Gabapentin-Induced Adrenal Insufficiency: The Hypothalamic-Pituitary-Adrenal Axis Stress Misresponse and Risk of Infection: A Case Report and Literature Review
Abstract
1. Introduction
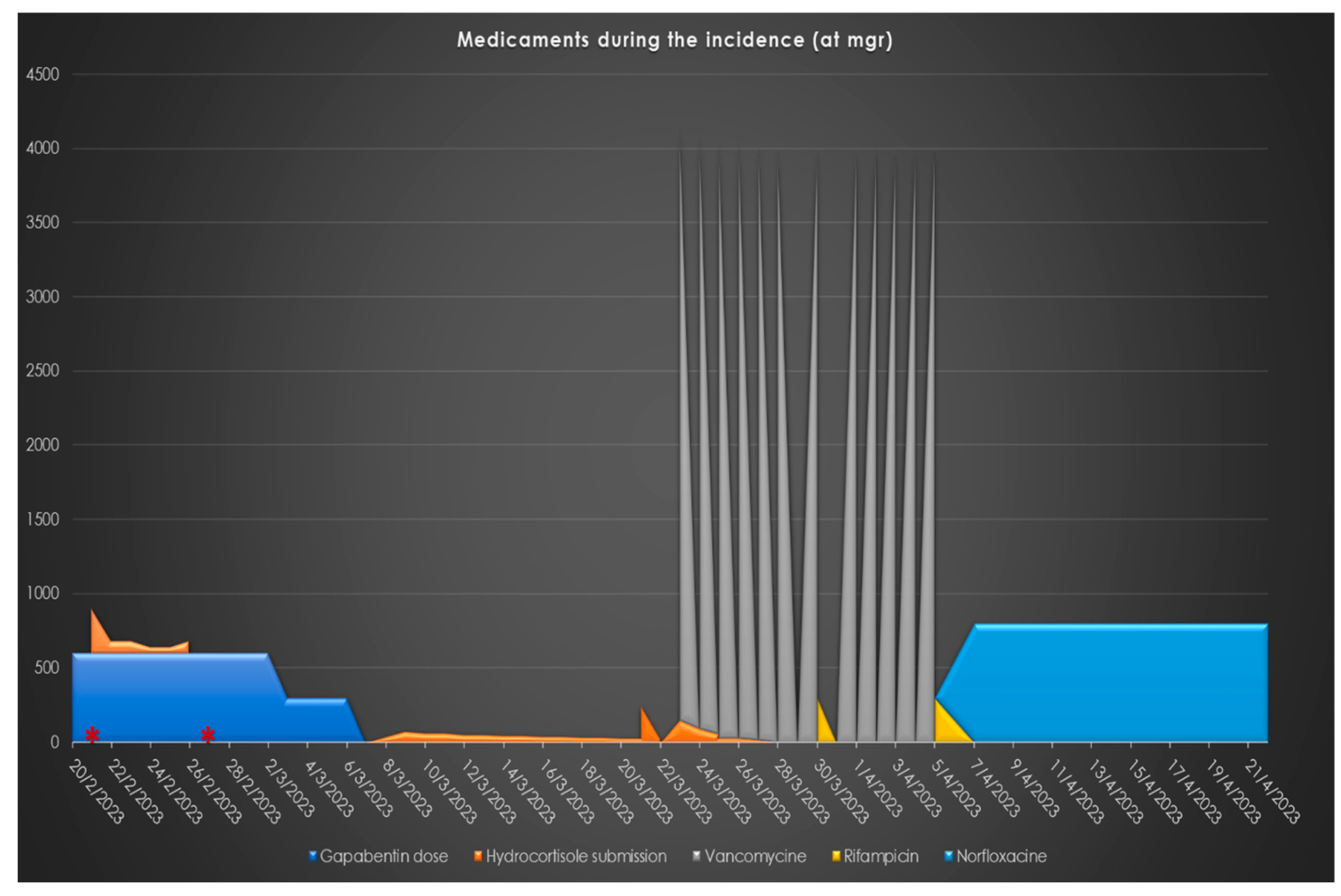
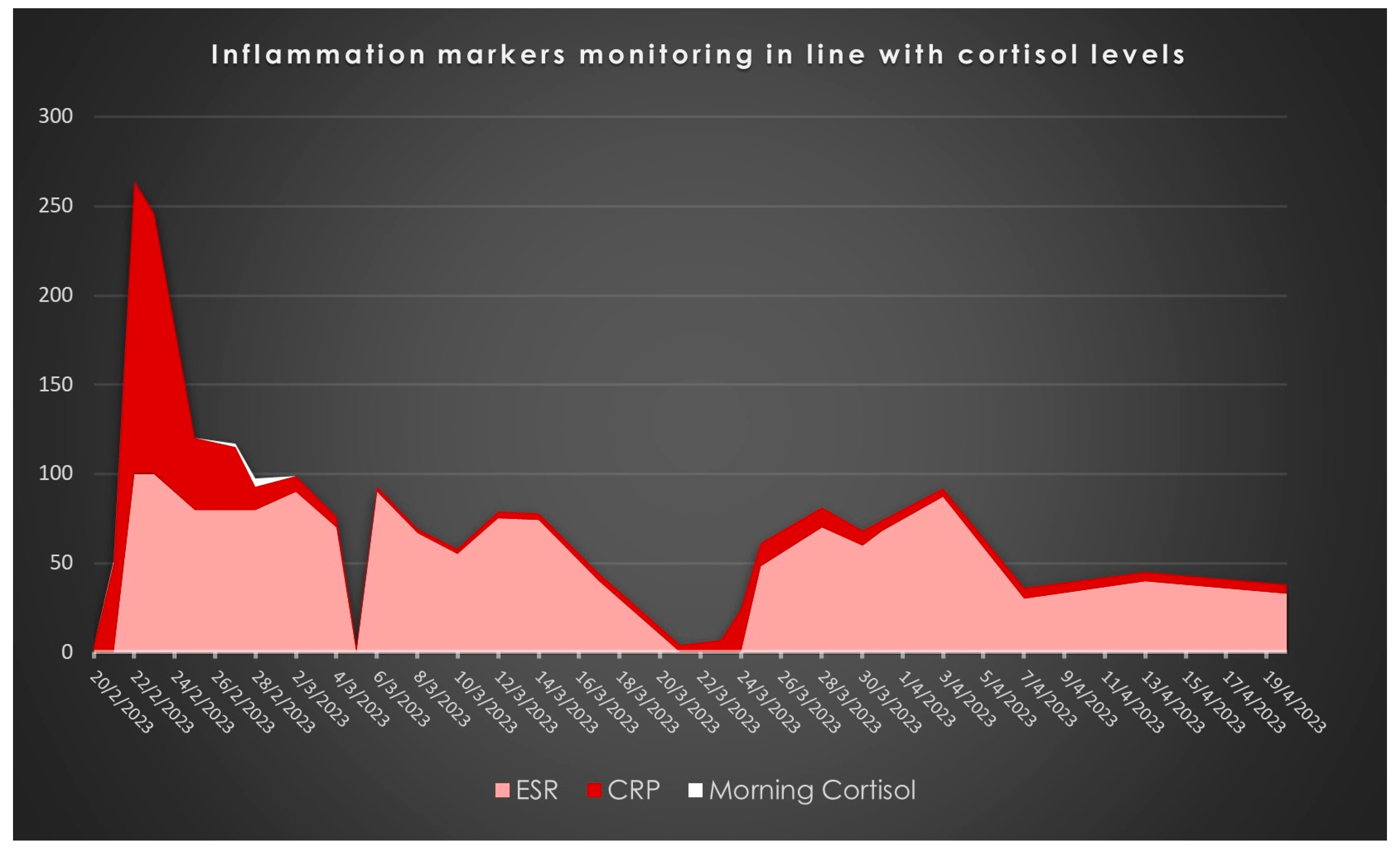
2. Case Report
3. Review
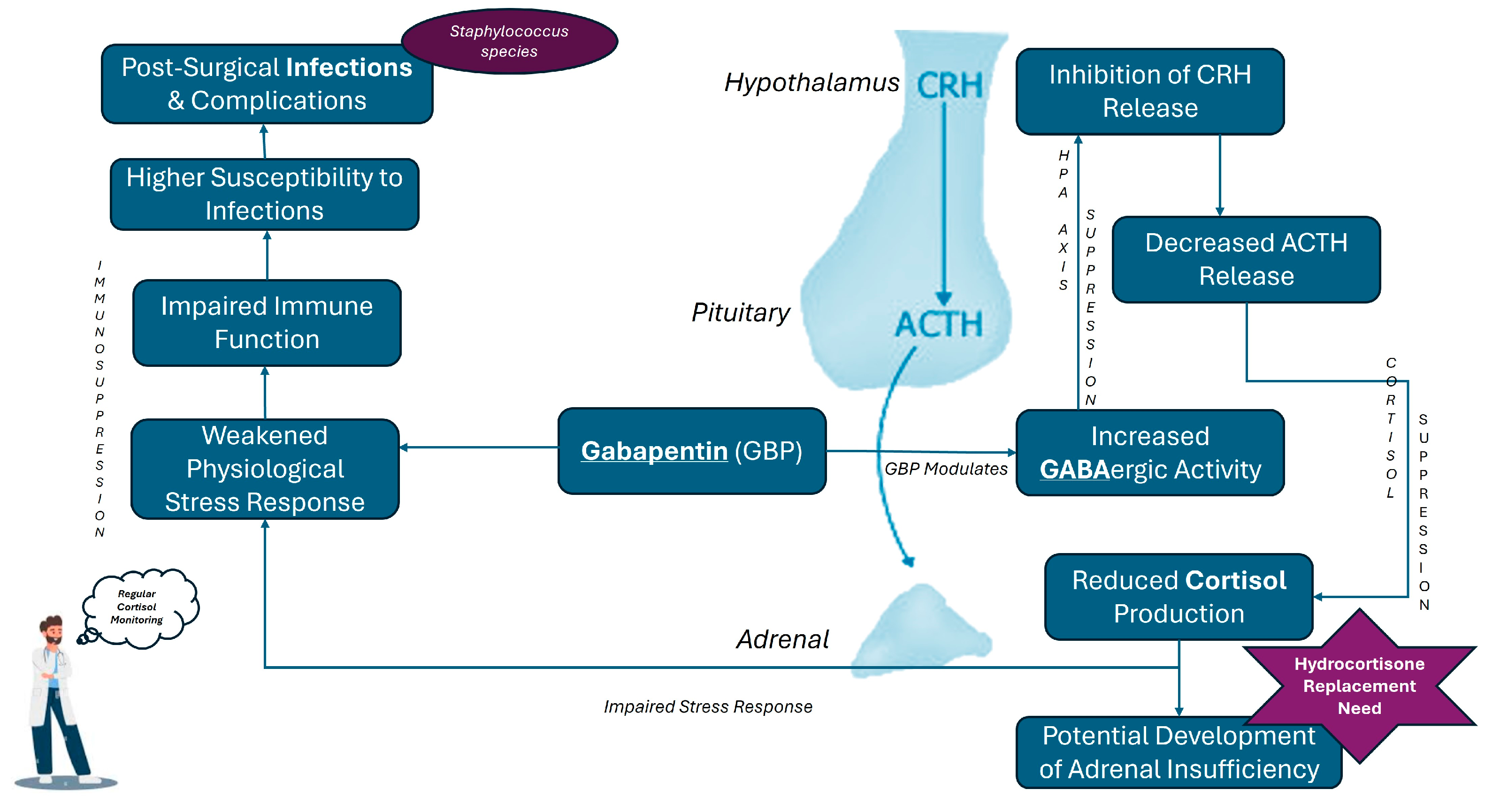
3.1. Gabapentin’s Pharmacological Profile, the HPA Axis and Stress Response
3.2. Gabapentin and Cortisol Levels in Clinical Settings
3.3. Clinical Implications of Gabapentin-Induced Adrenal Insufficiency
3.4. Gabapentin-Induced Hypocortisolemia and Infection Risk
4. Conclusions
- Complex Interplay: The review and case report highlight the intricate relationship between GBP use, adrenal insufficiency, and increased infection risk, particularly in patients undergoing major surgeries. It is also highlighting the principles of adverse effects management as the patients were not monitored for HPA axis and the hypocortisolemia