Magnolia kobus Extract Inhibits Periodontitis-Inducing Mediators in Porphyromonas gingivalis Lipopolysaccharide-Activated RAW 264.7 Cells
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Preparation of Magnolia kobus Extract
2.3. Cell Culture
2.4. Cell Viability Assay
2.5. Nitric Oxide (NO) Assay
2.6. Protein Extraction and Western Blot Analysis
2.7. Statistical Analysis
3. Results
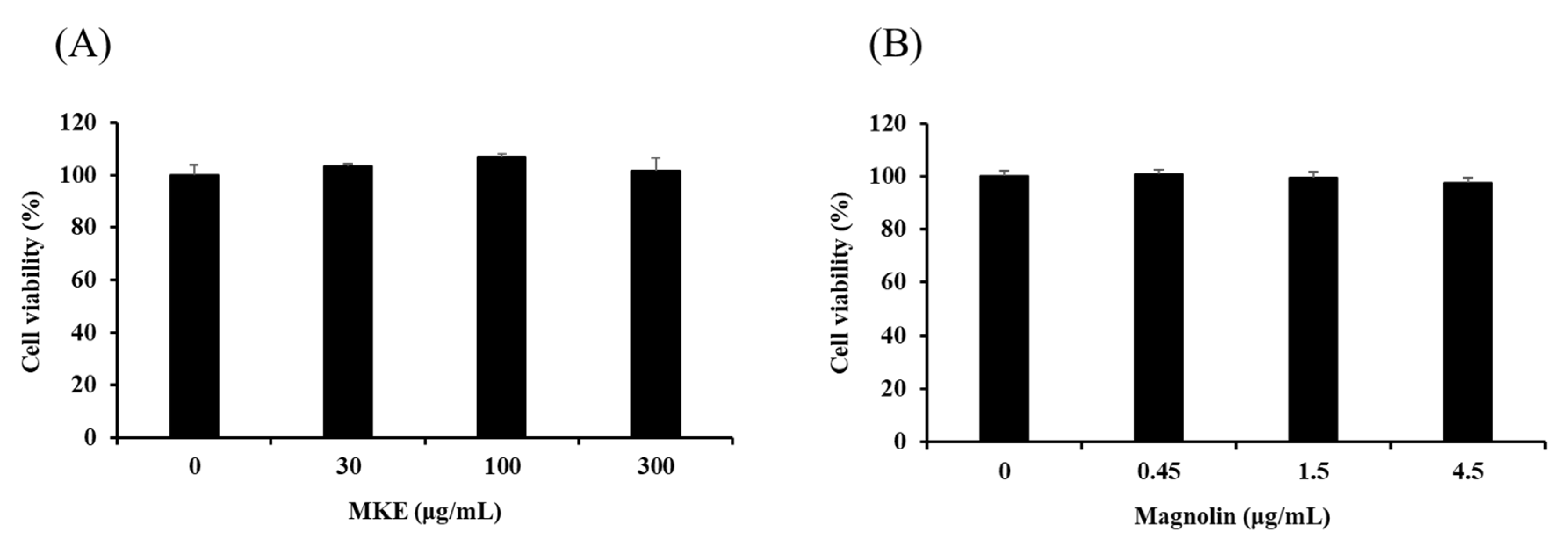
3.1. Cytotoxicity of MKE/Magnolin to RAW 264.7 Cells
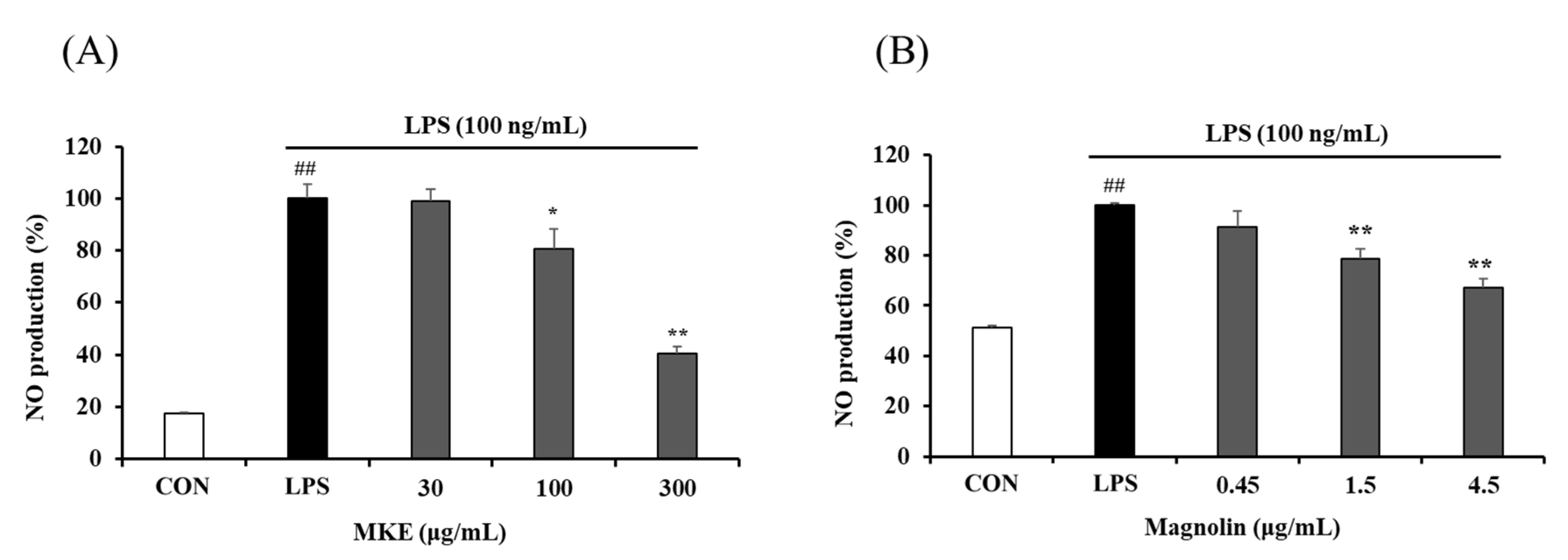
3.2. Effects of MKE/Magnolin on NO Production by RAW 264.7 Cells
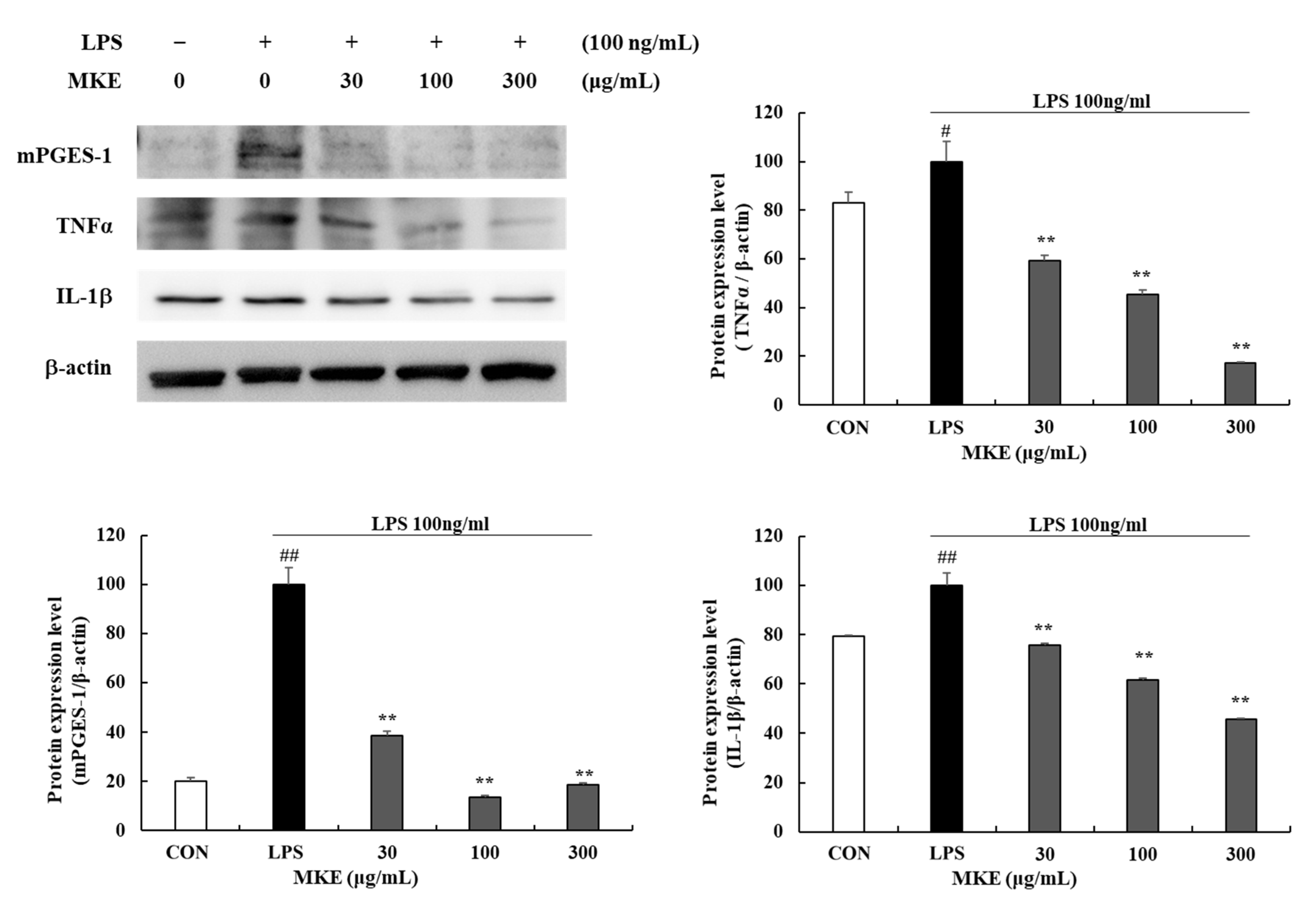
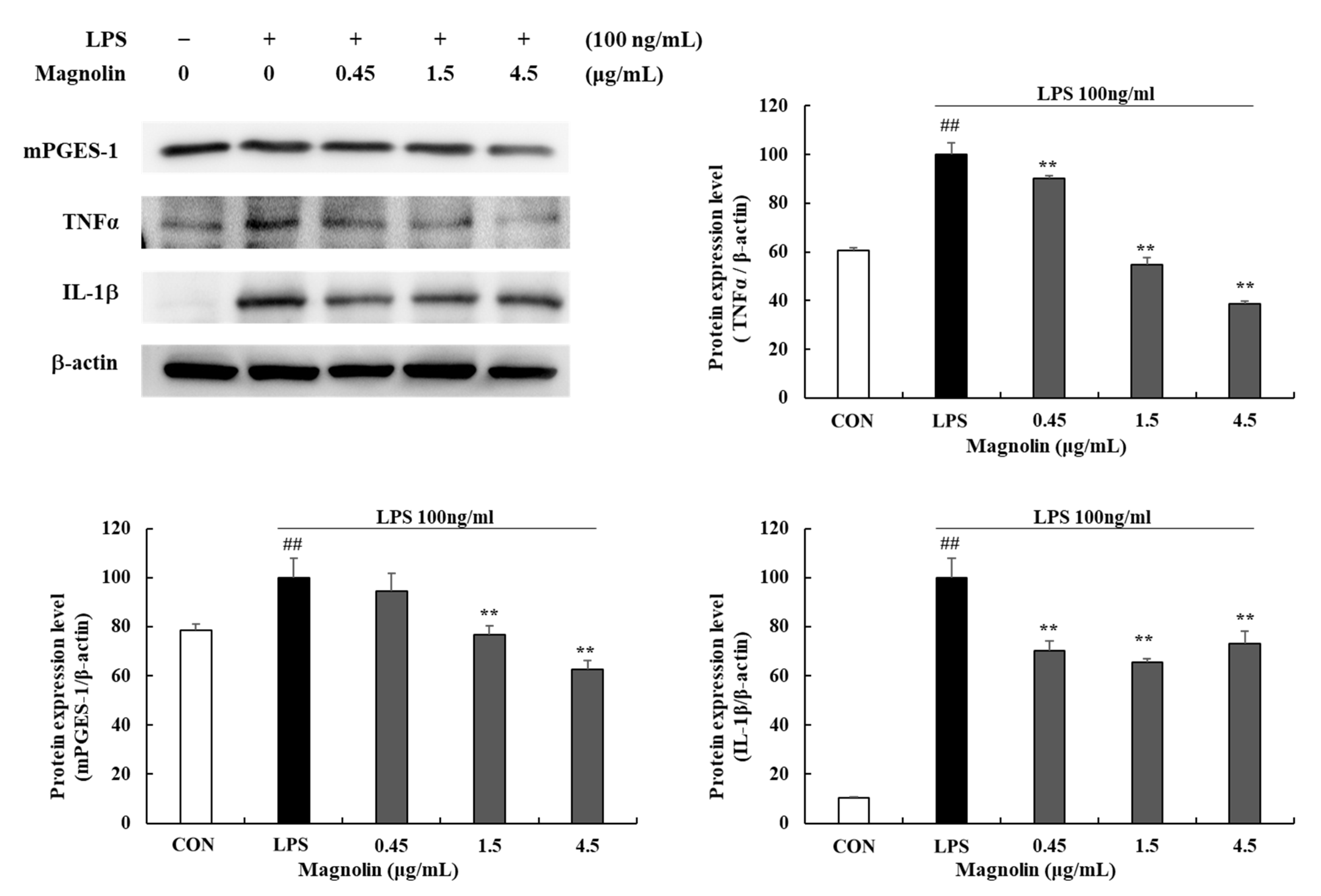
3.3. MKE/Magnolin Inhibits Production of Inflammatory Mediators
3.4. MKE/Magnolin Inhibits Matrix Metalloproteinases (MMPs)
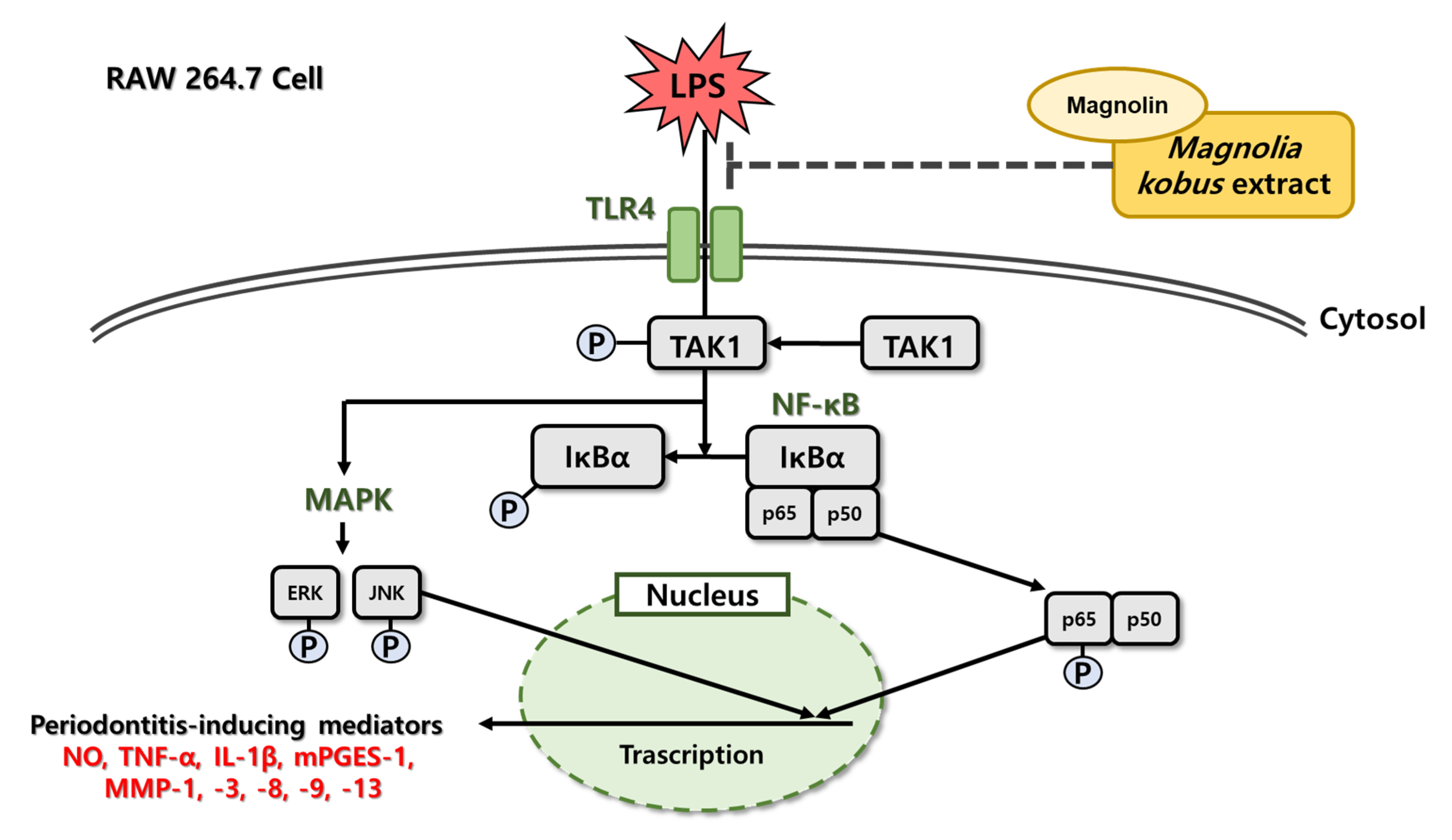
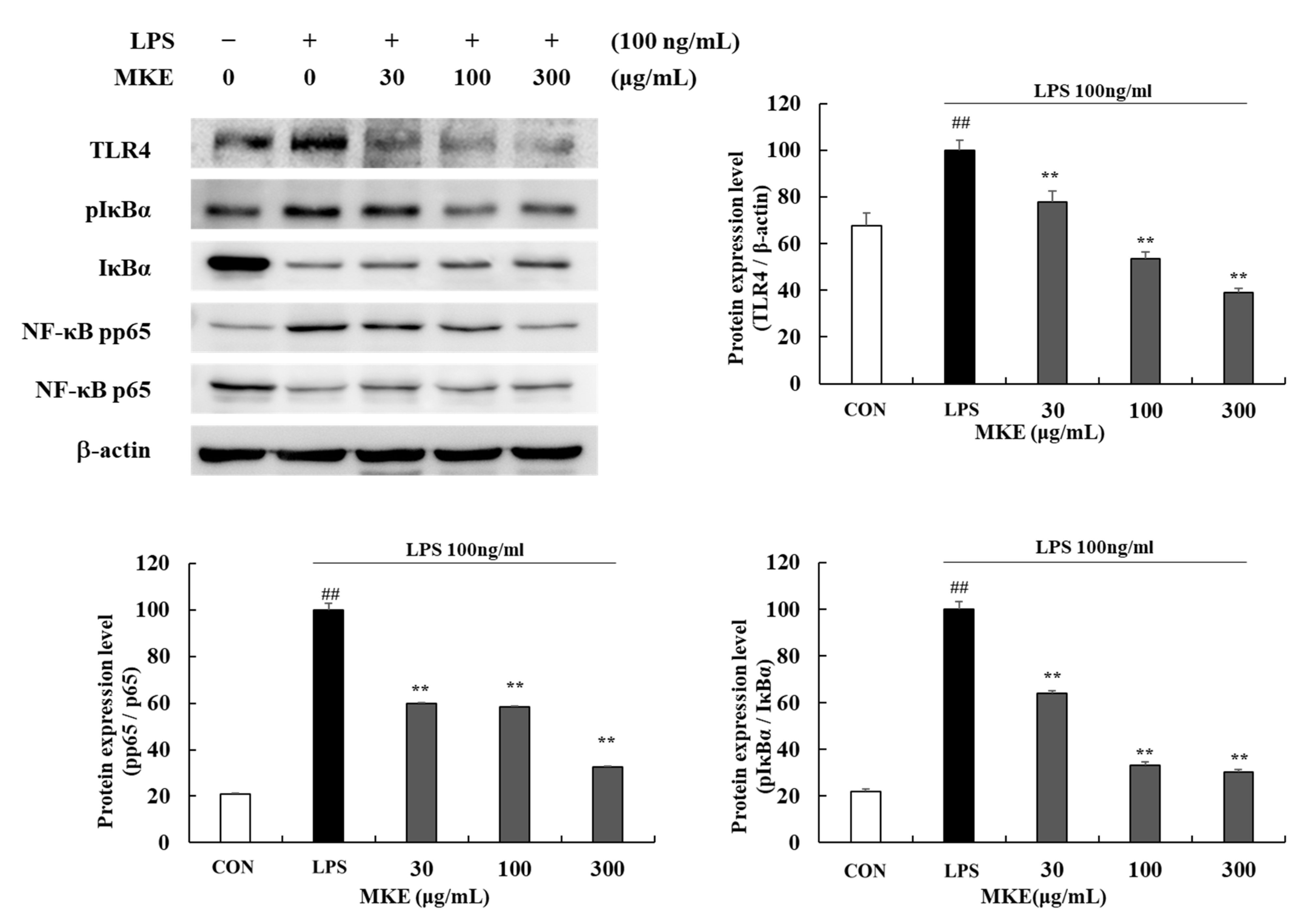
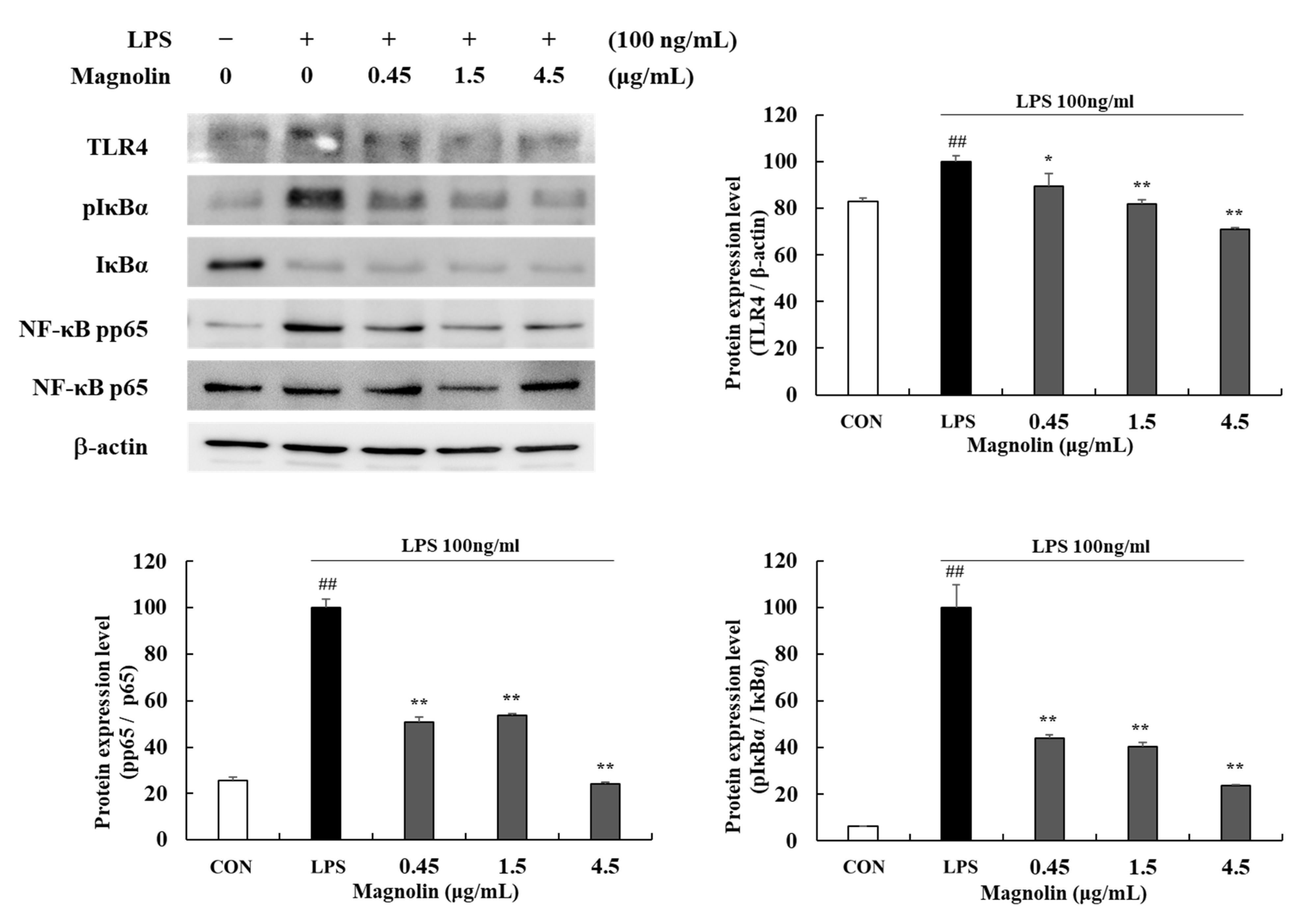
3.5. MKE/Magnolin Inhibits TLR4/NF-κB Signaling Pathways
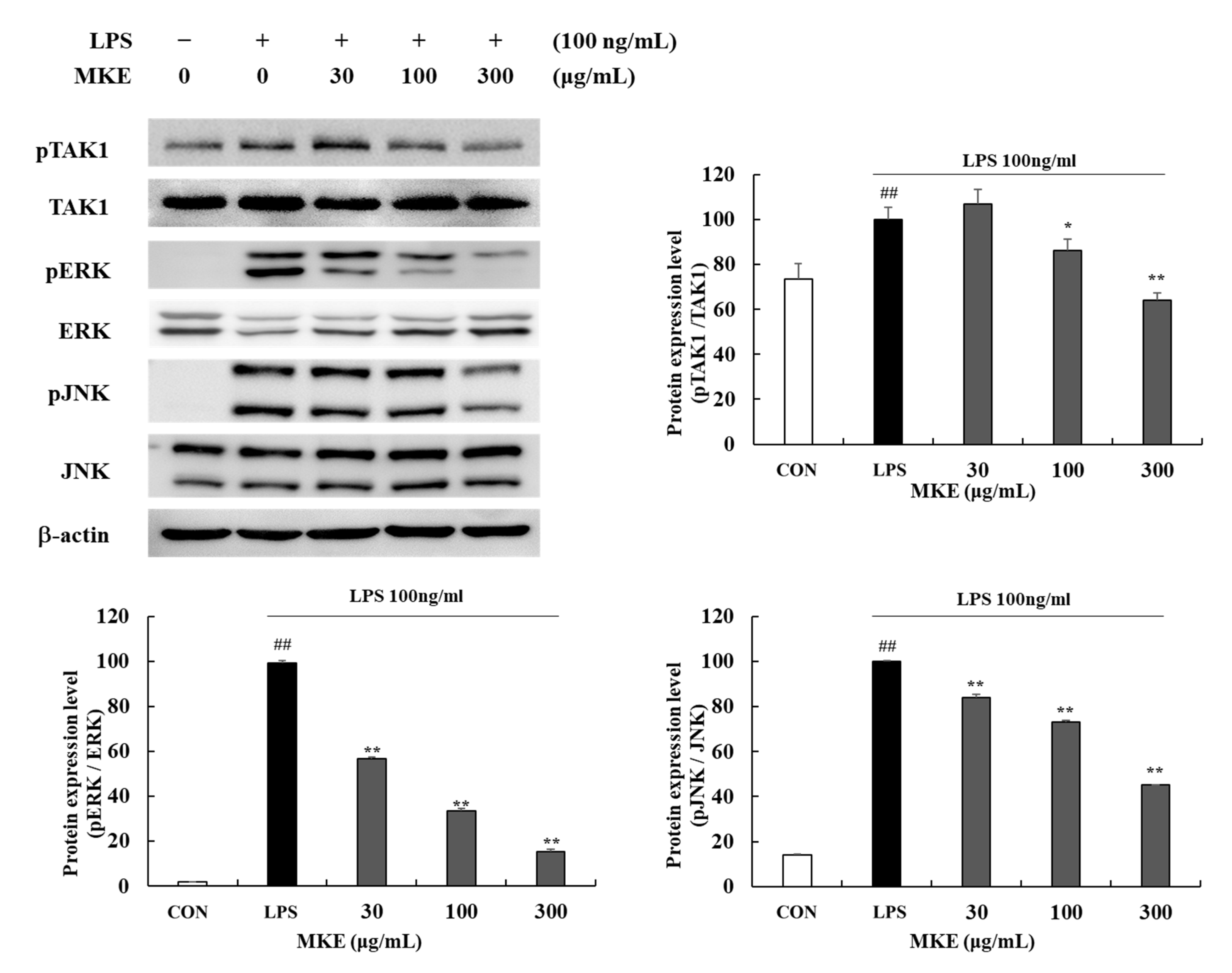
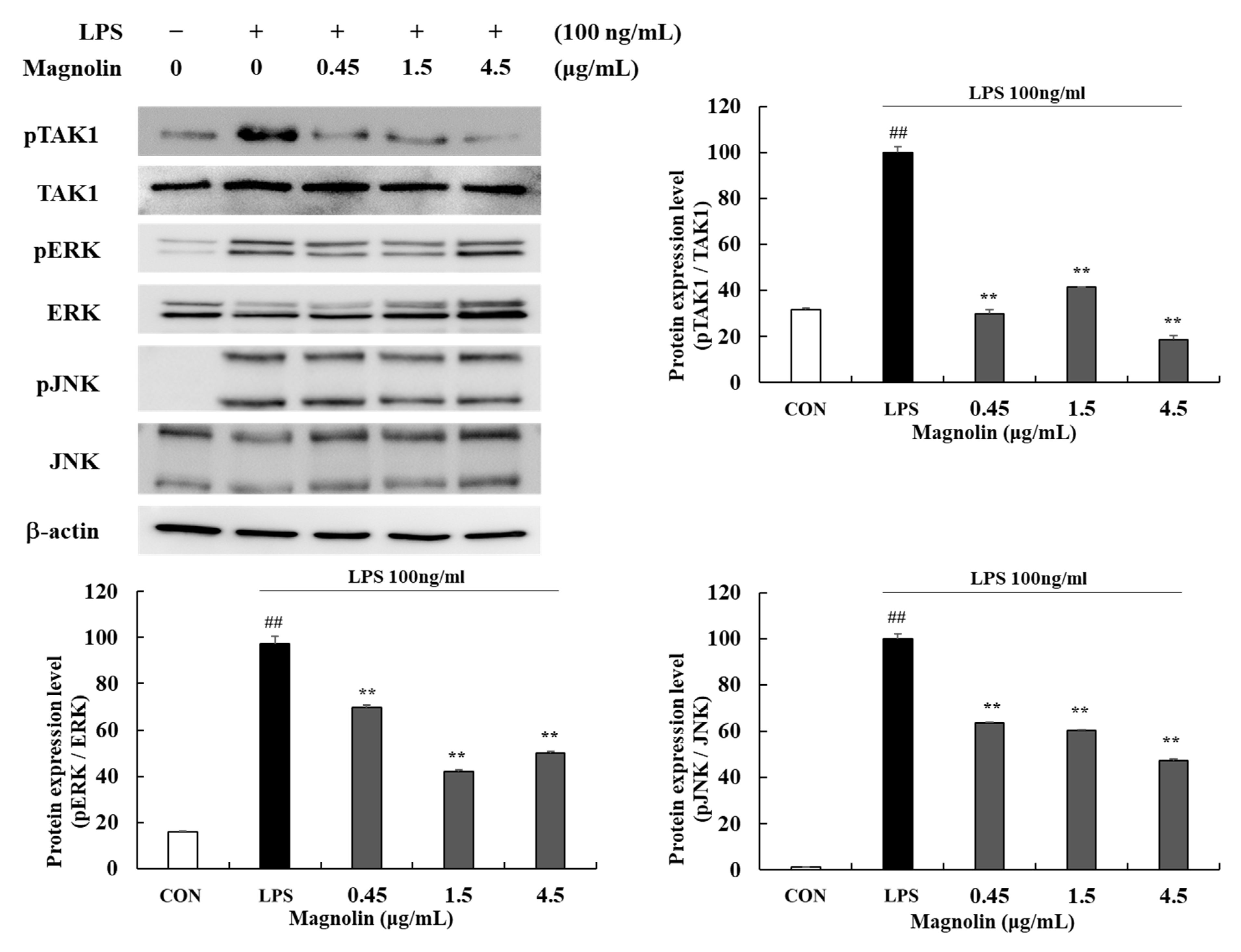
3.6. MKE/Magnolin Inhibits TAK1/MAPK Signaling Pathways
