Drug Delivery Systems for Glaucoma: A Narrative Review
Abstract
1. Introduction
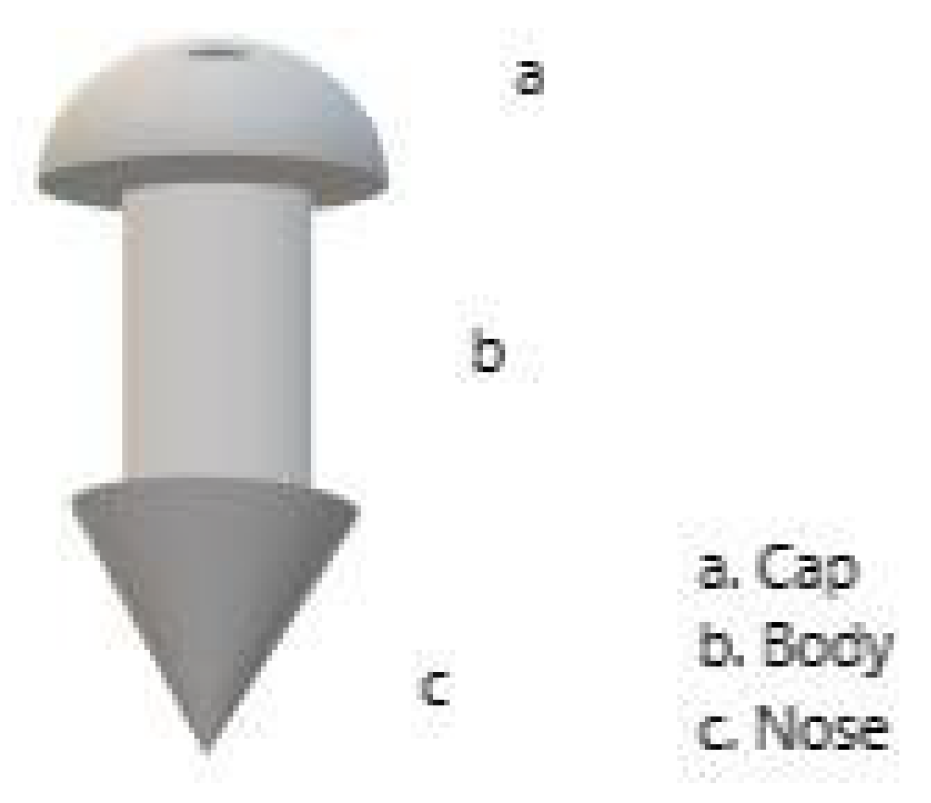
2. Punctal Plugs Delivery System
3. Conjunctival Fornix Delivery System
4. Contact Lens for Ophthalmic Drug Delivery
5. Periocular Drug Delivery Systems
6. Intracameral Delivery System
7. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Allison, K.; Patel, D.; Alabi, O. Epidemiology of Glaucoma: The Past, Present, and Predictions for the Future. Cureus 2020, 12, e11686. [Google Scholar] [CrossRef]
- Schuster, A.K.; Erb, C.; Hoffmann, E.M.; Dietlein, T.; Pfeiffer, N. The Diagnosis and Treatment of Glaucoma. Dtsch. Ärzteblatt Int. 2020, 117, 225. [Google Scholar] [CrossRef] [PubMed]
- Weinreb, R.N.; Aung, T.; Medeiros, F.A. The Pathophysiology and Treatment of Glaucoma: A Review. JAMA 2014, 311, 1901. [Google Scholar] [CrossRef] [PubMed]
- Newman-Casey, P.A.; Robin, A.L.; Blachley, T.; Farris, K.; Heisler, M.; Resnicow, K.; Lee, P.P. The Most Common Barriers to Glaucoma Medication Adherence. Ophthalmology 2015, 122, 1308–1316. [Google Scholar] [CrossRef] [PubMed]
- Olthoff, C.; Schouten, J.; Vandeborne, B.; Webers, C. Noncompliance with Ocular Hypotensive Treatment in Patients with Glaucoma or Ocular HypertensionAn Evidence-Based Review. Ophthalmology 2005, 112, 953–961.E7. [Google Scholar] [CrossRef]
- Rossi, G.C.; Pasinetti, G.M.; Scudeller, L.; Radaelli, R.; Bianchi, P.E. Do adherence rates and glaucomatous visual field progression correlate? Eur. J. Ophthalmol. 2011, 21, 410–414. [Google Scholar] [CrossRef] [PubMed]
- Kompella, U.B.; Hartman, R.R.; Patil, M.A. Extraocular, periocular and intraocular routes for sustained drug delivery for glaucoma. Prog. Retin. Eye Res. 2021, 82, 100901. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Singh, R.B.; Ichhpujani, P.; Thakur, S.; Jindal, S. Promising Therapeutic Drug Delivery Systems for Glaucoma: A Comprehensive Review. Ophthalmol. Eye Dis. 2020, 12, 251584142090574. [Google Scholar] [CrossRef]
- Kesav, N.P.; Young, C.E.C.; Ertel, M.K.; Seibold, L.K.; Kahook, M.Y. Sustained-Release Drug Delivery Systems for the Treatment of Glaucoma. Int. J. Ophthalmol. 2021, 14, 148–159. [Google Scholar] [CrossRef]
- Jehangir, N.; Bever, G.; Mahmood, S.M.J.; Moshirfar, M. Comprehensive Review of the Literature on Existing Punctal Plugs for the Management of Dry Eye Disease. J. Ophthalmol. 2016, 2016, 9312340. [Google Scholar] [CrossRef]
- Chen, X.; Shen, T. Advances in Innovative Delivery Systems for Antiglaucoma Drugs. Curr. Opin. Ophthalmol. 2023, 34, 123–128. [Google Scholar] [CrossRef] [PubMed]
- Calonge, M. The Treatment of Dry Eye. Surv. Ophthalmol. 2001, 45 (Suppl. S2), S227–S239. [Google Scholar] [CrossRef] [PubMed]
- Balaram, M.; Schaumberg, D.A.; Dana, M.R. Efficacy and Tolerability Outcomes after Punctal Occlusion with Silicone Plugs in Dry Eye Syndrome. Am. J. Ophthalmol. 2001, 131, 30–36. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.; Yung Choi, S. Preliminary Outcomes of Temporary Collagen Punctal Plugs for Patients with Dry Eye and Glaucoma. Med. Hypothesis Discov. Innov. Ophthalmol. 2020, 9, 56–60. [Google Scholar]
- Sherwin, J.C.; Ratnarajan, G.; Elahi, B.; Bilkiewicz-Pawelec, A.; Salmon, J.F. Effect of a Punctal Plug on Ocular Surface Disease in Patients Using Topical Prostaglandin Analogues: A Randomized Controlled Trial. Clin. Exp. Ophthalmol. 2018, 46, 888–894. [Google Scholar] [CrossRef]
