Optimization of Pramipexole-Loaded In Situ Thermosensitive Intranasal Gel for Parkinson’s Disease
Abstract
:1. Introduction
2. Results and Discussion
2.1. Preliminary Studies
2.2. Drug Excipient Interaction Study
2.3. Experimental Design
2.4. Gelling Temperature
2.5. Gel Strength
2.6. % Drug Diffused after 8 h
2.7. Validation of Model
2.8. Optimization of Formulation by Graphical Method
2.9. In Vivo Drug Retention Time
2.10. Stability Studies
3. Materials and Methods
3.1. Materials
3.2. Methods
3.2.1. Formulation of Thermoreversible In Situ Gels
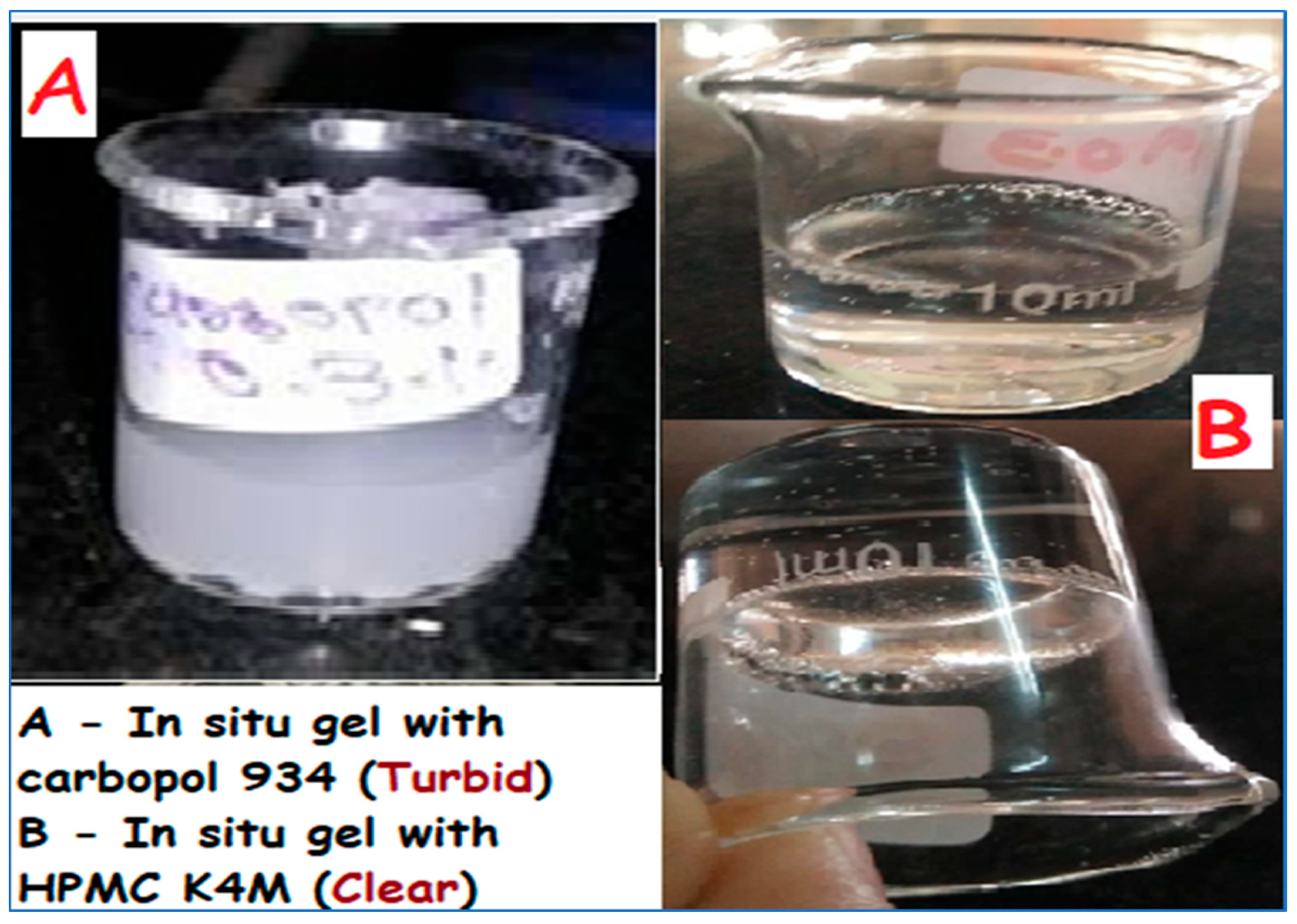
3.2.2. Preliminary Work
3.2.3. Drug Excipient Compatibility Studies
3.2.4. Experimental Design—Two-Factor and Three-Level Factorial Design
3.2.5. Evaluation of In Situ Gels
Physicochemical Parameters
pH of the Gels
Drug Content
Gelling Temperature
Viscosity of the Gels
Gel Strength
Determination of Mucoadhesive Force
In Vitro Diffusion Studies
Ex Vivo Diffusion Study
In Vivo Drug Retention Time
3.2.6. Stability Study
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Prabhakar, P.; Ahmed, A.B.A.; Chidambaram, S.B. The role of phloridzin and its possible potential therapeutic effect on Parkinson’s disease. Int. J. Nutr. Pharmacol. Neurol. Dis. 2020, 10, 69–74. [Google Scholar]
- Choi, H.-G.; Jung, J.-H.; Ryu, J.-M.; Yoon, S.-J.; Oh, Y.-K.; Kim, C.-K. Development of in situ-gelling and mucoadhesive acetaminophen liquid suppository. Int. J. Pharm. 1998, 165, 33–44. [Google Scholar] [CrossRef]
- Trist, B.G.; Hare, D.J.; Double, K.L. Oxidative stress in the aging substantia nigra and the etiology of Parkinson’s disease. Aging Cell 2019, 18, e13031. [Google Scholar] [CrossRef] [PubMed]
- Hamani, C.; Lozano, A.M. Physiology and pathophysiology of Parkinson’s disease. Ann. N. Y. Acad. Sci. 2003, 991, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Ashhar, M.U.; Vyas, P.; Vohora, D.; Sahoo, P.K.; Nigam, K.; Dang, S.; Ali, J.; Baboota, S. Amelioration of oxidative stress utilizing nanoemulsion loaded with bromocriptine and glutathione for the management of Parkinson’s disease. Int. J. Pharm. 2022, 618, 121683. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, J.; Haider, N.; Khan, M.A.; Md, S.; Alhakamy, N.A.; Ghoneim, M.M.; Alshehri, S.; Imam, S.S.; Ahmad, M.Z.; Mishra, A. Novel therapeutic interventions for combating Parkinson’s disease and prospects of Nose-to-Brain drug delivery. Biochem. Pharmacol. 2022, 195, 114849. [Google Scholar] [CrossRef] [PubMed]
- Rocca, W.A. The burden of Parkinson’s disease: A worldwide perspective. Lancet Neurol. 2018, 17, 928–929. [Google Scholar] [CrossRef]
