability of Highly Concentrated Total Nutrient Admixtures for Fluid-Restricted Patients. Am. J. Health Syst. Pharm. 2006, 63, 79–85. [Google Scholar] [CrossRef] [PubMed]
- Driscoll, D.F.; Giampietro, K.; Wichelhaus, D.P.; Peterss, H.; Nehne, J.; Niemann, W.; Bistrian, B.R. Physicochemical Stability Assessments of Lipid Emulsions of Varying Oil Composition. Clin. Nutr. 2001, 20, 151–157. [Google Scholar] [CrossRef] [PubMed]
- Lázaro Cebas, A.; Pablos Bravo, S.; Gomis Muñoz, P.; Orbaneja, M.Á.; Spiers, S.; Shinn, M.; Ferrari Piquero, J.M. Límites de precipitación en nutriciones parenterales pediátricas con fuentes de calcio y fosfato orgánicas. Nutr. Hosp. 2018, 35, 1009. [Google Scholar] [CrossRef]
- Otero-Millán, L.; Bea-Mascato, B.; Legido Soto, J.L.; Martínez-López-De-Castro, N.; Lago Rivero, N. Electron Microscopy for the Stability Assessment of Parenteral Nutrition Admixtures: Focus on Precipitation. Nutrients 2024, 16, 1390. [Google Scholar] [CrossRef]
- Turmezei, J.; Jávorszky, E.; Dredán, J.; Kállai-Szabó, B.; Zelkó, R. Effect of Storage Temperature on the Stability of Total Parenteral Nutrition Admixtures Prepared for Infants. Acta Pol. Pharm.—Drug Res. 2015, 72, 843–849. [Google Scholar]
- Ambados, F.; Brealey, J. Incompatibilities with Trace Elements During TPN Solution Admixture. Aust. J. Hosp. Pharm. 1998, 28, 112–114. [Google Scholar] [CrossRef]
- Otero-Millán, L.; Bea-Mascato, B.; Legido Soto, J.L.; Martínez-López-De-Castro, N.; Lago-Rivero, N. Physicochemical Stability of Hospital Parenteral Nutrition Solutions: Effect of Changes in Composition and Storage Protocol. Pharmaceutics 2024, 16, 572. [Google Scholar] [CrossRef]
- Barnett, M.I.; Cosslett, A.G.; Duffield, J.R.; Evans, D.A.; Hall, S.B.; Williams, D.R. Parenteral Nutrition. Pharmaceutical Problems of Compatibility and Stability. Drug Saf. 1990, 5 (Suppl. 1), 101–106. [Google Scholar] [CrossRef]
| Sample | N (g/L) | Prot (g/L) | Lip (g/L) | Na (mMol/L) | Mg (mMol/L) | P (mMol/L) | OSM (mOsm/L) | CAN (mMol/L) |
|---|---|---|---|---|---|---|---|---|
| PN1 | 4.00 | 25.00 | 20.00 | 40.00 | 25.00 | 12.50 | 1110.00 | 3300.00 |
| PN2 | 4.00 | 25.00 | 20.00 | 40.00 | 37.50 | 12.50 | 1160.00 | 4100.00 |
| PN3 | 4.00 | 25.00 | 20.00 | 40.00 | 50.00 | 12.50 | 1210.00 | 4900.00 |
| PN4 | 4.00 | 25.00 | 20.00 | 40.00 | 5.00 | 20.00 | 1043.50 | 2020.00 |
| PN5 | 4.00 | 25.00 | 20.00 | 48.00 | 5.00 | 30.00 | 1101.50 | 2028.00 |
| PN6 | 4.00 | 25.00 | 20.00 | 80.00 | 5.00 | 50.00 | 1217.50 | 2060.00 |
| PN7 | 4.00 | 25.00 | 20.00 | 120.00 | 5.00 | 100.00 | 1507.50 | 2100.00 |
| PN8 | 4.00 | 25.00 | 15.00 | 40.00 | 5.00 | 12.50 | 1015.00 | 2020.00 |
| PN9 | 4.00 | 25.00 | 10.00 | 40.00 | 5.00 | 12.50 | 1000.00 | 2020.00 |
| PN10 | 4.00 | 25.00 | 5.00 | 40.00 | 5.00 | 12.50 | 985.00 | 2020.00 |
| PN11 | 4.00 | 25.00 | 2.50 | 40.00 | 5.00 | 12.50 | 977.50 | 2020.00 |
| PN12 | 4.00 | 25.00 | 1.24 | 40.00 | 5.00 | 12.50 | 973.75 | 2020.00 |
| PN13 | 3.50 | 21.87 | 20.00 | 40.00 | 5.00 | 12.50 | 995.63 | 2020.00 |
| PN14 | 3.00 | 18.75 | 20.00 | 40.00 | 5.00 | 12.50 | 961.25 | 2020.00 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Otero-Millán, L.; Bea-Mascato, B.; Legido Soto, J.L.; Martín de la Cruz, M.C.; Martínez-López-De-Castro, N.; Lago-Rivero, N. Optical Microscopy as a Tool for Assessing Parenteral Nutrition Solution Stability: A Proof of Concept. Pharmaceuticals 2024, 17, 1330. https://doi.org/10.3390/ph17101330
Otero-Millán L, Bea-Mascato B, Legido Soto JL, Martín de la Cruz MC, Martínez-López-De-Castro N, Lago-Rivero N. Optical Microscopy as a Tool for Assessing Parenteral Nutrition Solution Stability: A Proof of Concept. Pharmaceuticals. 2024; 17(10):1330. https://doi.org/10.3390/ph17101330
Chicago/Turabian StyleOtero-Millán, Luis, Brais Bea-Mascato, Jose Luis Legido Soto, María Carmen Martín de la Cruz, Noemi Martínez-López-De-Castro, and Natividad Lago-Rivero. 2024. "Optical Microscopy as a Tool for Assessing Parenteral Nutrition Solution Stability: A Proof of Concept" Pharmaceuticals 17, no. 10: 1330. https://doi.org/10.3390/ph17101330






