Exploring the Antibiofilm Effect of Sertraline in Synergy with Cinnamomum verum Essential Oil to Counteract Candida Species
Abstract
1. Introduction
2. Results
2.1. Cinnamomum verum EO’s Chemical Composition
2.2. Antifungal Activity of Sertraline in Association with Cinnamomum verum EO against Planktonic Cells of Candida spp.
2.3. Inhibitory Effects on Candida spp. Biofilm Growth of Sertraline in Association with Cinnamomum verum EO
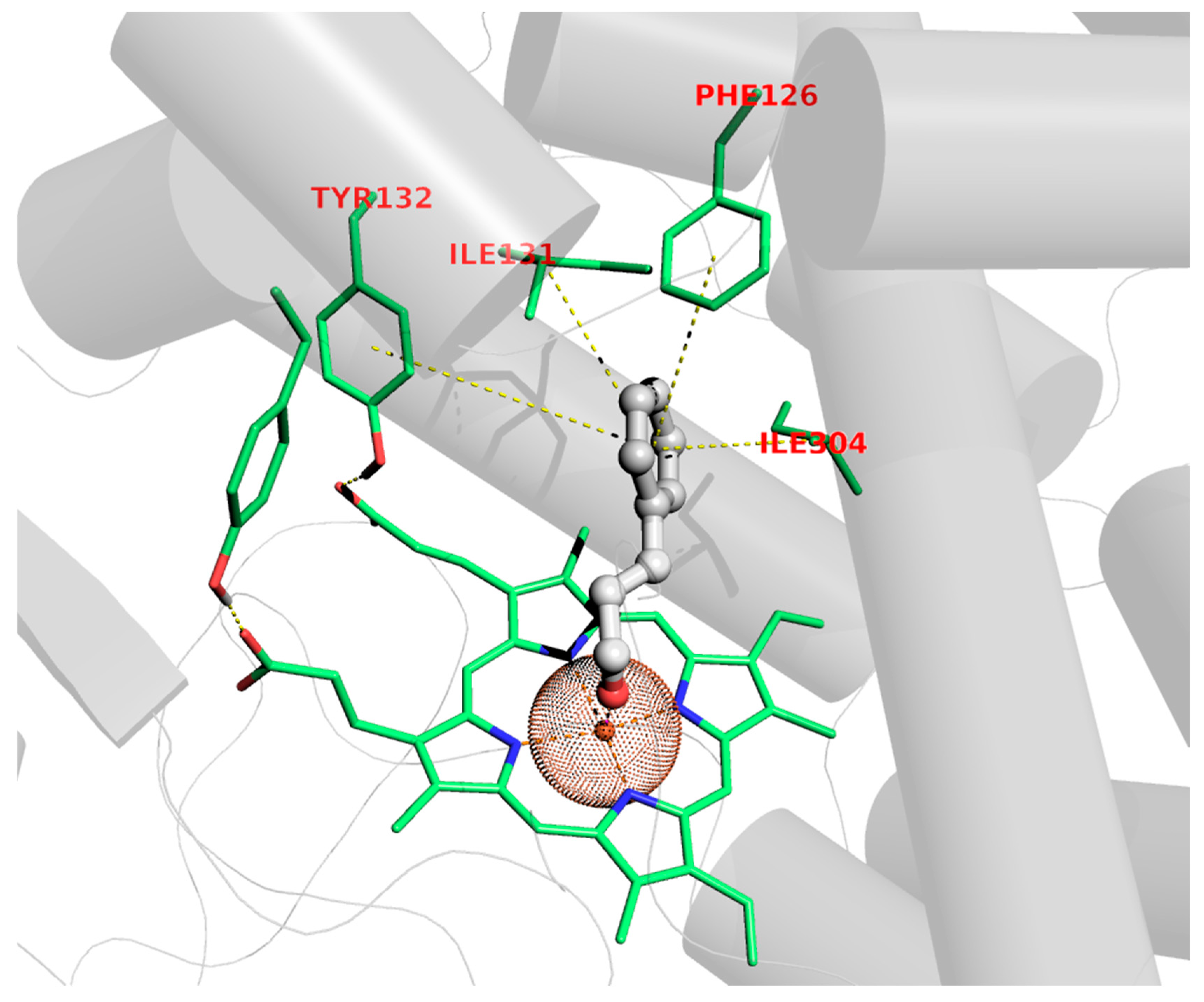
2.4. Molecular Modeling Studies
3. Discussion
4. Materials and Methods
4.1. Materials
4.1.1. Essential Oil
4.1.2. Chemicals
4.1.3. Fungal Strains
4.2. Methods
4.2.1. Antifungal Testing
4.2.2. Medium and Culture Conditions
4.2.3. Preparation of the Test Solution
4.2.4. The Checkerboard Test
4.2.5. Biofilm Biomass Measurement and Reduction
4.2.6. Molecular Modeling Studies
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Guinea, J. Global Trends in the Distribution of Candida Species Causing Candidemia. Clin. Microbiol. Infect. 2014, 20, 5–10. [Google Scholar] [CrossRef] [PubMed]
- Santos, G.C.D.O.; Vasconcelos, C.C.; Lopes, A.J.O.; Cartágenes, M.D.S.D.S.; Filho, A.K.D.B.; Nascimento, F.R.F.D.; Ramos, R.; Pires, E.R.R.B.; Andrade, M.; Rocha, F.M.G.; et al. Candida Infections and Therapeutic Strategies: Mechanisms of Action for Traditional and Alternative Agents. Front. Microbiol. 2018, 9, 1351. [Google Scholar]
- Barchiesi, F.; Orsetti, E.; Osimani, P.; Catassi, C.; Santelli, F.; Manso, E. Factors related to outcome of bloodstream infections due to Candida parapsilosis complex. BMC Infect. Dis. 2016, 16, 387. [Google Scholar] [CrossRef]
- Pathakumari, B.; Liang, G.; Liu, W. Immune defence to invasive fungal infections: A comprehensive review. Biomed. Pharmacother. 2020, 130, 110550. [Google Scholar] [CrossRef] [PubMed]
- Dominguez, E.G.; Andes, D.R. Candida Biofilm Tolerance: Comparison of Planktonic and Biofilm Resistance Mechanisms. In Candida albicans: Cellular and Molecular Biology; Springer International Publishing: Cham, Switzerland, 2017; pp. 77–92. [Google Scholar]
- De Barros, P.P.; Rossoni, R.D.; De Souza, C.M.; Scorzoni, L.; Fenley, J.C.; Junqueira, J.C. Candida Biofilms: An Update on Developmental Mechanisms and Therapeutic Challenges. Mycopathologia, 2020; published online ahead of print. [Google Scholar]
- Roemer, T.; Krysan, D.J. Antifungal drug development: Challenges, unmet clinical needs, and new approaches. Cold Spring Harb. Perspect. 2014, 4, a019703. [Google Scholar] [CrossRef] [PubMed]
- Kowalski, C.H.; Morelli, K.A.; Schultz, D.; Nadell, C.D.; Cramer, R.A. Fungal biofilm architecture produces hypoxic microenvironments that drive antifungal resistance. Proc. Natl. Acad. Sci. USA 2020, 117, 22473–22483. [Google Scholar] [CrossRef] [PubMed]
- Trubenová, B.; Roizman, D.; Moter, A.; Rolff, J.; Regoes, R.R. Population genetics, biofilm recalcitrance, and antibiotic resistance evolution. Trends Microbiol. 2022, 30, 841–852. [Google Scholar] [CrossRef]
- Moraes, D.C.; Ferreira-Pereira, A. Insights on the anti Candidal activity of non-antifungal drugs. J. Mycol. Med. 2019, 29, 253–259. [Google Scholar] [CrossRef] [PubMed]
- Caldara, M.; Marmiroli, N. Antimicrobial Properties of Antidepressants and Antipsychotics—Possibilities and Implications. Pharmaceuticals 2021, 14, 915. [Google Scholar] [CrossRef]