- Perera, S.A.; Ting, D.S.; Nongpiur, M.E.; Chew, P.T.; Aquino, M.C.D.; Sng, C.C.; Ho, S.-W.; Aung, T. Feasibility Study of Sustained-Release Travoprost Punctum Plug for Intraocular Pressure Reduction in an Asian Population. Clin. Ophthalmol. 2016, 10, 757–764. [Google Scholar] [CrossRef]
- Kompella, U.B.; Kadam, R.S.; Lee, V.H.L. Recent Advances in Ophthalmic Drug Delivery. Ther. Deliv. 2010, 1, 435–456. [Google Scholar] [CrossRef]
- Zimmerman, T.J.; Kooner, K.S.; Kandarakis, A.S.; Ziegler, L.P. Improving the Therapeutic Index of Topically Applied Ocular Drugs. Arch. Ophthalmol. 1984, 102, 551–553. [Google Scholar] [CrossRef]
- Huang, T.C.; Lee, D.A. Punctal Occlusion and Topical Medications for Glaucoma. Am. J. Ophthalmol. 1989, 107, 151–155. [Google Scholar] [CrossRef]
- Tyson, S.L.; Bafna, S.; Gira, J.P.; Goldberg, D.F.; Jones, J.J.; Jones, M.P.; Kim, J.K.; Martel, J.M.; Nordlund, M.L.; Piovanetti-Perez, I.K.; et al. Multicenter Randomized Phase 3 Study of a Sustained-Release Intracanalicular Dexamethasone Insert for Treatment of Ocular Inflammation and Pain after Cataract Surgery. J. Cataract. Refract. Surg. 2019, 45, 204–212. [Google Scholar] [CrossRef]
- Gira, J.P.; Sampson, R.; Silverstein, S.M.; Walters, T.R.; Metzinger, J.L.; Talamo, J.H. Evaluating the Patient Experience after Implantation of a 0.4 mg Sustained Release Dexamethasone Intracanalicular Insert (DextenzaTM): Results of a Qualitative Survey. Patient Prefer. Adherence 2017, 11, 487–494. [Google Scholar] [CrossRef] [PubMed]
- Wilson, C.; Sall, K.N.; Bafna, S.; Gira, J.P.; McLaurin, E.B.; Protzko, E.; Sampson, R.; Tekwani, N.; Tepedino, M.; Vold, S.; et al. Results of A Randomized, Double-Masked, Parallel-Arm Phase 2b Study Evaluating the Safety and Efficacy of OTX-TP (Travoprost Insert) Compared to Timolol Drops for the Treatment of Patients with Open-Angle Glaucoma or Ocular Hypertension. Investig. Ophthalmol. Vis. Sci. 2017, 58, 2111. [Google Scholar]
- Vantipalli, S.; Sall, K.N.; Stein, E.; Schenker, H.; Mulaney, J.; Smyth-Medina, R.; Day, D.; Benza, R.; Dixon, E.-R.; Rissman, N.; et al. Evaluation of the Safety and Efficacy of OTX-TP, an Intracanalicular Travoprost Insert, for the Treatment of Patients with Open-Angle Glaucoma or Ocular Hypertension: A Phase 3 Study. Investig. Ophthalmol. Vis. Sci. 2020, 61, 3488. [Google Scholar]
- Goldberg, D.F.; Williams, R. A Phase 2 Study Evaluating Safety and Efficacy of the Latanoprost Punctal Plug Delivery System (L-PPDS) in Subjects with Ocular Hypertension (OH) or Open-Angle Glaucoma (OAG). Investig. Ophthalmol. Vis. Sci. 2012, 53, 5095. [Google Scholar]
- Tost, F.H.; Geerling, G. Plugs for Occlusion of the Lacrimal Drainage System. Surg. Dry Eye 2008, 41, 193–212. [Google Scholar]
- Stout, N.; Harsch, A.G.; Lighthizer, N. Plug the Drain with Lacrimal Occlusion: Keep Dry Eye Patients Flowing into Your Office with This Time-Honored Technique. Rev. Optom. 2016, 153, 70–75. [Google Scholar]
- Macoul, K.L.; Pavan-Langston, D. Pilocarpine Ocusert System for Sustained Control of Ocular Hypertension. Arch. Ophthalmol. 1975, 93, 587–590. [Google Scholar] [CrossRef] [PubMed]
- Brandt, J.D.; Sall, K.; DuBiner, H.; Benza, R.; Alster, Y.; Walker, G.; Semba, C.P.; Budenz, D.; Day, D.; Flowers, B.; et al. Six-Month Intraocular Pressure Reduction with a Topical Bimatoprost Ocular Insert. Ophthalmology 2016, 123, 1685–1694. [Google Scholar] [CrossRef]
