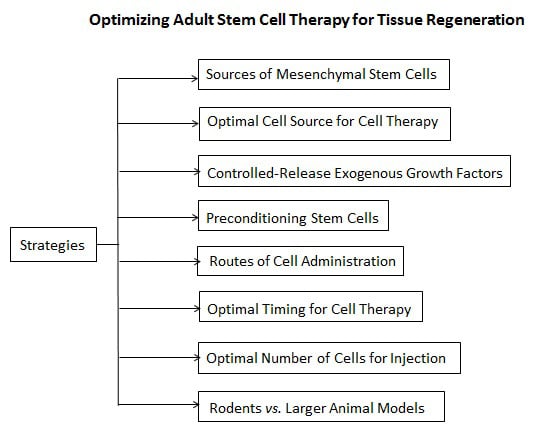
Strategies to Optimize Adult Stem Cell Therapy for Tissue Regeneration
Abstract
:1. Introduction
2. Sources of MSCs
3. Optimal Cell Source for Cell Therapy
3.1. Combinations of Somatic and Stem Cells
3.2. Primary Cultured Cells vs. Cell Lines
3.3. Passages of Stem Cells Used for Implantation
3.4. Non-Induced Differentiation of Stem Cells vs. Induced Differentiation of Stem Cells in Tissue Repair
4. Controlled-Release Exogenous Growth Factors
5. Preconditioning Stem Cells
6. Routes of Cell Administration
6.1. Systemic Administration of Stem Cells
6.2. Local Administration of Stem Cells
7. Optimal Timing for Cell Therapy
8. Optimal Number of Cells for Injection
9. Rodents vs. Larger Animal Models
10. Future Directions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Nauta, A.J.; Fibbe, W.E. Immunomodulatory properties of mesenchymal stromal cells. Blood 2007, 110, 3499–3506. [Google Scholar] [CrossRef] [PubMed]
- Trounson, A.; Thakar, R.G.; Lomax, G.; Gibbons, D. Clinical trials for stem cell therapies. BMC Med. 2011, 9, 52. [Google Scholar] [CrossRef] [PubMed]
- Lv, F.J.; Tuan, R.S.; Cheung, K.M.; Leung, V.Y. Concise review: The surface markers and identity of human mesenchymal stem cells. Stem Cells 2014, 32, 1408–1419. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Jacot, J.G. Stem cells and progenitor cells for tissue-engineered solutions to congenital heart defects. Biomark. Insights 2015, 10, 139–146. [Google Scholar] [PubMed]
- Fauza, D.O. Tissue engineering in congenital diaphragmatic hernia. Semin. Pediatr. Surg. 2014, 23, 135–140. [Google Scholar] [CrossRef] [PubMed]
- Wang, A.; Brown, E.G.; Lankford, L.; Keller, B.A.; Pivetti, C.D.; Sitkin, N.A.; Beattie, M.S.; Bresnahan, J.C.; Farmer, D.L. Placental mesenchymal stromal cells rescue ambulation in ovine myelomeningocele. Stem Cells Trans. Med. 2015, 4, 659–669. [Google Scholar] [CrossRef] [PubMed]
- Guijarro, D.; Lebrin, M.; Lairez, O.; Bourin, P.; Piriou, N.; Pozzo, J.; Lande, G.; Berry, M.; le Tourneau, T.; Cussac, D.; et al. Intramyocardial transplantation of mesenchymal stromal cells for chronic myocardial ischemia and impaired left ventricular function: Results of the MESAMI 1 pilot trial. Int. J. Cardiol. 2016, 209, 258–265. [Google Scholar] [CrossRef] [PubMed]
- Dasari, V.R.; Veeravalli, K.K.; Dinh, D.H. Mesenchymal stem cells in the treatment of spinal cord injuries: A review. World J. Stem Cells 2014, 6, 120–133. [Google Scholar] [CrossRef] [PubMed]
- Jiang, M.H.; Li, G.; Liu, J.; Liu, L.; Wu, B.; Huang, W.; He, W.; Deng, C.; Wang, D.; Li, C.; et al. Nestin+ kidney resident mesenchymal stem cells for the treatment of acute kidney ischemia injury. Biomaterials 2015, 50, 56–66. [Google Scholar] [CrossRef] [PubMed]
- Thakkar, U.G.; Trivedi, H.L.; Vanikar, A.V.; Dave, S.D. Insulin-secreting adipose-derived mesenchymal stromal cells with bone marrow-derived hematopoietic stem cells from autologous and allogenic sources for type 1 diabetes mellitus. Cytotherapy 2015, 17, 940–947. [Google Scholar] [CrossRef] [PubMed]
- De Bari, C. Are mesenchymal stem cells in rheumatoid arthritis the good or bad guys? Arthritis Res. Ther. 2015, 17, 113. [Google Scholar] [CrossRef] [PubMed]
- Gharibi, T.; Ahmadi, M.; Seyfizadeh, N.; Jadidi-Niaragh, F.; Yousefi, M. Immunomodulatory characteristics of mesenchymal stem cells and their role in the treatment of multiple sclerosis. Cell. Immunol. 2015, 293, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Marfia, G.; Campanella, R.; Navone, S.E.; Zucca, I.; Scotti, A.; Figini, M.; di Vito, C.; Alessandri, G.; Riboni, L.; Parati, E. Potential use of human adipose mesenchymal stromal cells for intervertebral disc regeneration: A preliminary study on biglycan-deficient murine model of chronic disc degeneration. Arthritis Res. Ther. 2014, 16, 457. [Google Scholar] [CrossRef] [PubMed]
- Parmar, N.; Ahmadi, R.; Day, R.M. A novel method for differentiation of human mesenchymal stem cells into smooth muscle-like cells on clinically deliverable thermally induced phase separation microspheres. Tissue Eng. Part C Methods 2015, 21, 404–412. [Google Scholar] [CrossRef] [PubMed]
- Choi, M.Y.; Yeo, S.W.; Park, K.H. Hearing restoration in a deaf animal model with intravenous transplantation of mesenchymal stem cells derived from human umbilical cord blood. Biochem. Biophys. Res. Commun. 2012, 427, 629–636. [Google Scholar] [CrossRef] [PubMed]
- Crisan, M.; Yap, S.; Casteilla, L.; Chen, C.W.; Corselli, M.; Park, T.S.; Andriolo, G.; Sun, B.; Zheng, B.; Zhang, L.; et al. A perivascular origin for mesenchymal stem cells in multiple human organs. Cell Stem Cell 2008, 3, 301–313. [Google Scholar] [CrossRef] [PubMed]