- Bottega, A.; Serafin, M.B.; Da Rosa, T.F.; Foletto, V.S.; Machado, C.D.S.; Coelho, S.S.; Mainardi, A.; Hörner, R. Antimicrobial and Antineoplastic Properties of Sertraline. Am. J. Ther. 2020, 27, e632–e635. [Google Scholar] [CrossRef]
- Muthu, D.; Gowri, M.; Kumar, G.S.; Kattimani, V.S.; Girija, E.K. Repurposing of antidepression drug sertraline for antimicrobial activity against Staphylococcus aureus: A potential approach for the treatment of osteomyelitis. New J. Chem. 2019, 43, 5315–5324. [Google Scholar] [CrossRef]
- Gowri, M.; Jayashree, B.; Jeyakanthan, J.; Girija, E. Sertraline as a promising antifungal agent: Inhibition of growth and biofilm of Candida auris with special focus on the mechanism of action in vitro. J. Appl. Microbiol. 2019, 128, 426–437. [Google Scholar] [CrossRef]
- Treviño-Rangel, R.D.J.; Villanueva-Lozano, H.; Méndez-Galomo, K.S.; Solís-Villegas, E.M.; Becerril-García, M.A.; Montoya, A.M.; Robledo-Leal, E.R.; González, G.M. In vivo evaluation of the antifungal activity of sertraline against Aspergillus fumigatus. J. Antimicrob. Chemother. 2019, 74, 663–666. [Google Scholar] [CrossRef] [PubMed]
- da Silva, C.R.; Sá, L.G.D.A.V.; Ferreira, T.L.; Leitão, A.C.; de Farias Cabral, V.P.; Rodrigues, D.S.; Barbosa, A.D.; Moreira, L.E.A.; Filho, H.L.P.; de Andrade Neto, J.B.; et al. Antifungal activity of selective serotonin reuptake inhibitors against Cryptococcus spp. and their possible mechanism of action. J. Mycol. Med. 2023, 33, 101431. [Google Scholar] [CrossRef]
- Lagrouh, F.; Dakka, N.; Bakri, Y. The antifungal activity of Moroccan plants and the mechanism of action of secondary metabolites from plants. J. Med. Mycol. 2017, 27, 303–311. [Google Scholar] [CrossRef]
- Arif, T.; Bhosale, J.D.; Kumar, N.; Mandal, T.K.; Bendre, R.S.; Lavekar, G.S.; Dabur, R. Natural products—Antifungal agents derived from plants. J. Asian Nat. Prod. Res. 2009, 11, 621–638. [Google Scholar] [CrossRef]
- Dias, M.C.; Pinto, D.C.G.A.; Silva, A.M.S. Plant Flavonoids: Chemical Characteristics and Biological Activity. Molecules 2021, 26, 5377. [Google Scholar] [CrossRef] [PubMed]
- Nazzaro, F.; Fratianni, F.; Coppola, R.; De Feo, V. Essential oils and antifungal activity. Pharmaceuticals 2017, 10, 86. [Google Scholar] [CrossRef]
- Angane, M.; Swift, S.; Huang, K.; Butts, C.A.; Quek, S.Y. Essential oils and their major components: An updated review on antimicrobial activities, mechanism of action and their potential application in the food industry. Foods 2022, 11, 464. [Google Scholar] [CrossRef]
- Hyldgaard, M.; Mygind, T.; Rikke, L.M. Essential oils in food preservation: Mode of action, synergies, and interactions with food matrix components. Front. Microbiol. 2012, 3, 12. [Google Scholar] [CrossRef]
- Chouhan, S.; Sharma, K.; Guleria, S. Antimicrobial Activity of Some Essential Oils—Present Status and Future Perspectives. Medicines 2017, 4, 58. [Google Scholar] [CrossRef]
- El-Tarabily, K.A.; El-Saadony, M.T.; Alagawany, M.; Arif, M.; Batiha, G.E.; Khafaga, A.F.; Elwan, H.A.M.; Elnesr, S.S.; El-Hack, M.E.A. Using essential oils to overcome bacterial biofilm formation and their antimicrobial resistance. Saudi J. Biol. Sci. 2021, 28, 5145–5156. [Google Scholar] [CrossRef] [PubMed]
