Purinergic Receptor Antagonists: A Complementary Treatment for Hypertension
Abstract
1. Introduction
2. Purinergic Receptors
3. Purinergic Receptors in the Regulation of Blood Pressure
| Nephron Segments | P2X Purinergic Receptors | P2Y Purinergic Receptors |
|---|---|---|
| Proximal tubule | P2X1, P2X4, P2X5, P2X6 | P2Y1, P2Y2, P2Y4, P2Y6 |
| Loop of Henle, thick ascending limb | P2X4, P2X5 | P2Y2, P2Y4 |
| Loop of Henle, medullary thick ascending limb | P2X1, P2X4, P2X5, P2X6 | P2Y1, P2Y2, P2Y4, P2Y6 |
| Loop of Henle, thin descending limb | P2X4, P2X6 | P2Y1, P2Y2 |
| Loop of Henle, thin ascending limb | P2X4, P2X6 | P2Y2, P2Y4 |
| Distal tubule | P2X4, P2X5, P2X6 | |
| Collecting duct | P2X1, P2X2, P2X3, P2X4, P2X5, P2X6 | P2Y1, P2Y2, P2Y4, P2Y6 |
| Afferent arteriole | P2X1, P2X7 | P2Y1, P2Y2, P2Y6 |
| Efferent arteriole | P2Y1 | |
| Glomeruli | P2X2, P2X4, P2X7 | P2Y1, P2Y2, P2Y4, P2Y6 |
| Perivascular capillaries and descending vasa recta | P2X7 | P2Y1 |
| Smooth muscle cells | P2X1, P2X2, P2X3, P2X7 | P2Y1, P2Y2, P2Y4 |
| Endothelium | P2X7, P2X4 | P2Y1, P2Y2, P2Y6 |
4. Purinergic Receptors in Hypertension
5. Beneficial Effects of Purinergic Receptor Blockade in Renal Microcirculation in Hypertension
6. Purinergic Receptors in Inflammation and Immunity
7. Perspectives
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chobufo, M.D.; Gayam, V.; Soluny, J.; Rahman, E.U.; Enoru, S.; Foryoung, J.B.; Agbor, V.N.; Dufresne, A.; Nfor, T. Prevalence and control rates of hypertension in the USA: 2017–2018. Int. J. Cardiol. Hypertens. 2020, 6, 100044. [Google Scholar] [CrossRef]
- Ostchega, Y.; Hughes, J.P.; Zhang, G.; Nwankwo, T.; Graber, J.; Nguyen, D.T. Differences in Hypertension Prevalence and Hypertension Control by Urbanization Among Adults in the United States, 2013–2018. Am. J. Hypertens. 2022, 35, 31–41. [Google Scholar] [CrossRef]
- Muselli, M.; Bocale, R.; Necozione, S.; Desideri, G. Is the response to antihypertensive drugs heterogeneous? Rationale for personalized approach. Eur. Heart J. 2024, 26 (Suppl. S1), i60–i63. [Google Scholar] [CrossRef]
- Shokoples, B.G.; Paradis, P.; Schiffrin, E.L. Immunological insights into hypertension: Unraveling triggers and potential therapeutic avenues. Hypertens. Res. 2024, 47, 2115–2125. [Google Scholar] [CrossRef]
- Camargo, L.L.; Rios, F.J.; Montesano, A.C.; Touyz, R.M. Reactive oxygen species in hypertension. Nat. Rev. Cardiol. 2024; ahead of print. [Google Scholar] [CrossRef]
- Guzic, T.J.; Nosalki, T.; Maffia, P.; Drummond, G.R. Immune and inflammatory mechanisms in hypertension. Nat. Rev. Cardiol. 2024, 21, 396–416. [Google Scholar] [CrossRef]