- Wexler, S.A.; Donaldson, C.; Denning-Kendall, P.; Rice, C.; Bradley, B.; Hows, J.M. Adult bone marrow is a rich source of human mesenchymal ‘stem’ cells but umbilical cord and mobilized adult blood are not. Br. J. Haematol. 2003, 121, 368–374. [Google Scholar] [CrossRef] [PubMed]
- Zuk, P.A.; Zhu, M.; de Ugarte, D.A.; Huang, J.I.; Mizuno, H.; Alfonso, Z.C.; Fraser, J.K.; Benhaim, P.; Hedrick, M.H. Human adipose tissue is a source of multipotent stem cells. Mol. Biol. Cell 2002, 13, 4279–4295. [Google Scholar] [CrossRef] [PubMed]
- Pierdomenico, L.; Calvitti, M.; Rondelli, D.; Arpinati, M.; Chirumbolo, G.; Becchetti, E.; Marchionni, C.; Alviano, F.; Fossati, V.; Staffolani, N.; et al. Multipotent mesenchymal stem cells with immunosuppressive activity can be easily isolated from dental pulp. Transplantation 2005, 80, 836–842. [Google Scholar] [CrossRef] [PubMed]
- Murata, D.; Miyakoshi, D.; Hatazoe, T.; Miura, N.; Tokunaga, S.; Fujiki, M.; Nakayama, K.; Misumi, K. Multipotency of equine mesenchymal stem cells derived from synovial fluid. Vet. J. 2014, 202, 53–61. [Google Scholar] [CrossRef] [PubMed]
- Nomura, Y.; Ishikawa, M.; Yashiro, Y.; Sanggarnjanavanich, S.; Yamaguchi, T.; Arai, C.; Noda, K.; Takano, Y.; Nakamura, Y.; Hanada, N. Human periodontal ligament fibroblasts are the optimal cell source for induced pluripotent stem cells. Histochem. Cell Biol. 2012, 137, 719–732. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Liu, J.; Tan, X.; Li, G.; Gao, Y.; Liu, X.; Zhang, L.; Li, Y. Induced pluripotent stem cells from human hair follicle mesenchymal stem cells. Stem Cell Rev. 2013, 9, 451–560. [Google Scholar] [CrossRef] [PubMed]
- Mutlu, L.; Hufnagel, D.; Taylor, H.S. The endometrium as a source of mesenchymal stem cells for regenerative medicine. Biol. Reprod. 2015, 92, 138. [Google Scholar] [CrossRef] [PubMed]
- Hu, C.; Cao, H.; Pan, X.; Li, J.; He, J.; Pan, Q.; Xin, J.; Yu, X.; Wang, Y.; Zhu, D.; et al. Adipogenic placenta-derived mesenchymal stem cells are not lineage restricted by withdrawing extrinsic factors: Developing a novel visual angle in stem cell biology. Cell Death Dis. 2016, 7, e2141. [Google Scholar] [CrossRef] [PubMed]
- Capelli, C.; Gotti, E.; Morigi, M.; Rota, C.; Weng, L.; Dazzi, F.; Spinelli, O.; Cazzaniga, G.; Trezzi, R.; Gianatti, A.; et al. Minimally manipulated whole human umbilical cord is a rich source of clinical-grade human mesenchymal stromal cells expanded in human platelet lysate. Cytotherapy 2011, 13, 786–801. [Google Scholar] [CrossRef] [PubMed]
- Koerner, J.; Nesic, D.; Romero, J.D.; Brehm, W.; Mainil-Varlet, P.; Grogan, S.P. Equine peripheral blood-derived progenitors in comparison to bone marrow-derived mesenchymal stem cells. Stem Cells 2006, 24, 1613–1619. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.S.; Zhang, C.; Zhang, X.; Chen, X.H. Human umbilical cord blood-derived stromal cells: A new source of stromal cells in hematopoietic stem cell transplantation. Crit. Rev. Oncol. Hematol. 2014, 90, 93–98. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, D.; Achermann, J.; Odermatt, B.; Genoni, M.; Zund, G.; Hoerstrup, S.P. Cryopreserved amniotic fluid-derived cells: A lifelong autologous fetal stem cell source for heart valve tissue engineering. J. Heart Valve Dis. 2008, 17, 446–455. [Google Scholar] [PubMed]
- Mehrabani, D.P.; Nazarabadi, R.B.M.; Kasraeian, M.M.; Tamadon, A.P.; Dianatpour, M.P.; Vahdati, A.P.; Zare, S.B.; Ghobadi, F.D. Growth kinetics, characterization, and plasticity of human menstrual blood stem cells. Iran. J. Med. Sci. 2016, 41, 132–139. [Google Scholar] [PubMed]
- Hassiotou, F.; Beltran, A.; Chetwynd, E.; Stuebe, A.M.; Twigger, A.J.; Metzger, P.; Trengove, N.; Lai, C.T.; Filgueira, L.; Blancafort, P.; et al. Breastmilk is a novel source of stem cells with multilineage differentiation potential. Stem Cells 2012, 30, 2164–2174. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; McNeill, E.; Tian, H.; Soker, S.; Andersson, K.E.; Yoo, J.J.; Atala, A. Urine derived cells are a potential source for urological tissue reconstruction. J. Urol. 2008, 180, 2226–2233. [Google Scholar] [CrossRef] [PubMed]
- Alvarez, R.; Lee, H.L.; Wang, C.Y.; Hong, C. Characterization of the osteogenic potential of mesenchymal stem cells from human periodontal ligament based on cell surface markers. Int. J. Oral. Sci. 2015, 7, 213–219. [Google Scholar] [CrossRef] [PubMed]
- Luzzani, C.; Neiman, G.; Garate, X.; Questa, M.; Solari, C.; Fernandez Espinosa, D.; Garcia, M.; Errecalde, A.L.; Guberman, A.; Scassa, M.E.; et al. A therapy-grade protocol for differentiation of pluripotent stem cells into mesenchymal stem cells using platelet lysate as supplement. Stem Cell Res. Ther. 2015, 6, 6. [Google Scholar] [CrossRef] [PubMed]