founded during basic routine pre- or post-operative tests. It emphasizes the need for always careful and deep clinical brainstorming when patients with a controversial history suddenly present irregularities in vital axes, such as the glucocorticoids’ axis.
- HPA Axis and Cortisol Regulation: The findings underscore the significance of understanding GBP’s diverse effects on the hypothalamic–pituitary–adrenal (HPA) axis and cortisol regulation.
- Need for Vigilant Monitoring: There is a crucial need to carefully monitor patients receiving GBP, especially in perioperative settings, to mitigate potential risks.
- Future Research: Further research is necessary to clarify the mechanisms behind GBP’s impact on the HPA axis and to develop evidence-based guidelines for managing these cases.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hayes, W.J.; Ferdinand, A.; Neabore, S.; Kappes, J.A.; Hayes, K.M.; Berendse, J. Patient Case Report: Gabapentin-Induced Hypoglycemia. J. Pharm. Pract. 2022, 35, 298–301. [Google Scholar] [CrossRef]
- Product Information. Neurontin(R) Oral Capsules, Tablets, Solution, Gabapentin Oral Capsules, Tablets, Solution; Food and Drug Administration: Silver Spring, MD, 2010.
- Taylor, C.P. Mechanisms of action of gabapentin. Rev. Neurol. 1997, 153 (Suppl. S1), S39–S45. [Google Scholar]
- Taylor, C.P.; Gee, N.S.; Su, T.Z.; Kocsis, J.D.; Welty, D.F.; Brown, J.P.; Dooley, D.J.; Boden, P.; Singh, L. A summary of mechanistic hypotheses of gabapentin pharmacology. Epilepsy Res. 1998, 29, 233–249. [Google Scholar] [CrossRef] [PubMed]
- Gurba, K.N.; Chaudhry, R.; Haroutounian, S. Central Neuropathic Pain Syndromes: Current and Emerging Pharmacological Strategies. CNS Drugs 2022, 36, 483–516. [Google Scholar] [CrossRef] [PubMed]
- Cullinan, W.E.; Ziegler, D.R.; Herman, J.P. Functional role of local GABAergic influences on the HPA axis. Brain Struct. Funct. 2008, 213, 63–72. [Google Scholar] [CrossRef] [PubMed]
- Maguire, J. The relationship between GABA and stress: ‘it’s complicated’. J. Physiol. 2018, 596, 1781–1782. [Google Scholar] [CrossRef] [PubMed]
- Maguire, J.; Mody, I. GABA(A)R plasticity during pregnancy: Relevance to postpartum depression. Neuron 2008, 59, 207–213. [Google Scholar] [CrossRef]
- Douglass, A.M.; Resch, J.M.; Madara, J.C.; Kucukdereli, H.; Yizhar, O.; Grama, A.; Yamagata, M.; Yang, Z.; Lowell, B.B. Neural basis for fasting activation of the hypothalamic-pituitary-adrenal axis. Nature 2023, 620, 154–162. [Google Scholar] [CrossRef]
- Camille Melon, L.; Maguire, J. GABAergic regulation of the HPA and HPG axes and the impact of stress on reproductive function. J. Steroid Biochem. Mol. Biol. 2016, 160, 196–203. [Google Scholar] [CrossRef]
- Alam, W.R.; Srinivasan. Gabapentin induced low cortisol. Presented at the Society for Endocrinology BES 2017, Harrogate, UK, 6–8 November 2017; Endocrine Abstracts 50 PL1 2022.