- Maiti, P.; Manna, J.; Dunbar, G.L. Current understanding of the molecular mechanisms in Parkinson’s disease: Targets for potential treatments. Transl. Neurodegener. 2017, 6, 1–35. [Google Scholar]
- Bennett, J.P., Jr.; Piercey, M.F. Pramipexole—A new dopamine agonist for the treatment of Parkinson’s disease. J. Neurol. Sci. 1999, 163, 25–31. [Google Scholar] [CrossRef]
- Reichmann, H.; Brecht, M.H.; Köster, J.; Kraus, P.H.; Lemke, M.R. Pramipexole in routine clinical practice: A prospective observational trial in Parkinson’s disease. CNS Drugs 2003, 17, 965–973. [Google Scholar] [CrossRef]
- Wright, C.E.; Sisson, T.L.; Ichhpurani, A.K.; Peters, G.R. Steady-state pharmacokinetic properties of pramipexole in healthy volunteers. J. Clin. Pharmacol. 1997, 37, 520–525. [Google Scholar] [CrossRef] [PubMed]
- Dahlin, M.; Bergman, U.; Jansson, B.; Björk, E.; Brittebo, E. Transfer of dopamine in the olfactory pathway following nasal administration in mice. Pharm. Res. 2000, 17, 737–742. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.; Lohan, S.; Murthy, R. Formulation and characterization of intranasal mucoadhesive nanoparticulates and thermo-reversible gel of levodopa for brain delivery. Drug Dev. Ind. Pharm. 2014, 40, 869–878. [Google Scholar] [CrossRef] [PubMed]
- Sridhar, V.; Wairkar, S.; Gaud, R.; Bajaj, A.; Meshram, P. Brain targeted delivery of mucoadhesive thermosensitive nasal gel of selegiline hydrochloride for treatment of Parkinson’s disease. J. Drug Target. 2018, 26, 150–161. [Google Scholar] [CrossRef]
- Uppuluri, C.T.; Ravi, P.R.; Dalvi, A.V. Design, optimization and pharmacokinetic evaluation of Piribedil loaded solid lipid nanoparticles dispersed in nasal in situ gelling system for effective management of Parkinson’s disease. Int. J. Pharm. 2021, 606, 120881. [Google Scholar] [CrossRef] [PubMed]
- Meenakshi, P.; Hetal, T.; Kasture, P. Preparation and evaluation of thermoreversible formulations of flunarizine hydrochloride for nasal delivery. Int. J. Pharm. Pharm. Sci. 2010, 2, 115–120. [Google Scholar]
- Schmolka, I.R. Artificial skin I. Preparation and properties of pluronic F-127 gels for treatment of burns. J. Biomed. Mater. Res. 1972, 6, 571–582. [Google Scholar] [CrossRef] [PubMed]
- Ansari, M.J.; Rajendran, R.R.; Mohanto, S.; Agarwal, U.; Panda, K.; Dhotre, K.; Manne, R.; Deepak, A.; Zafar, A.; Yasir, M. Poly (N-isopropylacrylamide)-based hydrogels for biomedical applications: A review of the state-of-the-art. Gels 2022, 8, 454. [Google Scholar] [CrossRef]
- García-Couce, J.; Tomás, M.; Fuentes, G.; Que, I.; Almirall, A.; Cruz, L.J. Chitosan/Pluronic F127 thermosensitive hydrogel as an injectable dexamethasone delivery carrier. Gels 2022, 8, 44. [Google Scholar] [CrossRef]