- Hao, X.M.; Liu, Y.; Hailati, D.; Gong, Y.; Zhang, X.D.; Yue, B.N.; Liu, J.P.; Wu, X.L.; Yang, K.Z.; Wang, J.; et al. Mechanisms of inflammation modulation by different immune cells in hypertensive nephrophaty. Front. Immunol. 2024, 13, 1333170. [Google Scholar] [CrossRef]
- Guyton, A.C. The surprising kidney-fluid mechanism for pressure control--its infinite gain. Hypertension 1990, 16, 725–730. [Google Scholar] [CrossRef]
- Guyton, A.C. Blood pressure control: Special role of the kidneys and body fluids. Science 1991, 252, 1813–1816. [Google Scholar] [CrossRef]
- Ivy, J.R.; Bailey, M.A. Pressure natriuresis and the renal control of arterial blood pressure. J. Physiol. 2014, 592, 3955–3967. [Google Scholar] [CrossRef]
- Johnson, R.J.; Herrera-Acosta, J.; Schreiner, G.F.; Rodríguez-Iturbe, B. Subtle acquires renal injury as a mechanism of salt-sensitive hypertension. N. Engl. J. Med. 2002, 346, 913–923. [Google Scholar] [CrossRef]
- Brenner, B.M.; Lawler, E.V.; Mackenzie, H.S. The hyperfiltration theory: A paradigm shifts in nephrology. Kidney Int. 1996, 49, 1774. [Google Scholar] [CrossRef]
- Neuringer, J.R.; Brenner, B.M. Hemodynamic theory of progressive renal disease: A 10-year update in brief review. Am. J. Kidney Dis. 1993, 22, 98–104. [Google Scholar] [CrossRef]
- Tolins, J.P.; Shultz, P.; Raij, L. Mechanisms of hypertensive glomerular injury. Am. J. Cardiol. 1988, 62, 54G–58G. [Google Scholar] [CrossRef]
- Sealey, J.E.; Blumenfield, J.D.; Bell, G.M.; Pecker, M.S.; Sommers, S.C.; Laragh, J.H. On the renal basis for essential hypertension: Nephron heterogeneity with discordant renin secretion and sodium excretion causing hypertensive vasoconstriction-volume relationship. J. Hypertens. 1988, 6, 763–777. [Google Scholar] [CrossRef]
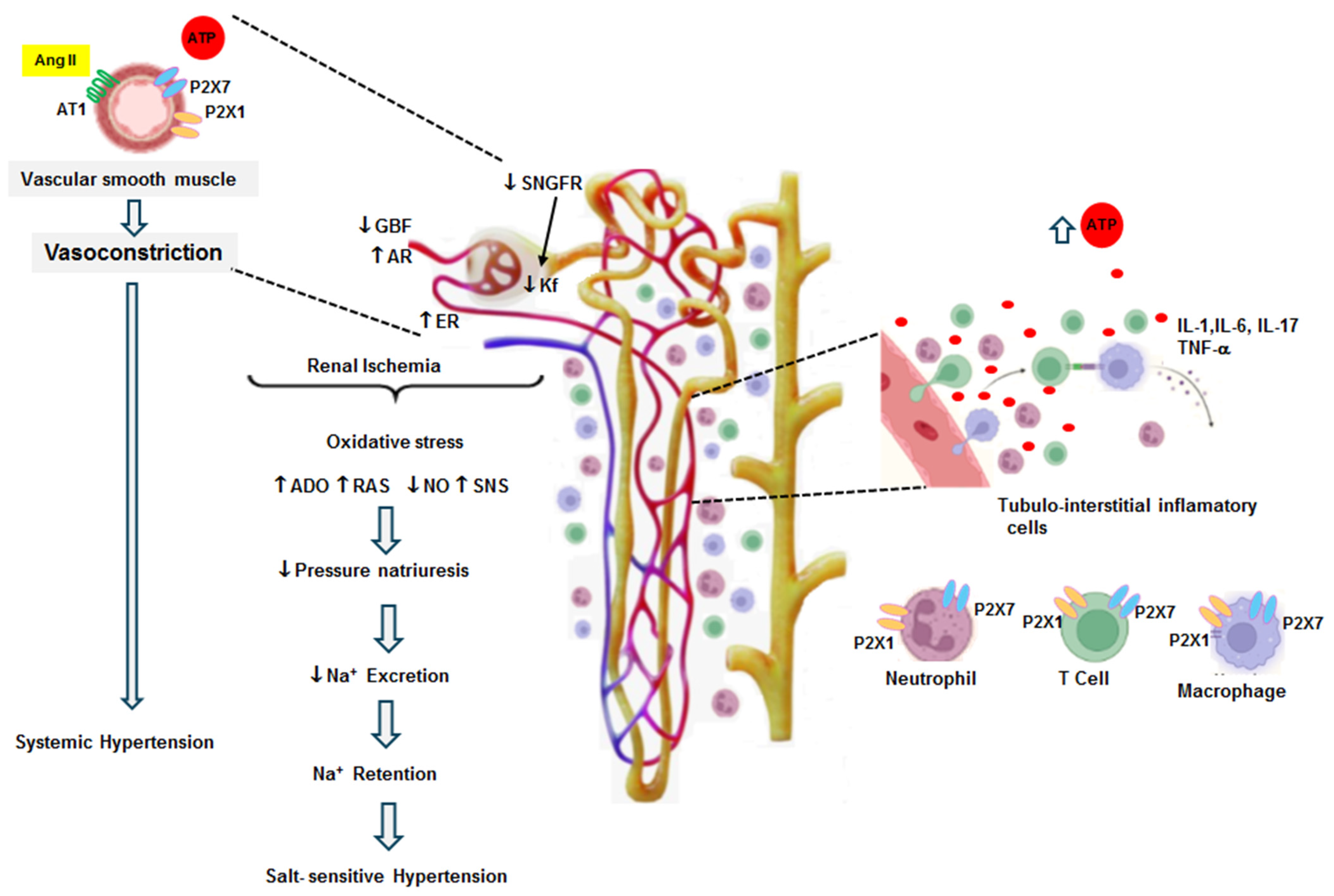
- Franco, M.; Martínez, F.; Rodríguez-Iturbe, B.; Johnson, R.J.; Santamaría, J.; Montoya, A.; Nepomuceno, T.; Bautista, R.; Tapia, E.; Herrera-Acosta, J. Angiotensin II, interstitial inflammation, and the pathogenesis of salt-sensitive hypertension. Am. J. Physiol. Renal Physiol. 2006, 291, F1281–F1287. [Google Scholar] [CrossRef]
- Franco, M.; Tapia, E.; Bautista, R.; Pacheco, U.; Santamaria, J.; Quiroz, Y.; Johnson, R.J.; Rodriguez-Iturbe, B. Impaired pressure natriuresis resulting in salt-sensitive hypertension is caused by tubulointerstitial immune cell infiltration in the kidney. Am. J. Physiol. Renal Physiol. 2013, 304, F982–F990. [Google Scholar] [CrossRef]