- Maleki, M.; Ghanbarvand, F.; Reza Behvarz, M.; Ejtemaei, M.; Ghadirkhomi, E. Comparison of mesenchymal stem cell markers in multiple human adult stem cells. Int. J. Stem Cells 2014, 7, 118–126. [Google Scholar] [CrossRef] [PubMed]
- Mohanty, N.; Gulati, B.R.; Kumar, R.; Gera, S.; Kumar, P.; Somasundaram, R.K.; Kumar, S. Immunophenotypic characterization and tenogenic differentiation of mesenchymal stromal cells isolated from equine umbilical cord blood. Vitro Cell. Dev. Biol. Anim. 2014, 50, 538–548. [Google Scholar] [CrossRef] [PubMed]
- Mohanty, N.; Gulati, B.R.; Kumar, R.; Gera, S.; Kumar, S.; Kumar, P.; Yadav, P.S. Phenotypical and functional characteristics of mesenchymal stem cells derived from equine umbilical cord blood. Cytotechnology 2014, 12, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Trivedi, P.; Hematti, P. Derivation and immunological characterization of mesenchymal stromal cells from human embryonic stem cells. Exp. Hematol. 2008, 36, 350–359. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Liu, Y.; Zhou, K.; Zhang, G.; Wang, F.; Ren, J. Isolation and characterization of cd105+/cd90+ subpopulation in breast cancer MDA-MB-231 cell line. Int. J. Clin. Exp. Pathol. 2015, 8, 5105–5112. [Google Scholar] [PubMed]
- Szala, S.; Wisniewska, E.; Czapla, J. [mesenchymal stromal cells]. Postepy Hig. Med. Dosw. (Online) 2014, 68, 1287–1298. [Google Scholar] [CrossRef]
- Miranda, H.C.; Herai, R.H.; Thome, C.H.; Gomes, G.G.; Panepucci, R.A.; Orellana, M.D.; Covas, D.T.; Muotri, A.R.; Greene, L.J.; Faca, V.M. A quantitative proteomic and transcriptomic comparison of human mesenchymal stem cells from bone marrow and umbilical cord vein. Proteomics 2012, 12, 2607–2617. [Google Scholar] [CrossRef] [PubMed]
- Wegmeyer, H.; Broske, A.M.; Leddin, M.; Kuentzer, K.; Nisslbeck, A.K.; Hupfeld, J.; Wiechmann, K.; Kuhlen, J.; von Schwerin, C.; Stein, C.; et al. Mesenchymal stromal cell characteristics vary depending on their origin. Stem Cells Dev. 2013, 22, 2606–2618. [Google Scholar] [CrossRef] [PubMed]
- Sorensen, A.L.; Timoskainen, S.; West, F.D.; Vekterud, K.; Boquest, A.C.; Ahrlund-Richter, L.; Stice, S.L.; Collas, P. Lineage-specific promoter DNA methylation patterns segregate adult progenitor cell types. Stem Cells Dev. 2010, 19, 1257–1266. [Google Scholar] [CrossRef] [PubMed]
- Pizzute, T.; Lynch, K.; Pei, M. Impact of tissue-specific stem cells on lineage-specific differentiation: A focus on the musculoskeletal system. Stem Cell Rev. 2015, 11, 119–132. [Google Scholar] [CrossRef] [PubMed]
- Xie, L.; Zhang, N.; Marsano, A.; Vunjak-Novakovic, G.; Zhang, Y.; Lopez, M.J. In vitro mesenchymal trilineage differentiation and extracellular matrix production by adipose and bone marrow derived adult equine multipotent stromal cells on a collagen scaffold. Stem Cell Rev. 2013, 9, 858–872. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; Zhang, X.J.; Fang, L.; Zhao, T.B. Co-culture of annulus fibrosus cells and bone marrow mesenchymal stem cells. GMR 2015, 14, 3932–3938. [Google Scholar] [CrossRef] [PubMed]
- Strassburg, S.; Nienhueser, H.; Bjorn Stark, G.; Finkenzeller, G.; Torio-Padron, N. Co-culture of adipose-derived stem cells and endothelial cells in fibrin induces angiogenesis and vasculogenesis in a chorioallantoic membrane model. J. Tissue Eng. Regen. Med. 2013. [Google Scholar] [CrossRef] [PubMed]
- Pan, C.; Kumar, C.; Bohl, S.; Klingmueller, U.; Mann, M. Comparative proteomic phenotyping of cell lines and primary cells to assess preservation of cell type-specific functions. MCP 2009, 8, 443–450. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, P.H.; Boura, J.S.; Abecasis, M.M.; Gimble, J.M.; da Silva, C.L.; Cabral, J.M. Impact of hypoxia and long-term cultivation on the genomic stability and mitochondrial performance of ex vivo expanded human stem/stromal cells. Stem Cell Res. 2012, 9, 225–236. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.S.; Lee, B.J.; Park, H.Y.; Song, J.S.; Shin, S.C.; Lee, J.C.; Wang, S.G.; Jung, J.S. Effects of donor age, long-term passage culture, and cryopreservation on tonsil-derived mesenchymal stem cells. Cell. Physiol. Biochem. 2015, 36, 85–99. [Google Scholar] [CrossRef] [PubMed]
- Khoo, M.L.; Shen, B.; Tao, H.; Ma, D.D. Long-term serial passage and neuronal differentiation capability of human bone marrow mesenchymal stem cells. Stem Cells Dev. 2008, 17, 883–896. [Google Scholar] [CrossRef] [PubMed]
- Tan, A.R.; Alegre-Aguaron, E.; O’Connell, G.D.; VandenBerg, C.D.; Aaron, R.K.; Vunjak-Novakovic, G.; Chloe Bulinski, J.; Ateshian, G.A.; Hung, C.T. Passage-dependent relationship between mesenchymal stem cell mobilization and chondrogenic potential. Osteoarthr. Cartil. 2015, 23, 319–327. [Google Scholar] [CrossRef] [PubMed]