- Ayaz, M.; Ullah, F.; Sadiq, A.; Ullah, F.; Ovais, M.; Ahmed, J.; Devkota, H.P. Synergistic interactions of phytochemicals with antimicrobial agents: Potential strategy to counteract drug resistance. Chem. Biol. Interact. 2019, 308, 294–303. [Google Scholar] [CrossRef]
- Singh, N.; Rao, A.S.; Nandal, A.; Kumar, S.; Yadav, S.S.; Ganaie, S.A.; Narasimhan, B. Phytochemical and pharmacological review of Cinnamomum verum J. Presl-a versatile spice used in food and nutrition. Food Chem. 2020, 338, 127773. [Google Scholar] [CrossRef] [PubMed]
- Al-Mijalli, S.H.; Mrabti, H.N.; El Hachlafi, N.; El Kamili, T.; Elbouzidi, A.; Abdallah, E.M.; Flouchi, R.; Assaggaf, H.; Qasem, A.; Zengin, G.; et al. Integrated analysis of antimicrobial, antioxidant, and phytochemical properties of Cinnamomum verum: A comprehensive In vitro and In silico study. Biochem. Syst. Ecol. 2023, 110, 104700. [Google Scholar] [CrossRef]
- Wijesinghe, G.K.; de Oliveira, T.R.; Maia, F.C.; de Feiria, S.B.; Barbosa, J.P.; Joia, F.; Boni, G.C.; Höfling, J.F. Efficacy of true cinnamon (Cinnamomum verum) leaf essential oil as a therapeutic alternative for Candida biofilm infections. Iran J. Basic Med. Sci. 2021, 24, 787–795. [Google Scholar] [PubMed]
- Pagliari, S.; Forcella, M.; Lonati, E.; Sacco, G.; Romaniello, F.; Rovellini, P.; Fusi, P.; Palestini, P.; Campone, L.; Labra, M.; et al. Antioxidant and Anti-Inflammatory Effect of Cinnamon (Cinnamomum verum J. Presl) Bark Extract after In Vitro Digestion Simulation. Foods 2023, 12, 452. [Google Scholar] [CrossRef]
- Valková, V.; Ďúranová, H.; Galovičová, L.; Vukovic, N.L.; Vukic, M.; Kowalczewski, P.Ł.; Kačániová, M. Application of Three Types of Cinnamon Essential Oils as Natural Antifungal Preservatives in Wheat Bread. Appl. Sci. 2022, 12, 10888. [Google Scholar] [CrossRef]
- Narayanankutty, A.; Kunnath, K.; Alfarhan, A.; Rajagopal, R.; Ramesh, V. Chemical composition of Cinnamomum verum leaf and flower essential oils and analysis of their antibacterial, insecticidal, and larvicidal properties. Molecules 2021, 26, 6303. [Google Scholar] [CrossRef]
- Padalia, H.; Rathod, T.; Moteriya, P.; Chanda, S. Antimicrobial efficacy of Cinnamonum verum essential oil alone and in combination with antibiotics and other essential oils. Int. J. Curr. Microbiol. Appl. 2017, 6, 3377–3395. [Google Scholar] [CrossRef]
- Erkmen, O. Antimicrobial effects of Cinnamomum verum essential oil against Enterococcus faecalis and Staphylococcus aureus in mulberry and carrot juices. Int. J. Food Sci. Technol. 2024, 59, 2297–2304. [Google Scholar] [CrossRef]
- Rosato, A.; Sblano, S.; Salvagno, L.; Carocci, A.; Clodoveo, M.L.; Corbo, F.; Fracchiolla, G. Anti-biofilm inhibitory synergistic effects of combinations of essential oils and antibiotics. Antibiotics 2020, 9, 637. [Google Scholar] [CrossRef] [PubMed]
- Rosato, A.; Altini, E.; Sblano, S.; Salvagno, L.; Maggi, F.; de Michele, G.; Carocci, A.; Clodoveo, M.L.; Corbo, F.; Fracchiolla, G. Synergistic Activity of New Diclofenac and Essential Oils Combinations against Different Candida spp. Antibiotics 2021, 10, 688. [Google Scholar] [CrossRef]
- Barbarossa, A.; Rosato, A.; Carrieri, A.; Tardugno, R.; Corbo, F.; Clodoveo, M.L.; Fracchiolla, G.; Carocci, A. Antifungal Biofilm Inhibitory Effects of Combinations of Diclofenac and Essential Oils. Antibiotics 2023, 12, 1673. [Google Scholar] [CrossRef] [PubMed]