- Burnstock, G. Purinergic signalling: Its unpopular beginning, its acceptance and its exciting future. Bioessays 2012, 34, 218–225. [Google Scholar] [CrossRef]
- Ralevic, V.; Burnstock, G. Receptors for purines and pyrimidines. Pharmacol. Rev. 1998, 50, 413–492. [Google Scholar]
- Schrader, J. Ectonucleotidases as bridge between the ATP and adenosine world: Reflections on Geoffrey Burnstock. Purinergic Signal. 2022, 18, 193–198. [Google Scholar] [CrossRef]
- Van Beusecum, J.; Inscho, E.W. Regulation of renal function and blood pressure control by P2 purinoceptors in the kidney. Curr. Opin. Pharmacol. 2015, 21, 82–88. [Google Scholar] [CrossRef]
- Burnstock, G. Purinergical signaling in the cardiovascular system. Circ. Res. 2017, 120, 207–228. [Google Scholar] [CrossRef]
- Li, X.; Zhu, L.-J.; Lv, J.; Cao, X. Purinoceptor: A novel target for hypertension. Purinergic Signal. 2023, 19, 185–197. [Google Scholar] [CrossRef]
- Soares, A.G.; Contreras, J.; Mironova, E.; Archer, C.R.; Stockand, J.D.; Abd El-Aziz, T.M. P2Y2 receptor decreases blood pressure by inhibiting ENaC. JCI Insight 2023, 24, e167704. [Google Scholar] [CrossRef]
- Toney, G.M.; Vallon, V.; Stockand, J.D. Intrinsic control of sodium excretion in the distal nephron by inhibitory purinergic regulation of the epithelial Na+ channel. Curr. Opin. Nephrol. Hypertens. 2012, 21, 52–60. [Google Scholar] [CrossRef]
- Menzies, R.I.; Frederick, T.W.T.; Unwin, R.J.; Bailey, M.A. Purinergic signaling in kidney disease. Kidney Int. 2017, 91, 315–316. [Google Scholar] [CrossRef]
- Nishiyama, A.; Majid, D.S.; Taher, K.A.; Miyatake, A.; Navar, L.G. Relation between interstitial ATP concentrations and autoregulaion-mediated changes in vascular resistance. Cir. Res. 2000, 86, 656–662. [Google Scholar] [CrossRef]
- Palygin, O.; Evans, L.C.; Cowley, A.W., Jr.; Staruschenko, A. Acute in vivo analysis of ATP release in rat kidneys in response to changes of renal perfusion pressure. J. Am. Heart Assoc. 2017, 6, e006658. [Google Scholar] [CrossRef]
- Yamamoto, K.; Korenaga, R.; Kamiya, A.; Ando, J. Fluid shear stress activates Ca2+ influx into human endothelial cells via P2X4 purinoceptors. Circ. Res. 2000, 87, 385–391. [Google Scholar] [CrossRef]
- Vallon, V.; Unwin, R.; Inscho, E.W.; Leipziger, J.; Kishore, B.K. Extracellular nucleotides and P2 receptors in renal function. Physiol. Rev. 2020, 100, 211–269. [Google Scholar] [CrossRef]
- Ji, X.; Naito, Y.; Hirokawa, G.; Weng, H.; Hiura, Y.; Takahashi, R.; Iwai, N. 2X (7) receptor antagonism attenuates the hypertension and renal injury in Dahl salt-sensitive rats. Hypertens. Res. 2012, 35, 173–179. [Google Scholar] [CrossRef]