- Wagner, W.; Bork, S.; Horn, P.; Krunic, D.; Walenda, T.; Diehlmann, A.; Benes, V.; Blake, J.; Huber, F.X.; Eckstein, V.; et al. Aging and replicative senescence have related effects on human stem and progenitor cells. PLoS ONE 2009, 4, e5846. [Google Scholar] [CrossRef] [PubMed]
- Sureshkumar, P.; Srinivasan, S.P.; Natarajan, K.; Gaspar, J.A.; Hescheler, J.; Sachinidis, A. Stem cells and differentiation—A synoptic review of patents granted since 2009. Exp. Opin. Ther. Pat. 2015, 25, 663–673. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, K.; Yamanaka, S. Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell 2006, 126, 663–676. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Singh, V.K.; Kalsan, M.; Kumar, N.; Saini, A.; Chandra, R. Induced pluripotent stem cells: Applications in regenerative medicine, disease modeling, and drug discovery. Front. Cell Dev. Biol. 2015, 3, 2. [Google Scholar] [CrossRef] [PubMed]
- Cefalo, M.G.; Carai, A.; Miele, E.; Po, A.; Ferretti, E.; Mastronuzzi, A.; Germano, I.M. Human iPSC for therapeutic approaches to the nervous system: Present and future applications. Stem Cells Int. 2016, 2016, 4869071. [Google Scholar] [CrossRef] [PubMed]
- Hacein-Bey-Abina, S.; von Kalle, C.; Schmidt, M.; le Deist, F.; Wulffraat, N.; McIntyre, E.; Radford, I.; Villeval, J.L.; Fraser, C.C.; Cavazzana-Calvo, M.; et al. A serious adverse event after successful gene therapy for X-linked severe combined immunodeficiency. N. Engl. J. Med. 2003, 348, 255–256. [Google Scholar] [CrossRef] [PubMed]
- Lehrman, S. Virus treatment questioned after gene therapy death. Nature 1999, 401, 517–518. [Google Scholar] [CrossRef] [PubMed]
- Taha, M.F. Cell based-gene delivery approaches for the treatment of spinal cord injury and neurodegenerative disorders. Curr. Stem Cell Res. Ther. 2010, 5, 23–36. [Google Scholar] [CrossRef] [PubMed]
- Jabbarzadeh, E.; Starnes, T.; Khan, Y.M.; Jiang, T.; Wirtel, A.J.; Deng, M.; Lv, Q.; Nair, L.S.; Doty, S.B.; Laurencin, C.T. Induction of angiogenesis in tissue-engineered scaffolds designed for bone repair: A combined gene therapy-cell transplantation approach. Proc. Natl. Acad. Sci. USA 2008, 105, 11099–11104. [Google Scholar] [CrossRef] [PubMed]
- Ouyang, B.; Sun, X.; Han, D.; Chen, S.; Yao, B.; Gao, Y.; Bian, J.; Huang, Y.; Zhang, Y.; Wan, Z.; et al. Human urine-derived stem cells alone or genetically-modified with FGF2 improve type 2 diabetic erectile dysfunction in a rat model. PLoS ONE 2014, 9, e92825. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Jiang, Z.; Fitzgerald, D.C.; Ma, C.; Yu, S.; Li, H.; Zhao, Z.; Li, Y.; Ciric, B.; Curtis, M.; et al. Adult neural stem cells expressing IL-10 confer potent immunomodulation and remyelination in experimental autoimmune encephalitis. J. Clin. Investig. 2009, 119, 3678–3691. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Tew, S.R.; Russell, A.M.; Gonzalez, K.R.; Hardingham, T.E.; Hawkins, R.E. Transduction of passaged human articular chondrocytes with adenoviral, retroviral, and lentiviral vectors and the effects of enhanced expression of SOX9. Tissue Eng. 2004, 10, 575–584. [Google Scholar] [CrossRef] [PubMed]
- Mark Saltzman, W.; Baldwin, S.P. Materials for protein delivery in tissue engineering. Adv. Drug Deliv. Rev. 1998, 33, 71–86. [Google Scholar] [PubMed]
- Sukarto, A.; Yu, C.; Flynn, L.E.; Amsden, B.G. Co-delivery of adipose-derived stem cells and growth factor-loaded microspheres in RGD-grafted N-methacrylate glycol chitosan gels for focal chondral repair. Biomacromolecules 2012, 13, 2490–2502. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.W.; Jeon, O.; Kim, B.S. Poly(lactic-co-glycolic acid) microspheres as an injectable scaffold for cartilage tissue engineering. Tissue Eng. 2005, 11, 438–447. [Google Scholar] [CrossRef] [PubMed]
- Eswaramoorthy, R.; Chang, C.C.; Wu, S.C.; Wang, G.J.; Chang, J.K.; Ho, M.L. Sustained release of PTH(1–34) from PLGA microspheres suppresses osteoarthritis progression in rats. Acta Biomater. 2012, 8, 2254–2262. [Google Scholar] [CrossRef] [PubMed]
- Niu, X.; Feng, Q.; Wang, M.; Guo, X.; Zheng, Q. Porous nano-HA/collagen/PLLA scaffold containing chitosan microspheres for controlled delivery of synthetic peptide derived from BMP-2. J. Control. Release 2009, 134, 111–117. [Google Scholar] [CrossRef] [PubMed]
- Bian, L.; Zhai, D.Y.; Tous, E.; Rai, R.; Mauck, R.L.; Burdick, J.A. Enhanced MSC chondrogenesis following delivery of TGF-β3 from alginate microspheres within hyaluronic acid hydrogels in vitro and in vivo. Biomaterials 2011, 32, 6425–6434. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Wei, Y.T.; Zu, Z.H.; Ju, R.K.; Guo, M.Y.; Wang, X.M.; Xu, Q.Y.; Cui, F.Z. Combination of hyaluronic acid hydrogel scaffold and PLGA microspheres for supporting survival of neural stem cells. Pharm. Res. 2011, 28, 1406–1414. [Google Scholar] [CrossRef] [PubMed]