- Karbić, V.O.; Skoda, M.; Antoncic, D.; Kristofic, I.; Komar, D.; Trobonjaca, Z. Gabapentin-induced changes of plasma cortisol level and immune status in hysterectomized women. Int. Immunopharmacol. 2014, 23, 530–536. [Google Scholar] [CrossRef]
- Kong, V.K.; Irwin, M.G. Gabapentin: A multimodal perioperative drug? Br. J. Anaesth. 2007, 99, 775–786. [Google Scholar] [CrossRef] [PubMed]
- Panah Khahi, M.; Marashi, S.; Khajavi, M.R.; Najafi, A.; Yaghooti, A.; Imani, F. Postoperative gabapentin to prevent postoperative pain: A randomized clinical trial. Anesthesiol. Pain Med. 2012, 2, 77–80. [Google Scholar] [CrossRef] [PubMed]
- Smeland, S.; Bielack, S.S.; Whelan, J.; Bernstein, M.; Hogendoorn, P.; Krailo, M.D.; Gorlick, R.; Janeway, K.A.; Ingleby, F.C.; Anninga, J.; et al. Survival and prognosis with osteosarcoma: Outcomes in more than 2000 patients in the EURAMOS-1 (European and American Osteosarcoma Study) cohort. Eur. J. Cancer 2019, 109, 36–50. [Google Scholar] [CrossRef]
- Takeuchi, A.; Yamamoto, N.; Hayashi, K.; Matsubara, H.; Miwa, S.; Igarashi, K.; Tsuchiya, H. Joint-preservation surgery for pediatric osteosarcoma of the knee joint. Cancer Metastasis Rev. 2019, 38, 709–722. [Google Scholar] [CrossRef]
- Bockbrader, H.N.; Wesche, D.; Miller, R.; Chapel, S.; Janiczek, N.; Burger, P. A comparison of the pharmacokinetics and pharmacodynamics of pregabalin and gabapentin. Clin. Pharmacokinet. 2010, 49, 661–669. [Google Scholar] [CrossRef]
- Chen, L.; Xu, M.; Zhou, J. Gabapentin regulates expression of corticotropin-releasing hormone in the hypothalamus through the μ-opioid receptor and ERK signaling pathway. Acta Biochim. Biophys. Sin. 2018, 50, 1257–1263. [Google Scholar]
- Taylor, C.P. Mechanisms of analgesia by gabapentin and pregabalin--calcium channel alpha2-delta [Cavalpha2-delta] ligands. Pain 2009, 142, 13–16. [Google Scholar] [CrossRef] [PubMed]
- Baram, T.Z.; Hatalski, C.G. Neuropeptide-mediated excitability: A key triggering mechanism for seizure generation in the developing brain. Trends Neurosci. 1998, 21, 471–476. [Google Scholar] [CrossRef]
- Johannessen Landmark, C.; Henning, O.; Johannessen, S.I. Proconvulsant effects of antidepressants—What is the current evidence? Epilepsy Behav. 2016, 61, 287–291. [Google Scholar] [CrossRef]
- Herman, J.P.; McKlveen, J.M.; Ghosal, S.; Kopp, B.; Wulsin, A.; Makinson, R.; Scheimann, J.; Myers, B. Regulation of the Hypothalamic-Pituitary-Adrenocortical Stress Response. Compr. Physiol. 2016, 6, 603–621. [Google Scholar] [CrossRef]
- Van Bockstaele, E.J.; Valentino, R.J. Neuropeptide regulation of the locus coeruleus and opiate-induced plasticity of stress responses. Adv. Pharmacol. 2013, 68, 405–420. [Google Scholar] [CrossRef] [PubMed]
- Theophilus, S.C.N.R.; Abrams, R.; Silverman, D.G.; Silverman, D.G. Perioperative gabapentin and postoperative pain: A systematic review. Anesth. Analg. 2009, 108, 682–687. [Google Scholar]