- Barbarossa, A.; Sblano, S.; Rosato, A.; Carrieri, A.; Corbo, F.; Clodoveo, M.L.; Fracchiolla, G.; Carocci, A. Synergistic Action of Cinnamomum verum Essential Oil with Sertraline. Antibiotics 2022, 11, 1617. [Google Scholar] [CrossRef]
- Oliveira, A.S.; Martinez-de-Oliveira, J.; Donders, G.G.G.; Palmeira-de-Oliveira, R.; Palmeira-de-Oliveira, A. Anti-Candida Activity of Antidepressants Sertraline and Fluoxetine: Effect upon Pre-Formed Biofilms. Med. Microbiol. Immunol. 2018, 207, 195–200. [Google Scholar] [CrossRef]
- Rodrigues, D.S.; Cabral, V.P.D.F.; Barbosa, A.D.; Sá, L.G.D.A.V.; Moreira, L.E.A.; de Andrade Neto, J.B.; da Silva, C.R.; de Moraes, M.O.; Silva, J.; Marinho, E.S.; et al. Sertraline has in vitro activity against both mature and forming biofilms of different Candida species. J. Med. Microbiol. 2023, 72, 001664. [Google Scholar] [CrossRef]
- Adams, R.P. Identification of Essential Oil Components by Gas Chromatography/Mass Spectrometry; Allured Publishing Corporation: Carol Steam, IL, USA, 1995; ISBN 978-1-932633-21-4. [Google Scholar]
- NIST Chemistry WebBook 2022. Available online: https://webbook.nist.gov/chemistry/ (accessed on 20 April 2022).
- Koo, I.; Kim, S.; Zhang, X. Comparative analysis of mass spectral matching-based compound identification in gas chromatographymass spectrometry. J. Chromatogr. A 2013, 1298, 132–138. [Google Scholar] [CrossRef]
- Wan, K.X.; Vidavsky, I.; Gross, M.L. From similarity index to spectral contrast angle. J. Am. Soc. Mass Spectrom. 2002, 13, 85–88. [Google Scholar] [CrossRef]
- Vanden Bossche, H.; Koymans, L. Cytochromes P450 in fungi. Mycoses 1998, 41 (Suppl. S1), 32–38. [Google Scholar]
- Sheehan, D.J.; Hitchcock, C.A.; Sibley, C.M. Current and emerging azole antifungal agents. Clin. Microbiol. Rev. 1999, 12, 40–79. [Google Scholar] [CrossRef] [PubMed]
- Lamb, D.C.; Kelly, D.E.; Kelly, S.L. Molecular diversity of sterol 14α-demethylase substrates in plants, fungi and humans. FEBS Lett. 1998, 425, 263–265. [Google Scholar] [CrossRef] [PubMed]
- Lepesheva, G.I.; Waterman, M.R. Sterol 14alpha-demethylase cytochrome P450 (CYP51), a P450 in all biological kingdoms. Biochim. Biophy. Acta 2007, 1770, 467–477. [Google Scholar] [CrossRef] [PubMed]
- Sevrioukova, I.F.; Poulos, T.L. Structure and mechanism of the complex between cytochrome P4503A4 and ritonavir. Proc. Nat. Acad. Sci. USA 2010, 107, 18422–18427. [Google Scholar] [CrossRef]
- De Cian, A.; Weiss, R. Structures de complexes π carbonyés du fer. II. Structure cristalline et moléculaire de l’aldéhyde cinnamique fertricarbonyle: C6H5CH=CH–CHO.Fe(CO)3. Acta Cryst. 1972, B28, 3273–3280. [Google Scholar] [CrossRef]
- Sacerdoti, M.; Bertolasi, V.; Gilli, G. The structure of dicarbonyl(η4-cinnamaldehyde)(triphenylphosphine)iron(0). Acta Cryst. 1980, B36, 1061–1065. [Google Scholar] [CrossRef]
- O’Boyle, N.M.; Banck, M.; James, C.A.; Morley, C.; Vandermeersch, T.; Hutchison, G.R. Open Babel: An open chemical toolbox. J. Cheminform. 2011, 3, 33. [Google Scholar] [CrossRef]
- Keniya, M.V.; Sabherwal, M.; Wilson, R.K.; Woods, M.A.; Sagatova, A.A.; Tyndall, J.D.A.; Monk, B.C. Crystal Structures of Full-Length Lanosterol 14α-Demethylases of Prominent Fungal Pathogens Candida albicans and Candida glabrata Provide Tools for Antifungal Discovery. Antimicrob. Agents Chemother. 2018, 62, 1134. [Google Scholar] [CrossRef]
- Schrödinger Release 2023-4: Maestro; Schrödinger, LLC.: New York, NY, USA, 2023.