- Liu, Y.; Zhu, Y.-y.; Wei, G.; Lu, W.-Y. Effect of carrageenan on poloxamer-based in situ gel for vaginal use: Improved in vitro and in vivo sustained-release properties. Eur. J. Pharm. Sci. 2009, 37, 306–312. [Google Scholar] [CrossRef]
- Hirun, N.; Kraisit, P.; Tantishaiyakul, V. Thermosensitive polymer blend composed of poloxamer 407, poloxamer 188 and polycarbophil for the use as mucoadhesive in situ gel. Polymers 2022, 14, 1836. [Google Scholar] [CrossRef] [PubMed]
- Boonlai, W.; Tantishaiyakul, V.; Hirun, N.; Phaisan, S.; Uma, T. The effect of the preservative methylparaben on the thermoresponsive gelation behavior of aqueous solutions of poloxamer 407. J. Mol. Liq. 2017, 240, 622–629. [Google Scholar] [CrossRef]
- Patel, M.; Shaikh, F.; Patel, V.; Surti, N. Optimization of glipizide floating matrix tablet using simplex lattice design. Indian J. Pharm. Sci. 2021, 83, 306–315. [Google Scholar] [CrossRef]
- Patel, M.; Shelke, S.; Shaikh, F.; Surti, N.; Panzade, P.; Panjwani, D. Gastroretentive Floating Microsponges of Mitiglinide: Design, Preparation, and Pharmacokinetic Evaluation. J. Pharm. Innov. 2023, 18, 1–15. [Google Scholar] [CrossRef]
- Patel, M.B.; Shaikh, F.; Patel, V.B.; Surti, N. Application of experiential design for framing gastroretentive microsponges of glipizide: Screening of critical variables by plackett-burman design and optimization by box-behnken design. Indian J. Pharm. Educ. Res. 2021, 55, 966–978. [Google Scholar] [CrossRef]
- Patel, M.B.; Shaikh, F.; Patel, V.; Surti, N.I. Application of simplex centroid design in formulation and optimization of floating matrix tablets of metformin. J. Appl. Pharm. Sci. 2017, 7, 23–30. [Google Scholar]
- Fathalla, Z.M.; Vangala, A.; Longman, M.; Khaled, K.A.; Hussein, A.K.; El-Garhy, O.H.; Alany, R.G. Poloxamer-based thermoresponsive ketorolac tromethamine in situ gel preparations: Design, characterisation, toxicity and transcorneal permeation studies. Eur. J. Pharm. Biopharm. 2017, 114, 119–134. [Google Scholar] [CrossRef]
- Grela, K.P.; Marciniak, D.M.; Karolewicz, B. Poloxamer 407-Based Thermosensitive Emulgel as a Novel Formulation Providing a Controlled Release of Oil-Soluble Pharmaceuticals—Ibuprofen Case Study. Materials 2021, 14, 7266. [Google Scholar] [CrossRef]
- Vecchi, C.F.; Dos Santos, R.S.; Bruschi, M.L. Technological development of mucoadhesive film containing poloxamer 407, polyvinyl alcohol and polyvinylpyrrolidone for buccal metronidazole delivery. Ther. Deliv. 2020, 11, 431–446. [Google Scholar] [CrossRef]
- Kumar, S.; Gupta, S.K.; Pahwa, R. Designing lisuride intranasal nanocarrier system for reduction of oxidative damage with enhanced dopamine level in brain for Parkinsonism. J. Psychiatr. Res. 2023, 165, 205–218. [Google Scholar] [CrossRef]
