Unless specified, all reagents and starting materials were purchased from commercial sources and used as received without purification. “Concentrated” refers to the removal of volatile solvents via distillation using a rotary evaporator. “Dried” refers to pouring onto or passing through anhydrous magnesium sulfate followed by filtration. Flash chromatography was performed using silica gel (230–400 mesh) with hexanes, ethyl acetate, and dichloromethane as the eluents. All reactions were monitored by thin-layer chromatography on 0.25 mm silica plates (F-4) visualized with UV light. Melting points were measured by using a capillary melting point apparatus. 1H and 13C NMR spectra were recorded on a 400 MHz NMR spectrometer and were described as chemical shifts, multiplicity (s, singlet; d, doublet; t, triplet; q, quartet; m, multiplet), coupling constant in hertz (Hz), and number of protons. High-Resolution Mass Spectra (HRMS) were measured with an electrospray ionization (ESI) and Q-TOF mass analyzer.
3.1.1. General Procedure for the Synthesis of 7
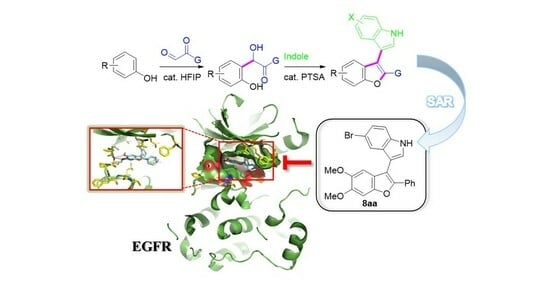
A reaction mixture of glyoxal (0.33 mmol, 1 equiv), 5 (2.0 equiv), and HFIP (0.5 equiv) in toluene (4.0 mL) was stirred at 70 °C for 36 h. The reaction mixture was concentrated in vacuo to give the crude residue, which was purified by silica gel column chromatography (hexane/ethyl acetate/dichloromethane = 8:1:2) to afford 7.
2-Hydroxy-2-(2-hydroxy-4-methoxyphenyl)-1-phenylethan-1-one (7a). Ivory solid, mp: 108.1–108.8 °C (81 mg, 95%); 1H NMR (400 MHz, (CD3)2CO) δ 8.04 (d, J = 8.0 Hz, 2H), 7.55 (t, J = 7.6 Hz, 1H), 7.44 (t, J = 7.6 Hz, 2H), 7.05 (d, J = 8.4 Hz, 1H), 6.42 (d, J = 2.4 Hz, 1H), 6.37 (dd, J = 8.4, 2.4 Hz, 1H), 6.32 (s, 1H), 3.68 (s, 3H); 13C NMR (100 MHz, CDCl3) δ 199.3, 161.0, 155.5, 133.9, 133.5, 129.6, 129.0, 128.6, 117.3, 106.9, 102.6, 71.7, 55.2; HRMS (ESI-QTOF) m/z [M+H]+ calcd for C15H15O4 259.0965, found 259.0993.
2-Hydroxy-2-(2-hydroxy-4-methoxyphenyl)-1-(3-methoxyphenyl)ethan-1-one (7b). Ivory solid, mp: 105.9–106.2 °C (91 mg, 96%); 1H NMR (400 MHz, (CD3)2CO) δ 7.70–7.55 (m, 2H), 7.34 (t, J = 8.0 Hz, 1H), 7.10 (d, J = 6.8 Hz, 1H), 7.05 (d, J = 8.0 Hz, 1H), 6.44 (s, 1H), 6.38 (d, J = 8.0 Hz, 1H), 6.31 (s, 1H), 3.80 (s, 3H), 3.68 (s, 3H); 13C NMR (100 MHz, (CD3)2CO) δ 199.0, 160.8, 159.7, 155.4, 152.5, 135.7, 129.5, 120.8, 119.4, 118.8, 113.1, 105.5, 101.5, 70.1, 54.8, 54.5; HRMS (ESI-QTOF) m/z [M+Na]+ calcd for C16H16NaO5 311.0890, found 311.0908.
2-Hydroxy-2-(2-hydroxy-4-methoxyphenyl)-1-(naphthalen-2-yl)ethan-1-one (7c). Ivory solid, mp: 107.2–107.9 °C (65 mg, 64%); 1H NMR (400 MHz, CDCl3) δ 8.53 (s, 1H), 8.00 (d, J = 8.4 Hz, 1H), 7.90 (d, J = 8.0 Hz, 1H), 7.86–7.82 (m, 2H), 7.59 (t, J = 6.8 Hz, 1H), 7.53 (t, J = 7.2 Hz, 1H), 7.02 (d, J = 8.8 Hz, 1H), 6.69 (s, 1H), 6.35 (s, 3H), 4.48 (s, 1H), 3.67 (s, 3H); 13C NMR (100 MHz, CDCl3) δ 199.2, 161.1, 155.8, 135.9, 132.3, 131.2, 131.0, 129.9, 129.8, 129.0, 128.6, 127.8, 126.9, 124.1, 117.1, 106.9, 102.9, 72.7, 55.3; HRMS (ESI-QTOF) m/z [M+Na]+ calcd for C19H16NaO4 331.0941, found 331.0938.
1-(3-Chlorophenyl)-2-hydroxy-2-(2-hydroxy-4-methoxyphenyl)ethan-1-one (7d). Ivory solid, mp: 107.4–107.9 °C (86 mg, 89%); 1H NMR (400 MHz, (CD3)2CO) δ 8.02 (s, 1H), 7.96 (d, J = 7.2 Hz, 1H), 7.58 (d, J = 8.4 Hz, 1H), 7.47 (t, J = 7.6 Hz, 1H), 7.09 (d, J = 8.4 Hz, 1H), 6.43 (s, 1H), 6.40 (d, J = 8.4 Hz, 1H), 6.28 (s, 1H), 3.69 (s, 3H); 13C NMR (100 MHz, CDCl3) δ 198.1, 161.2, 155.3, 135.1, 135.0, 133.8, 130.0, 129.8, 128.9, 127.0, 116.6, 107.0, 102.8, 72.1, 55.3; HRMS (ESI-QTOF) m/z [M+Na]+ calcd for C15H13ClNaO4 315.0395, found 315.0411.
1-(4-Bromophenyl)-2-hydroxy-2-(2-hydroxy-4-methoxyphenyl)ethan-1-one (7e). Ivory solid, mp: 108.1–108.8 °C (72 mg, 65%); 1H NMR (400 MHz, (CD3)2CO) δ 7.95 (d, J = 7.6 Hz, 2H), 7.62 (d, J = 8.4 Hz, 2H), 7.07 (d, J = 8.4 Hz, 1H), 6.43 (s, 1H), 6.39 (d, J = 7.2 Hz, 1H), 6.26 (s, 1H), 3.68 (s, 3H); 13C NMR (100 MHz, (CD3)2CO) δ 160.9, 155.6, 155.5, 133.8, 131.7, 130.3, 129.6, 127.5, 118.3, 105.6, 101.5, 70.5, 54.5; HRMS (ESI-QTOF) m/z [M+Na]+ calcd for C15H13BrNaO4 358.9889, found 358.9912.
1-(5-Bromothiophen-2-yl)-2-hydroxy-2-(2-hydroxy-4-methoxyphenyl)ethan-1-one (7f). Yellow solid, mp: 125.3–125.9 °C (92 mg, 81%); 1H NMR (400 MHz, (CD3)2CO) δ 7.76 (d, J = 3.6 Hz, 1H), 7.26–7.17 (m, 2H), 6.47–6.42 (m, 2H), 6.05 (s, 1H), 3.71 (s, 3H); 13C NMR (100 MHz, (CD3)2CO) δ 191.4, 161.0, 155.6, 142.6, 133.7, 131.8, 129.7, 121.8, 118.5, 105.6, 101.7, 71.3, 54.6; HRMS (ESI-QTOF) m/z [M+H]+ calcd for C13H12BrO4S 342.9634, found 342.9626.
2-Hydroxy-2-(2-hydroxy-4,5-dimethoxyphenyl)-1-phenylethan-1-one (7g). Ivory solid, mp: 145.9–146.3 °C (93 mg, 98%); 1H NMR (400 MHz, CDCl3) δ 7.97 (d, J = 7.6 Hz, 2H), 7.51 (t, J = 7.2 Hz, 1H), 7.37 (t, J = 7.6 Hz, 2H), 6.51 (s, 1H), 6.33 (s, 1H), 6.24 (s, 1H), 3.67 (s, 3H), 3.66 (s, 3H); 13C NMR (100 MHz, CDCl3) δ 199.3, 150.2, 148.4, 143.2, 134.0, 133.4, 128.9, 128.6, 115.5, 111.3, 101.8, 71.5, 56.4, 55.7; HRMS (ESI-QTOF) m/z [M+Na]+ calcd for C16H17O5 311.0890, found 311.0908.
2-Hydroxy-2-(2-hydroxy-4,5-dimethoxyphenyl)-1-(3-methoxyphenyl)ethan-1-one (7h). Ivory solid, mp: 162.9–163.2 °C (85 mg, 81%); 1H NMR (400 MHz, (CD3)2CO) δ 7.66 (d, J = 6.8 Hz, 1H), 7.62 (s, 1H), 7.34 (t, J = 8.0 Hz, 1H), 7.10 (d, J = 6.4 Hz, 1H), 6.73 (s, 1H), 6.51 (s, 1H), 6.32 (s, 1H), 3.81 (s, 3H), 3.70 (s, 3H), 3.64 (s, 3H); 13C NMR (100 MHz, (CD3)2CO) δ 199.1, 159.7, 150.5, 148.6, 143.1, 135.8, 129.5, 120.8, 119.4, 116.8, 113.1, 112.8, 101.0, 70.2, 56.0, 55.0, 54.8; HRMS (ESI-QTOF) m/z [M+Na]+ calcd for C17H18NaO6 341.0996, found 341.1006.
2-Hydroxy-2-(2-hydroxy-4,5-dimethoxyphenyl)-1-(4-methoxyphenyl)ethan-1-one (7i). Ivory solid, mp: 109.7–110.0 °C (100 mg, 95%); 1H NMR (400 MHz, CDCl3) δ 7.97 (d, J = 8.0 Hz, 2H), 6.86 (d, J = 8.0 Hz, 2H), 6.52 (s, 2H), 6.37 (s, 1H), 6.16 (s, 1H), 4.59 (s, 1H), 3.82 (s, 3H), 3.73 (s, 3H), 3.70 (s, 3H); 13C NMR (100 MHz, CDCl3) δ 197.6, 164.2, 150.2, 148.4, 143.3, 131.4, 126.2, 116.0, 113.9, 111.3, 101.9, 71.2, 56.5, 55.7, 55.5; HRMS (ESI-QTOF) m/z [M+H]+ calcd for C17H19O6 319.1176, found 319.1253.
1-(3-Chlorophenyl)-2-hydroxy-2-(2-hydroxy-4,5-dimethoxyphenyl)ethan-1-one (7j). Ivory solid, mp: 139.6–140.2 °C (100 mg, 94%); 1H NMR (400 MHz, (CD3)2CO) δ 8.05 (s, 1H), 7.98 (d, J = 7.6 Hz, 1H), 7.57 (d, J = 8.0 Hz, 1H), 7.46 (t, J = 7.6 Hz, 1H), 6.76 (s, 1H), 6.49 (s, 1H), 6.29 (s, 1H), 3.68 (s, 3H), 3.64 (s, 3H); 13C NMR (100 MHz, CDCl3) δ 199.3, 161.2, 157.6, 142.1, 141.6, 135.0, 130.5, 129.0, 127.8, 125.7, 109.9, 108.0, 100.6, 74.6, 56.3, 56.2; HRMS (ESI-QTOF) m/z [M+Na]+ calcd for C16H15ClNaO5 345.0500, found 340.0502.
2-Hydroxy-2-(2-hydroxy-4,6-dimethoxyphenyl)-1-phenylethan-1-one (7k). Ivory solid, mp: 145.9–146.3 °C (58 mg, 62%); 1H NMR (400 MHz, (CD3)2CO) δ 7.91 (d, J = 5.2 Hz, 2H), 7.50 (t, J = 6.8 Hz, 1H), 7.39 (t, J = 7.6 Hz, 2H), 6.25 (s, 1H), 6.04 (d, J = 8.0 Hz, 2H), 3.72 (s, 3H), 3.68 (s, 3H); 13C NMR (100 MHz, CDCl3) δ 200.2, 161.6, 158.3, 156.9, 133.9, 133.5, 128.4, 128.3, 106.1, 94.6, 91.7, 68.7, 55.6, 55.2; HRMS (ESI-QTOF) m/z [M+Na]+ calcd for C16H16NaO5 311.0890, found 311.0917.
2-(5-(Benzyloxy)-2-hydroxy-4-methoxyphenyl)-2-hydroxy-1-phenylethan-1-one (7l). Ivory solid, mp: 150.1–150.6 °C (72 mg, 60%); 1H NMR (400 MHz, CDCl3) δ 7.86 (d, J = 7.2 Hz, 2H), 7.52 (t, J = 7.2 Hz, 1H), 7.37 (d, J = 7.6 Hz, 2H), 7.34–7.27 (m, 6H), 6.59 (s, 1H), 6.39 (s, 1H), 6.06 (s, 1H), 4.95 (s, 2H), 3.76 (s, 3H); 13C NMR (100 MHz, CDCl3) δ 199.3, 149.5, 148.4, 143.8, 136.5, 134.0, 133.5, 129.0, 128.7, 128.5, 127.9, 127.2, 116.0, 112.3, 103.9, 71.7, 70.7, 56.7; HRMS (ESI-QTOF) m/z [M+Na]+ calcd for C22H20NaO5 387.1203, found 387.1227.
2-(5-(Benzyloxy)-2-hydroxy-4-methoxyphenyl)-2-hydroxy-1-(4-methoxyphenyl)ethan-1-one (7m). Ivory solid, mp: 151.2–151.8 °C (54 mg, 42%); 1H NMR (400 MHz, CDCl3) δ 7.97 (d, J = 8.4 Hz, 2H), 7.37–7.28 (m, 5H), 6.85 (d, J = 8.4 Hz, 2H), 6.55 (s, 1H), 6.50 (s, 1H), 6.38 (s, 1H), 6.14 (s, 1H), 4.96 (s, 2H), 4.58 (s, 1H), 3.81 (s, 3H), 3.68 (s, 3H); 13C NMR (100 MHz, CDCl3) δ 197.6, 164.2, 149.4, 148.4, 143.8, 136.6, 131.5, 128.5, 127.9, 127.2, 126.2, 116.6, 113.9, 112.2, 103.9, 71.2, 70.7, 56.8, 55.5; HRMS (ESI-QTOF) m/z [M+Na]+ calcd for C23H22NaO6 417.1309, found 417.1324.
2-Hydroxy-2-(6-hydroxybenzo[d][1,3]dioxol-5-yl)-1-phenylethan-1-one (7n). Ivory solid, mp: 139.2–139.9 °C (72 mg, 80%);
1H NMR (400 MHz, CDCl
3) δ 7.97 (d,
J = 7.2 Hz, 2H), 7.54 (d,
J = 7.6 Hz, 1H), 7.41 (t,
J = 7.6 Hz, 2H), 6.48 (s, 1H), 6.44 (s, 1H), 6.31 (s, 1H), 6.21 (d,
J = 4.4 Hz, 1H), 5.82 (d,
J = 4.0 Hz, 2H), 4.55 (d,
J = 4.4 Hz, 1H);
13C NMR (100 MHz, CDCl
3) δ 199.0, 149.3, 148.6, 141.8, 134.1, 133.3, 129.0, 128.7, 116.7, 107.4, 101.3, 99.6, 71.7;
HRMS (ESI-QTOF)
m/
z [M+Na]
+ calcd for C
15H
12NaO
5 295.0577, found 295.0592.
1-(4-Bromophenyl)-2-hydroxy-2-(6-hydroxybenzo[d][1,3]dioxol-5-yl)ethan-1-one (7o). Ivory solid, mp: 108.1–108.8 °C (81 mg, 70%);
1H NMR (400 MHz, (CD
3)
2SO) δ 9.62 (s, 1H), 7.87 (d,
J = 6.8 Hz, 2H), 7.67 (d,
J = 8.0 Hz, 2H), 6.62 (s, 1H), 6.40 (s, 1H), 6.12 (s, 1H), 5.88 (s, 1H), 5.84 (s, 1H), 5.68 (s, 1H);
13C NMR (100 MHz, (CD
3)
2SO) δ 198.6, 149.4, 147.7, 140.4, 134.4, 132.1, 130.6, 127.7, 118.0, 107.5, 101.3, 98.1, 69.7;
HRMS (ESI-QTOF)
m/
z [M+Na]
+ calcd for C
15H
11BrNaO
5 372.9682, found 372.9685.
2-Hydroxy-2-(2-hydroxynaphthalen-1-yl)-1-phenylethan-1-one (7p). White solid, mp: 114.8–115.5 °C (84 mg, 92%); 1H NMR (400 MHz, (CD3)2CO) δ 8.04 (d, J = 6.8 Hz, 1H), 7.90–7.75 (m, 4H), 7.47 (t, J = 6.8 Hz, 1H), 7.42–7.29 (m, 4H), 7.21 (d, J = 8.0 Hz, 1H), 6.25 (s, 1H); 13C NMR (100 MHz, (CD3)2CO) δ 155.3, 135.1, 132.5, 131.0, 129.4, 128.6, 128.5, 128.2, 127.6, 126.8, 126.1, 123.0, 122.8, 118.3, 117.7, 108.8; HRMS (ESI-QTOF) m/z [M+Na]+ calcd for C18H14NaO3 301.0835, found 301.0854.
2-Hydroxy-2-(1-hydroxynaphthalen-2-yl)-1-phenylethan-1-one (7q). Ivory solid, mp: 118.8–119.2 °C (73 mg, 80%); 1H NMR (400 MHz, (CD3)2CO) δ 8.23 (s, 1H), 8.06 (s, 2H), 7.76 (s, 1H), 7.56–7.51 (m, 1H), 7.49–7.41 (m, 4H), 7.36 (s, 2H), 6.54 (s, 1H); 13C NMR (100 MHz, CDCl3) δ 198.9, 151.2, 134.4, 134.1, 133.6, 129.0, 128.7, 127.5, 126.9, 125.7, 125.6, 125.5, 121.9, 120.7, 117.0, 74.2; HRMS (ESI-QTOF) m/z [M+Na]+ calcd for C18H14NaO3 301.0835, found 301.0855.
3.1.2. General Procedure for the Synthesis of 8
A reaction mixture of 7 (0.08 mmol, 1 equiv), indole (1.5 equiv), and PTSA (0.2 equiv) in CHCl3 (2.0 mL) was stirred at 60 °C for 18 h. The reaction mixture was concentrated in vacuo to give the crude residue, which was purified by silica gel column chromatography (hexane/ethyl acetate/dichloromethane = 30:1:2) to afford 8.
3-(6-Methoxy-2-phenylbenzofuran-3-yl)-1H-indole (8a). Ivory solid, mp: 69.5–70.1 °C (26 mg, 97%); 1H NMR (400 MHz, CDCl3) δ 8.36 (s, 1H), 7.72 (d, J = 7.2 Hz, 2H), 7.49 (d, J = 7.6 Hz, 1H), 7.37 (s, 1H), 7.32 (t, J = 8.8 Hz, 2H), 7.25–7.21 (m, 3H), 7.14 (s, 1H), 7.06 (t, J = 6.8 Hz, 1H), 6.86 (d, J = 8.8 Hz, 1H), 3.91 (s, 3H); 13C NMR (100 MHz, CDCl3) δ 158.3, 155.0, 150.0, 136.4, 131.3, 128.3, 127.6, 126.6, 126.2, 124.7, 123.5, 122.5, 120.8, 120.7, 112.0, 111.6, 111.3, 110.2, 107.9, 95.7, 55.8; HRMS (ESI-QTOF) m/z [M+H]+ calcd for C23H18NO2 340.1332, found 340.1316.
3-(6-Methoxy-2-phenylbenzofuran-3-yl)-4-methyl-1H-indole (8b). Brown solid, mp: 74.8–75.2 °C (27 mg, 97%); 1H NMR (400 MHz, CDCl3) δ 8.34 (s, 1H), 7.67 (d, J = 8.0 Hz, 2H), 7.35 (d, J = 8.0 Hz, 1H), 7.25–7.21 (m, 2H), 7.20–7.14 (m, 4H), 7.12 (s, 1H), 6.88–6.81 (m, 2H), 3.90 (s, 3H), 2.18 (s, 3H); 13C NMR (100 MHz, CDCl3) δ 158.3, 154.4, 150.7, 136.6, 131.7, 131.3, 128.4, 127.4, 126.6, 126.3, 125.6, 123.6, 122.6, 121.3, 120.8, 112.0, 111.8, 109.1, 107.6, 95.5, 55.8, 18.8; HRMS (ESI-QTOF) m/z [M+H]+ calcd for C24H20NO2 354.1489, found 354.1472.
5-Chloro-3-(6-methoxy-2-phenylbenzofuran-3-yl)-2-methyl-1H-indole (8c). Yellow solid, mp: 94.2–94.8 °C (30 mg, 96%); 1H NMR (400 MHz, CDCl3) δ 8.13 (s, 1H), 7.64 (d, J = 7.6 Hz, 2H), 7.32–7.27 (m, 3H), 7.25–7.21 (m, 2H), 7.18–7.12 (m, 3H), 6.85 (d, J = 8.4 Hz, 1H), 3.91 (s, 3H), 2.17 (s, 3H); 13C NMR (100 MHz, CDCl3) δ 158.4, 155.0, 150.5, 134.6, 134.1, 131.4, 129.4, 128.4, 127.6, 125.6, 124.3, 121.8, 120.8, 118.9, 111.7, 111.4, 109.2, 107.5, 104.5, 95.8, 55.8, 12.6; HRMS (ESI-QTOF) m/z [M+H]+ calcd for C24H19ClNO2 388.1099, found 388.1025.
6-Chloro-3-(6-methoxy-2-phenylbenzofuran-3-yl)-1H-indole (8d). Brown solid, mp: 128.5–128.9 °C (29 mg, 98%); 1H NMR (400 MHz, CDCl3) δ 8.35 (s, 1H), 7.66 (d, J = 6.8 Hz, 2H), 7.48 (s, 1H), 7.37 (s, 1H), 7.29 (d, J = 8.8 Hz, 2H), 7.25–7.22 (m, 2H), 7.20 (d, J = 8.4 Hz, 1H), 7.13 (s, 1H), 7.01 (d, J = 8.8 Hz, 1H), 6.86 (d, J = 8.4 Hz, 1H), 3.90 (s, 3H); 13C NMR (100 MHz, CDCl3) δ 158.4, 155.0, 150.2, 136.7, 131.1, 128.4, 128.4, 127.7, 126.2, 125.1, 124.4, 124.1, 121.6, 120.8, 120.5, 111.8, 111.2, 109.5, 108.2, 95.8, 55.8; HRMS (ESI-QTOF) m/z [M+H]+ calcd for C23H17ClNO2 374.0942, found 374.0922.
5-Bromo-3-(6-methoxy-2-phenylbenzofuran-3-yl)-1H-indole (8e). Brown solid, mp: 183.5–184.6 °C (31 mg, 92%); 1H NMR (400 MHz, CDCl3) δ 8.38 (s, 1H), 7.69–7.65 (m, 2H), 7.46 (s, 1H), 7.35 (s, 3H), 7.30–7.27 (m, 3H), 7.25–7.24 (m, 1H), 7.16–7.13 (m, 1H), 6.87 (d, J = 8.4 Hz, 1H), 3.91 (s, 3H); 13C NMR (100 MHz, CDCl3) δ 158.4, 155.0, 150.4, 135.0, 131.1, 128.5, 128.4, 127.8, 126.2, 125.5, 124.6, 124.4, 123.1, 120.5, 113.4, 112.7, 111.8, 109.3, 107.8, 95.8, 55.8; HRMS (ESI-QTOF) m/z [M+H]+ calcd for C23H17BrNO2 418.0437, found 418.0437.
7-Bromo-3-(6-methoxy-2-phenylbenzofuran-3-yl)-1H-indole (8f). Brown solid, mp: 107.2–107.9 °C (23 mg, 69%); 1H NMR (400 MHz, CDCl3) δ 8.55 (s, 1H), 7.68 (d, J = 7.2 Hz, 2H), 7.43–7.39 (m, 2H), 7.32–7.27 (m, 2H), 7.25–7.22 (m, 3H), 7.14 (s, 1H), 6.93 (t, J = 8.0 Hz, 1H), 6.86 (d, J = 8.4 Hz, 1H), 3.90 (s, 3H); 13C NMR (100 MHz, CDCl3) δ 158.4, 155.0, 150.2, 135.1, 131.1, 128.3, 127.7, 126.2, 125.9, 124.8, 124.4, 124.0, 121.2, 120.5, 120.0, 111.8, 109.6, 109.3, 104.8, 95.8, 55.8; HRMS (ESI-QTOF) m/z [M+H]+ calcd for C23H17BrNO2 418.0437, found 418.0415.
5-Iodo-3-(6-methoxy-2-phenylbenzofuran-3-yl)-1H-indole (8g). Brown solid, mp: 135.1–135.9 °C (35 mg, 94%); 1H NMR (400 MHz, CDCl3) δ 8.39 (s, 1H), 7.65 (s, 3H), 7.50 (d, J = 8.4 Hz, 1H), 7.32–7.27 (m, 4H), 7.25–7.23 (m, 2H), 7.13 (s, 1H), 6.87 (d, J = 7.6 Hz, 1H), 3.90 (s, 3H); 13C NMR (100 MHz, CDCl3) δ 158.4, 155.0, 150.4, 135.4, 131.1, 130.9, 129.4, 129.2, 128.3, 127.8, 126.2, 124.4, 124.2, 120.5, 113.2, 111.8, 109.3, 107.4, 95.8, 83.5, 55.8; HRMS (ESI-QTOF) m/z [M+H]+ calcd for C23H17INO2 466.0298, found 466.0244.
3-(6-Methoxy-2-phenylbenzofuran-3-yl)-1-methyl-1H-indole (8h). Ivory solid, mp: 148.9–149.5 °C (15 mg, 54%); 1H NMR (400 MHz, CDCl3) δ 7.72 (d, J = 6.4 Hz, 2H), 7.42 (d, J = 7.6 Hz, 1H), 7.35–7.27 (m, 3H), 7.26–7.21 (m, 4H), 7.12 (s, 1H), 7.04 (t, J = 7.2 Hz, 1H), 6.85 (d, J = 8.4 Hz, 1H), 3.90–3.87 (m, 6H); 13C NMR (100 MHz, CDCl3) δ 158.3, 155.0, 149.8, 137.2, 131.4, 128.2, 128.0, 127.5, 127.0, 126.2, 124.7, 121.9, 120.9, 120.8, 119.5, 111.6, 110.2, 109.4, 106.2, 95.7, 55.8, 33.0; HRMS (ESI-QTOF) m/z [M+H]+ calcd for C24H20NO2 354.1489, found 354.1474.
3-(6-Methoxy-2-(3-methoxyphenyl)benzofuran-3-yl)-1H-indole (8i). White solid, mp: 136.5–136.9 °C (19 mg, 65%); 1H NMR (400 MHz, CDCl3) δ 8.37 (s, 1H), 7.48 (d, J = 7.2 Hz, 1H), 7.40 (s, 1H), 7.32 (d, J = 8.4 Hz, 3H), 7.24 (s, 2H), 7.16 (d, J = 7.6 Hz, 1H), 7.13 (s, 1H), 7.06 (t, J = 7.6 Hz, 1H), 6.86 (d, J = 8.4 Hz, 1H), 6.76 (d, J = 7.6 Hz, 1H), 3.90 (s, 3H), 3.51 (s, 3H); 13C NMR (100 MHz, CDCl3) δ 159.3, 158.4, 154.9, 149.8, 136.3, 132.5, 129.3, 126.4, 124.6, 123.6, 122.5, 120.8, 120.7, 120.0, 118.6, 114.1, 111.7, 111.2, 110.7, 107.9, 106.4, 95.6, 55.8, 54.9; HRMS (ESI-QTOF) m/z [M+H]+ calcd for C24H20NO3 370.1438, found 370.1427.
3-(6-Methoxy-2-(naphthalen-2-yl)benzofuran-3-yl)-1-methyl-1H-indole (8j). Ivory solid, mp: 110.5–110.9 °C (21 mg, 65%); 1H NMR (400 MHz, CDCl3) δ 8.30 (s, 1H), 7.80–7.70 (m, 3H), 7.61 (d, J = 8.8 Hz, 1H), 7.47–7.42 (m, 3H), 7.36 (t, J = 8.4 Hz, 2H), 7.31–7.27 (m, 2H), 7.17 (s, 1H), 7.02 (t, J = 7.6 Hz, 1H), 6.87 (t, J = 8.4 Hz, 1H), 3.91 (s, 6H); 13C NMR (100 MHz, CDCl3) δ 158.4, 155.1, 149.7, 137.2, 133.3, 132.6, 128.9, 128.3, 128.2, 127.6, 127.6, 127.1, 126.2, 126.0, 125.0, 124.7, 124.2, 122.0, 121.0, 120.9, 119.6, 111.6, 110.9, 109.4, 106.2, 95.6, 55.8, 33.1; HRMS (ESI-QTOF) m/z [M+H]+ calcd for C28H22NO2 404.1645, found 404.1626.
3-(2-(3-Chlorophenyl)-6-methoxybenzofuran-3-yl)-1H-indole (8k). Ivory solid, mp: 140.3–140.8 °C (26 mg, 87%); 1H NMR (400 MHz, CDCl3) δ 8.38 (s, 1H), 7.78 (s, 1H), 7.49 (d, J = 8.0 Hz, 2H), 7.37 (s, 1H), 7.34–7.28 (m, 2H), 7.26–7.23 (m, 1H), 7.18–7.14 (m, 1H), 7.12–7.05 (m, 3H), 6.85 (d, J = 8.4 Hz, 1H), 3.89 (s, 3H); 13C NMR (100 MHz, CDCl3) δ 158.7, 155.1, 148.3, 136.3, 134.3, 133.0, 129.5, 128.7, 127.4, 126.3, 125.8, 124.3, 124.1, 123.5, 122.6, 121.0, 120.6, 120.1, 111.9, 111.3, 107.5, 95.6, 55.8; HRMS (ESI-QTOF) m/z [M+H]+ calcd for C23H17ClNO2 374.0942, found 374.0919.
4-Bromo-3-(2-(4-bromophenyl)-6-methoxybenzofuran-3-yl)-1H-indole (8l). Yellow solid, mp: 207.5–207.9 °C (30 mg, 75%); 1H NMR (400 MHz, CDCl3) δ 8.47 (s, 1H), 7.47 (t, J = 8.4 Hz, 3H), 7.34 (d, J = 8.4 Hz, 2H), 7.29 (d, J = 7.6 Hz, 1H), 7.25–7.23 (m, 1H), 7.16–7.08 (m, 3H), 6.84 (d, J = 8.4 Hz, 1H), 3.89 (s, 3H); 13C NMR (100 MHz, CDCl3) δ 158.4, 154.4, 150.4, 137.2, 131.5, 130.4, 127.2, 126.6, 125.9, 125.2, 124.7, 123.6, 121.4, 121.0, 114.5, 111.9, 110.9, 110.7, 108.0, 95.4, 55.8; HRMS (ESI-QTOF) m/z [M+H]+ calcd for C23H16Br2NO2 495.9542, found 495.9517.
3-(2-(5-Bromothiophen-2-yl)-6-methoxybenzofuran-3-yl)-1H-indole (8m). Brown solid, mp: 74.8–75.2 °C (18 mg, 54%); 1H NMR (400 MHz, CDCl3) δ 8.40 (s, 1H), 7.50 (d, J = 8.4 Hz, 1H), 7.45 (d, J = 2.0 Hz, 1H), 7.39 (d, J = 8.0 Hz, 1H), 7.30–7.27 (m, 2H), 7.17 (d, J = 4.4 Hz, 1H), 7.13–7.07 (m, 2H), 6.94 (t, J = 4.8 Hz, 1H), 6.84 (dd, J = 8.4, 1.6 Hz, 1H), 3.89 (s, 3H); 13C NMR (100 MHz, CDCl3) δ 158.4, 154.8, 146.6, 136.3, 133.2, 127.2, 126.6, 125.0, 124.7, 124.4, 124.1, 122.5, 120.6, 120.6, 120.0, 111.7, 111.3, 109.4, 107.0, 95.7, 55.8; HRMS (ESI-QTOF) m/z [M+H]+ calcd for C21H15BrNO2S 424.0001, found 424.0004.
3-(5,6-Dimethoxy-2-phenylbenzofuran-3-yl)-1H-indole (8n). Brown solid, mp: 183.7–184.2 °C (24 mg, 80%); 1H NMR (400 MHz, CDCl3) δ 8.39 (s, 1H), 7.67 (d, J = 8.0 Hz, 2H), 7.50 (d, J = 8.0 Hz, 1H), 7.38–7.34 (m, 2H), 7.27–7.19 (m, 4H), 7.15 (s, 1H), 7.07 (t, J = 8.0 Hz, 1H), 6.85 (s, 1H), 3.98 (s, 3H), 3.80 (s, 3H); 13C NMR (100 MHz, CDCl3) δ 150.2, 148.7, 148.3, 146.6, 136.4, 131.4, 128.2, 127.4, 126.6, 126.0, 123.4, 123.2, 122.5, 120.7, 120.0, 111.3, 110.4, 108.1, 101.7, 95.1, 56.4; HRMS (ESI-QTOF) m/z [M+H]+ calcd for C24H20NO3 370.1438, found 370.1428.
3-(5,6-Dimethoxy-2-(3-methoxyphenyl)benzofuran-3-yl)-1H-indole (8o). Brown solid, mp: 128.9–129.4 °C (28 mg, 89%); 1H NMR (400 MHz, CDCl3) δ 8.44 (s, 1H), 7.49 (d, J = 7.2 Hz, 1H), 7.42–7.34 (m, 2H), 7.32–7.27 (m, 1H), 7.22–7.12 (m, 4H), 7.08 (t, J = 7.2 Hz, 1H), 6.86 (s, 1H), 6.76 (d, J = 5.2 Hz, 1H), 3.99 (s, 3H), 3.81 (s, 3H), 3.51 (s, 3H); 13C NMR (100 MHz, CDCl3) δ 159.3, 150.0, 148.6, 148.4, 146.6, 136.3, 132.5, 129.3, 126.6, 123.5, 123.2, 122.5, 120.7, 120.1, 118.4, 113.9, 111.3, 110.7, 110.6, 108.0, 101.7, 95.1, 56.4, 54.9; HRMS (ESI-QTOF) m/z [M+H]+ calcd for C25H22NO4 400.1543, found 400.1550.
6-Bromo-3-(5,6-dimethoxy-2-(4-methoxyphenyl)benzofuran-3-yl)-1H-indole (8p). Brown solid, mp: 249.9–250.4 °C (31 mg, 81%); 1H NMR (400 MHz, CDCl3) δ 8.43 (s, 1H), 7.64 (s, 1H), 7.56 (d, J = 8.4 Hz, 2H), 7.34 (s, 1H), 7.21–7.13 (m, 3H), 6.79 (s, 2H), 6.77 (s, 1H), 3.97 (s, 3H), 3.81 (s, 3H), 3.78 (s, 3H); 13C NMR (100 MHz, CDCl3) δ 159.1, 150.5, 148.4, 147.9, 146.5, 137.1, 127.4, 125.5, 124.0, 123.9, 123.4, 123.1, 121.9, 116.1, 114.2, 113.8, 108.5, 108.0, 101.3, 95.1, 56.4, 55.2; HRMS (ESI-QTOF) m/z [M+Na]+ calcd for C25H20BrNNaO4 500.0468, found 500.0473.
3-(2-(3-Chlorophenyl)-5,6-dimethoxybenzofuran-3-yl)-5-iodo-1H-indole (8q). Brown solid, mp: 230.7–231.0 °C (42 mg, 99%); 1H NMR (400 MHz, CDCl3) δ 8.48 (s, 1H), 7.71 (s, 2H), 7.53 (d, J = 8.4 Hz, 1H), 7.45 (d, J = 7.6 Hz, 1H), 7.34–7.28 (m, 2H), 7.20–7.12 (m, 3H), 6.79 (s, 1H), 3.99 (s, 3H), 3.83 (s, 3H); 13C NMR (100 MHz, CDCl3) δ 148.8, 148.7, 146.8, 135.4, 134.3, 132.8, 131.1, 129.6, 129.3, 129.0, 127.5, 125.7, 124.2, 123.9, 122.6, 113.4, 110.8, 107.0, 101.5, 95.1, 83.7, 56.4; HRMS (ESI-QTOF) m/z [M+Na]+ calcd for C24H17ClINNaO3 551.9834, found 551.9838.
3-(4,6-Dimethoxy-2-phenylbenzofuran-3-yl)-6-methyl-1H-indole (8r). Brown solid, mp: 154.9–155.5 °C (25 mg, 80%); 1H NMR (400 MHz, CDCl3) δ 8.10 (s, 1H), 7.58 (d, J = 8.0 Hz, 2H), 7.24–7.17 (m, 6H), 6.86 (d, J = 8.0 Hz, 1H), 6.76 (s, 1H), 6.30 (s, 1H), 3.89 (s, 3H), 3.58 (s, 3H), 2.47 (s, 3H); 13C NMR (100 MHz, CDCl3) δ 159.0, 156.0, 155.0, 149.2, 136.4, 131.6, 131.4, 128.1, 127.2, 126.1, 125.3, 123.8, 121.4, 120.6, 114.0, 110.9, 109.5, 108.3, 94.5, 87.9, 55.8, 55.5, 21.8; HRMS (ESI-QTOF) m/z [M+H]+ calcd for C25H22NO3 384.1594, found 384.1590.
3-(5-(Benzyloxy)-6-methoxy-2-phenylbenzofuran-3-yl)-1H-indole (8s). Brown solid, mp: 162.7–163.2 °C (35 mg, 99%); 1H NMR (400 MHz, CDCl3) δ 8.38 (s, 1H), 7.68 (d, J = 6.8 Hz, 2H), 7.48 (d, J = 8.0 Hz, 1H), 7.43–7.39 (m, 2H), 7.37–7.22 (m, 9H), 7.18 (s, 1H), 7.05 (t, J = 7.2 Hz, 1H), 6.95 (s, 1H), 5.05 (s, 2H), 3.98 (s, 3H); 13C NMR (100 MHz, CDCl3) δ 150.1, 149.2, 149.2, 145.6, 137.2, 136.3, 131.4, 128.4, 128.2, 127.8, 127.6, 127.4, 126.5, 126.1, 123.4, 123.2, 122.4, 120.7, 120.1, 111.2, 110.4, 108.0, 105.4, 95.6, 71.9, 56.5; HRMS (ESI-QTOF) m/z [M+H]+ calcd for C30H24NO3 446.1751, found 446.1755.
2-(6-(Benzyloxy)-5-methoxy-2-(4-methoxyphenyl)benzofuran-3-yl)-3-methyl-1H-indole (8t). Brown solid, mp: 194.8–195.2 °C (25 mg, 65%); 1H NMR (400 MHz, CDCl3) δ 7.98 (s, 1H), 7.67 (d, J = 7.6 Hz, 1H), 7.53 (d, J = 8.8 Hz, 2H), 7.49 (d, J = 7.6 Hz, 2H), 7.43–7.37 (m, 3H), 7.36–7.31 (m, 1H), 7.25–7.18 (m, 2H), 7.12 (s, 1H), 6.83 (d, J = 8.8 Hz, 2H), 6.80 (s, 1H), 5.24 (s, 2H), 3.85 (s, 3H), 3.79 (s, 3H), 2.20 (s, 3H); 13C NMR (100 MHz, CDCl3) δ 159.5, 151.7, 148.1, 147.5, 147.0, 136.9, 136.3, 129.4, 128.6, 127.9, 127.3, 126.0, 123.3, 122.9, 122.1, 119.3, 118.9, 114.1, 110.9, 107.0, 101.7, 97.9, 71.5, 56.6, 55.2, 9.5; HRMS (ESI-QTOF) m/z [M+H]+ calcd for C32H28NO4 490.2013, found 490.2007.
3-(6-Phenyl-[1,3]dioxolo[4,5-f]benzofuran-7-yl)-1H-indole (8u). Brown solid, mp: 193.9–194.4 °C (19 mg, 68%);
1H NMR (400 MHz, CDCl
3) δ 8.33 (s, 1H), 7.66 (d,
J = 8.0 Hz, 2H), 7.47 (d,
J = 8.0 Hz, 1H), 7.34–7.30 (m, 2H), 7.25–7.18 (m, 4H), 7.08–7.03 (m, 2H), 6.79 (s, 1H), 5.97 (s, 2H);
13C NMR (100 MHz, CDCl
3) δ 150.6, 149.2, 146.4, 144.5, 136.3, 131.3, 128.3, 127.5, 126.5, 126.0, 124.7, 123.4, 122.5, 120.6, 120.0, 111.3, 110.7, 107.9, 101.3, 99.1, 93.3;
HRMS (ESI-QTOF)
m/
z [M+H]
+ calcd for C
23H
16NO
3 354.1125, found 354.1118.
7-Methyl-3-(6-phenyl-[1,3]dioxolo[4,5-f]benzofuran-7-yl)-1H-indole (8v). Brown solid, mp: 185.8–186.4 °C (27 mg, 92%);
1H NMR (400 MHz, CDCl
3) δ 8.27 (s, 1H), 7.69 (d,
J = 7.6 Hz, 2H), 7.31 (s, 1H), 7.25–7.20 (m, 4H), 7.11–7.05 (m, 2H), 7.00 (t,
J = 6.4 Hz, 1H), 6.82–6.80 (m, 1H), 5.99 (s, 2H), 2.58 (s, 3H);
13C NMR (100 MHz, CDCl
3) δ 150.5, 149.2, 146.3, 144.5, 136.0, 131.3, 128.3, 127.5, 126.1, 126.0, 124.7, 123.2, 123.0, 120.5, 120.2, 118.4, 110.9, 108.3, 101.3, 99.1, 93.3, 16.7;
HRMS (ESI-QTOF)
m/
z [M+H]
+ calcd for C
24H
18NO
3 368.1281, found 368.1259.
3-(6-(4-Bromophenyl)-[1,3]dioxolo[4,5-f]benzofuran-7-yl)-5-methyl-1H-indole (8w). Brown solid, mp: 205.4–206.0 °C (32 mg, 89%);
1H NMR (400 MHz, CDCl
3) δ 8.28 (s, 1H), 7.53 (d,
J = 8.4 Hz, 2H), 7.38 (d,
J = 8.8 Hz, 1H), 7.35 (d,
J = 8.8 Hz, 2H), 7.13–7.09 (m, 2H), 7.06 (s, 1H), 6.78 (s, 1H), 5.99 (s, 2H), 2.36 (s, 3H);
13C NMR (100 MHz, CDCl
3) δ 149.5, 149.2, 146.6, 144.6, 134.6, 131.4, 130.2, 129.6, 127.3, 126.7, 124.7, 124.3, 123.5, 121.3, 119.9, 111.5, 111.0, 106.9, 101.3, 99.1, 93.3, 21.5;
HRMS (ESI-QTOF)
m/
z [M+H]
+ calcd for C
24H
16BrNO
3 445.0314, found 445.0315.
3-(2-Phenylnaphtho[2,1-b]furan-1-yl)-1H-indole (8x). Brown solid, mp: 148.2–148.9 °C (25 mg, 88%); 1H NMR (400 MHz, CDCl3) δ 8.41 (s, 1H), 7.92 (d, J = 8.0 Hz, 1H), 7.79 (s, 2H), 7.67–7.61 (m, 3H), 7.57 (d, J = 8.4 Hz, 1H), 7.43 (d, J = 7.6 Hz, 1H), 7.39–7.32 (m, 2H), 7.31–7.29 (m, 1H), 7.25–7.19 (m, 3H), 7.15 (t, J = 7.6 Hz, 1H), 7.09 (t, J = 7.2 Hz, 1H); 13C NMR (100 MHz, CDCl3) δ 151.69, 151.66, 136.5, 131.1, 130.8, 128.7, 128.6, 128.3, 127.8, 127.7, 126.1, 125.9, 125.7, 124.6, 124.2, 123.6, 123.2, 122.7, 120.5, 120.4, 112.3, 111.3, 111.2, 109.2; HRMS (ESI-QTOF) m/z [M+H]+ calcd for C26H18NO 360.1383, found 360.1370.
2-Methyl-3-(2-phenylnaphtho[1,2-b]furan-3-yl)-1H-indole (8y). Brown solid, mp: 95.3–95.9 °C (19 mg, 62%); 1H NMR (400 MHz, CDCl3) δ 8.51 (d, J = 8.4 Hz, 1H), 8.13 (s, 1H), 7.96 (d, J = 8.0 Hz, 1H), 7.83 (d, J = 8.0 Hz, 2H), 7.69–7.61 (m, 2H), 7.53 (t, J = 7.6 Hz, 1H), 7.43 (d, J = 7.6 Hz, 2H), 7.37 (d, J = 8.0 Hz, 1H), 7.32 (t, J = 7.2 Hz, 2H), 7.28–7.27 (m, 1H), 7.25–7.21 (m, 1H), 7.09 (t, J = 8.0 Hz, 1H), 2.23 (s, 3H); 13C NMR (100 MHz, CDCl3) δ 150.6, 149.5, 135.8, 133.1, 131.7, 131.6, 130.1, 129.2, 128.5, 128.3, 127.6, 126.7, 126.5, 126.3, 125.8, 125.1, 123.2, 121.6, 121.4, 120.2, 119.9, 119.7, 119.6, 110.4, 12.7; HRMS (ESI-QTOF) m/z [M+H]+ calcd for C27H20NO 374.1539, found 374.1544.
5-Chloro-3-(6-methoxy-2-phenylbenzofuran-3-yl)-1H-indole (8z). Ivory solid, mp: 88.2–88.9 °C (28 mg, 92%); 1H NMR (400 MHz, CDCl3) δ 8.40 (s, 1H), 7.67 (d, J = 8.0 Hz, 2H), 7.42–7.36 (m, 2H), 7.31–7.27 (m, 3H), 7.25–7.19 (m, 3H), 7.14 (s, 1H), 6.87 (d, J = 8.4 Hz, 1H), 3.91 (s, 3H); 13C NMR (100 MHz, CDCl3) δ 158.4, 155.0, 150.3, 134.7, 131.1, 128.4, 127.8, 126.1, 125.8, 124.8, 124.4, 122.9, 120.5, 120.0, 112.3, 111.8, 109.4, 107.8, 95.7, 55.8; HRMS (ESI-QTOF) m/z [M+H]+ calcd for C23H17ClNO2 374.0942, found 374.0951.
5-Bromo-3-(5,6-dimethoxy-2-phenylbenzofuran-3-yl)-1H-indole (8aa). White solid, mp: 100.2–100.5 °C (29 mg, 81%); 1H NMR (400 MHz, CDCl3) δ 8.46 (s, 1H), 7.63 (d, J = 7.6 Hz, 2H), 7.49 (s, 1H), 7.37–7.31 (m, 3H), 7.25–7.21 (m, 3H), 7.15 (s, 1H), 6.79 (s, 1H), 3.97 (s, 3H), 3.81 (s, 3H); 13C NMR (100 MHz, CDCl3) δ 150.4, 148.6, 148.3, 146.6, 134.9, 131.1, 128.5, 128.3, 127.6, 125.9, 125.5, 124.6, 123.0, 122.9, 113.4, 112.8, 109.5, 107.8, 101.4, 95.1, 56.4, 56.3; HRMS (ESI-QTOF) m/z [M+Na]+ calcd for C24H18BrNNaO3 470.0362, found 470.0356.
5-Bromo-3-(5,6-dimethoxy-2-(4-methoxyphenyl)benzofuran-3-yl)-1H-indole (8ab). Ivory solid, mp: 92.2–92.9 °C (34 mg, 89%); 1H NMR (400 MHz, (CD3)2CO) δ 7.67 (s, 1H), 7.59–7.55 (m, 2H), 7.52 (d, J = 8.4 Hz, 1H), 7.30–7.28 (m, 1H), 7.26–7.24 (m, 1H), 6.88 (s, 1H), 6.84 (d, J = 8.8 Hz, 3H), 3.90 (s, 3H), 3.77 (s, 3H), 3.73 (s, 3H); 13C NMR (100 MHz, (CD3)2CO) δ 159.4, 150.0, 148.8, 148.5, 147.2, 135.6, 128.3, 127.2, 126.2, 126.0, 124.4, 124.0, 122.9, 122.2, 113.8, 112.1, 108.5, 106.5, 102.0, 95.5, 55.68, 55.65, 54.7; HRMS (ESI-QTOF) m/z [M+Na]+ calcd for C25H20BrNNaO4 500.0468, found 500.0454.
5-Bromo-3-(6-phenyl-[1,3]dioxolo[4,5-f]benzofuran-7-yl)-1H-indole (8ac). Ivory solid, mp: 110.2–110.9 °C (33 mg, 96%);
1H NMR (400 MHz, CDCl
3) δ 8.38 (s, 1H), 7.63–7.59 (m, 2H), 7.44 (s, 1H), 7.34 (s, 2H), 7.31–7.29 (m, 1H), 7.25–7.21 (m, 3H), 7.07 (s, 1H), 6.73 (s, 1H), 5.98 (s, 2H);
13C NMR (100 MHz, CDCl
3) δ 150.9, 149.2, 146.5, 144.6, 134.9, 131.0, 128.4, 128.3, 127.7, 125.9, 125.5, 124.6, 124.5, 122.9, 113.4, 112.8, 109.9, 107.6, 101.3, 98.8, 93.4;
HRMS (ESI-QTOF)
m/
z [M+H]
+ calcd for C
23H
15BrNO
3 432.0230, found 423.0211.
5-Iodo-3-(6-phenyl-[1,3]dioxolo[4,5-f]benzofuran-7-yl)-1H-indole (8ad). Ivory solid, mp: 113.9–114.2 °C (36 mg, 94%);
1H NMR (400 MHz, CDCl
3) δ 8.38 (s, 1H), 7.63 (s, 1H), 7.60 (d,
J = 8.0 Hz, 2H), 7.49 (d,
J = 8.8 Hz, 1H), 7.28–7.21 (m, 5H), 7.07 (s, 1H), 6.72 (s, 1H), 5.98 (s, 2H);
13C NMR (100 MHz, CDCl
3) δ 151.0, 149.2, 146.5, 144.6, 135.4, 131.0, 130.9, 129.2, 129.1, 128.3, 127.7, 125.9, 124.5, 124.2, 113.3, 109.8, 107.3, 101.3, 98.7, 93.4, 83.6;
HRMS (ESI-QTOF)
m/
z [M+H]
+ calcd for C
23H
15INO
3 480.0091, found 480.0061.