- Lim, J.J.; Hammoudi, T.M.; Bratt-Leal, A.M.; Hamilton, S.K.; Kepple, K.L.; Bloodworth, N.C.; McDevitt, T.C.; Temenoff, J.S. Development of nano- and microscale chondroitin sulfate particles for controlled growth factor delivery. Acta Biomater. 2011, 7, 986–995. [Google Scholar] [CrossRef] [PubMed]
- Zhao, W.; Zhang, C.; Jin, C.; Zhang, Z.; Kong, D.; Xu, W.; Xiu, Y. Periurethral injection of autologous adipose-derived stem cells with controlled-release nerve growth factor for the treatment of stress urinary incontinence in a rat model. Eur. Urol. 2011, 59, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Olson, A.; Graver, A.; Grande, D. Scaffolds for articular cartilage repair. J. Long Term Eff. Med. Implant. 2012, 22, 219–227. [Google Scholar] [CrossRef]
- Nie, T.; Baldwin, A.; Yamaguchi, N.; Kiick, K.L. Production of heparin-functionalized hydrogels for the development of responsive and controlled growth factor delivery systems. J. Control. Release 2007, 122, 287–296. [Google Scholar] [CrossRef] [PubMed]
- Skop, N.B.; Calderon, F.; Levison, S.W.; Gandhi, C.D.; Cho, C.H. Heparin crosslinked chitosan microspheres for the delivery of neural stem cells and growth factors for central nervous system repair. Acta Biomater. 2013, 9, 6834–6843. [Google Scholar] [CrossRef] [PubMed]
- Webber, M.J.; Han, X.; Murthy, S.N.; Rajangam, K.; Stupp, S.I.; Lomasney, J.W. Capturing the stem cell paracrine effect using heparin-presenting nanofibres to treat cardiovascular diseases. J. Tissue Eng. Regen. Med. 2010, 4, 600–610. [Google Scholar] [CrossRef] [PubMed]
- Jung, H.H.; Park, K.; Han, D.K. Preparation of TGF-β1-conjugated biodegradable pluronic F127 hydrogel and its application with adipose-derived stem cells. J. Control. Release 2010, 147, 84–91. [Google Scholar] [CrossRef] [PubMed]
- Yu, S.P.; Wei, Z.; Wei, L. Preconditioning strategy in stem cell transplantation therapy. Trans. Stroke Res. 2013, 4, 76–88. [Google Scholar] [CrossRef] [PubMed]
- Chang, W.; Song, B.W.; Moon, J.Y.; Cha, M.J.; Ham, O.; Lee, S.Y.; Choi, E.; Hwang, K.C. Anti-death strategies against oxidative stress in grafted mesenchymal stem cells. Histol. Histopathol. 2013, 28, 1529–1536. [Google Scholar] [PubMed]
- Lo, E.H.; Wang, X.; Cuzner, M.L. Extracellular proteolysis in brain injury and inflammation: Role for plasminogen activators and matrix metalloproteinases. J. Neurosci. Res. 2002, 69, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Sart, S.; Ma, T.; Li, Y. Preconditioning stem cells for in vivo delivery. BioRes. Open Access 2014, 3, 137–149. [Google Scholar] [CrossRef] [PubMed]
- Boyette, L.B.; Creasey, O.A.; Guzik, L.; Lozito, T.; Tuan, R.S. Human bone marrow-derived mesenchymal stem cells display enhanced clonogenicity but impaired differentiation with hypoxic preconditioning. Stem Cells Trans. Med. 2014, 3, 241–254. [Google Scholar] [CrossRef] [PubMed]
- Wei, L.; Fraser, J.L.; Lu, Z.Y.; Hu, X.; Yu, S.P. Transplantation of hypoxia preconditioned bone marrow mesenchymal stem cells enhances angiogenesis and neurogenesis after cerebral ischemia in rats. Neurobiol. Dis. 2012, 46, 635–645. [Google Scholar] [CrossRef] [PubMed]
- Haider, H.; Ashraf, M. Preconditioning and stem cell survival. J. Cardiovasc. Trans. Res. 2010, 3, 89–102. [Google Scholar] [CrossRef] [PubMed]
- Rosova, I.; Dao, M.; Capoccia, B.; Link, D.; Nolta, J.A. Hypoxic preconditioning results in increased motility and improved therapeutic potential of human mesenchymal stem cells. Stem Cells 2008, 26, 2173–2182. [Google Scholar] [CrossRef] [PubMed]
- Pati, S.; Supeno, N.E.; Muthuraju, S.; Abdul Hadi, R.; Ghani, A.R.; Idris, F.M.; Maletic-Savatic, M.; Abdullah, J.M.; Jaafar, H. MicroRNA profiling reveals unique mirna signatures in IGF-1 treated embryonic striatal stem cell fate decisions in striatal neurogenesis in vitro. BioMed Res. Int. 2014, 2014, 503162. [Google Scholar] [CrossRef] [PubMed]
- Lu, G.; Ashraf, M.; Haider, K.H. Insulin-like growth factor-1 preconditioning accentuates intrinsic survival mechanism in stem cells to resist ischemic injury by orchestrating protein kinase Cα-Erk1/2 activation. Antioxid. Redox Signal. 2012, 16, 217–227. [Google Scholar] [CrossRef] [PubMed]
- Xinaris, C.; Morigi, M.; Benedetti, V.; Imberti, B.; Fabricio, A.S.; Squarcina, E.; Benigni, A.; Gagliardini, E.; Remuzzi, G. A novel strategy to enhance mesenchymal stem cell migration capacity and promote tissue repair in an injury specific fashion. Cell Trans. 2013, 22, 423–436. [Google Scholar] [CrossRef] [PubMed]
- Ma, H.L.; Chen, T.H.; Low-Tone Ho, L.; Hung, S.C. Neocartilage from human mesenchymal stem cells in alginate: Implied timing of transplantation. J. Biomed. Mater. Res. Part A 2005, 74, 439–446. [Google Scholar] [CrossRef] [PubMed]
- Doorn, J.; van de Peppel, J.; van Leeuwen, J.P.; Groen, N.; van Blitterswijk, C.A.; de Boer, J. Pro-osteogenic trophic effects by PKA activation in human mesenchymal stromal cells. Biomaterials 2011, 32, 6089–6098. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.; Ali, F.; Mohsin, S.; Akhtar, S.; Mehmood, A.; Choudhery, M.S.; Khan, S.N.; Riazuddin, S. Preconditioning diabetic mesenchymal stem cells with myogenic medium increases their ability to repair diabetic heart. Stem Cell Res. Ther. 2013, 4, 58. [Google Scholar] [CrossRef] [PubMed]
- Chacko, S.M.; Ahmed, S.; Selvendiran, K.; Kuppusamy, M.L.; Khan, M.; Kuppusamy, P. Hypoxic preconditioning induces the expression of prosurvival and proangiogenic markers in mesenchymal stem cells. Am. J. Physiol. Cell Physiol. 2010, 299, C1562–C1570. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.S.; Watkins, E.; Burnsed, O.A.; Schwartz, Z.; Boyan, B.D. Tailoring adipose stem cell trophic factor production with differentiation medium components to regenerate chondral defects. Tissue Eng. Part A 2013, 19, 1451–1464. [Google Scholar] [CrossRef] [PubMed]
- Tratwal, J.; Mathiasen, A.B.; Juhl, M.; Brorsen, S.K.; Kastrup, J.; Ekblond, A. Influence of vascular endothelial growth factor stimulation and serum deprivation on gene activation patterns of human adipose tissue-derived stromal cells. Stem Cell Res. Ther. 2015, 6, 62. [Google Scholar] [CrossRef] [PubMed]
- Karp, J.M.; Leng Teo, G.S. Mesenchymal stem cell homing: The devil is in the details. Cell Stem Cell 2009, 4, 206–216. [Google Scholar] [CrossRef] [PubMed]
- Fujiwara, H.; Kubota, T.; Amaike, H.; Inada, S.; Takashima, K.; Atsuji, K.; Yoshimura, M.; Maemondo, M.; Narumi, K.; Nukiwa, T.; et al. Suppression of peritoneal implantation of gastric cancer cells by adenovirus vector-mediated NK4 expression. Cancer Gene Ther. 2005, 12, 206–216. [Google Scholar] [CrossRef] [PubMed]
- Fu, X.M.; Yamawaki-Ogata, A.; Oshima, H.; Ueda, Y.; Usui, A.; Narita, Y. Intravenous administration of mesenchymal stem cells prevents angiotensin II-induced aortic aneurysm formation in apolipoprotein E-deficient mouse. J. Trans. Med. 2013, 11, 175. [Google Scholar] [CrossRef] [PubMed]
- Chan, J.; Waddington, S.N.; O’Donoghue, K.; Kurata, H.; Guillot, P.V.; Gotherstrom, C.; Themis, M.; Morgan, J.E.; Fisk, N.M. Widespread distribution and muscle differentiation of human fetal mesenchymal stem cells after intrauterine transplantation in dystrophic mdx mouse. Stem Cells 2007, 25, 875–884. [Google Scholar] [CrossRef] [PubMed]
- Yamaoka, K. [potential of bone regenerative therapy with mesenchymal stem cells in rheumatoid arthritis]. Clin. Calcium 2016, 26, 758–762. [Google Scholar] [PubMed]
- Zhang, L.; Li, K.; Liu, X.; Li, D.; Luo, C.; Fu, B.; Cui, S.; Zhu, F.; Zhao, R.C.; Chen, X. Repeated systemic administration of human adipose-derived stem cells attenuates overt diabetic nephropathy in rats. Stem Cells Dev. 2013. [Google Scholar] [CrossRef] [PubMed]
- Goncalves Fda, C.; Schneider, N.; Pinto, F.O.; Meyer, F.S.; Visioli, F.; Pfaffenseller, B.; Lopez, P.L.; Passos, E.P.; Cirne-Lima, E.O.; Meurer, L.; et al. Intravenous vs. intraperitoneal mesenchymal stem cells administration: What is the best route for treating experimental colitis? World J. Gastroenterol. 2014. [Google Scholar] [CrossRef]
- Muschler, G.F.; Nakamoto, C.; Griffith, L.G. Engineering principles of clinical cell-based tissue engineering. J. Bone Jt. Surg. Am. 2004, 86, 1541–1558. [Google Scholar]
- Rivera, F.J.; Aigner, L. Adult mesenchymal stem cell therapy for myelin repair in multiple sclerosis. Biol. Res. 2012, 45, 257–268. [Google Scholar] [CrossRef] [PubMed]
- Mangera, A.; Chapple, C.R. Tissue engineering in urethral reconstruction—An update. Asian J. Androl. 2013, 15, 89–92. [Google Scholar] [CrossRef] [PubMed]
- Cai, J.; Yu, X.; Xu, R.; Fang, Y.; Qian, X.; Liu, S.; Teng, J.; Ding, X. Maximum efficacy of mesenchymal stem cells in rat model of renal ischemia-reperfusion injury: Renal artery administration with optimal numbers. PLoS ONE 2014, 9, e92347. [Google Scholar] [CrossRef] [PubMed]
- Deng, K.; Lin, D.L.; Hanzlicek, B.; Balog, B.; Penn, M.S.; Kiedrowski, M.J.; Hu, Z.; Ye, Z.; Zhu, H.; Damaser, M.S. Mesenchymal stem cells and their secretome partially restore nerve and urethral function in a dual muscle and nerve injury stress urinary incontinence model. Am. J. Physiol. Ren. Physiol. 2015, 308, F92–F100. [Google Scholar] [CrossRef] [PubMed]
- Herrmann, J.L.; Abarbanell, A.M.; Weil, B.R.; Wang, Y.; Poynter, J.A.; Manukyan, M.C.; Meldrum, D.R. Postinfarct intramyocardial injection of mesenchymal stem cells pretreated with TGF-α improves acute myocardial function. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2010, 299, R371–R378. [Google Scholar] [CrossRef] [PubMed]
- Sun, C.; Lin, H.; Yu, W.; Li, X.; Chen, Y.; Qiu, X.; Wang, R.; Dai, Y. Neurotrophic effect of bone marrow mesenchymal stem cells for erectile dysfunction in diabetic rats. Int. J. Androl. 2012, 35, 601–607. [Google Scholar] [CrossRef] [PubMed]
- Zhang, D.; Liu, X.; Peng, J.; He, D.; Lin, T.; Zhu, J.; Li, X.; Zhang, Y.; Wei, G. Potential spermatogenesis recovery with bone marrow mesenchymal stem cells in an azoospermic rat model. Int. J. Mol. Sci. 2014, 15, 13151–13165. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.; Zhang, Y.; Zhao, J.; Jiang, B. Intramuscular injection of bone marrow mesenchymal stem cells with small gap neurorrhaphy for peripheral nerve repair. Neurosci. Lett. 2015, 585, 119–125. [Google Scholar] [CrossRef] [PubMed]
- Jarvinen, T.A.; Jarvinen, M.; Kalimo, H. Regeneration of injured skeletal muscle after the injury. Muscles Ligaments Tend. J. 2013, 3, 337–345. [Google Scholar]
- Deten, A.; Volz, H.C.; Briest, W.; Zimmer, H.G. Cardiac cytokine expression is upregulated in the acute phase after myocardial infarction. Experimental studies in rats. Cardiovasc. Res. 2002, 55, 329–340. [Google Scholar] [CrossRef]
- Hampel, C.; Wienhold, D.; Benken, N.; Eggersmann, C.; Thuroff, J.W. Definition of overactive bladder and epidemiology of urinary incontinence. Urology 1997, 50, 4–14. [Google Scholar] [CrossRef]
- Ota, S.; Uehara, K.; Nozaki, M.; Kobayashi, T.; Terada, S.; Tobita, K.; Fu, F.H.; Huard, J. Intramuscular transplantation of muscle-derived stem cells accelerates skeletal muscle healing after contusion injury via enhancement of angiogenesis. Am. J. Sports Med. 2011, 39, 1912–1922. [Google Scholar] [CrossRef] [PubMed]
- Le Blanc, K.; Frassoni, F.; Ball, L.; Locatelli, F.; Roelofs, H.; Lewis, I.; Lanino, E.; Sundberg, B.; Bernardo, M.E.; Remberger, M.; et al. Mesenchymal stem cells for treatment of steroid-resistant, severe, acute graft-versus-host disease: A phase ii study. Lancet 2008, 371, 1579–1586. [Google Scholar] [CrossRef]
- Dong, J.Y.; Zhang, Y.H.; Qin, L.Q. Erectile dysfunction and risk of cardiovascular disease: Meta-analysis of prospective cohort studies. J. Am. Coll. Cardiol. 2011, 58, 1378–1385. [Google Scholar] [CrossRef] [PubMed]
- Van Koppen, A.; Joles, J.A.; Bongartz, L.G.; van den Brandt, J.; Reichardt, H.M.; Goldschmeding, R.; Nguyen, T.Q.; Verhaar, M.C. Healthy bone marrow cells reduce progression of kidney failure better than CKD bone marrow cells in rats with established chronic kidney disease. Cell Transplant. 2012, 21, 2299–2312. [Google Scholar] [CrossRef] [PubMed]
- Kebriaei, P.; Isola, L.; Bahceci, E.; Holland, K.; Rowley, S.; McGuirk, J.; Devetten, M.; Jansen, J.; Herzig, R.; Schuster, M.; et al. Adult human mesenchymal stem cells added to corticosteroid therapy for the treatment of acute graft-versus-host disease. Biol. Blood Marrow Transplant. 2009, 15, 804–811. [Google Scholar] [CrossRef] [PubMed]
- Sharma, R.R.; Pollock, K.; Hubel, A.; McKenna, D. Mesenchymal stem or stromal cells: A review of clinical applications and manufacturing practices. Transfusion 2014, 54, 1418–1437. [Google Scholar] [CrossRef] [PubMed]
- Behfar, A.; Crespo-Diaz, R.; Terzic, A.; Gersh, B.J. Cell therapy for cardiac repair—Lessons from clinical trials. Nat. Rev. Cardiol. 2014, 11, 232–246. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.S.; Lin, G.; Lue, T.F. Allogeneic and xenogeneic transplantation of adipose-derived stem cells in immunocompetent recipients without immunosuppressants. Stem Cells Dev. 2012, 21, 2770–2778. [Google Scholar] [CrossRef] [PubMed]
- Wei, A.; Tao, H.; Chung, S.A.; Brisby, H.; Ma, D.D.; Diwan, A.D. The fate of transplanted xenogeneic bone marrow-derived stem cells in rat intervertebral discs. J. Orthop. Res. 2009, 27, 374–379. [Google Scholar] [CrossRef] [PubMed]
- Coulthard, M.G.; Flecknell, P.; Orr, H.; Manas, D.; O’Donnell, M. Renal scarring caused by vesicoureteric reflux and urinary infection: A study in pigs. Pediatr. Nephrol. 2002, 17, 481–484. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Zhang, F.; Song, G.; Gu, W.; Chen, M.; Yang, B.; Li, D.; Wang, D.; Cao, K. Intramyocardial injection of pig pluripotent stem cells improves left ventricular function and perfusion: A study in a porcine model of acute myocardial infarction. PLoS ONE 2013, 8, e66688. [Google Scholar] [CrossRef] [PubMed]