- Lale, A.; Mason, J.; Jones, N. Mucociliary transport and its assessment: A review. Clin. Otolaryngol. Allied Sci. 1998, 23, 388–396. [Google Scholar] [CrossRef] [PubMed]
- Ravi, P.; Aditya, N.; Patil, S.; Cherian, L. Nasal in-situ gels for delivery of rasagiline mesylate: Improvement in bioavailability and brain localization. Drug Deliv. 2015, 22, 903–910. [Google Scholar] [CrossRef] [PubMed]
- Galgatte, U.C.; Kumbhar, A.B.; Chaudhari, P.D. Development of in situ gel for nasal delivery: Design, optimization, in vitro and in vivo evaluation. Drug Deliv. 2014, 21, 62–73. [Google Scholar] [CrossRef] [PubMed]






| Concentration of Poloxamer 407 (% w/v) | Gelation Temperature (°C) (N = 3) |
|---|---|
| 16 | 39 ± 0.5 |
| 17 | 37 ± 0.3 |
| 18 | 34 ± 0.4 |
| 19 | 32 ± 0.2 |
| 20 | 29 ± 0.5 |
| 21 | 27 ± 0.5 |
| Concentration of Poloxamer 407 (20% w/v) + Excipients | Gelation Point in °C ± S.D | Effect on the Gelation Point |
|---|---|---|
| Poloxamer 407 + drug (2.5 mg) | 27 ± 0.3 | Decrease |
| Poloxamer 407 + Carbopol 934 (0.3% w/v) | 26 ± 0.3 | Decrease |
| Poloxamer 407 + HPMC K4M (0.3% w/v) | 27 ± 0.3 | Decrease |
| Poloxamer 407 + benzyl alkonium chloride (0.01% w/v) | 31 ± 0.3 | Increase |
| Poloxamer 407 + sodium chloride (0.9% w/v) | 32 ± 0.3 | Increase |
| Batches | pH | Viscosity (cps) at 4 °C ± S.D. | Viscosity (cps) at 37 °C ± S.D. | Drug Content (%) | Mucoadhesive Force (Dyne/cm2) ± S.D. |
|---|---|---|---|---|---|
| PG1 | 4.95 | 17 ± 3.3 | 4965 ± 6.12 | 95 ± 2.5 | 1632.09 ± 10.5 |
| PG2 | 5.15 | 21 ± 2.45 | 5123 ± 2.44 | 94 ± 3.2 | 2028.3 ± 13.74 |
| PG3 | 5.10 | 29 ± 2.36 | 5441 ± 2.55 | 92 ± 2.7 | 2896.8 ± 18.21 |
| PG4 | 5.18 | 24 ± 3.21 | 5785 ± 3.14 | 95 ± 1.1 | 3082.09 ± 15.3 |
| PG5 | 4.99 | 31 ± 2.6 | 5320 ± 3.44 | 96 ± 2.1 | 2508.3 ± 11.17 |
| PG6 | 4.79 | 37 ± 1.0 | 5031 ± 3.71 | 93 ± 3.7 | 2466.8 ± 15.24 |
| PG7 | 5.22 | 39 ± 2.5 | 5392 ± 1.23 | 94 ± 2.1 | 2746.5 ± 16.82 |
| PG8 | 5.09 | 43 ± 3.1 | 5782 ± 3.14 | 91 ± 3.4 | 3495.5 ± 19.71 |
| PG9 | 4.82 | 45 ± 2.28 | 5938 ± 3.14 | 90 ± 2.6 | 3862.5 ± 14.52 |
| Source | Sum of Squares | Degree of Freedom | Mean Square | F Value | p-Value |
|---|---|---|---|---|---|
| Gelling temperature (°C) | |||||
| Model | 39.58 | 5 | 7.92 | 57.00 | 0.0036 |
| Residual | 0.42 | 3 | 0.14 | - | - |
| Corrected total | 40.00 | 8 | - | - | - |
| Gel strength (s) | |||||
| Model | 195.11 | 5 | 39.02 | 65.85 | 0.0029 |
| Residual | 1.78 | 3 | 0.59 | - | - |
| Corrected total | 196.89 | 8 | - | - | - |
| Drug diffused after 8 h (%) | |||||
| Model | 74.03 | 5 | 15.62 | 60.26 | 0.0033 |
| Residual | 0.86 | 3 | - | - | - |
| Corrected total | 74.89 | 8 | - | - | - |