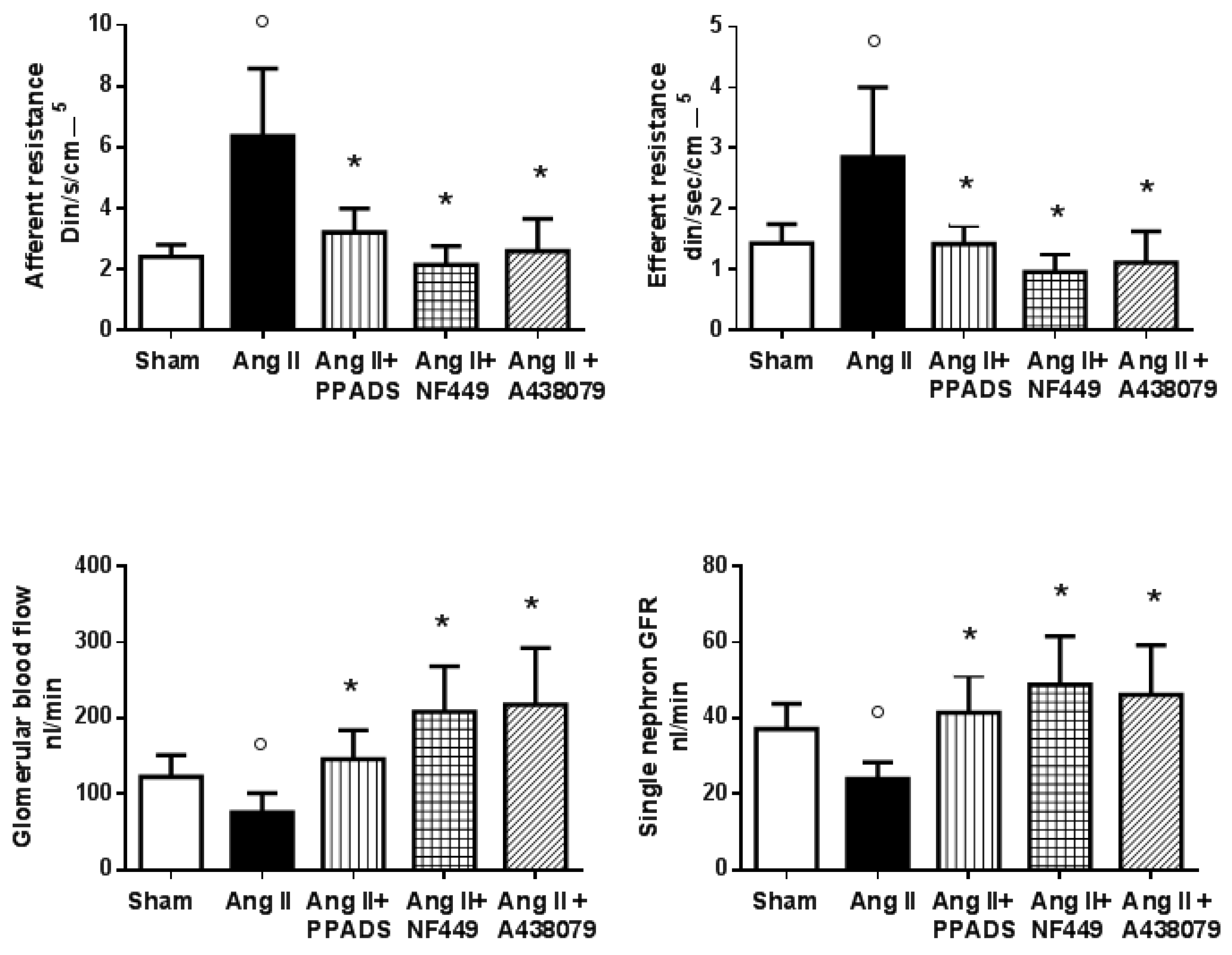
- Franco, M.; Bautista, R.; Tapia, E.; Soto, V.; Santamaría, J.; Osorio, H.; Pacheco, U.; Sánchez-Lozada, L.G.; Kobori, H.; Navar, L.G. Contribution of renal purinergic receptors to renal vasoconstriction in angiotensin II-induced hypertensive rats. Am. J. Physiol. Renal Physiol. 2011, 300, F1301–F1309. [Google Scholar] [CrossRef]
- Vonend, O.; Turner, C.M.; Chan, C.M.; Loesch, A.; DellÄnn, G.C.; Srai, K.S.; Burnstock, G.; Unwin, R.J. Glomerular exression of the ATP-sensitive P2X receptor in diabetic and hypertensive rat models. Kidney Int. 2004, 66, 157–166. [Google Scholar] [CrossRef]
- Franco, M.; Bautista-Pérez, R.; Cano-Martínez, A.; Pacheco, U.; Santamaría, J.; Del Valle-Mondragón, L.; Pérez-Méndez, O.; Navar, L.G. Physiopathological implications of P2X1 and P2X7 receptors in regulation of glomerular hemodynamics in angiotensin II-induced hypertension. Am. J. Physiol. Renal Physiol. 2017, 312, 9–19. [Google Scholar] [CrossRef] [PubMed]
- Menzies, R.I.; Unwin, R.J.; Bailey, M.A. Renal P2 receptors and hypertension. Acta Physiol. 2015, 213, 232–241. [Google Scholar] [CrossRef]
- Menzies, R.I.; Unwin, R.J.; Rash, R.; Beard, D.A.; Cowley, A.W., Jr.; Carlson, B.E.; Mullins, J.J.; Bailey, M.A. Effect of P2X4 and P2X7 receptor antagonism on the pressure diuresis relationship in rats. Front. Physiol. 2013, 4, 235. [Google Scholar] [CrossRef] [PubMed]
- Bell, P.D.; Komlosi, P.; Zhang, Z.R. ATP as a mediator of macula densa cell signalling. Purinergic Signal. 2009, 5, 461–471. [Google Scholar] [CrossRef]
- Osmond, D.A.; Inscho, E.W. P2X(1) Receptor blockade inhibits whole kidney autoregulation of renal blood flow in vivo. Am. J. Physiol. Renal Physiol. 2010, 298, F1360–F1368. [Google Scholar] [CrossRef]
- Wang, D.J.; Huang, N.N.; Heppel, L.A. Extracellular ATP and ADP stimulate proliferation of porcine aortic smooth muscle cells. J. Cell Physiol. 1992, 153, 221–233. [Google Scholar] [CrossRef] [PubMed]
- Erlinge, D.; Yoo, H.; Edvinsson, L.; Reis, D.J.; Wahlestedt, C. Mitogenic effects of ATP on vascular smooth muscle cells vs. other growth factors and sympathetic cotransmitters. Am. J. Physiol. Heart Circ. Physiol. 1993, 265, H1089–H1097. [Google Scholar] [CrossRef]
- Johnson, R.J.; Alpers, C.E.; Yoshimura, A.; Lombardi, D.; Prinzl, P.; Floege, J.; Schwartz, S.M. Renal injury from angiotensin II-mediated hypertension. Hypertension 1992, 19, 464–474. [Google Scholar] [CrossRef]