- Ho, K.Y.; Gan, T.J.; Habib, A.S. Gabapentin and postoperative pain--a systematic review of randomized controlled trials. Pain 2006, 126, 91–101. [Google Scholar] [CrossRef] [PubMed]
- Finnerty, C.C.; Mabvuure, N.T.; Ali, A.; Kozar, R.A.; Herndon, D.N. The surgically induced stress response. JPEN J. Parenter. Enteral Nutr. 2013, 37, 21S–29S. [Google Scholar] [CrossRef] [PubMed]
- Prete, A.; Yan, Q.; Al-Tarrah, K.; Akturk, H.K.; Prokop, L.J.; Alahdab, F.; Foster, M.A.; Lord, J.M.; Karavitaki, N.; Wass, J.A.; et al. The cortisol stress response induced by surgery: A systematic review and meta-analysis. Clin. Endocrinol. 2018, 89, 554–567. [Google Scholar] [CrossRef] [PubMed]
- Hudec, C.P.; Griffin, C.E. Changes in the stress markers cortisol and glucose before and during intradermal testing in cats after single administration of pre-appointment gabapentin. J. Feline Med. Surg. 2020, 22, 138–145. [Google Scholar] [CrossRef]
- Gilron, I.; Bailey, J.M.; Tu, D.; Holden, R.R.; Jackson, A.C.; Houlden, R.L. Nortriptyline and gabapentin, alone and in combination for neuropathic pain: A double-blind, randomised controlled crossover trial. Lancet 2009, 374, 1252–1261. [Google Scholar] [CrossRef]
- Tiippana, E.M.; Hamunen, K.; Kontinen, V.K.; Kalso, E. Do surgical patients benefit from perioperative gabapentin/pregabalin? A systematic review of efficacy and safety. Anesth. Analg. 2007, 104, 1545–1556. [Google Scholar] [CrossRef]
- Fareau, G.G.; Vassilopoulou-Sellin, R. Hypercortisolemia and infection. Infect. Dis. Clin. N. Am. 2007, 21, 639–657. [Google Scholar] [CrossRef]
- Cain, D.W.; Cidlowski, J.A. Immune regulation by glucocorticoids. Nat. Rev. Immunol. 2017, 17, 233–247. [Google Scholar] [CrossRef]
- Brand, Y.E.; Rufer, B. Late prosthetic knee joint infection with Staphylococcus xylosus. IDCases 2021, 24, e01160. [Google Scholar] [CrossRef] [PubMed]
- Scorzolini, L.; Lichtner, M.; Iannetta, M.; Mengoni, F.; Russo, G.; Panni, A.S.; Vasso, M.; Bove, M.; Villani, C.; Mastroianni, C.M.; et al. Sonication technique improves microbiological diagnosis in patients treated with antibiotics before surgery for prosthetic joint infections. New Microbiol. 2014, 37, 321–328. [Google Scholar] [PubMed]
- Dordet-Frisoni, E.; Dorchies, G.; De Araujo, C.; Talon, R.; Leroy, S. Genomic diversity in Staphylococcus xylosus. Appl. Environ. Microbiol. 2007, 73, 7199–7209. [Google Scholar] [CrossRef]
- Leroy, S.; Lebert, I.; Andant, C.; Talon, R. Interaction in dual species biofilms between Staphylococcus xylosus and Staphylococcus aureus. Int. J. Food Microbiol. 2020, 326, 108–653. [Google Scholar] [CrossRef] [PubMed]

| Study/Case Report | Patient Characteristics | Medical Condition | GBP Dosage | Effect on Cortisol Levels | Other Findings |
|---|---|---|---|---|---|