- Brandt, J.D.; DuBiner, H.B.; Benza, R.; Sall, K.N.; Walker, G.A.; Semba, C.P.; Budenz, D.; Day, D.; Flowers, B.; Lee, S.; et al. Long-Term Safety and Efficacy of a Sustained-Release Bimatoprost Ocular Ring. Ophthalmology 2017, 124, 1565–1566. [Google Scholar] [CrossRef]
- Nair, R.V.; Shefrin, S.; Suresh, A.; Anoop, K.R.; Nair, S.C. Sustained Release Timolol Maleate Loaded Ocusert Based on Biopolymer Composite. Int. J. Biol. Macromol. 2018, 110, 308–317. [Google Scholar] [CrossRef]
- Kelly, J.A.; Molyneux, P.D.; Smith, S.A.; Smith, S.E. Relative Bioavailability of Pilocarpine from a Novel Ophthalmic Delivery System and Conventional Eye Drop Formulations. Br. J. Ophthalmol. 1989, 73, 360–362. [Google Scholar] [CrossRef] [PubMed]
- Greaves, J.; Wilson, C.; Birmingham, A.; Richardson, M.; Bentley, P. Scintigraphic Studies on the Corneal Residence of a New Ophthalmic Delivery System (NODS): Rate of Clearance of a Soluble Marker in Relation to Duration of Pharmacological Action of Pilocarpine. Br. J. Clin. Pharmacol. 1992, 33, 603–609. [Google Scholar] [CrossRef] [PubMed]
- Diestelhorst, M.; Krieglstein, G.K. The Ocular Tolerability of a New Ophthalmic Drug Delivery System (NODS). Int. Ophthalmol. 1994, 18, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Bigdeli, A.; Makhmalzadeh, B.S.; Feghhi, M.; SoleimaniBiatiani, E. Cationic Liposomes as Promising Vehicles for Timolol/Brimonidine Combination Ocular Delivery in Glaucoma: Formulation Development and in Vitro/in Vivo Evaluation. Drug Deliv. Transl. Res. 2023, 13, 1035–1047. [Google Scholar] [CrossRef]
- Awwad, S.; Mohamed Ahmed, A.H.A.; Sharma, G.; Heng, J.S.; Khaw, P.T.; Brocchini, S.; Lockwood, A. Principles of Pharmacology in the Eye: Principles of Pharmacology in the Eye. Br. J. Pharmacol. 2017, 174, 4205–4223. [Google Scholar] [CrossRef]
- Pollack, I.P.; Quigley, H.A.; Harbin, T.S. The Ocusert Pilocarpine System: Advantages and Disadvantages. South. Med. J. 1976, 69, 1296–1298. [Google Scholar] [CrossRef]
- Uner, B.; Ozdemir, S.; Nur Pilevne, S.; Cenk Celebi, A.R. Timolol-loaded ethosomes for ophthalmic delivery: Reduction of high intraocular pressure in vivo. Int. J. Pharm. 2023, 640, 123021. [Google Scholar] [CrossRef] [PubMed]
- Cuggino, J.C.; Tártara, L.I.; Gugliotta, L.M.; Palma, S.D.; Alvarez Igarzabal, C.I. Mucoadhesive and responsive nanogels as carriers for sustainable delivery of timolol for glaucoma therapy. Mater. Sci. Eng. C Mater. Biol. Appl. 2021, 118, 111383. [Google Scholar] [CrossRef] [PubMed]
- Ilka, R.; Mohseni, M.; Kianirad, M.; Naseripour, M.; Ashtari, K.; Mehravi, B. Nanogel-based natural polymers as smart carriers for the controlled delivery of Timolol Maleate through the cornea for glaucoma. Int. J. Biol. Macromol. 2018, 109, 955–962. [Google Scholar] [CrossRef] [PubMed]
- Cegielska, O.; Sierakowski, M.; Sajkiewicz, P.; Lorenz, K.; Kogermann, K. Mucoadhesive brinzolamide-loaded nanofibers for alternative glaucoma treatment. Eur. J. Pharm. Biopharm. 2022, 180, 48–62. [Google Scholar] [CrossRef] [PubMed]
- Agban, Y.; Lian, J.; Prabakar, S.; Seyfoddin, A.; Rupenthal, I.D. Nanoparticle Cross-Linked Collagen Shields for Sustained Delivery of Pilocarpine Hydrochloride. Int. J. Pharm. 2016, 501, 96–101. [Google Scholar] [CrossRef] [PubMed]
- Hiratani, H.; Alvarez-Lorenzo, C. Timolol Uptake and Release by Imprinted Soft Contact Lenses Made of N,N-Diethylacrylamide and Methacrylic Acid. J. Control. Release 2002, 83, 223–230. [Google Scholar] [CrossRef]