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jain, S.; Darveau, R.P. Contribution of Porphyromonas gingivalis lipopolysachharide to periodontitis. Periodontol. 2000 2010, 54, 53. [Google Scholar] [CrossRef] [PubMed]
- Hajishengallis, G.; Darveau, R.P.; Curtis, M.A. The keystone-pathogen hypothesis. Nat. Rev. Microbiol. 2012, 10, 717–725. [Google Scholar] [CrossRef] [PubMed]
- Yucel-Lindberg, T.; Båge, T. Inflammatory mediators in the pathogenesis of periodontitis. Expert Rev. Mol. Med. 2013, 15, e7. [Google Scholar] [CrossRef] [PubMed]
- WHO. References. In Global Oral Health Status Report: Towards Universal Health Coverage for Oral Health by 2030; World Health Organization, Ed.; World Health Organization: Geneva, Switzerland, 2022; ISBN 978-92-4-006148-4. [Google Scholar]
- Cekici, A.; Kantarci, A.; Hasturk, H.; Van Dyke, T.E. Inflammatory and immune pathways in the pathogenesis of periodontal disease. Periodontol. 2000 2014, 64, 57–80. [Google Scholar] [CrossRef] [PubMed]
- Zemedikun, D.T.; Chandan, J.S.; Raindi, D.; Rajgor, A.D.; Gokhale, K.M.; Thomas, T.; Falahee, M.; De Pablo, P.; Lord, J.M.; Raza, K. Burden of chronic diseases associated with periodontal diseases: A retrospective cohort study using UK primary care data. BMJ open 2021, 11, e048296. [Google Scholar] [CrossRef]
- Cardoso, E.M.; Reis, C.; Manzanares-Céspedes, M.C. Chronic periodontitis, inflammatory cytokines, and interrelationship with other chronic diseases. Postgrad. Med. 2018, 130, 98–104. [Google Scholar] [CrossRef]
- How, K.Y.; Song, K.P.; Chan, K.G. Porphyromonas gingivalis: An overview of periodontopathic pathogen below the gum line. Front. Microbiol. 2016, 7, 53. [Google Scholar] [CrossRef]
- Tokutomi, F.; Wada-Takahashi, S.; Sugiyama, S.; Toyama, T.; Sato, T.; Hamada, N.; Tsukinoki, K.; Takahashi, S.-S.; Lee, M.C.-I. Porphyromonas gingivalis-induced alveolar bone loss is accelerated in the stroke-prone spontaneously hypertensive rat. Arch. Oral Biol. 2015, 60, 911–918. [Google Scholar] [CrossRef]
- Aleksijević, L.H.; Aleksijević, M.; Škrlec, I.; Šram, M.; Šram, M.; Talapko, J. Porphyromonas gingivalis Virulence Factors and Clinical Significance in Periodontal Disease and Coronary Artery Diseases. Pathogens 2022, 11, 1173. [Google Scholar] [CrossRef]