| Karbić et al. (2014) [12] | 60 women, undergoing hysterectomy | Abdominal Hysterectomy | 600 mg, 1 h pre-surgery | Significant reduction 24 h post-op | Reduced catecholamines (epinephrine, norepinephrine), mitigated surgical stress |
| Hudec and Griffin (2020) [28] | Veterinary context (cats) | Pre-appointment stress | 25.0–30.5 mg/kg | Slight, non-significant reduction | Suggests effects may be due to sedative properties rather than direct HPA axis suppression |
| Alam and Srinivasan (2017) [11] | 56-year-old male, post-knee replacement | Total Knee Replacement | 100 mg 3 times per day | Significantly low on days 1 and 4 post-op | Normal adrenal response to Short Synacthen Test, indicating stress response suppression without adrenal insufficiency |
| Current Case (2024) | 17-year-old boy with osteosarcoma | Megaprostheses placement revision surgeries | 300 mg twice daily before revision surgery, tapered to 300 mg once daily before discontinuation | Morning cortisol levels dropped to 1.18 μg/dL, below normal range, necessitating hydrocortisone replacement therapy | Developed transient adrenal insufficiency, requiring multiple interventions; GBP administration associated with suppressed cortisol levels and complex clinical management |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pechlivanidou, E.; Chatzikyriakos, A.; Zisi, M.A.; Paraskevopoulos, N.; Kaltsa, S.; Konstantas, O.K.; Zogakis, P.; Catsouli, A.; Sekouris, N.; Margariti, R.E. Gabapentin-Induced Adrenal Insufficiency: The Hypothalamic-Pituitary-Adrenal Axis Stress Misresponse and Risk of Infection: A Case Report and Literature Review. Pharmaceuticals 2024, 17, 1174. https://doi.org/10.3390/ph17091174
Pechlivanidou E, Chatzikyriakos A, Zisi MA, Paraskevopoulos N, Kaltsa S, Konstantas OK, Zogakis P, Catsouli A, Sekouris N, Margariti RE. Gabapentin-Induced Adrenal Insufficiency: The Hypothalamic-Pituitary-Adrenal Axis Stress Misresponse and Risk of Infection: A Case Report and Literature Review. Pharmaceuticals. 2024; 17(9):1174. https://doi.org/10.3390/ph17091174
Chicago/Turabian StylePechlivanidou, Evmorfia, Alexandros Chatzikyriakos, Maria Anna Zisi, Nikolaos Paraskevopoulos, Semeli Kaltsa, Orestis K. Konstantas, Panteleimon Zogakis, Aikaterini Catsouli, Nick Sekouris, and Rodanthi E. Margariti. 2024. "Gabapentin-Induced Adrenal Insufficiency: The Hypothalamic-Pituitary-Adrenal Axis Stress Misresponse and Risk of Infection: A Case Report and Literature Review" Pharmaceuticals 17, no. 9: 1174. https://doi.org/10.3390/ph17091174
APA StylePechlivanidou, E., Chatzikyriakos, A., Zisi, M. A., Paraskevopoulos, N., Kaltsa, S., Konstantas, O. K., Zogakis, P., Catsouli, A., Sekouris, N., & Margariti, R. E. (2024). Gabapentin-Induced Adrenal Insufficiency: The Hypothalamic-Pituitary-Adrenal Axis Stress Misresponse and Risk of Infection: A Case Report and Literature Review. Pharmaceuticals, 17(9), 1174. https://doi.org/10.3390/ph17091174