- Kim, J.; Conway, A.; Chauhan, A. Extended Delivery of Ophthalmic Drugs by Silicone Hydrogel Contact Lenses. Biomaterials 2008, 29, 2259–2269. [Google Scholar] [CrossRef] [PubMed]
- Peng, C.-C.; Burke, M.T.; Carbia, B.E.; Plummer, C.; Chauhan, A. Extended Drug Delivery by Contact Lenses for Glaucoma Therapy. J. Control. Release 2012, 162, 152–158. [Google Scholar] [CrossRef] [PubMed]
- Braga, M.E.M.; Costa, V.P.; Pereira, M.J.T.; Fiadeiro, P.T.; Gomes, A.P.; Duarte, C.M.M.; De Sousa, H.C. Effects of Operational Conditions on the Supercritical Solvent Impregnation of Acetazolamide in Balafilcon A Commercial Contact Lenses. Int. J. Pharm. 2011, 420, 231–243. [Google Scholar] [CrossRef]
- Jung, H.J.; Chauhan, A. Temperature Sensitive Contact Lenses for Triggered Ophthalmic Drug Delivery. Biomaterials 2012, 33, 2289–2300. [Google Scholar] [CrossRef]
- Peng, C.-C.; Ben-Shlomo, A.; Mackay, E.O.; Plummer, C.E.; Chauhan, A. Drug Delivery by Contact Lens in Spontaneously Glaucomatous Dogs. Curr. Eye Res. 2012, 37, 204–211. [Google Scholar] [CrossRef]
- Jung, H.J.; Abou-Jaoude, M.; Carbia, B.E.; Plummer, C.; Chauhan, A. Glaucoma Therapy by Extended Release of Timolol from Nanoparticle Loaded Silicone-Hydrogel Contact Lenses. J. Control. Release 2013, 165, 82–89. [Google Scholar] [CrossRef]
- Hsu, K.-H.; Carbia, B.E.; Plummer, C.; Chauhan, A. Dual Drug Delivery from Vitamin E Loaded Contact Lenses for Glaucoma Therapy. Eur. J. Pharm. Biopharm. 2015, 94, 312–321. [Google Scholar] [CrossRef]
- Ciolino, J.B.; Ross, A.E.; Tulsan, R.; Watts, A.C.; Wang, R.-F.; Zurakowski, D.; Serle, J.B.; Kohane, D.S. Latanoprost-Eluting Contact Lenses in Glaucomatous Monkeys. Ophthalmology 2016, 123, 2085–2092. [Google Scholar] [CrossRef]
- Wichterle, O.; Lím, D. Hydrophilic Gels for Biological Use. Nature 1960, 185, 117–118. [Google Scholar] [CrossRef]
- Muntz, A.; Subbaraman, L.N.; Sorbara, L.; Jones, L. Tear Exchange and Contact Lenses: A Review. J. Optom. 2015, 8, 2–11. [Google Scholar] [CrossRef] [PubMed]
- Sedlácek, J. Possibility of the application of ophthalmic drugs with the use of gel contact lenses. Ceskoslovenska Oftalmol. 1965, 21, 509–512. [Google Scholar]
- North, D.P. Treatment of Acute Glaucoma. Can. Med. Assoc. J. 1971, 105, 561. [Google Scholar]
- Uchida, R.; Sato, T.; Tanigawa, H.; Uno, K. Azulene incorporation and release by hydrogel containing methacrylamide propyltrimenthylammonium chloride, and its application to soft contact lens. J. Control. Release 2003, 92, 259–264. [Google Scholar] [CrossRef]
- Lovrec-Krstič, T.; Orthaber, K.; Maver, U.; Sarenac, T. Review of Potential Drug-Eluting Contact Lens Technologies. Materials 2023, 16, 3653. [Google Scholar] [CrossRef]
- Venkatesh, S.; Saha, J.; Pass, S.; Byrne, M. Transport and Structural Analysis of Molecular Imprinted Hydrogels for Controlled Drug Delivery. Eur. J. Pharm. Biopharm. 2008, 69, 852–860. [Google Scholar] [CrossRef]
- Yañez, F.; Martikainen, L.; Braga, M.E.M.; Alvarez-Lorenzo, C.; Concheiro, A.; Duarte, C.M.M.; Gil, M.H.; De Sousa, H.C. Supercritical Fluid-Assisted Preparation of Imprinted Contact Lenses for Drug Delivery. Acta Biomater. 2011, 7, 1019–1030. [Google Scholar] [CrossRef]
- Janagam, D.R.; Wu, L.; Lowe, T.L. Nanoparticles for Drug Delivery to the Anterior Segment of the Eye. Adv. Drug Deliv. Rev. 2017, 122, 31–64. [Google Scholar] [CrossRef]
- Xu, J.; Xue, Y.; Hu, G.; Lin, T.; Gou, J.; Yin, T.; He, H.; Zhang, Y.; Tang, X. A Comprehensive Review on Contact Lens for Ophthalmic Drug Delivery. J. Control. Release 2018, 281, 97–118. [Google Scholar] [CrossRef]
- Wang, M.T.M.; Ganesalingam, K.; Loh, C.S.; Alberquerque, T.; Al-Kanani, S.; Misra, S.L.; Craig, J.P. Compatibility of Phospholipid Liposomal Spray with Silicone Hydrogel Contact Lens Wear. Contact Lens Anterior Eye 2017, 40, 53–58. [Google Scholar] [CrossRef] [PubMed]
- Lim, C.H.L.; Stapleton, F.; Mehta, J.S. Review of Contact Lens–Related Complications. Eye Contact Lens Sci. Clin. Pract. 2018, 44, S1–S10. [Google Scholar] [CrossRef]
- Rouen, P.A.; White, M.L. Dry Eye Disease: Prevalence, Assessment, and Management. Home Healthc. Now 2018, 36, 74–83. [Google Scholar] [CrossRef]
- Stewart, W.C.; Garrison, P.M. β-Blocker–Induced Complications and the Patient With Glaucoma: Newer Treatments to Help Reduce Systemic Adverse Events. Arch. Intern. Med. 1998, 158, 221. [Google Scholar] [CrossRef]
- Raghava, S.; Hammond, M.; Kompella, U.B. Periocular routes for retinal drug delivery. Expert. Opin. Drug Deliv. 2004, 1, 99–114. [Google Scholar] [CrossRef] [PubMed]
- Natarajan, J.V.; Chattopadhyay, S.; Ang, M.; Darwitan, A.; Foo, S.; Zhen, M.; Koo, M.; Wong, T.T.; Venkatraman, S.S. Sustained Release of an Anti-Glaucoma Drug: Demonstration of Efficacy of a Liposomal Formulation in the Rabbit Eye. PLoS ONE 2011, 6, e24513. [Google Scholar] [CrossRef] [PubMed]
- Natarajan, J.V.; Ang, M.; Darwitan, A.; Chattopadhyay, S.; Wong, T.T.; Venkatraman, S.S. Nanomedicine for Glaucoma: Liposomes Provide Sustained Release of Latanoprost in the Eye. Int. J. Nanomed. 2012, 7, 123–131. [Google Scholar] [CrossRef][Green Version]
- Wong, T.T.; Novack, G.D.; Natarajan, J.V.; Ho, C.L.; Htoon, H.M.; Venkatraman, S.S. Nanomedicine for Glaucoma: Sustained Release Latanoprost Offers a New Therapeutic Option with Substantial Benefits over Eyedrops. Drug Deliv. Transl. Res. 2014, 4, 303–309. [Google Scholar] [CrossRef]
- Amrite, A.C.; Ayalasomayajula, S.P.; Cheruvu, N.P.S.; Kompella, U.B. Single Periocular Injection of Celecoxib-PLGA Microparticles Inhibits Diabetes-Induced Elevations in Retinal PGE 2, VEGF, and Vascular Leakage. Investig. Ophthalmol. Vis. Sci. 2006, 47, 1149. [Google Scholar] [CrossRef]
- Amrite, A.C.; Kompella, U.B. Size-Dependent Disposition of Nanoparticles and Microparticles Following Subconjunctival Administration. J. Pharm. Pharmacol. 2010, 57, 1555–1563. [Google Scholar] [CrossRef]
- Nagai, N.; Tsukamoto, A.; Kotake, T.; Ito, Y.; Okamoto, N.; Shimomura, Y. Evaluation of Rabbit Model for Glaucoma Study: Drug Interaction in a Rabbit Model Instilled with Ophthalmic Preparation containing Latanoprost and Timolol. Iryo Yakugaku (Jpn. J. Pharm. Health Care Sci.) 2016, 42, 645–650. [Google Scholar] [CrossRef]
- Gautam, M.; Gupta, R.; Singh, P.; Verma, V.; Verma, S.; Mittal, P.; Karkhur, S.; Sampath, A.; Mohan, R.R.; Sharma, B. Intracameral Drug Delivery: A Review of Agents, Indications, and Outcomes. J. Ocul. Pharmacol. Ther. 2023, 39, 102–116. [Google Scholar] [CrossRef] [PubMed]
- Bacharach, J.; Tatham, A.; Ferguson, G.; Belalcázar, S.; Thieme, H.; Goodkin, M.L.; Chen, M.Y.; Guo, Q.; Liu, J.; Robinson, M.R.; et al. ARTEMIS 2 Study Group. Phase 3, Randomized, 20-Month Study of the Efficacy and Safety of Bimatoprost Implant in Patients with Open-Angle Glaucoma and Ocular Hypertension (ARTEMIS 2). Drugs 2021, 81, 2017–2033. [Google Scholar] [CrossRef] [PubMed]