- Kibune, R.; Muraoka, K.; Morishita, M.; Ariyoshi, W.; Awano, S. Relationship between Dynamics of TNF-α and Its Soluble Receptors in Saliva and Periodontal Health State. Dent. J. 2022, 10, 25. [Google Scholar] [CrossRef]
- Khosravi, R.; Ka, K.; Huang, T.; Khalili, S.; Nguyen, B.H.; Nicolau, B.; Tran, S.D. Tumor necrosis factor-α and interleukin-6: Potential interorgan inflammatory mediators contributing to destructive periodontal disease in obesity or metabolic syndrome. Mediat. Inflamm. 2013, 2013, 728987. [Google Scholar] [CrossRef] [PubMed]
- Yao, Z.; Getting, S.J.; Locke, I.C. Regulation of TNF-induced osteoclast differentiation. Cells 2021, 11, 132. [Google Scholar] [CrossRef]
- Kong, L.; Smith, W.; Hao, D. Overview of RAW264. 7 for osteoclastogensis study: Phenotype and stimuli. J. Cell. Mol. Med. 2019, 23, 3077–3087. [Google Scholar] [CrossRef] [PubMed]
- Skurska, A.; Pietruska, M.; Paniczko-Drężek, A.; Dolińska, E.; Żelazowska-Rutkowska, B.; Żak, J.; Pietruski, J.; Milewski, R.; Wysocka, J. Evaluation of the influence of ozonotherapy on the clinical parameters and MMP levels in patients with chronic and aggressive periodontitis. Adv. Med. Sci. 2010, 55, 297–307. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Cox, S.; Eley, B.; Mäntylä, P.; Rönkä, H.; Sorsa, T. Matrix metalloproteinase-8 levels and elastase activities in gingival crevicular fluid from chronic adult periodontitis patients. J. Clin. Periodontol. 2000, 27, 366–369. [Google Scholar] [CrossRef]
- Sirniö, P.; Tuomisto, A.; Tervahartiala, T.; Sorsa, T.; Klintrup, K.; Karhu, T.; Herzig, K.-H.; Mäkelä, J.; Karttunen, T.J.; Salo, T. High-serum MMP-8 levels are associated with decreased survival and systemic inflammation in colorectal cancer. Br. J. Cancer 2018, 119, 213–219. [Google Scholar] [CrossRef]
- Checchi, V.; Maravic, T.; Bellini, P.; Generali, L.; Consolo, U.; Breschi, L.; Mazzoni, A. The role of matrix metalloproteinases in periodontal disease. Int. J. Environ. Res. Public Health 2020, 17, 4923. [Google Scholar] [CrossRef]
- Luchian, I.; Goriuc, A.; Sandu, D.; Covasa, M. The Role of Matrix Metalloproteinases (MMP-8, MMP-9, MMP-13) in Periodontal and Peri-Implant Pathological Processes. Int. J. Mol. Sci. 2022, 23, 1806. [Google Scholar] [CrossRef]
- Balli, U.; Cetinkaya, B.O.; Keles, G.C.; Keles, Z.P.; Guler, S.; Sogut, M.U.; Erisgin, Z. Assessment of MMP-1, MMP-8 and TIMP-2 in experimental periodontitis treated with kaempferol. J. Periodontal Implant. Sci. 2016, 46, 84–95. [Google Scholar] [CrossRef]
- Elgezawi, M.; Haridy, R.; Almas, K.; Abdalla, M.A.; Omar, O.; Abuohashish, H.; Elembaby, A.; Christine Wölfle, U.; Siddiqui, Y.; Kaisarly, D. Matrix Metalloproteinases in Dental and Periodontal Tissues and Their Current Inhibitors: Developmental, Degradational and Pathological Aspects. Int. J. Mol. Sci. 2022, 23, 8929. [Google Scholar] [CrossRef]
- Ghosh, P.; Muthuraj, T.S.; Bandyopadhyay, P.; Swarnakar, S.; Sarkar, P.; Varatharajan, A. Expression of matrix metalloproteinase-9 in gingival tissue biopsy in patients with slowly/moderately and rapidly progressing periodontitis: An observational study. J. Indian Soc. Periodontol. 2021, 25, 386. [Google Scholar] [PubMed]
- Zahednasab, H.; Harirchian, M.H.; Karampoor, S.; Keyvani, H. MMP-9 as a biomarker of PML development in MS patients receiving Natalizumab. Ann. Neurol. 2017, 82, 647–648. [Google Scholar] [CrossRef]
- Unemori, E.N.; Bair, M.; Bauer, E.; Amento, E. Stromelysin expression regulates collagenase activation in human fibroblasts. Dissociable control of two metalloproteinases by interferon-gamma. J. Biol. Chem. 1991, 266, 23477–23482. [Google Scholar] [CrossRef] [PubMed]
- Laronha, H.; Caldeira, J. Structure and function of human matrix metalloproteinases. Cells 2020, 9, 1076. [Google Scholar] [CrossRef] [PubMed]
- Chung, I.-M.; Malathy, R.; Priyadharshini, R.; Hemapriya, V.; Kim, S.-H.; Prabakaran, M. Inhibition of mild steel corrosion using Magnolia kobus extract in sulphuric acid medium. Mater. Today Commun. 2020, 25, 101687. [Google Scholar] [CrossRef]
- Ghorbani, F.; Haghgoo, R.; Aramjoo, H.; Rakhshandeh, H.; Jamehdar, S.A.; Zare-Bidaki, M. The antibacterial effect of Magnolia mouthwash on the levels of salivary Streptococcus mutans in dental plaque: A randomized, single-blind, placebo-controlled trial. Iran. J. Microbiol. 2021, 13, 104. [Google Scholar] [CrossRef]
- Kim, J.-Y.; Kim, K.-H.; Kwag, E.-H.; Seol, Y.J.; Lee, Y.M.; Ku, Y.; Rhyu, I.-C. Magnoliae Cortex and maize modulate Porphyromonas gingivalis-induced inflammatory reactions. J. Periodontal Implant. Sci. 2018, 48, 70. [Google Scholar] [CrossRef]
- Lu, S.-H.; Hsu, W.-L.; Chen, T.-H.; Chou, T.-C. Activation of Nrf2/HO-1signaling pathway involves the anti-inflammatory activity of magnolol in Porphyromonas gingivalis lipopolysaccharide-stimulated mouse RAW 264.7 macrophages. Int. Immunopharmacol. 2015, 29, 770–778. [Google Scholar] [CrossRef]
- Pan, J.-X.; Hensens, O.D.; Zink, D.L.; Chang, M.N.; Hwang, S.-B. Lignans with platelet activating factor antagonist activity from Magnolia biondii. Phytochemistry 1987, 26, 1377–1379. [Google Scholar] [CrossRef]
- Shen, Y.; Pang, E.C.; Xue, C.C.; Zhao, Z.; Lin, J.; Li, C.G. Inhibitions of mast cell-derived histamine release by different Flos Magnoliae species in rat peritoneal mast cells. Phytomedicine 2008, 15, 808–814. [Google Scholar] [CrossRef]
- Wang, F.; Zhang, G.; Zhou, Y.; Gui, D.; Li, J.; Xing, T.; Wang, N. Magnolin protects against contrast-induced nephropathy in rats via antioxidation and antiapoptosis. Oxid. Med. Cell. Longev. 2014, 2014, 203458. [Google Scholar] [CrossRef] [PubMed]
- Xu, K.; Gao, Y.; Yang, L.; Liu, Y.; