Anticancer Mechanism of Astragalus Polysaccharide and Its Application in Cancer Immunotherapy
Abstract
1. Introduction
2. Anticancer Mechanism of Astragalus Polysaccharide
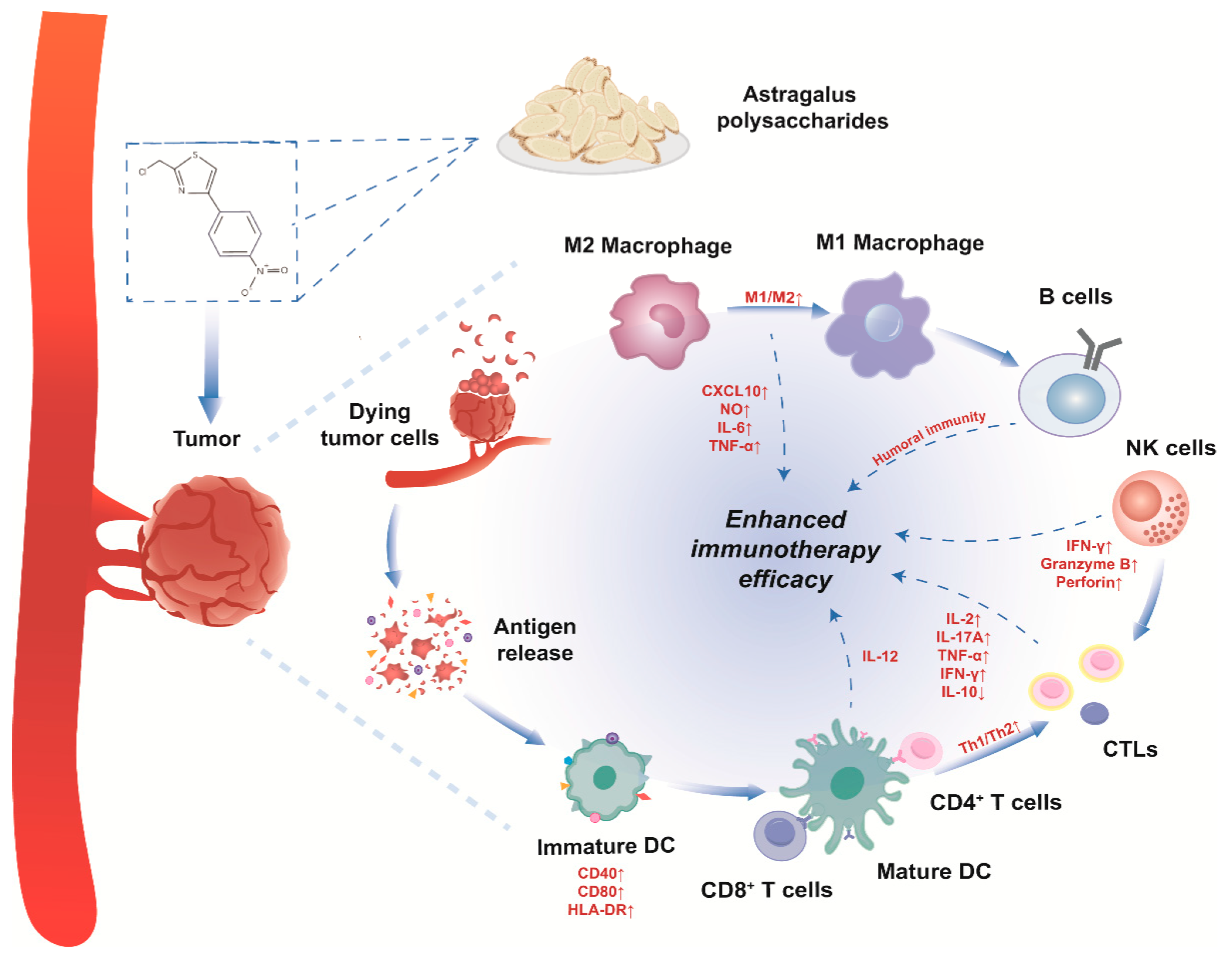
2.1. Activation and Regulation of Immune Cells
2.2. Anti-Proliferative and Apoptosis-Inducing Effects on Cancer Cells
2.2.1. APS Interferes with the Cell Cycle
2.2.2. APS Inhibits Signal Transduction Pathways
2.2.3. APS Induces Apoptosis in Cancer Cells
2.3. Other Antitumor Effects of APS
2.3.1. APS Activates Cellular Autophagy
2.3.2. APS Inhibits Lipid Metabolism
2.3.3. APS Affects the Tumour Microenvironment and Regulates Cytokine and Hormone Levels
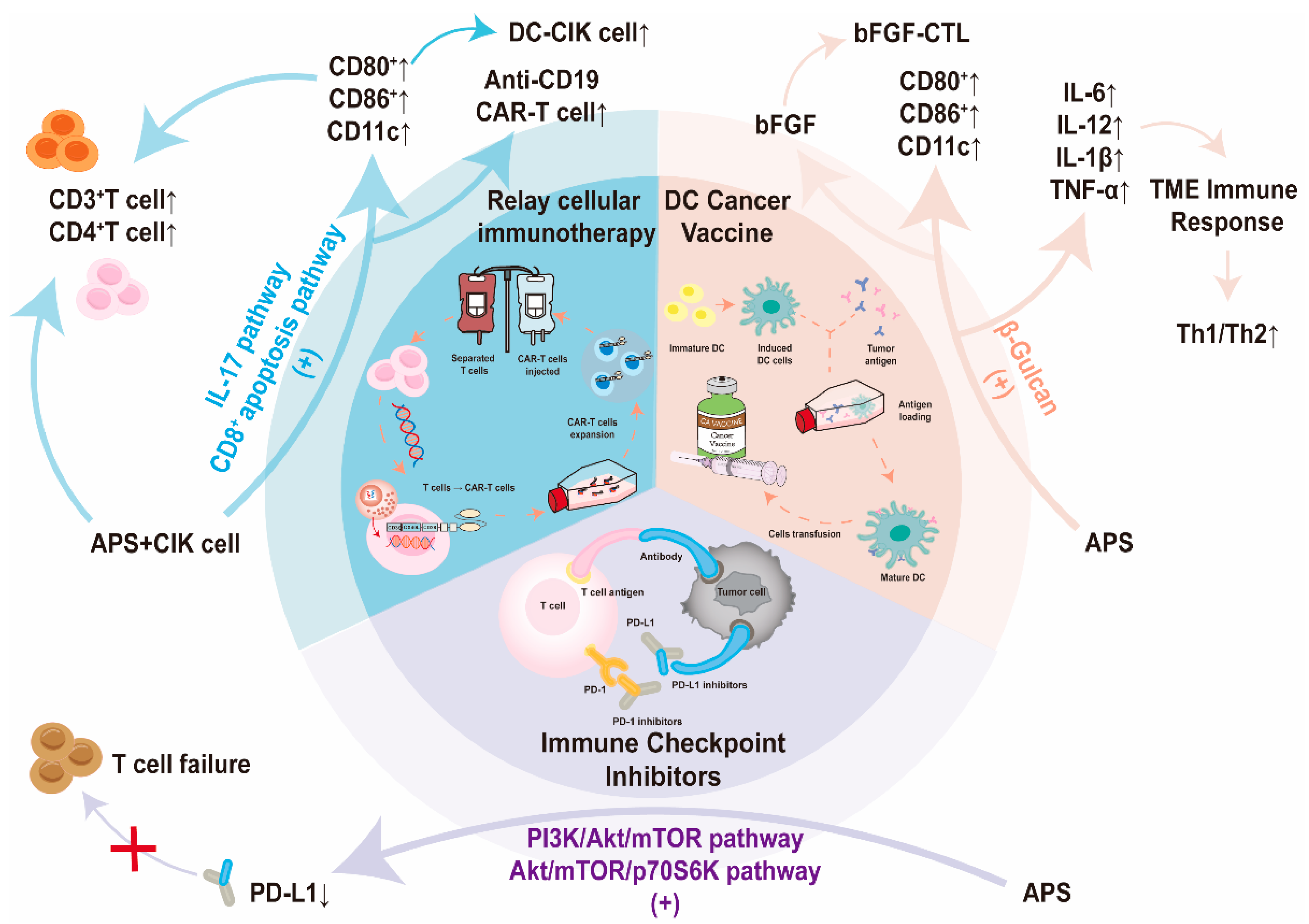
3. APS-Assisted Cancer Immunotherapy
3.1. APS Boosts the Effectiveness of Immune Checkpoint Inhibitors in Therapy
3.2. APS Enhances Relay Cellular Immunotherapy
3.3. Utilizing APS as an Adjunct to Enhance the Effectiveness of Cancer Vaccines in Therapy
4. Clinical Trials on the Antitumor Effects of APS
4.1. Malignant Tumors of the Digestive System
4.2. Malignant Tumors of the Respiratory System
4.3. Other Malignant Tumors
5. Comparison of Anticancer Effects of Astragalus Polysaccharide and Other Polysaccharides
5.1. Astragalus Polysaccharide and β-Glucan
5.2. Astragalus Polysaccharide and Pectin Polysaccharide
5.3. Astragalus Polysaccharide and Xanthanate Gum
5.4. Astragalus Polysaccharide and Marine Complex Polysaccharide Substances
5.5. Production of Astragalus Polysaccharide
6. Conclusions and Outlook
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Wagle, N.S.; Jemal, A. Cancer Statistics, 2023. CA Cancer J. Clin. 2023, 73, 17–48. [Google Scholar] [CrossRef] [PubMed]
- Stoop, T.F.; Theijse, R.T.; Seelen, L.W.F.; Groot Koerkamp, B.; Van Eijck, C.H.J.; Wolfgang, C.L.; Van Tienhoven, G.; Van Santvoort, H.C.; Molenaar, I.Q.; Wilmink, J.W.; et al. Preoperative Chemotherapy, Radiotherapy and Surgical Decision-Making in Patients with Borderline Resectable and Locally Advanced Pancreatic Cancer. Nat. Rev. Gastroenterol. Hepatol. 2024, 21, 101–124. [Google Scholar] [CrossRef] [PubMed]
- Bukowski, K.; Kciuk, M.; Kontek, R. Mechanisms of Multidrug Resistance in Cancer Chemotherapy. Int. J. Mol. Sci. 2020, 21, 3233. [Google Scholar] [CrossRef] [PubMed]
- Engle, K.; Kumar, G. Cancer Multidrug-Resistance Reversal by ABCB1 Inhibition: A Recent Update. Eur. J. Med. Chem. 2022, 239, 114542. [Google Scholar] [CrossRef] [PubMed]
- Abdelbaky, S.B.; Ibrahim, M.T.; Samy, H.; Mohamed, M.; Mohamed, H.; Mustafa, M.; Abdelaziz, M.M.; Forrest, M.L.; Khalil, I.A. Cancer Immunotherapy from Biology to Nanomedicine. J. Control. Release 2021, 336, 410–432. [Google Scholar] [CrossRef]
- Nygren, P.; SBU-group. Swedish Council on Technology Assessment in Health Care What Is Cancer Chemotherapy? Acta Oncol. 2001, 40, 166–174. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.; Kim, S.W.; Charchoghlyan, H.; Jeong, H.; Han, G.D. Combinatorial Herbal Extracts Alleviate Alcohol-Induced Hepatic Disorders. Plant Foods Hum. Nutr. 2023, 78, 432–438. [Google Scholar] [CrossRef] [PubMed]
- Pu, R.; Zhang, L.; Zhou, X.; Yin, W.; Zhang, X.; Liu, H.; Duan, X.; Yu, C.; Luo, X.; Zhong, Q.; et al. Strategy of Using Herbal Extract Preparations for Stage IV Cancer in Palliative Care: An Enhanced and Maintenance Therapy. J. Clin. Oncol. 2016, 34, 89. [Google Scholar] [CrossRef]
- Nai, J.; Zhang, C.; Shao, H.; Li, B.; Li, H.; Gao, L.; Dai, M.; Zhu, L.; Sheng, H. Extraction, Structure, Pharmacological Activities and Drug Carrier Applications of Angelica Sinensis Polysaccharide. Int. J. Biol. Macromol. 2021, 183, 2337–2353. [Google Scholar] [CrossRef]
- Wang, Y.; Zhang, Q.; Chen, Y.; Liang, C.L.; Liu, H.; Qiu, F.; Dai, Z. Antitumor Effects of Immunity-Enhancing Traditional Chinese Medicine. Biomed. Pharmacother. 2020, 121, 109570. [Google Scholar] [CrossRef]
- Tian, X.; Liang, T.; Liu, Y.; Ding, G.; Zhang, F.; Ma, Z. Extraction, Structural Characterization, and Biological Functions of Lycium barbarum Polysaccharides: A Review. Biomolecules 2019, 9, 389. [Google Scholar] [CrossRef] [PubMed]
- Sun, K.; Wu, L.; Wang, S.; Deng, W. Antitumor Effects of Chinese Herbal Medicine Compounds and Their Nano-Formulations on Regulating the Immune System Microenvironment. Front. Oncol. 2022, 12, 949332. [Google Scholar] [CrossRef] [PubMed]
- Jin, M.; Zhao, K.; Huang, Q.; Shang, P. Structural Features and Biological Activities of the Polysaccharides from Astragalus membranaceus. Int. J. Biol. Macromol. 2014, 64, 257–266. [Google Scholar] [CrossRef] [PubMed]
- Zhao, M.; Zhang, Z.F.; Ding, Y.; Wang, J.B.; Li, Y. Astragalus Polysaccharide Improves Palmitate-Induced Insulin Resistance by Inhibiting PTP1B and NF-κB in C2C12 Myotubes. Molecules 2012, 17, 7083–7092. [Google Scholar] [CrossRef] [PubMed]
- Fan, Y.; Hu, Y.; Wang, D.; Liu, J.; Zhang, J.; Zhao, X.; Liu, X.; Liu, C.; Yuan, J.; Ruan, S. Effects of Astragalus Polysaccharide Liposome on Lymphocyte Proliferation In Vitro and Adjuvanticity In Vivo. Carbohydr. Polym. 2012, 88, 68–74. [Google Scholar] [CrossRef]
- Tian, Q.-E.; Li, H.-D.; Yan, M.; Cai, H.-L.; Tan, Q.-Y.; Zhang, W.-Y. Astragalus Polysaccharides Can Regulate Cytokine and P-Glycoprotein Expression in H22 Tumor-Bearing Mice. World J. Gastroenterol. 2012, 18, 7079–7086. [Google Scholar] [CrossRef] [PubMed]
- Gong, H.; Li, W.; Sun, J.; Jia, L.; Guan, Q.; Guo, Y.; Wang, Y. A Review on Plant Polysaccharide Based on Drug Delivery System for Construction and Application, with Emphasis on Traditional Chinese Medicine Polysaccharide. Int. J. Biol. Macromol. 2022, 211, 711–728. [Google Scholar] [CrossRef] [PubMed]
- Xu, Q.; Cheng, W.; Wei, J.; Ou, Y.; Xiao, X.; Jia, Y. Synergist for Antitumor Therapy: Astragalus Polysaccharides Acting on Immune Microenvironment. Discov. Oncol. 2023, 14, 179. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Qin, L.; Huang, J.; Li, Y.; Xu, S.; Wang, H.; Zhu, S.; Wang, J.; Zhu, B.; Li, F.; et al. Astragalus Polysaccharide Attenuates LPS-Related Inflammatory Osteolysis by Suppressing Osteoclastogenesis by Reducing the MAPK Signalling Pathway. J. Cell. Mol. Med. 2021, 25, 6800–6814. [Google Scholar] [CrossRef]
- Long, H.; Lin, H.; Zheng, P.; Hou, L.; Zhang, M.; Lin, S.; Yin, K.; Zhao, G. WTAP Mediates the Anti-Inflammatory Effect of Astragalus mongholicus Polysaccharide on THP-1 Macrophages. Front. Pharmacol. 2022, 13, 1023878. [Google Scholar] [CrossRef]
- Yan, X.; Miao, J.; Zhang, B.; Liu, H.; Ma, H.; Sun, Y.; Liu, P.; Zhang, X.; Wang, R.; Kan, J.; et al. Study on Semi-Bionic Extraction of Astragalus Polysaccharide and Its Anti-Aging Activity in Vivo. Front. Nutr. 2023, 10, 1201919. [Google Scholar] [CrossRef] [PubMed]
- Dong, M.; Li, J.; Yang, D.; Li, M.; Wei, J. Biosynthesis and Pharmacological Activities of Flavonoids, Triterpene Saponins and Polysaccharides Derived from Astragalus membranaceus. Molecules 2023, 28, 5018. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Y.; Ren, W.; Zhang, L.; Zhang, Y.; Liu, D.; Liu, Y. A Review of the Pharmacological Action of Astragalus Polysaccharide. Front. Pharmacol. 2020, 11, 349. [Google Scholar] [CrossRef] [PubMed]
- Yang, B.; Xiao, B.; Sun, T. Antitumor and Immunomodulatory Activity of Astragalus membranaceus Polysaccharides in H22 Tumor-Bearing Mice. Int. J. Biol. Macromol. 2013, 62, 287–290. [Google Scholar] [CrossRef] [PubMed]
- Guo, L.; Bai, S.P.; Zhao, L.; Wang, X.H. Astragalus Polysaccharide Injection Integrated with Vinorelbine and Cisplatin for Patients with Advanced Non-Small Cell Lung Cancer: Effects on Quality of Life and Survival. Med. Oncol. 2012, 29, 1656–1662. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.M.; Park, H.B.; Jin, J.O. Polysaccharide from Astragalus membranaceus Promotes the Activation of Human Peripheral Blood and Mouse Spleen Dendritic Cells. Chin. J. Nat. Med. 2021, 19, 56–62. [Google Scholar] [CrossRef] [PubMed]
- Zhu, N.; Lv, X.; Wang, Y.; Li, J.; Liu, Y.; Lu, W.; Yang, L.; Zhao, J.; Wang, F.; Zhang, L.W. Comparison of Immunoregulatory Effects of Polysaccharides from Three Natural Herbs and Cellular Uptake in Dendritic Cells. Int. J. Biol. Macromol. 2016, 93, 940–951. [Google Scholar] [CrossRef]
- Chang, W.T.; Lai, T.H.; Chyan, Y.J.; Yin, S.Y.; Chen, Y.H.; Wei, W.C.; Yang, N.S. Specific Medicinal Plant Polysaccharides Effectively Enhance the Potency of a DC-Based Vaccine against Mouse Mammary Tumor Metastasis. PLoS ONE 2015, 10, e0122374. [Google Scholar] [CrossRef]
- Pang, G.; Chen, C.; Liu, Y.; Jiang, T.; Yu, H.; Wu, Y.; Wang, Y.; Wang, F.J.; Liu, Z.; Zhang, L.W. Bioactive Polysaccharide Nanoparticles Improve Radiation-Induced Abscopal Effect through Manipulation of Dendritic Cells. ACS Appl. Mater. Interfaces 2019, 11, 42661–42670. [Google Scholar] [CrossRef]
- Bamodu, O.A.; Kuo, K.T.; Wang, C.H.; Huang, W.C.; Wu, A.T.H.; Tsai, J.T.; Lee, K.Y.; Yeh, C.T.; Wang, L.S. Astragalus Polysaccharides (PG2) Enhances the M1 Polarization of Macrophages, Functional Maturation of Dendritic Cells, and T Cell-Mediated Anticancer Immune Responses in Patients with Lung Cancer. Nutrients 2019, 11, 2264. [Google Scholar] [CrossRef]
- Hwang, J.; Zhang, W.; Dhananjay, Y.; An, E.K.; Kwak, M.; You, S.; Lee, P.C.W.; Jin, J.O. Astragalus membranaceus Polysaccharides Potentiate the Growth-Inhibitory Activity of Immune Checkpoint Inhibitors against Pulmonary Metastatic Melanoma in Mice. Int. J. Biol. Macromol. 2021, 182, 1292–1300. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.; Liu, Z.; Long, T.; Zhou, L.; Bao, Y. Immunomodulatory Effects of Herbal Formula of Astragalus Polysaccharide (APS) and Polysaccharopeptide (PSP) in Mice with Lung Cancer. Int. J. Biol. Macromol. 2018, 106, 596–601. [Google Scholar] [CrossRef] [PubMed]
- Yu, Z.; Wang, D.; Qi, Y.; Liu, J.; Zhou, T.; Rao, W.; Hu, K. Autologous-Cancer-Cryoablation-Mediated Nanovaccine Augments Systematic Immunotherapy. Mater. Horiz. 2023, 10, 1661–1677. [Google Scholar] [CrossRef]
- Xu, S.; Wu, Z.; Cai, G.; Zhang, Y.; Peng, S.; Jiao, L.; Liu, Z.; Yang, Y.; Wang, D. Astragalus Polysaccharides Combined with Simvastatin as an Immunostimulant Enhances the Immune Adjuvanticity of Oil-in-Water Emulsion and Immune Responses in Mice. Vaccine 2023, 41, 1684–1693. [Google Scholar] [CrossRef] [PubMed]
- Meng, Y.; Zhang, Y.; Jia, N.; Qiao, H.; Zhu, M.; Meng, Q.; Lu, Q.; Zu, Y. Synthesis and Evaluation of a Novel Water-Soluble High Se-Enriched Astragalus Polysaccharide Nanoparticles. Int. J. Biol. Macromol. 2018, 118, 1438–1448. [Google Scholar] [CrossRef] [PubMed]
- Wei, W.; Li, Z.P.; Bian, Z.X.; Han, Q.B. Astragalus Polysaccharide RAP Induces Macrophage Phenotype Polarization to M1 via the Notch Signaling Pathway. Molecules 2019, 24, 2016. [Google Scholar] [CrossRef] [PubMed]
- Wei, W.; Xiao, H.T.; Bao, W.R.; Ma, D.L.; Leung, C.H.; Han, X.Q.; Ko, C.H.; Lau, C.B.S.; Wong, C.K.; Fung, K.P.; et al. TLR-4 May Mediate Signaling Pathways of Astragalus Polysaccharide RAP Induced Cytokine Expression of RAW264.7 Cells. J. Ethnopharmacol. 2016, 179, 243–252. [Google Scholar] [CrossRef]
- Lee, Y.S.; Han, O.K.; Park, C.W.; Yang, C.H.; Jeon, T.W.; Yoo, W.K.; Kim, S.H.; Kim, H.J. Pro-Inflammatory Cytokine Gene Expression and Nitric Oxide Regulation of Aqueous Extracted Astragali Radix in RAW 264.7 Macrophage Cells. J. Ethnopharmacol. 2005, 100, 289–294. [Google Scholar] [CrossRef]
- Li, W.; Hu, X.; Wang, S.; Wang, H.; Parungao, R.; Wang, Y.; Liu, T.; Song, K. Detection and Evaluation of Anti-Cancer Efficiency of Astragalus Polysaccharide via a Tissue Engineered Tumor Model. Macromol. Biosci. 2018, 18, 1800223. [Google Scholar] [CrossRef]
- Shao, B.M.; Xu, W.; Dai, H.; Tu, P.; Li, Z.; Gao, X.M. A Study on the Immune Receptors for Polysaccharides from the Roots of Astragalus membranaceus, a Chinese Medicinal Herb. Biochem. Biophys. Res. Commun. 2004, 320, 1103–1111. [Google Scholar] [CrossRef]
- Wu, J.; Xu, H.; Zhang, L.; Zhang, X. Radix Astragali and Tanshinone Help Carboplatin Inhibit B16 Tumor Cell Growth. Technol. Cancer Res. Treat. 2016, 15, 583–588. [Google Scholar] [CrossRef]
- Yu, J.; Ji, H.; Liu, A. Alcohol-Soluble Polysaccharide from Astragalus membranaceus: Preparation, Characteristics and Antitumor Activity. Int. J. Biol. Macromol. 2018, 118, 2057–2064. [Google Scholar] [CrossRef] [PubMed]
- Mu, J.Y.; Li, Y.D.; Zhao, X.K.; Li, J.; Yang, A.J. Astragalus Polysaccharide Restores Activation of NK Cells in Radiation Therapy of Tumors. Int. J. Clin. Exp. Med. 2019, 12, 8609–8621. [Google Scholar]
- Wculek, S.K.; Cueto, F.J.; Mujal, A.M.; Melero, I.; Krummel, M.F.; Sancho, D. Dendritic Cells in Cancer Immunology and Immunotherapy. Nat. Rev. Immunol. 2020, 20, 7–24. [Google Scholar] [CrossRef] [PubMed]
- Banchereau, J.; Briere, F.; Caux, C.; Davoust, J.; Lebecque, S.; Liu, Y.J.; Pulendran, B.; Palucka, K. Immunobiology of Dendritic Cells. Annu. Rev. Immunol. 2000, 18, 767–811. [Google Scholar] [CrossRef] [PubMed]
- Joffre, O.P.; Segura, E.; Savina, A.; Amigorena, S. Cross-Presentation by Dendritic Cells. Nat. Rev. Immunol. 2012, 12, 557–569. [Google Scholar] [CrossRef] [PubMed]
- Cao, Y.; Chen, Z.; Sun, L.; Lin, Y.; Yang, Y.; Cui, X.; Wang, C. Herb Polysaccharide-Based Drug Delivery System: Fabrication, Properties, and Applications for Immunotherapy. Pharmaceutics 2022, 14, 1703. [Google Scholar] [CrossRef] [PubMed]
- Sanmamed, M.F.; Chen, L. A Paradigm Shift in Cancer Immunotherapy: From Enhancement to Normalization. Cell 2019, 176, 677. [Google Scholar] [CrossRef] [PubMed]
- O’Donnell, J.S.; Teng, M.W.L.; Smyth, M.J. Cancer Immunoediting and Resistance to T Cell-Based Immunotherapy. Nat. Rev. Clin. Oncol. 2019, 16, 151–167. [Google Scholar] [CrossRef]
- Raskov, H.; Orhan, A.; Christensen, J.P.; Gögenur, I. Cytotoxic CD8+ T Cells in Cancer and Cancer Immunotherapy. Br. J. Cancer 2021, 124, 359–367. [Google Scholar] [CrossRef]
- Banstola, A.; Jeong, J.H.; Yook, S. Immunoadjuvants for Cancer Immunotherapy: A Review of Recent Developments. Acta Biomater. 2020, 114, 16–30. [Google Scholar] [CrossRef] [PubMed]
- Li, C.X.; Liu, Y.; Zhang, Y.Z.; Li, J.C.; Lai, J. Astragalus Polysaccharide: A Review of Its Immunomodulatory Effect. Arch. Pharm. Res. 2022, 45, 367–389. [Google Scholar] [CrossRef] [PubMed]
- Crotty, S. Follicular Helper CD4+ T Cells (TFH). Annu. Rev. Immunol. 2011, 29, 621–663. [Google Scholar] [CrossRef] [PubMed]
- Sheu, K.M.; Hoffmann, A. Functional Hallmarks of Healthy Macrophage Responses: Their Regulatory Basis and Disease Relevance. Annu. Rev. Immunol. 2022, 40, 295–321. [Google Scholar] [CrossRef] [PubMed]
- Kong, F.; Chen, T.; Li, X.; Jia, Y. The Current Application and Future Prospects of Astragalus Polysaccharide Combined With Cancer Immunotherapy: A Review. Front. Pharmacol. 2021, 12, 737674. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.; Dong, X.; Jiao, J.; Ji, H.; Liu, A. Antitumor and Immunoregulatory Activities of a Novel Polysaccharide from Astragalus membranaceus on S180 Tumor-Bearing Mice. Int. J. Biol. Macromol. 2021, 189, 930–938. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.; Ji, H.; Dong, X.; Feng, Y.; Liu, A. Apoptosis of Human Gastric Carcinoma MGC-803 Cells Induced by a Novel Astragalus membranaceus Polysaccharide via Intrinsic Mitochondrial Pathways. Int. J. Biol. Macromol. 2019, 126, 811–819. [Google Scholar] [CrossRef] [PubMed]
- Jiao, J.; Yu, J.; Ji, H.; Liu, A. Synthesis of Macromolecular Astragalus Polysaccharide-Nano Selenium Complex and the Inhibitory Effects on HepG2 Cells. Int. J. Biol. Macromol. 2022, 211, 481–489. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Hu, X.; Wang, S.; Jiao, Z.; Sun, T.; Liu, T.; Song, K. Characterization and Anti-Tumor Bioactivity of Astragalus Polysaccharides by Immunomodulation. Int. J. Biol. Macromol. 2020, 145, 985–997. [Google Scholar] [CrossRef]
- Bao, W.R.; Li, Z.P.; Zhang, Q.W.; Li, L.F.; Liu, H.B.; Ma, D.L.; Leung, C.H.; Lu, A.P.; Bian, Z.X.; Han, Q.B. Astragalus Polysaccharide RAP Selectively Attenuates Paclitaxel-Induced Cytotoxicity Toward RAW 264.7 Cells by Reversing Cell Cycle Arrest and Apoptosis. Front. Pharmacol. 2019, 9, 1580. [Google Scholar] [CrossRef]
- Li, W.; Song, K.; Wang, S.; Zhang, C.; Zhuang, M.; Wang, Y.; Liu, T. Anti-Tumor Potential of Astragalus Polysaccharides on Breast Cancer Cell Line Mediated by Macrophage Activation. Mater. Sci. Eng. C 2019, 98, 685–695. [Google Scholar] [CrossRef]
- Chen, L.; He, C.; Zhou, M.; Long, J.; Li, L. Research Progress on the Mechanisms of Polysaccharides against Gastric Cancer. Molecules 2022, 27, 5828. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.L.; Lin, Z.W.; He, P.T.; Nie, H.; Yao, Q.Y.; Zhang, S.Y. Inhibitory Effect of Astragalus Polysaccharide Combined with Cisplatin on Cell Cycle and Migration of Nasopharyngeal Carcinoma Cell Lines. Biol. Pharm. Bull. 2021, 44, 926–931. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Yu, J.; Wang, J.; Zhang, C.; Shang, K.; Yao, X.; Cao, B. Astragalus Polysaccharide Enhanced Antitumor Effects of Apatinib in Gastric Cancer AGS Cells by Inhibiting AKT Signalling Pathway. Biomed. Pharmacother. 2018, 100, 176–183. [Google Scholar] [CrossRef]
- Wang, F.; Bai, J.; Li, F.; Liu, J.; Wang, Y.; Li, N.; Wang, Y.; Xu, J.; Liu, W.; Xu, L.; et al. Investigation of the Mechanism of the Anti-Cancer Effects of Astragalus Propinquus Schischkin and Pinellia Pedatisecta Schott (A&P) on Melanoma via Network Pharmacology and Experimental Verification. Front. Pharmacol. 2022, 13, 895738. [Google Scholar] [CrossRef]
- Gong, Q.; Yu, H.; Ding, G.; Ma, J.; Wang, Y.; Cheng, X. Suppression of Stemness and Enhancement of Chemosensibility in the Resistant Melanoma Were Induced by Astragalus Polysaccharide through PD-L1 Downregulation. Eur. J. Pharmacol. 2022, 916, 174726. [Google Scholar] [CrossRef]
- Feng, S.; Ding, H.; Liu, L.; Peng, C.; Huang, Y.; Zhong, F.; Li, W.; Meng, T.; Li, J.; Wang, X.; et al. Astragalus Polysaccharide Enhances the Immune Function of RAW264.7 Macrophages via the NF-κB P65/MAPK Signaling Pathway. Exp. Ther. Med. 2021, 21, 20. [Google Scholar] [CrossRef]
- Song, J.; Peng, L. IDDF2019-ABS-0248 Astragalus Polysaccharide Promotes Adriamycin-Induced Apoptosis in Gastric Cancer Cells. Gut 2019, 68, A25–A26. [Google Scholar] [CrossRef]
- Wu, C.Y.; Ke, Y.; Zeng, Y.F.; Zhang, Y.W.; Yu, H.J. Anticancer Activity of Astragalus Polysaccharide in Human Non-Small Cell Lung Cancer Cells. Cancer Cell Int. 2017, 17, 115. [Google Scholar] [CrossRef]
- Fang, J.; Wu, Z.; Wang, J.; Feng, J.; Ying, L. Astragalus Polysaccharides Inhibit Pancreatic Cancer Progression by Downregulation of TLR4/NF-κB Signaling Pathway. J. Nanomater. 2022, 2022, 5351611. [Google Scholar] [CrossRef]
- Zhang, Y.M.; Liu, Y.Q.; Liu, D.; Zhang, L.; Qin, J.; Zhang, Z.; Su, Y.; Yan, C.; Luo, Y.L.; Li, J.; et al. The Effects of Astragalus Polysaccharide on Bone Marrow-Derived Mesenchymal Stem Cell Proliferation and Morphology Induced by A549 Lung Cancer Cells. Med. Sci. Monit. 2019, 25, 4110–4121. [Google Scholar] [CrossRef]
- Wu, C.; Chen, W.; Fang, M.; Boye, A.; Tao, X.; Xu, Y.; Hou, S.; Yang, Y. Compound Astragalus and Salvia Miltiorrhiza Extract Inhibits Hepatocellular Carcinoma Progression via miR-145/miR-21 Mediated Smad3 Phosphorylation. J. Ethnopharmacol. 2019, 231, 98–112. [Google Scholar] [CrossRef]
- Liu, X.; Yang, Y.; Zhang, X.; Xu, S.; He, S.; Huang, W.; Roberts, M.S. Compound Astragalus and Salvia miltiorrhiza Extract Inhibits Cell Invasion by Modulating Transforming Growth Factor-β/Smad in HepG2 Cell. J. Gastroenterol. Hepatol. 2010, 25, 420–426. [Google Scholar] [CrossRef] [PubMed]
- Lai, X.; Xia, W.; Wei, J.; Ding, X. Therapeutic Effect of Astragalus Polysaccharides on Hepatocellular Carcinoma H22-Bearing Mice. Dose-Response 2017, 15, 155932581668518. [Google Scholar] [CrossRef] [PubMed]
- Xie, R.D.; Sun, S.B.; He, J.X.; Dong, J.N.; Long, F. Effect of astragalus polysaccharide on growth and tumor-related apoptosis protein of human breast cancer Mda-Mb-231 transplanted tumor in nude mice. Chin. J. Exp. Tradit. Med. Form. 2019, 25, 27–43. [Google Scholar] [CrossRef]
- Lv, J.; Zhu, P.F.; Liu, Y.M.; Zeng, Q.L.; Yu, Z.J. Astragalus polysaccharides downregulates apoptosis in Hepg2 cell through Wnt/B-catenin signaling pathway. Chin. Tradit. Herbal Drug. 2018, 49, 5155–5160. [Google Scholar] [CrossRef]
- Li, C.; Hong, L.; Liu, C.; Min, J.; Hu, M.; Guo, W. Astragalus Polysaccharides Increase the Sensitivity of SKOV3 Cells to Cisplatin. Arch. Gynecol. Obstet. 2018, 297, 381–386. [Google Scholar] [CrossRef]
- Zhou, Z.; Meng, M.; Ni, H. Chemosensitizing Effect of Astragalus Polysaccharides on Nasopharyngeal Carcinoma Cells by Inducing Apoptosis and Modulating Expression of Bax/Bcl-2 Ratio and Caspases. Med. Sci. Monit. 2017, 23, 462–469. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Zhang, Z.; Wang, Z.; Liu, G.; Liu, Y.; Wang, H. Astragalus Polysaccharides Inhibit Ovarian Cancer Cell Growth via microRNA-27a/FBXW7 Signaling Pathway. Biosci. Rep. 2020, 40, BSR20193396. [Google Scholar] [CrossRef]
- Chu, Y.; Fang, Y.; Chi, J.; Li, J.; Zhang, D.; Zou, Y.; Wang, Z. Astragalus Polysaccharides Decrease Proliferation, Migration, and Invasion but Increase Apoptosis of Human Osteosarcoma Cells by up-Regulation of microRNA-133a. Braz. J. Med. Biol. Res. 2018, 51, e7665. [Google Scholar] [CrossRef]
- Tao, X.; Zhang, X.; Feng, F. Astragalus Polysaccharide Suppresses Cell Proliferation and Invasion by Up-Regulation of miR-195-5p in Non-Small Cell Lung Cancer. Biol. Pharm. Bull. 2022, 45, 553–560. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.X.; Han, Y.P.; Bai, C.; Li, Q. Notch1/3 and P53/P21 Are a Potential Therapeutic Target for APS-Induced Apoptosis in Non-Small Cell Lung Carcinoma Cell Lines. Int. J. Clin. Exp. Med. 2015, 8, 12539–12547. [Google Scholar] [PubMed]
- Li, C.J.; Shen, G.H. Mechanism of astragalus polysaccharides promote colon cancer stem cell apoptosis byinducing autophagy. Chin. J. Tradit. Chin. Med. Pharm. 2022, 37, 2274–2279. [Google Scholar]
- Li, M.; Duan, F.; Pan, Z.; Liu, X.; Lu, W.; Liang, C.; Fang, Z.; Peng, P.; Jia, D. Astragalus Polysaccharide Promotes Doxorubicin-Induced Apoptosis by Reducing O-GlcNAcylation in Hepatocellular Carcinoma. Cells 2023, 12, 866. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Liu, F.; Zhao, S.; Guo, B.; Ling, P.; Han, G.; Cui, Z. Purification of an Acidic Polysaccharide from Suaeda Salsa Plant and Its Anti-Tumor Activity by Activating Mitochondrial Pathway in MCF-7 Cells. Carbohydr. Polym. 2019, 215, 99–107. [Google Scholar] [CrossRef] [PubMed]
- Jose, G.M.; Raghavankutty, M.; Kurup, G.M. Sulfated Polysaccharides from Padina Tetrastromatica Induce Apoptosis in HeLa Cells through ROS Triggered Mitochondrial Pathway. Process Biochem. 2018, 68, 197–204. [Google Scholar] [CrossRef]
- Hafner, A.; Bulyk, M.L.; Jambhekar, A.; Lahav, G. The Multiple Mechanisms That Regulate P53 Activity and Cell Fate. Nat. Rev. Mol. Cell Biol. 2019, 20, 199–210. [Google Scholar] [CrossRef]
- Zhang, Q.; Gao, L.; Huang, S.; Liang, Y.; Hu, J.; Zhang, Y.; Wei, S.; Hu, X. Cocktail of Astragalus membranaceus and Radix Trichosanthis Suppresses Melanoma Tumor Growth and Cell Migration Through Regulation of Akt-Related Signaling Pathway. Front. Pharmacol. 2022, 13, 880215. [Google Scholar] [CrossRef]
- Backman, L.J.; Danielson, P. Akt-mediated Anti-apoptotic Effects of Substance P in Anti-Fas-induced Apoptosis of Human Tenocytes. J. Cell. Mol. Med. 2013, 17, 723–733. [Google Scholar] [CrossRef]
- Li, S.; Sun, Y.; Huang, J.; Wang, B.; Gong, Y.; Fang, Y.; Liu, Y.; Wang, S.; Guo, Y.; Wang, H.; et al. Anti-Tumor Effects and Mechanisms of Astragalus membranaceus (AM) and Its Specific Immunopotentiation: Status and Prospect. J. Ethnopharmacol. 2020, 258, 112797. [Google Scholar] [CrossRef]
- García-Gómez, R.; Bustelo, X.R.; Crespo, P. Protein–Protein Interactions: Emerging Oncotargets in the RAS-ERK Pathway. Trends Cancer 2018, 4, 616–633. [Google Scholar] [CrossRef] [PubMed]
- Liao, X.; Bu, Y.; Jia, Q. Traditional Chinese Medicine as Supportive Care for the Management of Liver Cancer: Past, Present, and Future. Genes Dis. 2020, 7, 370–379. [Google Scholar] [CrossRef]
- Derynck, R.; Zhang, Y.E. Smad-Dependent and Smad-Independent Pathways in TGF-β Family Signalling. Nature 2003, 425, 577–584. [Google Scholar] [CrossRef] [PubMed]
- Iwayama, H.; Sakamoto, T.; Nawa, A.; Ueda, N. Crosstalk between Smad and Mitogen-Activated Protein Kinases for the Regulation of Apoptosis in Cyclosporine A-Induced Renal Tubular Injury. Nephron Extra 2011, 1, 178–189. [Google Scholar] [CrossRef] [PubMed]
- Yang, Q.; Meng, D.; Zhang, Q.; Wang, J. Advances in Research on the Anti-Tumor Mechanism of Astragalus Polysaccharides. Front. Oncol. 2024, 14, 1334915. [Google Scholar] [CrossRef] [PubMed]
- Akyol, Z.; Çoker-Gürkan, A.; Arisan, E.D.; Obakan-Yerlikaya, P.; Palavan-Ünsal, N. DENSpm Overcame Bcl-2 Mediated Resistance against Paclitaxel Treatment in MCF-7 Breast Cancer Cells via Activating Polyamine Catabolic Machinery. Biomed. Pharmacother. 2016, 84, 2029–2041. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.S.; Dutta, A. MicroRNAs in Cancer. Annu. Rev. Pathol. Mech. Dis. 2009, 4, 199–227. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Ji, G.; Wu, Q.; Feng, S.; Zhao, Y.; Cao, Z.; Tao, C. Integrated Microarray Meta-Analysis Identifies miRNA-27a as an Oncogene in Ovarian Cancer by Inhibiting FOXO1. Life Sci. 2018, 210, 263–270. [Google Scholar] [CrossRef] [PubMed]
- Ding, L.; Zhang, S.; Xu, M.; Zhang, R.; Sui, P.; Yang, Q. MicroRNA-27a Contributes to the Malignant Behavior of Gastric Cancer Cells by Directly Targeting PH Domain and Leucine-Rich Repeat Protein Phosphatase 2. J. Exp. Clin. Cancer Res. 2017, 36, 45. [Google Scholar] [CrossRef] [PubMed]
- Peng, H.; Wang, X.; Zhang, P.; Sun, T.; Ren, X.; Xia, Z. miR-27a Promotes Cell Proliferation and Metastasis in Renal Cell Carcinoma. Int. J. Clin. Exp. Pathol. 2015, 8, 2259–2266. [Google Scholar]
- Cheng, Y.; Wang, Y.; Cheng, Y.; Yang, Q.; Zhang, L.; Li, Z.; Cheng, J. FOXD3-Induced miR-133a Blocks Progression and Metastasis of Colorectal Cancer through Regulating UBA2. J. Cancer 2021, 12, 6145–6154. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Zhu, L.; Lin, X.; Huang, Y.; Lin, Z. MiR-133a-3p Inhibits the Malignant Progression of Oesophageal Cancer by Targeting CDCA8. J. Biochem. 2022, 170, 689–698. [Google Scholar] [CrossRef] [PubMed]
- Sakr, M.; Takino, T.; Sabit, H.; Nakada, M.; Li, Z.; Sato, H. miR-150-5p and miR-133a Suppress Glioma Cell Proliferation and Migration through Targeting Membrane-Type-1 Matrix Metalloproteinase. Gene 2016, 587, 155–162. [Google Scholar] [CrossRef] [PubMed]
- Whibley, C.; Pharoah, P.D.P.; Hollstein, M. P53 Polymorphisms: Cancer Implications. Nat. Rev. Cancer 2009, 9, 95–107. [Google Scholar] [CrossRef]
- Gottlieb, T.M.; Oren, M. P53 and Apoptosis. Semin. Cancer Biol. 1998, 8, 359–368. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, D.I.; Nally, K.; Kelly, R.G.; O’Connor, T.M.; Shanahan, F.; O’Connell, J. Targeting the Fas/Fas Ligand Pathway in Cancer. Expert Opin. Ther. Targets 2005, 9, 1031–1044. [Google Scholar] [CrossRef]
- Liang, X.H.; Jackson, S.; Seaman, M.; Brown, K.; Kempkes, B.; Hibshoosh, H.; Levine, B. Induction of Autophagy and Inhibition of Tumorigenesis by Beclin 1. Nature 1999, 402, 672–676. [Google Scholar] [CrossRef]
- Mathew, R.; Karantza-Wadsworth, V.; White, E. Role of Autophagy in Cancer. Nat. Rev. Cancer 2007, 7, 961–967. [Google Scholar] [CrossRef]
- Yang, Z.J.; Chee, C.E.; Huang, S.; Sinicrope, F.A. The Role of Autophagy in Cancer: Therapeutic Implications. Mol. Cancer Ther. 2011, 10, 1533–1541. [Google Scholar] [CrossRef]
- Cordani, M.; Somoza, Á. Targeting Autophagy Using Metallic Nanoparticles: A Promising Strategy for Cancer Treatment. Cell. Mol. Life Sci. 2019, 76, 1215–1242. [Google Scholar] [CrossRef]
- Wang, X.; Li, Y.; Liu, D.; Wang, Y.; Ming, H. Astragalus polysaccharide inhibits autophagy and regulates expression of autophagy-related proteins in lung cancer A549 cells induced by xanthine oxidase. Chin. J. Cell. Mol. Immunol. 2019, 35, 619–624. [Google Scholar]
- Duan, Z.; Liang, M.; Yang, C.; Yan, C.; Wang, L.; Song, J.; Han, L.; Fan, Y.; Li, W.; Liang, T.; et al. Selenium Nanoparticles Coupling with Astragalus Polysaccharides Exert Their Cytotoxicities in MCF-7 Cells by Inhibiting Autophagy and Promoting Apoptosis. J. Trace Elem. Med. Biol. 2022, 73, 127006. [Google Scholar] [CrossRef] [PubMed]
- Zhai, Q.L.; Hu, X.D.; Xiao, J.; Yu, D.Q. Astragalus polysaccharide may increase sensitivity of cervical cancer HeLa cells to cisplatin by regulating cell autophagy. J. Chin. Mater. Medica 2018, 43, 805–812. [Google Scholar] [CrossRef] [PubMed]
- Röhrig, F.; Schulze, A. The Multifaceted Roles of Fatty Acid Synthesis in Cancer. Nat. Rev. Cancer 2016, 16, 732–749. [Google Scholar] [CrossRef] [PubMed]
- Li, D.; Li, Y. The Interaction between Ferroptosis and Lipid Metabolism in Cancer. Signal Transduct. Target. Ther. 2020, 5, 108. [Google Scholar] [CrossRef]
- Cheng, C.; Geng, F.; Cheng, X.; Guo, D. Lipid Metabolism Reprogramming and Its Potential Targets in Cancer. Cancer Commun. 2018, 38, 27. [Google Scholar] [CrossRef]
- Pope, E.D.; Kimbrough, E.O.; Vemireddy, L.P.; Surapaneni, P.K.; Copland, J.A.; Mody, K. Aberrant Lipid Metabolism as a Therapeutic Target in Liver Cancer. Expert Opin. Ther. Targets 2019, 23, 473–483. [Google Scholar] [CrossRef]
- Yi, M.; Li, J.; Chen, S.; Cai, J.; Ban, Y.; Peng, Q.; Zhou, Y.; Zeng, Z.; Peng, S.; Li, X.; et al. Emerging Role of Lipid Metabolism Alterations in Cancer Stem Cells. J. Exp. Clin. Cancer Res. 2018, 37, 118. [Google Scholar] [CrossRef]
- Cheng, L.; Zhu, Y.; Han, H.; Zhang, Q.; Cui, K.; Shen, H.; Zhang, J.; Yan, J.; Prochownik, E.; Li, Y. MicroRNA-148a Deficiency Promotes Hepatic Lipid Metabolism and Hepatocarcinogenesis in Mice. Cell Death Dis. 2017, 8, e2916. [Google Scholar] [CrossRef]
- Pham, D.V.; Park, P.H. Adiponectin Triggers Breast Cancer Cell Death via Fatty Acid Metabolic Reprogramming. J. Exp. Clin. Cancer Res. 2022, 41, 9. [Google Scholar] [CrossRef]
- Guo, S.; Ma, B.; Jiang, X.; Li, X.; Jia, Y. Astragalus Polysaccharides Inhibits Tumorigenesis and Lipid Metabolism Through miR-138-5p/SIRT1/SREBP1 Pathway in Prostate Cancer. Front. Pharmacol. 2020, 11, 598. [Google Scholar] [CrossRef]
- Pitt, J.M.; Marabelle, A.; Eggermont, A.; Soria, J.-C.; Kroemer, G.; Zitvogel, L. Targeting the Tumor Microenvironment: Removing Obstruction to Anticancer Immune Responses and Immunotherapy. Ann. Oncol. 2016, 27, 1482–1492. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Y.; Yu, D. Tumor Microenvironment as a Therapeutic Target in Cancer. Pharmacol. Ther. 2021, 221, 107753. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.N.; Gui, M.B.; Qu, L.P.; Zou, M.; Gao, F. Astragalus polysaccharide inhibits IDO1 expression in colon tumor microenvironment to increase intratumoral CD8+ T cell infiltration. China J. Chin. Mater. Medica 2023, 48, 4722–4730. [Google Scholar] [CrossRef] [PubMed]
- Elham, S.; Mohammad-Reza, S.; Kobra, E.; Samaneh, K.; Mona, A.; Morteza, M.; Elahe, S. Immunomodulatory Effects of Astragalus Polysaccharide on Human Peripheral Blood Mononuclear Cells Co-Cultured with Cervical Cancer Cell Line. J. Tradit. Chin. Med. 2021, 41, 684–694. [Google Scholar] [CrossRef] [PubMed]
- Zhao, L.; Zhong, Y.; Liang, J.; Gao, H.; Tang, N. Effect of Astragalus Polysaccharide on the Expression of VEGF and EGFR in Mice with Lewis Transplantable Lung Cancer. J. Coll. Physicians Surg. Pak. 2019, 29, 392–394. [Google Scholar] [CrossRef]
- Lee, Y.C.; Huang, H.T.; Chang, C.D.; Chen, C.T.; Lin, T.Y.; Yang, T.W.; Chang, F.L.; Lu, M.K.; Chiou, C.T.; Chen, W.C.; et al. Isolation of Anti-VEGF Monoclonal Antibodies with Neutralizing Effects from an Astragalus-Induced Immune Antibody Library. Int. Immunopharmacol. 2020, 88, 107007. [Google Scholar] [CrossRef] [PubMed]
- Brock, S.E.; Rendon, B.E.; Yaddanapudi, K.; Mitchell, R.A. Negative Regulation of AMP-Activated Protein Kinase (AMPK) Activity by Macrophage Migration Inhibitory Factor (MIF) Family Members in Non-Small Cell Lung Carcinomas. J. Biol. Chem. 2012, 287, 37917–37925. [Google Scholar] [CrossRef] [PubMed]
- Liao, C.H.; Yong, C.Y.; Lai, G.M.; Chow, J.M.; Cheng, C.F.; Fang, C.L.; Lin, P.C.; Chang, C.L.; Zheng, Y.M.; Chuang, S.E.; et al. Astragalus Polysaccharide (PG2) Suppresses Macrophage Migration Inhibitory Factor and Aggressiveness of Lung Adenocarcinoma Cells. Am. J. Chin. Med. 2020, 48, 1491–1509. [Google Scholar] [CrossRef]
- Li, R.; Chen, W.; Wang, W.; Tian, W.; Zhang, X. Extraction, Characterization of Astragalus Polysaccharides and Its Immune Modulating Activities in Rats with Gastric Cancer. Carbohydr. Polym. 2009, 78, 738–742. [Google Scholar] [CrossRef]
- Li, Q.; Bao, J.; Li, X.; Zhang, T.; Shen, X. Inhibiting Effect of Astragalus Polysaccharides on the Functions of CD4+CD25 highTreg Cells in the Tumor Microenvironment of Human Hepatocellular Carcinoma. Chin. Med. J. 2012, 125, 786–793. [Google Scholar]
- Bian, Y.; Zhang, Y.; Zhou, Y.; Li, G.H.; Feng, X.S. Progress in the Pretreatment and Analysis of Flavonoids: An Update since 2013. Sep. Purif. Rev. 2022, 51, 11–37. [Google Scholar] [CrossRef]
- Yang, S.; Sun, S.; Xu, W.; Yu, B.; Wang, G.; Wang, H. Astragalus Polysaccharide Inhibits Breast Cancer Cell Migration and Invasion by Regulating Epithelial-mesenchymal Transition via the Wnt/Β-catenin Signaling Pathway. Mol. Med. Rep. 2020, 21, 1819–1832. [Google Scholar] [CrossRef]
- Tian, Q.E.; De Li, H.; Yan, M.; Cai, H.L.; Tan, Q.Y.; Zhang, W.Y. Effects of Astragalus Polysaccharides on P-Glycoprotein Efflux Pump Function and Protein Expression in H22 Hepatoma Cells in Vitro. BMC Complement. Altern. Med. 2012, 12, 94. [Google Scholar] [CrossRef]
- Wang, Y.; Zhang, X.; Wang, Y.; Zhao, W.; Li, H.; Zhang, L.; Li, X.; Zhang, T.; Zhang, H.; Huang, H.; et al. Application of Immune Checkpoint Targets in the Anti-Tumor Novel Drugs and Traditional Chinese Medicine Development. Acta Pharm. Sin. B 2021, 11, 2957–2972. [Google Scholar] [CrossRef]
- Di Ciaula, A.; Stella, A.; Bonfrate, L.; Wang, D.Q.H.; Portincasa, P. Gut Microbiota between Environment and Genetic Background in Familial Mediterranean Fever (FMF). Genes 2020, 11, 1041. [Google Scholar] [CrossRef] [PubMed]
- Chang, H.L.; Kuo, Y.H.; Wu, L.H.; Chang, C.M.; Cheng, K.J.; Tyan, Y.C.; Lee, C.H. The Extracts of Astragalus membranaceus Overcome Tumor Immune Tolerance by Inhibition of Tumor Programmed Cell Death Protein Ligand-1 Expression. Int. J. Med. Sci. 2020, 17, 939–945. [Google Scholar] [CrossRef]
- Chang, F.L.; Tsai, K.C.; Lin, T.Y.; Yang, T.W.; Lo, Y.N.; Chen, W.C.; Chang, J.H.; Lu, M.K.; Chiou, C.T.; Chen, P.-H.; et al. Astragalus membranaceus-Derived Anti-Programmed Death-1 Monoclonal Antibodies with Immunomodulatory Therapeutic Effects against Tumors. BioMed Res. Int. 2020, 2020, 3415471. [Google Scholar] [CrossRef]
- Tsao, S.M.; Wu, T.C.; Chen, J.; Chang, F.; Tsao, T. Astragalus Polysaccharide Injection (PG2) Normalizes the Neutrophil-to-Lymphocyte Ratio in Patients with Advanced Lung Cancer Receiving Immunotherapy. Integr. Cancer Ther. 2021, 20, 153473542199525. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhang, Z. The History and Advances in Cancer Immunotherapy: Understanding the Characteristics of Tumor-Infiltrating Immune Cells and Their Therapeutic Implications. Cell. Mol. Immunol. 2020, 17, 807–821. [Google Scholar] [CrossRef]
- Rosenberg, S.A.; Restifo, N.P. Adoptive Cell Transfer as Personalized Immunotherapy for Human Cancer. Science 2015, 348, 62–68. [Google Scholar] [CrossRef]
- Zhang, S.; Mou, X.Y.; Wang, H.M.; Jiang, S.J. Astragalus polysaccharide-induced enhancement of CIK cell killing in dendritic cells. Chin. J. Immunol. 2009, 140–142. [Google Scholar]
- Wang, J.T.; Han, Q.Q.; Wang, B.Y.; Yan, X.J.; Li, W.; Zhang, M.H.; Zhou, H.R.; Zhu, Y.Q. Effects of astragalus polysaccharide-induced DC combined with CIK on human oesophageal cancer Eca-109 cells. J. Tra. Chin. Med. 2016, 31, 478–481. [Google Scholar] [CrossRef]
- Zhang, Y.; Jia, Y.J.; Li, X.J.; Wang, L.; Du, M.N.; Zhang, X.X. Clinical observation of injectable astragalus polysaccharide combined with CIK cells in the treatment of middle and advanced qi deficiency type non-small cell lung cancer. Chin. Herb. Med. 2018, 1647–1651. [Google Scholar]
- Xu, Y.X.; Liu, X.J.; Qu, F. Combined treatment of ovarian cancer with herbal polysaccharides and overt immunisation. Chin. J. Exp. For. 2011, 17, 231–234. [Google Scholar] [CrossRef]
- Huo, H.Q.; Shan, B.E. Study on the Killing Effect of CIK Combined with Astragalus Polysaccharide on Hela Cells In Vitro and Ex Vivo; Hebei Medical University: Shijiazhuang, China, 2016. [Google Scholar]
- Chen, H.L.; Zhang, L.S. Astragalus Polysaccharide-Induced Killing Effect of DC Combined with CIK on Leukaemic K562 Cells; Lanzhou University: Lanzhou, China, 2013. [Google Scholar]
- Gong, Y.Z.; Gu, X.L. Effect of Four Kinds of Polysaccharides on Cytokine-Induced Anti-Tumor Activity of Killer Cells and Dendritic Cells; Shandong University: Jinan, China, 2016. [Google Scholar]
- Dong, S.; Wang, P.; Zhang, L.; Zhang, X.; Li, X.; Wang, J.; Cui, X.; Lan, T.; Gao, C.; Shi, Y.; et al. The Qi Yin San Liang San Decoction Enhances Anti-CD19 CAR-T Cell Function in the Treatment of B-Cell Lymphomas. J. Ethnopharmacol. 2024, 319, 117109. [Google Scholar] [CrossRef] [PubMed]
- To Investigate the Effect and Mechanism of Astragalus Polysaccharide (APS) on CAR T Therapy for HCC Based on T Cell Subsets Differentiation—National Natural Science Foundation Abstract Inquiry—MedSci.cn. Available online: https://www.medsci.cn/sci/nsfc_show.do?id=5275104433e32 (accessed on 20 April 2024).
- Liu, J.; Fu, M.; Wang, M.; Wan, D.; Wei, Y.; Wei, X. Cancer Vaccines as Promising Immuno-Therapeutics: Platforms and Current Progress. J. Hematol. Oncol. 2022, 15, 28. [Google Scholar] [CrossRef] [PubMed]
- Qiu, B.; Jing, X.N.; Wu, J.B.; Chen, D.D.; Liu, X.Q. Antitumor effect of dendritic cell vaccine induced by Astragalus polysaccharide on S180 tumor-bearing mice. J. Nanjing Univ. Chin. Med. 2015, 31, 44–47. [Google Scholar]
- Qiu, X.N.; Qiu, B.; Zhan, W.X.; Wu, J.B. Effect of dendritic cell vaccine induced by Astragalus polysaccharide on Th1/Th2 cytokines in S180 tumor-bearing mice. Tianjin Pharm. 2014, 42, 1080–1083. [Google Scholar]
- Yang, L.; Guo, C.; Zhang, X.P.; Ming, H.X.; Chen, Y.W. Effect of astragalus saponin-alumina hydroxide adjuvant complex on anti-breast cancer activity of bFGF tumor vaccine. J. Hexi Coll. 2018, 34, 26–31. [Google Scholar]
- Zhang, X.; Qiu, H.; Li, C.; Cai, P.; Qi, F. The Positive Role of Traditional Chinese Medicine as an Adjunctive Therapy for Cancer. Biosci. Trends 2021, 15, 283–298. [Google Scholar] [CrossRef] [PubMed]
- Deng, B.; Jia, L.; Cheng, Z. Radix Astragali-Based Chinese Herbal Medicine for Oxaliplatin-Induced Peripheral Neuropathy: A Systematic Review and Meta-Analysis. Evid.-Based Complement. Altern. Med. 2016, 2016, 2421876. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Qi, F.; Cui, Y.; Zhao, L.; Sun, X.; Tang, W.; Cai, P. An Update on Chinese Herbal Medicines as Adjuvant Treatment of Anticancer Therapeutics. Biosci. Trends 2018, 12, 220–239. [Google Scholar] [CrossRef] [PubMed]
- Sellami, M.; Slimeni, O.; Pokrywka, A.; Kuvačić, G.; D Hayes, L.; Milic, M.; Padulo, J. Herbal Medicine for Sports: A Review. J. Int. Soc. Sports Nutr. 2018, 15, 14. [Google Scholar] [CrossRef] [PubMed]
- Samuel, A.O.; Huang, B.T.; Chen, Y.; Guo, F.X.; Yang, D.D.; Jin, J.Q. Antioxidant and Antibacterial Insights into the Leaves, Leaf Tea and Medicinal Roots from Astragalus membranaceus (Fisch.) Bge. Sci. Rep. 2021, 11, 19625. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Li, X.; Wang, W.; Shan, Y.; Wang, C.; Zhu, M.; La, Q.; Zhong, Y.; Xu, Y.; Nan, P.; et al. Integrated Metabolomics and Transcriptomics Study of Traditional Herb Astragalus membranaceus Bge. Var. Mongolicus (Bge.) Hsiao Reveals Global Metabolic Profile and Novel Phytochemical Ingredients. BMC Genom. 2020, 21, 697. [Google Scholar] [CrossRef] [PubMed]
- Chang Gung Memorial Hospital. Efficacy Study of Chinese Medicine on Modulating Immune Alterations in Advanced Stage, Non-Small Cell Lung Cancer Patients Receiving 1st Line Doublet Chemotherapy and 2nd Line Target Therapy; ClinicalTrials.gov: Bethesda, MD, USA, 2013.
- ICTRP Search Portal. Available online: https://trialsearch.who.int/Trial2.aspx?TrialID=ChiCTR2300068199 (accessed on 19 February 2024).
- Yan, L. Clinical study of Astragalus polysaccharide combined with Iodine-125 in treatment of advanced lung cancer. Chin. J. Endem. Dis. Control 2014, 210. [Google Scholar]
- Qin, Z.Q.; Lu, L.Q.; Yuan, G.R.; Wu, G.Q.; Xue, Y. Clinical observation of Astragalus polysaccharide for injection combined with GP regimen in the treatment of advanced non-small cell lung cancer. J. Chin. Med. 2009, 73, 664–666. [Google Scholar] [CrossRef]
- ICTRP Search Portal. Available online: https://trialsearch.who.int/Trial2.aspx?TrialID=ITMCTR2100004716 (accessed on 24 February 2024).
- ICTRP Search Portal. Available online: https://trialsearch.who.int/Trial2.aspx?TrialID=ChiCTR2000040911 (accessed on 24 February 2024).
- ICTRP Search Portal. Available online: https://trialsearch.who.int/Trial2.aspx?TrialID=ITMCTR2000003215 (accessed on 24 February 2024).
- PhytoHealth Corporation. PG2 Treatment for Reduction of Chemotherapy-Induced Toxicity and Encouraging Compliance with Chemotherapy Among Stage II/III Breast Cancer Patients Receiving Adjuvant Chemotherapy; ClinicalTrials.gov: Bethesda, MD, USA, 2023.
- ICTRP Search Portal. Available online: https://trialsearch.who.int/Trial2.aspx?TrialID=ChiCTR2300076131 (accessed on 24 February 2024).
- Zhang, D.; Zheng, J.; Ni, M.; Wu, J.; Wang, K.; Duan, X.; Zhang, X.; Zhang, B. Comparative Efficacy and Safety of Chinese Herbal Injections Combined with the FOLFOX Regimen for Treating Gastric Cancer in China: A Network Meta-Analysis. Oncotarget 2017, 8, 68873–68889. [Google Scholar] [CrossRef]
- China Clinical Trial Registry. A Randomized Controlled Clinical Study of Astragalus membranaceus to Enhance Susceptibility to Immune Checkpoint Inhibitors in Advanced Gastric Cancer by Regulating Intestinal Flora. Available online: https://www.chictr.org.cn/showproj.html?proj=189330 (accessed on 19 February 2024).
- Zhang, X. Comparison of Neoadjuvant Treatment for Pancreatic Cancer: Astragalus Combined with Gemcitabine Versus Gemcitabine Alone—A Single-Center, Randomized, Double-Blind Study; ClinicalTrials.gov: Bethesda, MD, USA, 2024.
- Kim, E.H.; Yoon, J.H.; Yoon, S.S.; Lee, J.Y.; Yoon, S.W. Efficacy of Chemotherapy Integrated with Traditional Korean Medicine in Patients with Metastatic Pancreatic Cancer: A Single-Center Retrospective Study. Integr. Cancer Ther. 2020, 19, 1534735420983457. [Google Scholar] [CrossRef]
- ICTRP Search Portal. Available online: https://trialsearch.who.int/Trial2.aspx?TrialID=ChiCTR2000037982 (accessed on 18 February 2024).
- Lin, S.; An, X.; Guo, Y.; Gu, J.; Xie, T.; Wu, Q.; Sui, X. Meta-Analysis of Astragalus-Containing Traditional Chinese Medicine Combined With Chemotherapy for Colorectal Cancer: Efficacy and Safety to Tumor Response. Front. Oncol. 2019, 9, 749. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Cheng, C.S.; Tan, H.Y.; Tam, C.W.; Wang, N.; Feng, Y. Efficacy of Herbal Medicines Intervention for Colorectal Cancer Patients With Chemotherapy-Induced Gastrointestinal Toxicity—A Systematic Review and Meta-Analysis. Front. Oncol. 2021, 11, 629132. [Google Scholar] [CrossRef]
- Chen, M.; May, B.H.; Zhou, I.W.; Xue, C.C.L.; Zhang, A.L. FOLFOX 4 Combined with Herbal Medicine for Advanced Colorectal Cancer: A Systematic Review. Phytother. Res. 2014, 28, 976–991. [Google Scholar] [CrossRef] [PubMed]
- Han, J.; Lai, H.; Li, W.; Liao, H.; Xiao, C.; Li, X.; You, F.; Guo, J. Efficacy and Safety of Traditional Plant-Based Medicines for Preventing Chronic Oxaliplatin-Induced Peripheral Neurotoxicity in Patients with Colorectal Cancer: A Systematic Review and Meta-Analysis with Core Herb Contribution. J. Ethnopharmacol. 2024, 326, 117735. [Google Scholar] [CrossRef] [PubMed]
- ICTRP Search Portal. Available online: https://trialsearch.who.int/Trial2.aspx?TrialID=NCT01720563 (accessed on 24 February 2024).
- PhytoHealth Corporation. PG2 Concurrent with Chemoradiation for Locally Advanced Esophageal Cancer; ClinicalTrials.gov: Bethesda, MD, USA, 2023.
- PhytoHealth Corporation. PG2 Treatment for Improving Fatigue Among Advanced Cancer Patients under Standard Palliative Care; ClinicalTrials.gov: Bethesda, MD, USA, 2023.
- Nagtegaal, I.D.; Odze, R.D.; Klimstra, D.; Paradis, V.; Rugge, M.; Schirmacher, P.; Washington, K.M.; Carneiro, F.; Cree, I.A.; WHO Classification of Tumours Editorial Board. The 2019 WHO Classification of Tumours of the Digestive System. Histopathology 2020, 76, 182–188. [Google Scholar] [CrossRef] [PubMed]
- Smyth, E.C.; Nilsson, M.; Grabsch, H.I.; van Grieken, N.C.; Lordick, F. Gastric Cancer. Lancet 2020, 396, 635–648. [Google Scholar] [CrossRef] [PubMed]
- Xu, W.; Li, B.; Xu, M.; Yang, T.; Hao, X. Traditional Chinese Medicine for Precancerous Lesions of Gastric Cancer: A Review. Biomed. Pharmacother. 2022, 146, 112542. [Google Scholar] [CrossRef] [PubMed]
- Liang, Z.; Xu, Y.; Zhang, Y.; Zhang, X.; Song, J.; Jin, J.; Qian, H. Anticancer Applications of Phytochemicals in Gastric Cancer: Effects and Molecular Mechanism. Front. Pharmacol. 2023, 13, 1078090. [Google Scholar] [CrossRef]
- Wang, X.; Chen, J.; Yang, F.; Ali, F.; Mao, Y.; Hu, A.; Xu, T.; Yang, Y.; Wang, F.; Zhou, G.; et al. Two Kinds of Traditional Chinese Medicine Prescriptions Reduce Thymic Inflammation Levels and Improve Humoral Immunity of Finishing Pigs. Front. Vet. Sci. 2022, 9, 929112. [Google Scholar] [CrossRef]
- Ionkova, I.; Shkondrov, A.; Zarev, Y.; Kozuharova, E.; Krasteva, I. Anticancer Secondary Metabolites: From Ethnopharmacology and Identification in Native Complexes to Biotechnological Studies in Species of Genus Astragalus L. and Gloriosa L. Curr. Issues Mol. Biol. 2022, 44, 3884–3904. [Google Scholar] [CrossRef]
- Sakurai, M.; Egashira, N.; Kawashiri, T.; Yano, T.; Ikesue, H.; Oishi, R. Oxaliplatin-Induced Neuropathy in the Rat: Involvement of Oxalate in Cold Hyperalgesia but Not Mechanical Allodynia. Pain 2009, 147, 165–174. [Google Scholar] [CrossRef] [PubMed]
- Henricks, L.M.; Lunenburg, C.A.T.C.; De Man, F.M.; Meulendijks, D.; Frederix, G.W.J.; Kienhuis, E.; Creemers, G.J.; Baars, A.; Dezentjé, V.O.; Imholz, A.L.T.; et al. DPYD Genotype-Guided Dose Individualisation of Fluoropyrimidine Therapy in Patients with Cancer: A Prospective Safety Analysis. Lancet Oncol. 2018, 19, 1459–1467. [Google Scholar] [CrossRef]
- China Clinical Trial Registry. Clinical Study on the Treatment of Low Grade Gastric Intraepithelial Neoplasia by Regulating the Gastric Environment with Eqi Shicao Tang Based on Metabolomics Exploration. Available online: https://www.chictr.org.cn/showproj.html?proj=207037 (accessed on 19 February 2024).
- Dekker, E.; Tanis, P.J.; Vleugels, J.L.A.; Kasi, P.M.; Wallace, M.B. Colorectal Cancer. Lancet 2019, 394, 1467–1480. [Google Scholar] [CrossRef] [PubMed]
- Qi, F.; Li, A.; Inagaki, Y.; Gao, J.; Li, J.; Kokudo, N.; Li, X.; Tang, W. Chinese Herbal Medicines as Adjuvant Treatment during Chemo- or Radio-Therapy for Cancer. Biosci. Trends 2010, 4, 297–307. [Google Scholar] [PubMed]
- Yang, Y.; Ting, W.; Xiao, L.; Shufei, F.; Wangxiao, T.; Xiaoying, W.; Xiumei, G.; Boli, Z. Immunoregulation of Shenqi Fuzheng Injection Combined with Chemotherapy in Cancer Patients: A Systematic Review and Meta-Analysis. Evid. Based Complement. Altern. Med. 2017, 2017, 5121538. [Google Scholar] [CrossRef] [PubMed]
- Xu, R.; Lin, L.; Li, Y.; Li, Y. ShenQi FuZheng Injection Combined with Chemotherapy in the Treatment of Colorectal Cancer: A Meta-Analysis. PLoS ONE 2017, 12, e0185254. [Google Scholar] [CrossRef]
- Jiang, H.; Zhang, H.; Hu, X.; Ma, J. A Meta-Analysis of Shenqi Fuzheng Combined with Radiation in the Treatment of Nonsmall Cell Lung Cancer. J. Cancer Res. Ther. 2015, 11, C101–C103. [Google Scholar] [CrossRef] [PubMed]
- Cheng, X.; Huo, J.; Wang, D.; Cai, X.; Sun, X.; Lu, W.; Yang, Y.; Hu, C.; Wang, X.; Cao, P. Herbal Medicine AC591 Prevents Oxaliplatin-Induced Peripheral Neuropathy in Animal Model and Cancer Patients. Front. Pharmacol. 2017, 8, 344. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Ramadori, P.; Pfister, D.; Seehawer, M.; Zender, L.; Heikenwalder, M. The Immunological and Metabolic Landscape in Primary and Metastatic Liver Cancer. Nat. Rev. Cancer 2021, 21, 541–557. [Google Scholar] [CrossRef]
- Zhang, D.; Wang, K.; Zheng, J.; Wu, J.; Duan, X.; Ni, M.; Liu, S.; Zhang, B.; Zhao, Y. Comparative Efficacy and Safety of Chinese Herbal Injections Combined with Transcatheter Hepatic Arterial Chemoembolization in Treatment of Liver Cancer: A Bayesian Network Meta-Analysis. J. Tradit. Chin. Med. 2020, 40, 167–187. [Google Scholar]
- Li, Y.; Wang, W.P. Chinese Medicine Treatment of Pancreatic Cancer Analysis and Mechanism Analysis; Liaoning University of Traditional Chinese Medicine: Shenyang, China, 2023. [Google Scholar]
- Wang, J.Y.; Ma, G.W.; Dai, S.Q.; Rong, T.H.; Wang, X.; Lin, P.; Ye, W.F.; Zhang, L.J.; Li, X.D.; Zhang, X.; et al. Effect of Cellular Immune Supportive Treatment on Immunity of Esophageal Carcinoma Patients after Modern Two-Field Lymph Node Dissection. Chin. J. Cancer. 2007, 26, 778–781. [Google Scholar]
- Gao, X.P.; Zhao, W.X.; Zhang, Z.L. Effect of Huangqi Zengmian Powder on Interstitial Response in Patients with Esophageal Cancer at Peri-Operational Period. Chin. J. Integr. Tradit. West. Med. 2001, 21, 171–173. [Google Scholar]
- Brody, H. Lung Cancer. Nature 2020, 587, S7. [Google Scholar] [CrossRef]
- He, H.; Zhou, X.; Wang, Q.; Zhao, Y. Does the Couse of Astragalus-Containing Chinese Herbal Prescriptions and Radiotherapy Benefit to Non-Small-Cell Lung Cancer Treatment: A Meta-Analysis of Randomized Trials. Evid.-Based Complement. Altern. Med. 2013, 2013, 426207. [Google Scholar] [CrossRef]
- Zhou, Y.; Hong, T.; Tong, L.; Liu, W.; Yang, X.; Luo, J.; Wang, F.; Li, J.; Yan, L. Astragalus Polysaccharide Combined with 10-Hydroxycamptothecin Inhibits Metastasis in Non-Small Cell Lung Carcinoma Cell Lines via the MAP4K3/mTOR Signaling Pathway. Int. J. Mol. Med. 2018, 42, 3093–3104. [Google Scholar] [CrossRef]
- Gan, Q.; Wang, J.; Hu, J.; Lou, G.; Xiong, H.; Peng, C.; Huang, Q. Modulation of Apoptosis by Plant Polysaccharides for Exerting Anti-Cancer Effects: A Review. Front. Pharmacol. 2020, 11, 792. [Google Scholar] [CrossRef]
- Cheon, C.; Yoo, J.E.; Yoo, H.S.; Cho, C.K.; Kang, S.; Kim, M.; Jang, B.H.; Shin, Y.C.; Ko, S.G. Efficacy and Safety of Sipjeondaebo-Tang for Anorexia in Patients with Cancer: A Pilot, Randomized, Double-Blind, Placebo-Controlled Trial. Evid.-Based Complement. Altern. Med. 2017, 2017, 8780325. [Google Scholar] [CrossRef]
- Ishiura, Y.; Shiba, Y.; Terasaki, Y.; Hayase, H.; Hamada, M.; Izawa, K.; Sugimoto, A.; Hirokami, K.; Segawa, M.; Kasahara, K.; et al. Effect of Japanese Traditional Medicine, TJ-48, on the Quality of Life of Patients with Non-Small Cell Lung Cancer Receiving Outpatient Chemotherapy. Gan Kagaku Ryoho 2016, 43, 331–334. [Google Scholar]
- Ikemoto, T.; Shimada, M.; Iwahashi, S.; Saito, Y.; Kanamoto, M.; Mori, H.; Morine, Y.; Imura, S.; Utsunomiya, T. Changes of Immunological Parameters with Administration of Japanese Kampo Medicine (Juzen-Taihoto/TJ-48) in Patients with Advanced Pancreatic Cancer. Int. J. Clin. Oncol. 2014, 19, 81–86. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Z.; Liang, R.; Wang, C.Q.; Xu, S.; Li, N.; He, Y.; Tang, F.; Chen, L.; Ma, H. Can Aidi Injection Alleviate the Toxicity and Improve the Clinical Efficacy of Radiotherapy in Lung Cancer?: A Meta-Analysis of 16 Randomized Controlled Trials Following the PRISMA Guidelines. Medicine 2016, 95, e4517. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Li, G.; Yu, L.; Mo, T.; Wu, Q.; Zhou, Z. Aidi Injection plus Platinum-Based Chemotherapy for Stage IIIB/IV Non-Small Cell Lung Cancer: A Meta-Analysis of 42 RCTs Following the PRISMA Guidelines. J. Ethnopharmacol. 2018, 221, 137–150. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.P.; Chan, A.T.C.; Le, Q.T.; Blanchard, P.; Sun, Y.; Ma, J. Nasopharyngeal Carcinoma. Lancet 2019, 394, 64–80. [Google Scholar] [CrossRef] [PubMed]
- Miao, J.; Wang, L.; Tan, S.H.; Li, J.G.; Yi, J.; Ong, E.H.W.; Tan, L.L.Y.; Zhang, Y.; Gong, X.; Chen, Q.; et al. Adjuvant Capecitabine Following Concurrent Chemoradiotherapy in Locoregionally Advanced Nasopharyngeal Carcinoma: A Randomized Clinical Trial. JAMA Oncol. 2022, 8, 1776–1785. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.; Cao, S.M.; Chang, E.T.; Liu, Z.; Cai, Y.; Zhang, Z.; Chen, G.; Huang, Q.H.; Xie, S.H.; Zhang, Y.; et al. Chinese Nonmedicinal Herbal Diet and Risk of Nasopharyngeal Carcinoma: A Population-Based Case-Control Study. Cancer 2019, 125, 4462–4470. [Google Scholar] [CrossRef] [PubMed]
- Harbeck, N.; Gnant, M. Breast Cancer. Lancet 2017, 389, 1134–1150. [Google Scholar] [CrossRef]
- Li, W.; Hu, X.; Li, Y.; Song, K. Cytotoxicity and Growth-Inhibiting Activity of Astragalus Polysaccharides against Breast Cancer via the Regulation of EGFR and ANXA1. J. Nat. Med. 2021, 75, 854–870. [Google Scholar] [CrossRef]
- Wang, B.; Guo, C.; Liu, Y.; Han, G.; Li, Y.; Zhang, Y.; Xu, H.; Chen, D. Novel Nano-Pomegranates Based on Astragalus Polysaccharides for Targeting ERα-Positive Breast Cancer and Multidrug Resistance. Drug Deliv. 2020, 27, 607–621. [Google Scholar] [CrossRef]
- Ghi, M.G.; Paccagnella, A.; Ferrari, D.; Foa, P.; Alterio, D.; Codecà, C.; Nolè, F.; Verri, E.; Orecchia, R.; Morelli, F.; et al. Induction TPF Followed by Concomitant Treatment versus Concomitant Treatment Alone in Locally Advanced Head and Neck Cancer. A Phase II-III Trial. Ann. Oncol. 2017, 28, 2206–2212. [Google Scholar] [CrossRef]
- Hsieh, C.H.; Lin, C.Y.; Hsu, C.L.; Fan, K.H.; Huang, S.F.; Liao, C.T.; Lee, L.Y.; Ng, S.K.; Yen, T.C.; Chang, J.T.C.; et al. Incorporation of Astragalus Polysaccharides Injection during Concurrent Chemoradiotherapy in Advanced Pharyngeal or Laryngeal Squamous Cell Carcinoma: Preliminary Experience of a Phase II Double-Blind, Randomized Trial. J. Cancer Res. Clin. Oncol. 2020, 146, 33–41. [Google Scholar] [CrossRef]
- Yan, P.H.; Yan, M.; Wang, X.M.; Wang, S.H. Effect of Huangqi Injection on Short-Term Prognosis in Children with Acute Lymphoblastic Leukemia. Chin. J. Contemp. Pediatr. 2014, 16, 141–146. [Google Scholar]
- Zhang, X.J.; Yan, M.; Liu, Y.; Wang, X.M.; Nuriding, H. Effects of Huangqi Injection on Infection Factors in Children with Acute Lymphoblastic Leukemia. Chin. J. Contemp. Pediatr. 2014, 16, 147–151. [Google Scholar]
- Li, L.J.; Li, M.Y.; Li, Y.T.; Feng, J.J.; Hao, F.Q.; Zhang, L. Adjuvant Activity of Sargassum Pallidum Polysaccharides against Combined Newcastle Disease, Infectious Bronchitis and Avian Influenza Inactivated Vaccines. Mar. Drugs 2012, 10, 2648–2660. [Google Scholar] [CrossRef] [PubMed]
- Cho, C.W.; Han, C.; Rhee, Y.K.; Lee, Y.C.; Shin, K.S.; Shin, J.S.; Lee, K.T.; Hong, H.D. Cheonggukjang Polysaccharides Enhance Immune Activities and Prevent Cyclophosphamide-Induced Immunosuppression. Int. J. Biol. Macromol. 2015, 72, 519–525. [Google Scholar] [CrossRef]
- Li, N.; Li, L.; Fang, J.C.; Wong, J.H.; Ng, T.B.; Jiang, Y.; Wang, C.R.; Zhang, N.Y.; Wen, T.Y.; Qu, L.Y.; et al. Isolation and Identification of a Novel Polysaccharide-Peptide Complex with Antioxidant, Anti-Proliferative and Hypoglycaemic Activities from the Abalone Mushroom. Biosci. Rep. 2012, 32, 221–228. [Google Scholar] [CrossRef] [PubMed]
- Xie, J.H.; Xie, M.Y.; Nie, S.P.; Shen, M.Y.; Wang, Y.X.; Li, C. Isolation, Chemical Composition and Antioxidant Activities of a Water-Soluble Polysaccharide from Cyclocarya paliurus (Batal.) Iljinskaja. Food Chem. 2010, 119, 1626–1632. [Google Scholar] [CrossRef]
- Cai, D.; He, F.; Wu, S.; Wang, Z.; Bian, Y.; Wen, C.; Ding, K. Functional Structural Domain Synthesis of Anti-Pancreatic Carcinoma Pectin-like Polysaccharide RN1. Carbohydr. Polym. 2024, 327, 121668. [Google Scholar] [CrossRef] [PubMed]
- Di, T.; Chen, G.; Sun, Y.; Ou, S.; Zeng, X.; Ye, H. Antioxidant and Immunostimulating Activities in Vitro of Sulfated Polysaccharides Isolated from Gracilaria Rubra. J. Funct. Foods 2017, 28, 64–75. [Google Scholar] [CrossRef]
- Liu, Y.; Zhao, J.; Zhao, Y.; Zong, S.; Tian, Y.; Chen, S.; Li, M.; Liu, H.; Zhang, Q.; Jing, X.; et al. Therapeutic Effects of Lentinan on Inflammatory Bowel Disease and Colitis-Associated Cancer. J. Cell. Mol. Med. 2019, 23, 750–760. [Google Scholar] [CrossRef]
- Wang, H.; Liu, Y.; Qi, Z.; Wang, S.; Liu, S.; Li, X.; Wang, H.; Xia, X. An Overview on Natural Polysaccharides with Antioxidant Properties. Curr. Med. Chem. 2013, 20, 2899–2913. [Google Scholar] [CrossRef]
- Chen, N.; Johnson, M.M.; Collier, M.A.; Gallovic, M.D.; Bachelder, E.M.; Ainslie, K.M. Tunable Degradation of Acetalated Dextran Microparticles Enables Controlled Vaccine Adjuvant and Antigen Delivery to Modulate Adaptive Immune Responses. J. Control. Release 2018, 273, 147–159. [Google Scholar] [CrossRef]
- Seweryn, E.; Ziała, A.; Gamian, A. Health-Promoting of Polysaccharides Extracted from Ganoderma lucidum. Nutrients 2021, 13, 2725. [Google Scholar] [CrossRef] [PubMed]
- Łysakowska, P.; Sobota, A.; Wirkijowska, A. Medicinal Mushrooms: Their Bioactive Components, Nutritional Value and Application in Functional Food Production—A Review. Molecules 2023, 28, 5393. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Wang, J.; Wu, Z.; Yang, J.; Li, W.; Shen, L. Extraction, Purification and Anti-Proliferative Activities of Polysaccharides from Lentinus Edodes. Int. J. Biol. Macromol. 2016, 93, 136–144. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.L.; Yang, X.; Wan, J.M.F. The Culture Duration Affects the Immunomodulatory and Anticancer Effect of Polysaccharopeptide Derived from Coriolus Versicolor. Enzym. Microb. Technol. 2006, 38, 14–21. [Google Scholar] [CrossRef]
- Dou, H.; Chang, Y.; Zhang, L. Chapter Fifteen—Coriolus Versicolor Polysaccharopeptide as an Immunotherapeutic in China. In Progress in Molecular Biology and Translational Science; Zhang, L., Ed.; Academic Press: Cambridge, MA, USA, 2019; Volume 163, pp. 361–381. ISBN 1877-1173. [Google Scholar]
- Wang, Y.Y.; Khoo, K.H.; Chen, S.T.; Lin, C.C.; Wong, C.H.; Lin, C.H. Studies on the Immuno-Modulating and Antitumor Activities of Ganoderma lucidum (Reishi) Polysaccharides: Functional and Proteomic Analyses of a Fucose-Containing Glycoprotein Fraction Responsible for the Activities. Bioorg. Med. Chem. 2002, 10, 1057–1062. [Google Scholar] [CrossRef] [PubMed]
- Zhao, L.; Dong, Y.; Chen, G.; Hu, Q. Extraction, Purification, Characterization and Antitumor Activity of Polysaccharides from Ganoderma lucidum. Carbohydr. Polym. 2010, 80, 783–789. [Google Scholar] [CrossRef]
- Zhou, Z.Q.; Xiao, J.; Fan, H.X.; Yu, Y.; He, R.R.; Feng, X.L.; Kurihara, H.; So, K.F.; Yao, X.S.; Gao, H. Polyphenols from Wolfberry and Their Bioactivities. Food Chem. 2017, 214, 644–654. [Google Scholar] [CrossRef] [PubMed]
- Xie, J.H.; Tang, W.; Jin, M.L.; Li, J.E.; Xie, M.Y. Recent Advances in Bioactive Polysaccharides from Lycium barbarum L., Zizyphus jujuba Mill, Plantago spp., and Morus spp.: Structures and Functionalities. Food Hydrocoll. 2016, 60, 148–160. [Google Scholar] [CrossRef]
- Ke, M.; Zhang, X.J.; Han, Z.H.; Yu, H.Y.; Lin, Y.; Zhang, W.G.; Sun, F.H.; Wang, T.J. Extraction, Purification of Lycium barbarum Polysaccharides and Bioactivity of Purified Fraction. Carbohydr. Polym. 2011, 86, 136–141. [Google Scholar] [CrossRef]
- Zhu, Z.; Liu, R.; Si, C.; Zhou, F.; Wang, Y.; Ding, L.; Jing, C.; Liu, A.; Zhang, Y. Structural Analysis and Anti-Tumor Activity Comparison of Polysaccharides from Astragalus. Carbohydr. Polym. 2011, 85, 895–902. [Google Scholar] [CrossRef]
- Morris, V.J.; Belshaw, N.J.; Waldron, K.W.; Maxwell, E.G. The Bioactivity of Modified Pectin Fragments. Bioact. Carbohydr. Diet. Fibre 2013, 1, 21–37. [Google Scholar] [CrossRef]
- Brouns, F.; Theuwissen, E.; Adam, A.; Bell, M.; Berger, A.; Mensink, R.P. Cholesterol-Lowering Properties of Different Pectin Types in Mildly Hyper-Cholesterolemic Men and Women. Eur. J. Clin. Nutr. 2012, 66, 591–599. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Liu, J.; Duan, H.; Li, R.; Peng, W.; Wu, C. Activation of Nrf2/HO-1 Signaling: An Important Molecular Mechanism of Herbal Medicine in the Treatment of Atherosclerosis via the Protection of Vascular Endothelial Cells from Oxidative Stress. J. Adv. Res. 2021, 34, 43–63. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.; Tao, Y.; Lai, C.; Huang, C.; Ling, Z.; Yong, Q. Influence of Glycosyl Composition on the Immunological Activity of Pectin and Pectin-Derived Oligosaccharide. Int. J. Biol. Macromol. 2022, 222, 671–679. [Google Scholar] [CrossRef] [PubMed]
- Emran, T.B.; Islam, F.; Mitra, S.; Paul, S.; Nath, N.; Khan, Z.; Das, R.; Chandran, D.; Sharma, R.; Lima, C.M.G.; et al. Pectin: A Bioactive Food Polysaccharide with Cancer Preventive Potential. Molecules 2022, 27, 7405. [Google Scholar] [CrossRef] [PubMed]
- Mukhtar, E.; Adhami, V.M.; Khan, N.; Mukhtar, H. Apoptosis and Autophagy Induction as Mechanism of Cancer Prevention by Naturally Occurring Dietary Agents. Curr. Drug Targets 2012, 13, 1831–1841. [Google Scholar] [CrossRef] [PubMed]
- Rahman, J.; Tareq, A.M.; Hossain, M.M.; Sakib, S.A.; Islam, M.N.; Ali, M.H.; Uddin, A.B.M.N.; Hoque, M.; Nasrin, M.S.; Emran, T.B.; et al. Biological Evaluation, DFT Calculations and Molecular Docking Studies on the Antidepressant and Cytotoxicity Activities of Cycas Pectinata Buch.-Ham. Compounds. Pharmaceuticals 2020, 13, 232. [Google Scholar] [CrossRef]
- Jiang, J.; Eliaz, I.; Sliva, D. Synergistic and Additive Effects of Modified Citrus Pectin with Two Polybotanical Compounds, in the Suppression of Invasive Behavior of Human Breast and Prostate Cancer Cells. Integr. Cancer Ther. 2013, 12, 145–152. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S.; Rakib, A.; Islam, M.A.; Khanam, B.H.; Faiz, F.B.; Paul, A.; Chy, M.N.U.; Bhuiya, N.M.M.A.; Uddin, M.M.N.; Ullah, S.M.A.; et al. In Vivo and in Vitro Pharmacological Activities of Tacca integrifolia Rhizome and Investigation of Possible Lead Compounds against Breast Cancer through in Silico Approaches. Clin. Phytosci. 2019, 5, 36. [Google Scholar] [CrossRef]
- Nsengiyumva, E.M.; Alexandridis, P. Xanthan Gum in Aqueous Solutions: Fundamentals and Applications. Int. J. Biol. Macromol. 2022, 216, 583–604. [Google Scholar] [CrossRef]
- Cortes, H.; Caballero-Florán, I.H.; Mendoza-Muñoz, N.; Escutia-Guadarrama, L.; Figueroa-González, G.; Reyes-Hernández, O.D.; González-Del Carmen, M.; Varela-Cardoso, M.; González-Torres, M.; Florán, B.; et al. Xanthan Gum in Drug Release. Cell. Mol. Biol. 2020, 66, 199–207. [Google Scholar] [CrossRef]
- Pei, Z.; Lou, Z.; Zhang, B.; Wang, H.; Li, Y. Development of a Compound Oral Liquid Containing Herbal Extracts and Its Effect on Immunity and Gastric Mucosa. J. Food Sci. 2021, 86, 2684–2699. [Google Scholar] [CrossRef]
- Takeuchi, A.; Kamiryou, Y.; Yamada, H.; Eto, M.; Shibata, K.; Haruna, K.; Naito, S.; Yoshikai, Y. Oral Administration of Xanthan Gum Enhances Antitumor Activity through Toll-like Receptor 4. Int. Immunopharmacol. 2009, 9, 1562–1567. [Google Scholar] [CrossRef] [PubMed]
- Shao, P.; Pei, Y.; Fang, Z.; Sun, P. Effects of Partial Desulfation on Antioxidant and Inhibition of DLD Cancer Cell of Ulva Fasciata Polysaccharide. Int. J. Biol. Macromol. 2014, 65, 307–313. [Google Scholar] [CrossRef]
- Shao, P.; Chen, X.; Sun, P. Chemical Characterization, Antioxidant and Antitumor Activity of Sulfated Polysaccharide from Sargassum Horneri. Carbohydr. Polym. 2014, 105, 260–269. [Google Scholar] [CrossRef]
- Li, A.N.; Li, S.; Zhang, Y.J.; Xu, X.R.; Chen, Y.M.; Li, H.B. Resources and Biological Activities of Natural Polyphenols. Nutrients 2014, 6, 6020–6047. [Google Scholar] [CrossRef] [PubMed]
- Zvyagintseva, T.N.; Usoltseva, R.V.; Shevchenko, N.M.; Surits, V.V.; Imbs, T.I.; Malyarenko, O.S.; Besednova, N.N.; Ivanushko, L.A.; Ermakova, S.P. Structural Diversity of Fucoidans and Their Radioprotective Effect. Carbohydr. Polym. 2021, 273, 118551. [Google Scholar] [CrossRef] [PubMed]
- Saliba, J.; Manseur, C.; Groult, H.; Akil, H.; Tannoury, M.; Troutaud, D.; Maugard, T.; Feuillard, J.; Arnaudin, I.; Jayat-Vignoles, C. Anti-Proliferative and Pro-Apoptotic vLMW Fucoidan Formulas Decrease PD-L1 Surface Expression in EBV Latency III and DLBCL Tumoral B-Cells by Decreasing Actin Network. Mar. Drugs 2023, 21, 132. [Google Scholar] [CrossRef]
- El-Sheekh, M.M.; Ward, F.; Deyab, M.A.; Al-Zahrani, M.; Touliabah, H.E. Chemical Composition, Antioxidant, and Antitumor Activity of Fucoidan from the Brown Alga Dictyota Dichotoma. Molecules 2023, 28, 7175. [Google Scholar] [CrossRef]
- Yang, J.; Yang, X.; Pan, W.; Wang, M.; Lu, Y.; Zhang, J.; Fang, Z.; Zhang, X.; Ji, Y.; Bei, J.-X.; et al. Fucoidan-Supplemented Diet Potentiates Immune Checkpoint Blockage by Enhancing Antitumor Immunity. Front. Cell Dev. Biol. 2021, 9, 733246. [Google Scholar] [CrossRef]
- Kiselevskiy, M.V.; Anisimova, N.Y.; Ustyuzhanina, N.E.; Vinnitskiy, D.Z.; Tokatly, A.I.; Reshetnikova, V.V.; Chikileva, I.O.; Shubina, I.Z.; Kirgizov, K.I.; Nifantiev, N.E. Perspectives for the Use of Fucoidans in Clinical Oncology. Int. J. Mol. Sci. 2022, 23, 11821. [Google Scholar] [CrossRef]
- Zhang, W.; Hwang, J.; Yadav, D.; An, E.K.; Kwak, M.; Lee, P.C.; Jin, J.O. Enhancement of Immune Checkpoint Inhibitor-Mediated Anti-Cancer Immunity by Intranasal Treatment of Ecklonia Cava Fucoidan against Metastatic Lung Cancer. Int. J. Mol. Sci. 2021, 22, 9125. [Google Scholar] [CrossRef]
- Park, H.B.; Hwang, J.; Lim, S.-M.; Zhang, W.; Jin, J.O. Dendritic Cell-Mediated Cancer Immunotherapy with Ecklonia Cava Fucoidan. Int. J. Biol. Macromol. 2020, 159, 941–947. [Google Scholar] [CrossRef]
- Tocaciu, S.; Oliver, L.J.; Lowenthal, R.M.; Peterson, G.M.; Patel, R.; Shastri, M.; McGuinness, G.; Olesen, I.; Fitton, J.H. The Effect of Undaria Pinnatifida Fucoidan on the Pharmacokinetics of Letrozole and Tamoxifen in Patients with Breast Cancer. Integr. Cancer Ther. 2018, 17, 99–105. [Google Scholar] [CrossRef]
- Figueroa, F.A.; Abdala-Díaz, R.T.; Pérez, C.; Casas-Arrojo, V.; Nesic, A.; Tapia, C.; Durán, C.; Valdes, O.; Parra, C.; Bravo-Arrepol, G.; et al. Sulfated Polysaccharide Extracted from the Green Algae Codium Bernabei: Physicochemical Characterization and Antioxidant, Anticoagulant and Antitumor Activity. Mar. Drugs 2022, 20, 458. [Google Scholar] [CrossRef]
- Xie, J.H.; Jin, M.L.; Morris, G.A.; Zha, X.Q.; Chen, H.Q.; Yi, Y.; Li, J.E.; Wang, Z.J.; Gao, J.; Nie, S.P.; et al. Advances on Bioactive Polysaccharides from Medicinal Plants. Crit. Rev. Food Sci. Nutr. 2016, 56 (Suppl. S1), S60–S84. [Google Scholar] [CrossRef]
- Chen, G.; Jiang, N.; Zheng, J.; Hu, H.; Yang, H.; Lin, A.; Hu, B.; Liu, H. Structural Characterization and Anti-Inflammatory Activity of Polysaccharides from Astragalus membranaceus. Int. J. Biol. Macromol. 2023, 241, 124386. [Google Scholar] [CrossRef]
- Tang, Z.; Huang, G. Extraction, Structure, and Activity of Polysaccharide from Radix Astragali. Biomed. Pharmacother. Biomed. Pharmacother. 2022, 150, 113015. [Google Scholar] [CrossRef]
- Berezutsky, M.A.; Matvienko, U.A.; Karetnikova, A.Y.; Durnova, N.A. Anti-Cancer Activity of Astragalus membranaceus—A Review. Int. J. Pharm. Res. 2021, 13, 09752366. [Google Scholar] [CrossRef]
- Yu, Z.; Guo, F.; Guo, Y.; Zhang, Z.; Wu, F.; Luo, X. Optimization and Evaluation of Astragalus Polysaccharide Injectable Thermoresponsive In-Situ Gels. PLoS ONE 2017, 12, e0173949. [Google Scholar] [CrossRef]

| Model Source | Dosage | Effect of APS on Immune Cells | Reference |
|---|---|---|---|
| C57BL/6 mice | 200 μg/mL, 24 h | bone marrow-derived dendritic cells(BMDCs) ↑ Splenic DCs in mice 6 h ↑18 h ↓ Human peripheral blood DCs (PBDCs) 6 h ↑ | [26] |
| C57BL/6J mice | 45 μg/mL, 24 h | BMDC ↑ | [27] |
| BALB/c mice | 200 μg/mL, 24 h | CD8+ T ↑ CD4+ T ↑ pDC ↑ | [28] |
| BALB/c mice | 50 μg/mL, 24 h | BMDC ↑ (CD4+ T/Treg cell)/(CD8+ T/Treg cell) ↑ CD4+ T ↑ | [29] |
| C57BL/6 mice | 16 mg/mL, 48 h | M1/M2 ↑ CD11c(high) CD45RB(low) DCs ↑ Th1/Th2 ↑ | [30] |
| C57BL/6 mice | 50 mg/kg, 18 h | CD11c+ DC ↑ CD3-NK1.1+ ↑ CD8+ T ↑ | [31] |
| Kunming mice C57 mice | 100 mL/kg, 3 days | CD4+ T/CD8+ T ↑ | [32] |
| C57BL/6J mice | 0.2 mg/mL | Treg ↓ BMDC ↑ CD3+CD8+ T ↑ MHC-I+CD11c+ cells ↑ | [33] |
| Swiss-Hauschka (ICR) mice | 5 mg/mL, 14 days | Th1/Th2 ↑ CD4+ T/CD8+ T ↑ | [34] |
| Spleen lymphocyte | 0.156 mg/mL | Th1/Th2 ↑ CD4+ T/CD8+ T ↑ | [35] |
| BALB/c mice | 300 μg/mL | Macrophage (M2 → M1) ↑ | [36] |
| Mouse peritoneal macrophages | 100 ng/mL, 24 h | Raw 264.7 ↑ | [37] |
| Murine macrophage RAW 264.7 cells | 2000 μg/mL, 24 h | Raw 264.7 ↑ (IL-1α, IL-1β, IL-6 ↑, NO ↓) | [38] |
| The fresh lung tissues of adult pigs | 500 μg/mL or 1000 μg/mL, 24 h | Raw 264.7 ↑ (TNF-α, NO ↑) | [39] |
| BALB/c mice or C3H/HeJ mice | 100 μg/mL, 6 h | Raw 264.7 ↑, B ↑ (IL-1β, TNF-α ↑) | [40] |
| ICR mice | 10 g/kg | CD8+ T ↑ CD4+ T ↑ NK ↑ CTL ↑ | [41] |
| BALB/c mice | 100, 200, 300 mg/kg, 30 days | Raw 264.7 ↑ NK ↑ B ↑ T ↑ | [42] |
| BALB/c mice | 100 mg/kg | NK ↑ | [43] |
| Model Source | Dosage | Effect of APS Cell Cycle, Signal Transduction Pathways, and Apoptosis | Reference |
|---|---|---|---|
| Kunming mice | 150, 300 mg/kg, 15 days | G1 phase retention ↓ S phase retention ↑ | [56] |
| MGC-803 cell | 200, 400, 800 μg/mL, 24 h | G0/G1 phase retention ↓ S phase retention ↑ G2/M phase retention ↓ | [57] |
| HepG2 cell | 200, 400, 800 μg/mL, 72 h | S phase retention ↑ | [58] |
| 4T1 cell | 50, 100, 200, 500, 1000 μg/mL, 72 h | G2/M phase retention ↑ | [59] |
| 4T1 cell | 50 μg/mL, 24 h | G1 phase retention ↓ G2/M phase retention ↑ | [60] |
| MCF-7 cell | 500, 1000 μg/mL, 24 h | G1 phase retention ↑ | [61] |
| SCG-1 cells | 25, 50, 100 mg/L, 12 h | G0 phase retention ↑ | [62] |
| CNE-1 cell | 200 μg/mL, 24 h | G0/G1 phase retention ↑ S phase retention ↑ | [63] |
| AGS cell | 200 μg/mL, 24 h | PI3K/Akt pathway ↓ | [64] |
| B16F10 cell | 1–5 mg/mL, 24 h | PI3K/Akt pathway ↓ | [65] |
| C57BL/6 mice | 200 mg/kg, 24 h | PI3K/Akt pathway ↓ | [66] |
| RAW264.7 cell | 0–100 μg/mL, 24 h | NF-κB/MAPK pathway ↑ P65 protein ↑ G2/M phase retention ↑ | [67] |
| GC-SGC-7901 cell GCSGC-7901/ADR cell GES-1 cell | 100–400 μg/mL, 24 h | p-AMPK level ↑ | [68] |
| A549 cell NCI-H358 cell | 20, 40 mg/mL | NF-κB pathway ↓ | [69] |
| PANC-1 cell | 0, 1, 5, 10, 15, 20 mg/mL | NF-κB P65 ↓ TLR4/NF-κB pathway ↓ | [70] |
| A549 cell BMSC cell | 50 μg/mL | RAS, ERK, NF-κB p65 protein ↓ TP53, caspase-3 protein ↑ | [71] |
| HepG2 cell Diethylnitrosamine-induced HCC in rats | 60, 120, 240 mg/kg (rats) 20, 40, 80 µg/mL (HepG2 cell) | TGF-β/MAPK/Smad pathway ↑ miR-145 ↑, miR-21 ↓ pSmad3L→pSmad3C ↑ | [72] |
| HepG2 cell | 40 mg/mL | TGF-β/Smad pathway ↑ pSmad3L→pSmad3C ↑ | [73] |
| H22 cell Kunming mice | 100, 200 mg/kg, 16 days | Bax ↑ Bcl-2 ↓ | [74] |
| MDA-MB-231 cell BALB/C mice | 200, 400 mg/kg, 21 days | Bax, Caspase7, Caspase9 ↑ Bcl-2 ↓ | [75] |
| HepG2 cell | 100, 200 mg/L, 48 h | Bcl-2 ↓ Caspase3 ↑ β-catenin, c-myc, Cyclin D1 mRNA ↓ | [76] |
| SKOV3 cell | 800 µg/mL, 24 h | Bcl-2 ↓ Bax, Caspase3 ↑ | [77] |
| BALB/C mice CNE-1 cell CNE-2 cell SUNE-1 cell | 40 µg/mL, 48 h | Bcl-2 ↓ Bax, Caspase3, Caspase9 ↑ | [78] |
| OV-90 cell SKOV-3 cell | 1 mg/mL, 24 h | miR-27a ↑ Caspase3 ↑ | [79] |
| OS MG63 cell | 10 mg/mL, 24 h | miR-133a ↑ S phase retention ↑ CyclinD1 ↓ p21 ↑ Bcl-2 ↓ Bax, Caspase3, Caspase9 ↑ | [80] |
| A549 cell NCIH1299 cell | 0, 5, 10, 20 µg/mL, | miR-195-5p ↑ | [81] |
| H460 cell | 0–30 mg/mL, 24/48 h | P53, P21, P16 ↑ Notch1,Notch3 ↑ Bcl-2 ↓ Bax, Caspase8 ↑ | [82] |
| CD133+/CD44+ cell | 0, 12.5, 25, 50 mg/mL, 48 h | Fas Caspase 3, Caspase 9, Fas, Bax ↑ Class III PI3K, Beclin 1 ↑ Bcl-2, XIAP ↓ LC3-I ↓LC3-II ↑ | [83] |
| Hep3B cell BALB/c mice | 10 mg/L | CHOP ↑ Bcl-2 ↓ Bax, Bim, Caspase3 ↑ OGT ↓OGA ↑ O-GlcNAc ↓ | [84] |
| Number | Pharmaceutical Ingredient | Disease | Status | Phase |
|---|---|---|---|---|
| NCT01802021 [161] | Astragalus-based Formula | Non-small-cell lung cancer | Recruiting | II/III |
| ChiCTR2300068199 [162] | Astragalus polysaccharides, Paclitaxel; Carboplatin | Non-small-cell lung cancer | Not Recruiting | − |
| [163] | Astragalus polysaccharides, Iodide 125 | Lung cancer | Not Recruiting | II/III |
| [25] | Astragalus polysaccharides, Vinorelbine; Cisplatin | Non-small-cell lung cancer | Not Recruiting | II/III |
| [164] | Astragalus polysaccharides, Gemcitabine; Cisplatin | Non-small-cell lung cancer | Not Recruiting | II/III |
| ITMCTR2100004716 [165] | Astragalus polysaccharides, Apatinib | Extensive-stage small-cell lung cancer | Not Recruiting | − |
| ChiCTR2000040911 [166] | Astragalus polysaccharides, Carrelizumab; Apatinib | Lung cancer | Recruiting | − |
| ITMCTR2000003215 [167] | Astragalus polysaccharides, Tansychia | Hepatocellular carcinoma; Lung cancer | Recruiting | − |
| NCT03314805 [168] | Astragalus polysaccharides | Breast cancer | Not recruiting | II |
| ChiCTR2300076131 [169] | Chinese herbal decoction (contains Astragalus polysaccharides) | Low-grade gastric intraepithelial neoplasia | Recruiting | − |
| [170] | Astragalus polysaccharides, FOLFOX | Gastric cancer | Not recruiting | − |
| ChiCTR2300068896 [171] | Astragalus polysaccharides | Gastric cancer | Not recruiting | IV |
| NCT06234072 [172] | Astragalus polysaccharides, Gemcitabine | Pancreatic cancer | Not recruiting | II |
| [173] | Traditional Korean Medicine (contains Astragalus polysaccharides), CTX | Metastatic pancreatic cancer | Not recruiting | − |
| ChiCTR2000037982 [174] | Astragalus, Panax-notoginseng, Oncolytic vaccine | Colorectal cancer | Recruiting | − |
| [175,176] | Astragalus polysaccharides | Colorectal cancer | Not recruiting | − |
| [177] | FOLFOX 4, Ginseng, Astragalus polysaccharides, Atractylodes rhizome, Poria cocos, Coix seed, Sophora flavescens | Advanced colorectal cancer | Not recruiting | − |
| [178] | Astragalus polysaccharides, Oxaliplatin, Poria cocos, Atractylodes macrocephala Koidz, Pilosula | Colorectal cancer | Not recruiting | − |
| NCT01720563 [179] | APS, Cisplatin, Leucovorin, Tegafur plus uracil | Advanced pharyngeal/laryngeal squamous cell carcinoma | Not recruiting | II |
| NCT03611712 [180] | Astragalus polysaccharides | Locally advanced esophageal cancer | Not recruiting | II |
| NCT01720550 [181] | Astragalus polysaccharides | Advanced cancer | Not recruiting | IV |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
He, Z.; Liu, X.; Qin, S.; Yang, Q.; Na, J.; Xue, Z.; Zhong, L. Anticancer Mechanism of Astragalus Polysaccharide and Its Application in Cancer Immunotherapy. Pharmaceuticals 2024, 17, 636. https://doi.org/10.3390/ph17050636
He Z, Liu X, Qin S, Yang Q, Na J, Xue Z, Zhong L. Anticancer Mechanism of Astragalus Polysaccharide and Its Application in Cancer Immunotherapy. Pharmaceuticals. 2024; 17(5):636. https://doi.org/10.3390/ph17050636
Chicago/Turabian StyleHe, Ziqing, Xiyu Liu, Simin Qin, Qun Yang, Jintong Na, Zhigang Xue, and Liping Zhong. 2024. "Anticancer Mechanism of Astragalus Polysaccharide and Its Application in Cancer Immunotherapy" Pharmaceuticals 17, no. 5: 636. https://doi.org/10.3390/ph17050636
APA StyleHe, Z., Liu, X., Qin, S., Yang, Q., Na, J., Xue, Z., & Zhong, L. (2024). Anticancer Mechanism of Astragalus Polysaccharide and Its Application in Cancer Immunotherapy. Pharmaceuticals, 17(5), 636. https://doi.org/10.3390/ph17050636