- Medeiros, F.A.; Walters, T.R.; Kolko, M.; Coote, M.; Bejanian, M.; Goodkin, M.L.; Guo, Q.; Zhang, J.; Robinson, M.R.; Weinreb, R.N.; et al. Phase 3, Randomized, 20-Month Study of Bimatoprost Implant in Open-Angle Glaucoma and Ocular Hypertension (ARTEMIS 1). Ophthalmology 2020, 127, 1627–1641. [Google Scholar] [CrossRef]
- Berdahl, J.P.; Sarkisian, S.R., Jr.; Ang, R.E.; Doan, L.V.; Kothe, A.C.; Usner, D.W.; Katz, L.J.; Navratil, T.; Travoprost Intraocular Implant Study Group. Efficacy and Safety of the Travoprost Intraocular Implant in Reducing Topical IOP-Lowering Medication Burden in Patients with Open-Angle Glaucoma or Ocular Hypertension. Drugs 2024, 84, 83–97. [Google Scholar] [CrossRef]
- Sirinek, P.E.; Lin, M.M. Intracameral Sustained Release Bimatoprost Implants (Durysta). Semin. Ophthalmol. 2022, 37, 385–390. [Google Scholar] [CrossRef]
- Stamer, W.D.; Perkumas, K.M.; Kang, M.H.; Dibas, M.; Robinson, M.R.; Rhee, D.J. Proposed Mechanism of Long-Term Intraocular Pressure Lowering With the Bimatoprost Implant. Investig. Ophthalmol. Vis. Sci. 2023, 64, 15. [Google Scholar] [CrossRef]
- Medeiros, F.A.; Sheybani, A.; Shah, M.M.; Rivas, M.; Bai, Z.; Werts, E.; Ahmed, I.I.K.; Craven, E.R. Single Administration of Intracameral Bimatoprost Implant 10 mg in Patients with Open-Angle Glaucoma or Ocular Hypertension. Ophthalmol. Ther. 2022, 11, 1517–1537. [Google Scholar] [CrossRef]
- Belamkar, A.; Harris, A.; Zukerman, R.; Siesky, B.; Oddone, F.; Verticchio Vercellin, A.; Ciulla, T.A. Sustained release glaucoma therapies: Novel modalities for overcoming key treatment barriers associated with topical medications. Ann. Med. 2022, 54, 343–358. [Google Scholar] [CrossRef]
- Miller, P.E.; Eaton, J.S. Medical Antiglaucoma Therapy: Beyond the Drop. Vet. Ophthalmol. 2021, 24, 2–15. [Google Scholar] [CrossRef]
| Authors | Type of Study | Year | Device | Drugs | Results |
|---|---|---|---|---|---|
| Chen et al. [14] | Case-control study | 2020 | Temporary Collagen Punctal Plugs | A statistically significant IOP diminution in the case group compared with the control group. DED ameliorated significantly in the case group rather than in the control group. | |
| Sherwin et al. [15] | Randomized controlled trial | 2018 | Punctal plugs in patients using prostaglandin analog monotherapy | Punctal plugs resulted in a significantly lowered IOP (MD 1.5 mm Hg, 95% CI 0.1–2.9, p = 0.032). | |
| Perera et al. [16] | Initial feasibility, prospective, single-arm | 2016 | OTX-TP | Travoprost | OTX-TP can reduce IOP by 24% (day 10) and 15.6% (day 30). |
| Kompella et al. [17] | Phase 2 trial | 2010 | L-PPDS | Latanoprost | A mean reduction in IOP by 3.5 mm Hg at the end of 4 weeks, with 36% of patients showing a decrease in IOP of more than 5 mm Hg. |
| Authors | Type of Study | Year | Device | Drugs | Results |
|---|---|---|---|---|---|
| Alza Corporation [27] | Phase 3 trial, randomized, multicenter, masked (previously on the market) | 1975 | Pilocarpine Ocusert | Conjunctival fornix delivery system, pilocarpine | Positive outcomes in IOP lowering but also many side effects. Withdrawn from the market in 1993. |
| James D. Brandt et al. [28] | Double-masked, randomized, multicenter, phase 2 study | 2016 | Topical Bimatoprost Ocular Insert | Conjunctival fornix delivery system, Bimatoprost | Bimatoprost Ocular Ring did not reach the non-inferiority standard in lowering IOP compared with timolol eye drops. |
| James D. Brandt et al. [29] | A 13-month open-label extension (OLE) study | 2017 | Topical Bimatoprost Ocular Insert | Conjunctival fornix delivery system, Bimatoprost | A median reduction of 4 mm Hg was reached over a follow-up period of 19 months. |
| Nair et al. [30] | Preclinical study | 2018 | Timolol maleate-loaded inserts | Conjunctival fornix delivery system, timolol | Faster response and longer persistence of the drug in timolol maleate-loaded inserts compared with timolol maleate drop solution. |
| Kelly et al. [31] | Single-dose crossover study | 1989 | New Ophthalmic Delivery System (NODS) | Conjunctival fornix delivery system, pilocarpine | The bioavailability of NODS is eight times greater compared with conventional eye drops. |
| Greaves et al. [32] | Gamma scintigraphic study on 12 volunteers | 1992 | Radiolabeled New Ophthalmic Delivery System (NODS) loaded with pilocarpine nitrate | Conjunctival fornix delivery system, pilocarpine | IOP-lowering; more significant pupil diameter reduction and higher bioavailability compared with a 25 µL drop of 2% pilocarpine nitrate solution. |
| M. Diestelhorst [33] | Open-label, crossover study | 1994 | Radiolabeled New Ophthalmic Delivery System (NODS) | Conjunctival fornix delivery system | NODS were less tolerated than conventional eye drops. |
| Bigdeli et al. [34] | In vivo (rabbits) | 2023 | Timolol Maleate-Brimonidine tartrate-loaded liposomes | Both liposomal and aqueous formulations reduce IOP, although liposomal formulation is more efficient (rabbits). |
| Authors | Type of Study | Year | Device | Drugs | Results |
|---|---|---|---|---|---|
| Hiratami and Alvarez-Lorenzo [42] | Preclinical trial | 2002 | Soft contact lenses of a cross-linked hydrogel loaded with molecular imprinting method | Timolol | This method improves the drug loading capacity and prolongs timolol release for more than 24 h |
| Kim et al. [43] | Preclinical trial | 2007 | Soaked silicone hydrogel soft contact lenses | Timolol | This method increases drug release for about 15–20 days |
| Peng et al. [44] | Preclinical trial (animal model) | 2012 | Silicone hydrogel contact lenses loaded with vitamin E | Timolol | This method increases the bioavailability of the drug and reduces systemic drug uptake |
| Braga et al. [45] | Preclinical trial | 2011 | Drug loaded into commercial soft contact lenses with a supercritical solvent impregnation process | Acetazolamide | With this method, it is possible to control acetazolamide-loaded amounts and adjust the drug release levels |
| Jung and Chauhan [46] | Preclinical trial | 2012 | Drug encapsulating highly cross-linked nanoparticles in contact lenses | Timolol | This method increases the duration of drug release to 2–4 weeks |
| Peng et al. [47] | Preclinical trial (animal model) | 2012 | Commercial soft contact lenses incorporating vitamin E | Timolol | This method increases the drug release duration and lowers the IOP by continuously wearing |
| Jung et al. [48] | Preclinical trial (animal model) | 2013 | Nanoparticle-loaded contact lenses | Timolol | This method allows a constant reduction in IOP |
| Hsu et al. [49] | Preclinical trial (animal model) | 2015 | Vitamin E-loaded contact lenses | Timolol and Dorzolamide | This method ensures prolonged release of the drug and further reduces IOP |