| Parameter | Gelling Temperature (°C) | Gel Strength (s) | % Drug Diffused (after 8 h) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Batches | PG10 | PG11 | PG12 | PG10 | PG11 | PG12 | PG10 | PG11 | PG12 |
| Predicted value | 32.21 | 33.97 | 35.39 | 38.41 | 37.03 | 33.88 | 89.91 | 90.70 | 92.30 |
| Experimental values | 31.25 ± 0.5 | 32.88 ± 0.8 | 34.32 ± 0.7 | 37.24 ± 2.1 | 36.92 ± 3.21 | 32.95 ± 2.15 | 88.78 ± 1.5 | 89.62 ± 1.3 | 90.97 ± 0.8 |
| % bias | 2.98 | 3.08 | 2.77 | 3.16 | 2.21 | 2.74 | 1.34 | 1.19 | 1.44 |
| Independent Variables/Levels | Amount of Poloxamer 407 | Amount of HPMC K4M |
|---|---|---|
| X1 (mg) | X2 (mg) | |
| Low | 16 | 0.2 |
| Medium | 16.5 | 0.4 |
| High | 17 | 0.6 |
| Dependent variable | Y1 = Gelling temperature (°C) Y2 = Gel strength (s) Y3 = % Drug diffused (after 8 h) | |
| Runs | Batch Code | Transformed Fractions of Variables * | Gelling Temperature (°C) | Gel Strength (s) | % Drug Diffused (after 8 h) | |
|---|---|---|---|---|---|---|
| X1 | X2 | |||||
| 1 | PG1 | 16 | 0.2 | 37 ± 0.32 | 30 ± 1.1 | 95.65 ± 0.03 |
| 2 | PG2 | 16 | 0.4 | 34 ± 0.53 | 34 ± 3.3 | 94.12 ± 0.54 |
| 3 | PG3 | 16 | 0.6 | 31 ± 0.33 | 39 ± 1.4 | 91.52 ± 0.01 |
| 4 | PG4 | 16.5 | 0.2 | 35 ± 0.41 | 35 ± 4.4 | 93.65 ± 0.17 |
| 5 | PG5 | 16.5 | 0.4 | 33 ± 0.32 | 37 ± 1.3 | 92.26 ± 0.17 |
| 6 | PG6 | 16.5 | 0.6 | 30 ± 0.44 | 42 ± 2.6 | 89.16 ± 0.02 |
| 7 | PG7 | 17 | 0.2 | 34 ± 0.28 | 38 ± 1.1 | 91.06 ± 0.39 |
| 8 | PG8 | 17 | 0.4 | 32 ± 0.48 | 41 ± 3.2 | 87.52 ± 0.27 |
| 9 | PG9 | 17 | 0.6 | 31 ± 0.39 | 47 ± 3.2 | 85.52 ± 0.39 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Trivedi, R.; Minglani, V.V.; El-Gazzar, A.M.; Batiha, G.E.-S.; Mahmoud, M.H.; Patel, M.; Patel, M. Optimization of Pramipexole-Loaded In Situ Thermosensitive Intranasal Gel for Parkinson’s Disease. Pharmaceuticals 2024, 17, 172. https://doi.org/10.3390/ph17020172
Trivedi R, Minglani VV, El-Gazzar AM, Batiha GE-S, Mahmoud MH, Patel M, Patel M. Optimization of Pramipexole-Loaded In Situ Thermosensitive Intranasal Gel for Parkinson’s Disease. Pharmaceuticals. 2024; 17(2):172. https://doi.org/10.3390/ph17020172
Chicago/Turabian StyleTrivedi, Rushi, Vahid Vikram Minglani, Ahmed M. El-Gazzar, Gaber El-Saber Batiha, Mohamed H. Mahmoud, Mitesh Patel, and Meenakshi Patel. 2024. "Optimization of Pramipexole-Loaded In Situ Thermosensitive Intranasal Gel for Parkinson’s Disease" Pharmaceuticals 17, no. 2: 172. https://doi.org/10.3390/ph17020172
APA StyleTrivedi, R., Minglani, V. V., El-Gazzar, A. M., Batiha, G. E.-S., Mahmoud, M. H., Patel, M., & Patel, M. (2024). Optimization of Pramipexole-Loaded In Situ Thermosensitive Intranasal Gel for Parkinson’s Disease. Pharmaceuticals, 17(2), 172. https://doi.org/10.3390/ph17020172