- Morris, G.M.; Goodsell, D.S.; Halliday, R.S.; Huey, R.; Hart, W.E.; Belew, R.K.; Olson, A.J. Automated docking using a Lamarckian genetic algorithm and an empirical binding free energy function. J. Comput. Chem. 1998, 19, 1639–1662. [Google Scholar] [CrossRef]
- Khoury, L.E.; Santos-Martins, D.; Sasmal, S.; Eberhardt, J.; Bianco, G.; Ambrosio, F.A.; Solis-Vasquez, L.; Koch, A.; Forli, S.; Mobley, D.L. Comparison of affinity ranking using AutoDock-GPU and MM-GBSA scores for BACE-1 inhibitors in the D3R Grand Challenge 4. J. Comput. Aided Mol. Des. 2019, 33, 1011–1020. [Google Scholar] [CrossRef]
- QUACPAC 2.1.0.4, OpenEye Scientific Software, Santa Fe, NM. Available online: http://www.eyesopen.com (accessed on 5 August 2024).
- Cornell, W.D.; Cieplak, P.; Bayly, C.I.; Gould, I.R.; Merz, K.M.; Ferguson, D.M.; Spellmeyer, D.C.; Fox, T.; Caldwell, J.W.; Kollman, P.A. A second generation force field for the simulation of proteins, nucleic acids, and organic molecules. J. Am. Chem. Soc. 1995, 117, 5179–5197. [Google Scholar] [CrossRef]
- Pristov, K.E.; Ghannoum, M.A. Resistance of Candida to azoles and echinocandins worldwide. Clin. Microbiol. Infect. 2019, 25, 792–798. [Google Scholar] [CrossRef]
- Gulati, M.; Nobile, C.J. Candida albicans biofilms: Development, regulation, and molecular mechanisms. Microbes Infect. 2016, 18, 310–321. [Google Scholar] [CrossRef]
- Nobile, C.J.; Johnson, A.D. Candida albicans Biofilms and Human Disease. Annu. Rev. Microbiol. 2015, 69, 71–92. [Google Scholar] [CrossRef] [PubMed]
- Mathe, L.; Van Dijck, P. Recent insights into Candida albicans biofilm resistance. Curr. Genet. 2013, 59, 251–264. [Google Scholar] [CrossRef] [PubMed]
- Foletto, V.S.; da Rosa, T.F.; Serafin, M.B.; Bottega, A.; Hörner, R. Repositioning of non-antibiotic drugs as an alternative to microbial resistance: A systematic review. Int. J. Antimicrob. Agents 2021, 58, 106380. [Google Scholar] [CrossRef] [PubMed]
- Caldara, M.; Marmiroli, N. Tricyclic antidepressants inhibit Candida albicans growth and biofilm formation. Int. J. Antimicrob. Agents 2018, 52, 500–505. [Google Scholar] [CrossRef] [PubMed]
- Alanís-Ríos, S.A.; González, G.M.; Andrade, A.; Becerril-García, M.A.; Bonifaz, A.; Robledo-Leal, E.R.; Montoya, A.M.; Treviño-Rangel, R.D.J. Evaluation of the synergistic antifungal activity of micafungin and voriconazole plus sertraline against Candida auris. Braz. J. Microbiol. 2022, 53, 2003–2008. [Google Scholar] [CrossRef]
- Alkhalifa, B.A.; Bulatova, N.R.; abuRokba, W.; Darwish, R.M. Serotonin reuptake inhibitors effect on fluconazole activity against resistant Candida glabrata strains. J. Glob. Antimicrob. Resist. 2022, 29, 49–54. [Google Scholar] [CrossRef]
- Ahmed, E.I.; Alhuwaydi, A.M.; Taha, A.E.; Abouelkheir, M. Anti-Candidal Activity of Reboxetine and Sertraline Antidepressants: Effects on Pre-Formed Biofilms. Antibiotics 2023, 12, 881. [Google Scholar] [CrossRef]
- Rodrigues, D.S.; Cabral, V.P.; Barbosa, A.D.; Valente Sá, L.G.; Silva, C.R.; Moreira, L.E.; Neto, J.B.A.; Silva, J.; Santos, H.S.; Marinho, E.S.; et al. Sertraline has fungicidal activity against Candida spp. and acts by inhibiting membrane and cell wall biosynthesis. Future Microbiol. 2023, 18, 1025–1039. [Google Scholar] [CrossRef] [PubMed]