- Harding, J.; Roberts, R.M.; Mirochnitchenko, O. Large animal models for stem cell therapy. Stem Cell Res. Ther. 2013, 4, 23. [Google Scholar] [CrossRef] [PubMed]
- Plews, J.R.; Gu, M.; Longaker, M.T.; Wu, J.C. Large animal induced pluripotent stem cells as pre-clinical models for studying human disease. J. Cell. Mol. Med. 2012, 16, 1196–1202. [Google Scholar] [CrossRef] [PubMed]
| Types of Disorders | Key Therapeutic Properties of Stem Cells |
|---|---|
| Congenital defects Trauma or injury | Pluripotency or able to differentiate into multiple cell types; Enables maintenance of an undifferentiated phenotype in multiple subcultures; Capacity for self-renewal |
| Immune disorders | Immunomodulatory effects or reduce local inflammation and fibrosis formation; Counteract chemotactic signals released to recruit immune cells to the site of injury; Paracrine effects, immune tolerance or blunt host immune response |
| Degenerated diseases | Neruoprotection; Anti-apoptosis; Anti-aging effects; Stimulate endogenous tissue regeneration potential |
| Comparison Items | Induced Differentiation of Stem Cells | Non-Induced Differentiation of Stem Cells |
|---|---|---|
| Differentiation status | Differentiated | Non-differentiated |
| In vitro manipulation | More cell expansion and in vitro differentiation | Less |
| Cell viability in vivo | Moderate | Higher |
| Lifespan in vivo | Shorter | Longer |
| Secretion of trophic factors | Moderate | More |
| Recruitment of resident cells | Moderate | More |
| Corporation with resident cells | Transitional stay | Cell fusion, differentiation, and stimulation |
| Effect on tissue repair in vivo | Limitation due to short cell life-span | Acceleration to guide local stem cells differentiation |
| Comparison Items | Systemic Administration | Local Administration | |||
|---|---|---|---|---|---|
| Intravenous Injection (iv) | Intra-Ventricular Injection | Intra-Peritoneal Injection (ip) | Intra-Organ Injection | Intra-Arterial Injection | |
| Ratio of implanted cell retention or Differentiation [95] | 1% | Up to 10% | 0 | 10%–30% | 10%–20% |
| Trophic effect | Yes | Yes | Yes (only) | Yes | Yes |
| Location of implanted cell | Lungs, Spleen, Liver [95] | Blood circulation | Omentum and mesentery [96], and most organs | Targeted organ or tissue | Targeted organ |
| Advantages of procedures | Easy [97] | Mainly for Rodent | Easy, particularly for rodent [98] | Immediate local action [99] | Applicable only for patients or large animals |
| Limitations or complications | <1% of implanted cells homing to the target organ; most in the lungs and spleen [100] | 10% of the cells in target organ [100] | Might inject into intestine, less effect [101] | An open surgery is need to deliver the majority of cells in the right sites [102] | Interventional therapy is required in large animals [102] |
| Comparison Items | Small Animals | Large Animals |
|---|---|---|
| Commonly used animals [125] | Mouse, rat, rabbit | Dog, pig, nonhuman primates |
| Commonly used cell sources | Xenogenous or allogeneic stem cells | Autologous stem cells |
| Optimal cell doses | 0.5–2 millions/injection | 1–5 millions/injection |
| Route of cell administration | Intravenous, intraperitoneal, intra-organ | Intra-arterial, intraperitoneal, intravenous, intra-organ |
| Advantages | Immunocompromised rodents (i.e., NOD/SCID mice, or NOD-Rag mice) used to test human cells; Rapid tissue repair process; Used for proof-of-concept studies [125] | Most organs are similar in anatomy and physiology to humans; Used for pre-clinical studies [126] |
| Disadvantages [125,126] | Not optimal for ureteral, bladder, or urethral reconstruction | Ethical issues in using some models More expensive for maintaining |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, S.; Zhou, J.; Zhang, X.; Liu, Y.; Chen, J.; Hu, B.; Song, J.; Zhang, Y. Strategies to Optimize Adult Stem Cell Therapy for Tissue Regeneration. Int. J. Mol. Sci. 2016, 17, 982. https://doi.org/10.3390/ijms17060982
Liu S, Zhou J, Zhang X, Liu Y, Chen J, Hu B, Song J, Zhang Y. Strategies to Optimize Adult Stem Cell Therapy for Tissue Regeneration. International Journal of Molecular Sciences. 2016; 17(6):982. https://doi.org/10.3390/ijms17060982
Chicago/Turabian StyleLiu, Shan, Jingli Zhou, Xuan Zhang, Yang Liu, Jin Chen, Bo Hu, Jinlin Song, and Yuanyuan Zhang. 2016. "Strategies to Optimize Adult Stem Cell Therapy for Tissue Regeneration" International Journal of Molecular Sciences 17, no. 6: 982. https://doi.org/10.3390/ijms17060982
APA StyleLiu, S., Zhou, J., Zhang, X., Liu, Y., Chen, J., Hu, B., Song, J., & Zhang, Y. (2016). Strategies to Optimize Adult Stem Cell Therapy for Tissue Regeneration. International Journal of Molecular Sciences, 17(6), 982. https://doi.org/10.3390/ijms17060982