| Ciolino et al. [50] | Preclinical trial (animal model) | 2016 | Contact lenses with a drug-polymer film | Latanoprost | This method is effective as delivery with daily Latanoprost ophthalmic solution |
| Authors | Type of Study | Year | Device | Drugs | Results |
|---|---|---|---|---|---|
| Wong et al. [66] | In vivo (rabbits) | 2014 | Subconjunctival Latanoprost injection | More significant IOP reduction than Latanoprost eye drops for about 80 days (2 injections-day one and day 50) (rabbits). | |
| Wong et al. [67] | In vivo (rabbits) | 2012 | Latanoprost-loaded EggPC liposomes | A single injection of these liposomes lowers the IOP for up to 90 days, a more significant IOP reduction than Latanoprost eye drops (rabbits). | |
| Wong et al. [68] | Open-label, non-comparative study | 2014 | Latanoprost-loaded nanoliposome | A single injection decreased IOP immediately in all six subjects; after three months, IOP was lower than baseline in all subjects except one (humans). | |
| Kesav et al. [9] | Phase 1/2a clinical trial, multicenter | 2017 | Eye-D VD-101 insert | Latanoprost-releasing subconjunctival insert | The implant reduces IOP by 24% from baseline at 12 weeks. Non-inferior to Latanoprost eye drops (humans). |
| Kesav et al. [9] | In vivo (rabbits) | 2018 | GB-401 injection | Beta adrenergic prodrug subconjunctival injection | The implant reduces IOP within the first week and up to 20% from baseline at 2 months (rabbits). |
| Authors | Type of Study | Year | Device | Drugs | Results |
|---|---|---|---|---|---|
| J. Bacharach et al. [73] | Phase 3 trial, randomized, multicenter, masked | 2021 | Durysta | Intracameral sustained released Bimatoprost | BimSR 10 μg and 15 μg were non-inferior in lowering IOP to timolol eye drops. |
| F.A. Medeiros et al. [74] | Phase 3 trial, randomized, multicenter, masked | 2020 | Durysta | Intracameral sustained released Bimatoprost | BimSR 10 μg and 15 μg were non-inferior in lowering IOP to timolol eye drops. |
| John P. Berdahl [75] | Phase 2 trial, randomized, multicenter, masked | 2023 | Idose | Intracameral sustained released travoprost | The fast-release and slow-release formulations were non-inferior in lowering IOP to timolol eye drops. |
| Courtesy of the producer | Phase 2 trial, randomized, multicenter, masked | ENV515 | Intracameral sustained released travoprost | ENV515 was non-inferior to topical travoprost on day 25 and to topical timolol 0.5% on the 11th month. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fea, A.M.; Vallino, V.; Cossu, M.; Marica, V.; Novarese, C.; Reibaldi, M.; Petrillo, F. Drug Delivery Systems for Glaucoma: A Narrative Review. Pharmaceuticals 2024, 17, 1163. https://doi.org/10.3390/ph17091163
Fea AM, Vallino V, Cossu M, Marica V, Novarese C, Reibaldi M, Petrillo F. Drug Delivery Systems for Glaucoma: A Narrative Review. Pharmaceuticals. 2024; 17(9):1163. https://doi.org/10.3390/ph17091163
Chicago/Turabian StyleFea, Antonio M., Veronica Vallino, Michela Cossu, Valentina Marica, Cristina Novarese, Michele Reibaldi, and Francesco Petrillo. 2024. "Drug Delivery Systems for Glaucoma: A Narrative Review" Pharmaceuticals 17, no. 9: 1163. https://doi.org/10.3390/ph17091163
APA StyleFea, A. M., Vallino, V., Cossu, M., Marica, V., Novarese, C., Reibaldi, M., & Petrillo, F. (2024). Drug Delivery Systems for Glaucoma: A Narrative Review. Pharmaceuticals, 17(9), 1163. https://doi.org/10.3390/ph17091163