- Sahal, G.; Woerdenbag, H.J.; Hinrichs, W.L.; Visser, A.; Tepper, P.G.; Quax, W.J.; van der Mei, H.C.; Bilkay, I.S. Antifungal and biofilm inhibitory effect of Cymbopogon citratus (lemongrass) essential oil on biofilm forming by Candida tropicalis isolates; an in vitro study. J. Ethnopharmacol. 2020, 246, 112188. [Google Scholar] [CrossRef]
- Garcia, L.G.S.; da Rocha, M.G.; Lima, L.R.; Cunha, A.P.; de Oliveira, J.S.; de Andrade, A.R.C.; Ricardo, N.M.P.S.; Pereira-Neto, W.A.; Sidrim, J.J.C.; Rocha, M.F.G.; et al. Essential oils encapsulated in chitosan microparticles against Candida albicans biofilms. Int. J. Biol. Macromol. 2021, 166, 621–632. [Google Scholar] [CrossRef] [PubMed]
- Rosato, A.; Barbarossa, A.; Mustafa, A.M.; Bonacucina, G.; Perinelli, D.R.; Petrelli, R.; Maggi, F.; Spinozzi, E. Comprehensive Evaluation of the Antibacterial and Antifungal Activities of Carlina acaulis L. Essential Oil and Its Nanoemulsion. Antibiotics 2021, 10, 1451. [Google Scholar] [CrossRef] [PubMed]
- Rosato, A.; Carocci, A.; Catalano, A.; Clodoveo, M.L.; Franchini, C.; Corbo, F.; Carbonara, G.G.; Carrieri, A.; Fracchiolla, G. Elucidation of the synergistic action of Mentha Piperita essential oil with common antimicrobials. PLoS ONE 2018, 13, e0200902. [Google Scholar] [CrossRef] [PubMed]
- Salvagno, L.; Sblano, S.; Fracchiolla, G.; Corbo, F.; Clodoveo, M.L.; Rosato, A. Antibiotics—Mentha piperita essential oil synergism inhibits mature bacterial biofilm. Chem. Today 2020, 38, 49–52. [Google Scholar]
- Rosato, A.; Vitali, C.; De Laurentis, N.; Armenise, D.; Milillo, M.A. Antibacterial effect of some essential oils administered alone or in combination with Norfloxacin. Phytomedicine 2007, 14, 727–732. [Google Scholar] [CrossRef]
- Yap, P.S.; Lim, S.H.; Hu, C.P.; Yiap, B.C. Combination of essential oils and antibiotics reduce antibiotic resistance in plasmid-conferred multidrug resistant bacteria. Phytomedicine 2013, 20, 710–713. [Google Scholar] [CrossRef]
- Yap, P.S.; Krishnan, T.; Chan, K.G.; Lim, S.H. Antibacterial Mode of Action of Cinnamomum verum Bark Essential Oil, Alone and in Combination with Piperacillin, Against a Multi-Drug-Resistant Escherichia coli Strain. J. Microbiol. Biotechnol. 2015, 25, 1299–1306. [Google Scholar] [CrossRef]
- Essid, R.; Hammami, M.; Gharbi, D.; Karkouch, I.; Hamouda, T.B.; Elkahoui, S.; Limam, F.; Tabbene, O. Antifungal Mechanism of the Combination of Cinnamomum Verum and Pelargonium Graveolens Essential Oils with Fluconazole against Pathogenic Candida Strains. Appl. Microbiol. Biotechnol. 2017, 101, 6993–7006. [Google Scholar] [CrossRef]
- Essid, R.; Gharbi, D.; Abid, G.; Karkouch, I.; Ben Hamouda, T.; Fares, N.; Trabelsi, D.; Mhadhbi, H.; Elkahoui, S.; Limam, F.; et al. Combined effect of Thymus capitatus and Cinnamomum verum essential oils with conventional drugs against Candida albicans biofilm formation and elucidation of the molecular mechanism of action. Ind. Crop. Prod. 2019, 140, 111720. [Google Scholar] [CrossRef]
- Shariati, A.; Didehdar, M.; Razavi, S.; Heidary, M.; Soroush, F.; Chegini, Z. Natural Compounds: A Hopeful Promise as an Antibiofilm Agent against Candida Species. Front. Pharmacol. 2022, 13, 917787. [Google Scholar] [CrossRef]
- Clinical and Laboratory Standards Institute (CLSI). Performance Standards for Antimicrobial Susceptibility Testing. Available online: https://clsi.org/media/3481/m100ed30_sample.pdf (accessed on 15 May 2023).