- Lombardi, D.; Gordon, K.L.; Polinsky, P.; Suga, S.; Schwartz, S.M.; Johnson, R.J. Salt-sensitive hypertension develops after short term exposure to angiotensin II. Hypertension 1999, 33, 1013–1019. [Google Scholar] [CrossRef] [PubMed]
- Franco, M.; Pérez-Méndez, O.; Kulthinee, S.; Navar, L.G. Integration of purinergic and angiotensin II receptor function in renal vascular responses and renal injury in angiotensin II-dependent hypertension. Purinergic Signal. 2019, 15, 277–285. [Google Scholar] [CrossRef] [PubMed]
- Ji, X.; Naito, Y.; Weng, H.; Endo, K.; Ma, X.; Iwai, N. P2X7 deficiency attenuates hypertension and renal injury in deoxycorticosterone acetate-salt hypertension. Am. J. Physiol. Renal Physiol. 2012, 303, F1207–F1215. [Google Scholar] [CrossRef] [PubMed]
- Menzies, R.I.; Howarth, A.R.; Unwin, R.J.; Frederick, W.K.; Mullis, J.J.; Bailey, M.A. Inhibition of the purinergic P2X7 receptor improves renal perfusion pressure in angiotensin-II-infused rats. Kidney Int. 2015, 88, 1079–1087. [Google Scholar] [CrossRef]
- Turner, C.M.; Vonend, O.; Chan, C.; Burnstock, G.; Unwin, R.J. The pattern of distribution of selected ATP-sensitive P2 receptor subtypes in normal rat kidney: An immunohistologycal study. Cells Tissues Organs 2003, 175, 105–117. [Google Scholar] [CrossRef] [PubMed]
- Graciano, M.L.; Nishiyama, A.; Jackson, K.; Seth, D.M.; Ortiz, R.M.; Prieto-Carrasquero, M.; Kobori, H.; Navar, L.G. Purinergic Receptors Contribute to Early Mesangial Transformation and Renal Vessel Hypertrophy during Angiotensin II-Induced Hypertension. Am. J. Physiol. Renal Physiol. 2008, 294, F161–F169. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.P.; Liu, S.C.; Hu, S.Q.; Lu, J.F.; Wu, C.L.; Hu, D.X.; Zhang, W.J. ATP ion channel P2X purinergic receptors in inflammation response. Biomed. Pharmacother. 2023, 158, 114205. [Google Scholar] [CrossRef] [PubMed]
- Wihlborg, A.K.; Wang, L.; Braun, O.O.; Eyjolfsson, A.; Gustafsson, R.; Gudbjartsson, T.; Erlinge, D. ADP receptor P2Y12 is expressed in vascular smooth muscle cells and stimulates contraction in human blood vessels. Arterioscler. Thromb. Vasc. Biol. 2004, 24, 1810–1815. [Google Scholar] [CrossRef] [PubMed]
- Linden, J.; Koch-Nolte, F.; Dahl, G. Purine Release, Metabolism, and signaling in the inflammatory response. Annu. Rev. Immunol. 2019, 37, 325–347. [Google Scholar] [CrossRef]
- Takenaka, T.; Inoue, T.; Kanno, Y.; Osaka, H.; Hill, C.E.; Suzuki, H. Conexin 37 and 40 transduce purinergic signals mediating renal autoregulation. Am. J. Physiol. Integr. Comp. Physiol. 2008, 294, R1–R11. [Google Scholar] [CrossRef]