- OuYang, Q.; Duan, X.; Li, L.; Tao, N. Cinnamaldehyde exerts its antifungal activity by disrupting the cell wall integrity of Geotrichum citri-aurantii. Front. Microbiol. 2019, 10, 55. [Google Scholar] [CrossRef] [PubMed]
- de Oliveira Pereira, F.; Mendes, J.M.; de Oliveira Lima, E. Investigation on mechanism of antifungal activity of eugenol against Trichophyton rubrum. Med. Mycol. 2013, 51, 507–513. [Google Scholar] [CrossRef]
- Lee, J.E.; Jung, M.; Lee, S.C.; Huh, M.J.; Seo, S.M.; Park, I.K. Antibacterial mode of action of trans-cinnamaldehyde derived from cinnamon bark (Cinnamomum verum) essential oil against Agrobacterium tumefaciens. Pestic. Biochem. Phys. 2020, 165, 104546. [Google Scholar] [CrossRef]
- Giske, C.G.; Turnidge, J.; Cantón, R.; Kahlmeter, G. Update from the European committee on antimicrobial susceptibility testing (EUCAST). J. Clin. Microbiol. 2022, 60, e00276-21. [Google Scholar] [CrossRef]
- Eloff, J.N. Quantifying the bioactivity of plant extracts during screening and bioassay-guided fractionation. Phytomedicine 2004, 11, 370–371. [Google Scholar] [CrossRef] [PubMed]
- Williamson, E.M. Synergy and other interactions in phytomedicines. Phytomedicine 2001, 8, 401–409. [Google Scholar] [CrossRef]
- White, D.C.; Arrage, A.A.; Nivens, D.E.; Palmer, R.J.; Rice, J.F.; Sayler, G.S. Biofilm ecology: On-line methods bring new insights into mic and microbial biofouling. Biofouling 1996, 10, 3–16. [Google Scholar] [CrossRef]
- Stepanovíc, S.; Vukovíc, D.; Dakíc, I.; Savíc, B.; Švabíc-Vlahovíc, M. A modified microtiter-plate test for quantification of staphylococcal biofilm formation. J. Microbiol. Methods 2000, 40, 175–179. [Google Scholar] [CrossRef]
- Saracino, I.M.; Foschi, C.; Pavoni, M.; Spigarelli, R.; Valerii, M.C.; Spisni, E. Antifungal Activity of Natural Compounds vs. Candida spp.: A Mixture of Cinnamaldehyde and Eugenol Shows Promising In Vitro Results. Antibiotics 2022, 11, 73. [Google Scholar]
| Compound | Peacks Area % ± SEM | Library/ID | SI/MS | LRI | AI |
|---|---|---|---|---|---|
| 1 | 0.3 ± 0.1 | α-Pinene a | 94 | 934 | 934 |
| 2 | 0.1 ± 0.03 | Camphene | 96 | 950 | 949 |
| 3 | 0.5 ± 0.1 | β-Thujene | 91 | 965 | 968 |
| 4 | 0.2 ± 0.1 | α-Phellandrene a | 90 | 1005 | 1001 |
| 5 | 0.5 ± 0.1 | p-Cymene | 95 | 1021 | 1021 |
| 6 | 1.5 ± 0.30 | Eucalyptol a | 98 | 1023 | 1023 |
| 7 | 7 ± 1 | Linalool a | 97 | 1095 | 1098 |
| 8 | 0.2 ± 0.01 | o-Anisaldehyde | 98 | 1220 | 1222 |
| 9 | 73 ± 5 | (E)-Cinnamaldehyde a | 97 | 1225 | 1226 |
| 10 | 0.2 ± 0.04 | Safrole | 97 | 1285 | 1287 |
| 11 | 0.4 ± 0.05 | α-Cubebene | 98 | 1348 | 1348 |
| 12 | 6 ± 1 | Eugenol a | 98 | 1360 | 1359 |
| 13 | 4 ± 1 | Caryophyllene a | 99 | 1410 | 1408 |
| 14 | 0.5 ± 0.1 | Humulene | 95 | 1452 | 1452 |
| 15 | 5 ± 1 | Cinnamyl Acetate a | 97 | 1455 | 1455 |
| 16 | 0.2 ± 0.02 | Eugenol Acetate | 96 | 1525 | 1524 |
| 17 | 0.3 ± 0.04 | Caryophyllene oxide | 83 | 1580 | 1578 |
| 18 | 0.6 ± 0.1 | Benzyl Benzoate | 96 | 1755 | 1753 |
| Strains | MICo a | MICc b | FIC c | FICI d | R% e |
|---|---|---|---|---|---|
| C. albicans ATCC 10231 | |||||
| Sertraline | 64.00 | 3.20 | 0.05 | 0.11 | 95 |
| C. verum EO | 0.32 | 0.02 | 0.06 | 94 | |
| C. albicans ATCC 90028 | |||||
| Sertraline | 32.00 | 0.80 | 0.03 | 0.08 | 97 |
| C. verum EO | 1.22 | 0.06 | 0.05 | 95 | |
| C. albicans 10 A12 | |||||
| Sertraline | 64.00 | 3.20 | 0.05 | 0.17 | 95 |
| C. verum EO | 0.64 | 0.08 | 0.12 | 87.5 | |
| C. albicans A18 | |||||
| Sertraline | 128.00 | 6.40 | 0.05 | 0.11 | 95 |
| C. verum EO | 0.32 | 0.02 | 0.06 | 94 | |
| C. glabrata ATCC 15126 | |||||
| Sertraline | 64.00 | 3.20 | 0.05 | 0.11 | 95 |
| C. verum EO | 0.64 | 0.04 | 0.60 | 94 | |
| C. kefyr ATCC 204093 | |||||
| Sertraline | 64.00 | 3.20 | 0.05 | 0.08 | 95 |
| C. verum EO | 0.32 | 0.01 | 0.03 | 97 | |
| C. krusei ATCC 6258 | |||||
| Sertraline | 64.00 | 6.40 | 0.10 | 0.16 | 90 |
| C. verum EO | 0.32 | 0.02 | 0.06 | 94 | |
| C. krusei 31A29 | |||||
| Sertraline | 64.00 | 3.20 | 0.05 | 0.11 | 95 |
| C. verum EO | 0.32 | 0.01 | 0.06 | 97 | |
| C. tropicalis ATCC 750 | |||||
| Sertraline | 128.00 | 12.80 | 0.10 | 0.16 | 90 |
| C. verum EO | 1.22 | 0.08 | 0.06 | 93 |
| C. verum EO mg/mL | Sertraline µg/mL | Synergism | ||||||
|---|---|---|---|---|---|---|---|---|
| Strains | sMIC50 a | %Red ± SD b | sMIC50 c | %Red ± SD d | C. verum EO mg/mL e | Sertraline µg/mL f | Sertraline + C. verum EO %Red ± SD g | FICI h |
| C. albicans ATCC 10231 | 0.80 | 52.90 ± 0.50 | 160.00 | 76.10 ± 0.82 | 0.05 | 16.00 | 72.8 ± 0.90 | 0.16 |
| C. albicans ATCC 90028 | 3.05 | 67.25 ± 0.55 | 40.00 | 57.59 ± 0.50 | 0.40 | 4.00 | 86.44 ± 1.00 | 0.23 |
| C. albicans 10 A12 | 1.60 | 55.16 ± 0.80 | 160.00 | 63.80 ± 0.80 | 0.20 | 16.00 | 75.29 ± 0.80 | 0.23 |
| C. albicans A18 | 1.60 | 55.21 ± 0.70 | 320.00 | 53.07 ± 0.40 | 0.40 | 32.00 | 77.02 ± 0.40 | 0.35 |
| C. glabrata ATCC 15126 | 0.8 | 83.09 ± 1.00 | 320.00 | 82.00 ± 1.00 | 0.10 | 16.00 | 59.90 ± 0.50 | 0.18 |
| C. kefyr ATCC 204093 | 0.40 | 64.40 ± 0.45 | 320.00 | 84.80 ± 0.90 | 0.05 | 16.00 | 79.80 ± 0.90 | 0.20 |
| C. krusei ATCC 6558 | 0.40 | 69.22 ± 0.20 | 320.00 | 67.43 ± 0.30 | 0.10 | 32.0 | 64.90 ± 1.00 | 0.35 |
| C. krusei 31 A29 | 0.80 | 62.15 ± 0.50 | 160.00 | 65.27 ± 1.00 | 0.2 | 8.00 | 69.44 ± 0.80 | 0.30 |
| C. tropicalis ATCC 750 | 1.52 | 55.30 ± 1.00 | 640.00 | 58.16 ± 0.80 | 0.38 | 32.00 | 68.25 ± 0.50 | 0.30 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barbarossa, A.; Rosato, A.; Carrieri, A.; Fumarola, L.; Tardugno, R.; Corbo, F.; Fracchiolla, G.; Carocci, A. Exploring the Antibiofilm Effect of Sertraline in Synergy with Cinnamomum verum Essential Oil to Counteract Candida Species. Pharmaceuticals 2024, 17, 1109. https://doi.org/10.3390/ph17091109
Barbarossa A, Rosato A, Carrieri A, Fumarola L, Tardugno R, Corbo F, Fracchiolla G, Carocci A. Exploring the Antibiofilm Effect of Sertraline in Synergy with Cinnamomum verum Essential Oil to Counteract Candida Species. Pharmaceuticals. 2024; 17(9):1109. https://doi.org/10.3390/ph17091109
Chicago/Turabian StyleBarbarossa, Alexia, Antonio Rosato, Antonio Carrieri, Luciana Fumarola, Roberta Tardugno, Filomena Corbo, Giuseppe Fracchiolla, and Alessia Carocci. 2024. "Exploring the Antibiofilm Effect of Sertraline in Synergy with Cinnamomum verum Essential Oil to Counteract Candida Species" Pharmaceuticals 17, no. 9: 1109. https://doi.org/10.3390/ph17091109
APA StyleBarbarossa, A., Rosato, A., Carrieri, A., Fumarola, L., Tardugno, R., Corbo, F., Fracchiolla, G., & Carocci, A. (2024). Exploring the Antibiofilm Effect of Sertraline in Synergy with Cinnamomum verum Essential Oil to Counteract Candida Species. Pharmaceuticals, 17(9), 1109. https://doi.org/10.3390/ph17091109