- Chekeni, F.B.; Elliott, M.R.; Sandilos, J.K.; Walk, S.F.; Kinchen, J.M.; Lazarowski, E.R.; Armstrong, A.J.; Penuela, S.; Laird, D.W.; Salvesen, G.S.; et al. Pannexin 1 channels mediate ‘find-me’ signal release and membrane permeability during apoptosis. Nature 2010, 467, 863–867. [Google Scholar] [CrossRef] [PubMed]
- Franco, M.; Bautista-Pérez, R.; Pérez-Méndez, O.; González, L.; Pacheco, U.; Sánchez-Lozada, L.G.; Tapia, E.; Martínez, F. Renal interstitial adenosine is increased in angiotensin II-induced hypertensive rats. Am. J. Physiol. Renal Physiol. 2008, 294, F84–F92. [Google Scholar] [CrossRef] [PubMed]
- Feng, M.G.; Navar, L.G. Afferent arteriolar vasodilator effect of adenosine predominantly involves A2B receptor activation. Am. J. Physiol. Renal Physiol. 2010, 299, F310–F315. [Google Scholar] [CrossRef] [PubMed]
- Idzko, M.; Ferrari, D.; Eltzschig, H.K. Nucleotide signalling during inflammation. Nature 2014, 509, 310–317. [Google Scholar] [CrossRef] [PubMed]
- McDonald, B.; Pittman, K.; Menezes, G.B.; Hirota, S.A.; Slaba, I.; Waterhouse, C.C.; Beck, P.L.; Muruve, D.A.; Kubes, P. Intravascular danger signals guide neutrophils to sites of sterile inflammation. Science 2010, 330, 362–366. [Google Scholar] [CrossRef] [PubMed]
- Dosh, M.; Gerber, J.; Jebbawi, F.; Beldi, G. Mechanisms of ATP release by inflammatory cells. Int. J. Mol. Sci. 2018, 19, 1222. [Google Scholar] [CrossRef] [PubMed]
- De Miguel, C.; Guo, C.; Lund, H.; Feng, D.; Mattson, D.L. Infiltrating T lymphocytes in the kidney increase oxidative stress and participate in the development of hypertension and renal disease. Am. J. Physiol. Renal Physiol. 2011, 300, F734–F742. [Google Scholar] [CrossRef] [PubMed]
- Krishnan, S.M.; Ling, Y.H.; Huuskes, B.M.; Ferens, D.M.; Saini, N.; Chan, C.T.; Diep, H.; Kett, M.M.; Samuel, C.S.; Kemp-Harper, B.K.; et al. Pharmacological inhibition of the NLRP3 inflammasome reduces blood pressure, renal damage, and dysfunction in salt-sensitive hypertension. Cardiovasc. Res. 2019, 115, 776–787. [Google Scholar] [CrossRef] [PubMed]
- Gomvault, A.; Baron, L.; Couillin, I. ATP reléase and purinergic signalling in NLRP3 inflammasome activation. Front. Immunol. 2012, 3, 414. [Google Scholar] [CrossRef]
- Karmakar, M.; Katsnelson, M.A.; Dubyak, G.R.; Pearlman, E. Neutrophil P2X7 receptors mediate NLRP3 inflammasome-dependent IL-1beta secretion in response to ATP. Nat. Commun. 2016, 7, 10555. [Google Scholar] [CrossRef]
- Juliana, C.; Fernandes-Alnemri, T.; Kang, S.; Farias, A.; Qin, F.; Alnemri, E.S. Nontranscriptional priming and deubiquitylation regulate NLRP3 inflammasome activation. J. Biol. Chem. 2012, 287, 36617–36622. [Google Scholar] [CrossRef] [PubMed]
- Hill, L.M.; Gavala, M.L.; Lenertz, L.Y.; Bertics, P.J. Extracellular ATP may contribute to tissue repair by rapidly stimulating purinergic receptor X7-dependent vascular endothelial growth factor release from primary human monocytes. J. Immunol. 2010, 185, 3028–3034. [Google Scholar] [CrossRef] [PubMed]
- Mattson, D.L.; James, L.; Berdan, E.A.; Meister, C.J. Immune suppression attenuates hypertension and renal disease in the Dahl salt-sensitive rat. Hypertension 2006, 48, 149–156. [Google Scholar] [CrossRef] [PubMed]
- Franco, M.; Martínez, F.; Quiroz, Y.; Galicia, O.; Bautista, R.; Johnson, R.J.; Rodríguez-Iturbe, B. Renal angiotensin II concentration and interstitial infiltration of immune cells are correlated with blood pressure levels in salt-sensitive hypertension. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2007, 293, R251–R256. [Google Scholar] [CrossRef] [PubMed]
- Vaziri, N.D.; Rodríguez-Iturbe, B. Mechanisms of disease: Oxidative stress and iflammation in the pathogenesis of hypertension. Nat. Clin. Pract. Nephrol. 2006, 2, 582–593. [Google Scholar] [CrossRef] [PubMed]
- Franco, M.; Tapia, E.; Santamaría, J.; Zafra, I.; García-Torres, R.; Gordon, K.L.; Pons, H.; Rodríguez-Iturbe, B.; Johnson, J.R.; Herrera-Acosta, J. Renal Cortical Vasoconstriction Contributes to the Development of Salt Sensitive Hypertension after Angiotensin II Exposure. J. Am. Soc. Nephrol. 2001, 10, 2263–2271. [Google Scholar] [CrossRef] [PubMed]
- Crowley, S.D.; Song, Y.S.; Lin, E.E.; Griffiths, R.; Kim, H.S.; Ruiz, P. Lymphocyte responses exacerbate angiotensin II-dependent hypertension. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2010, 298, R1089–R1097. [Google Scholar] [CrossRef]
- Hoch, N.E.; Guzik, T.J.; Chen, W.; Deans, T.; Maalouf, S.A.; Gratze, P.; Weyand, C.; Harrison, D.G. Regulation of T-cell function by endogenously produced angiotensin II. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2009, 296, R208–R216. [Google Scholar] [CrossRef] [PubMed]
- Lara, L.S.; McCormack, M.; Semprum-Prieto, L.S.; Shenouda, S.; Majid, D.S.; Kobori, H.; Navar, L.G.; Prieto, M.C. AT1 receptor-mediated augmentation of angiotensinogen, oxidative stress, and inflammation in ANG II-salt hypertension. Am. J. Physiol. Renal Physiol. 2012, 302, F85–F94. [Google Scholar] [CrossRef]
- Mironova, E.; Boiko, N.; Bugaj, V.; Kucher, V.; Stockand, J.D. Regulation of Na+ excretion and arterial blood pressure by purinergic signalling intrinsic to the distal nephron: Consequences and mechanisms. Acta Physiol. 2015, 213, 213–221. [Google Scholar] [CrossRef]
- Song, J.; Lu, Y.; Lai, E.Y.; Wei, J.; Wang, L.; Chandrashekar, K.; Wang, S.; Shen, C.; Juncos, L.A.; Liu, R. Oxidative status in the macula densa modulates tubuloglomerular feedback responsiveness in angiotensin II-induced hypertension. Acta Physiol. 2015, 213, 249–258. [Google Scholar] [CrossRef] [PubMed]
- Matavelli, L.C.; Zhou, X.; Varagic, J.; Susic, D.; Frohlich, E.D. Salt loading produces severe renal hemodynamic dysfunction independent of arterial pressure in spontaneously hypertensive rats. Am. J. Physiol. Heart Circ. Physiol. 2007, 292, H814–H819. [Google Scholar] [CrossRef] [PubMed]
- Sannai, T.; Kimur, G. Renal function reserve and sodium sensitivity in essential hypertension. J. Lab. Clin. Med. 1996, 128, 89–97. [Google Scholar] [CrossRef] [PubMed]
- Leh, S.; Hultström, M.; Rosenberger, C.; Iversen, B.M. Afferent arteriolopathy and glomerular collapse but not segmental sclerosis induce tubular atrophy in old spontaneously hypertensive rats. Virchows Arch. 2011, 459, 99–108. [Google Scholar] [CrossRef] [PubMed]
- Burnstock, G. Purinergic Signalling: Therapeutic developments. Front. Pharmacol. 2017, 8, 661. [Google Scholar] [CrossRef]
- Soni, S.; Lukhey1, M.S.; Baban, S.; Thawkar, B.S.; Chintamaneni, M.; Kaur, G.; Joshi, H.; Ramniwas, S.; Tuli, H.S. A current review on P2X7 receptor antagonist patents in the treatment of neuroinflammatory disorders: A patent review on antagonists. Naunyn-Schmiedeberg’s Arch Pharmacol. 2024, 397, 4643–4656. [Google Scholar] [CrossRef]
- Huang, Z.; Xie, N.; Illes, P.; Di Virgilio, F.; Ulrich, H.; Semyanov, A.; Verkhratsky, A.; Sperlagh, B.; Yu, S.-G.; Huang, C.; et al. From purines to purinergic signalling: Molecular functions and human diseases. Signal Transduct. Target. Ther. 2021, 6, 162. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bautista-Pérez, R.; Franco, M. Purinergic Receptor Antagonists: A Complementary Treatment for Hypertension. Pharmaceuticals 2024, 17, 1060. https://doi.org/10.3390/ph17081060
Bautista-Pérez R, Franco M. Purinergic Receptor Antagonists: A Complementary Treatment for Hypertension. Pharmaceuticals. 2024; 17(8):1060. https://doi.org/10.3390/ph17081060
Chicago/Turabian StyleBautista-Pérez, Rocio, and Martha Franco. 2024. "Purinergic Receptor Antagonists: A Complementary Treatment for Hypertension" Pharmaceuticals 17, no. 8: 1060. https://doi.org/10.3390/ph17081060
APA StyleBautista-Pérez, R., & Franco, M. (2024). Purinergic Receptor Antagonists: A Complementary Treatment for Hypertension. Pharmaceuticals, 17(8), 1060. https://doi.org/10.3390/ph17081060





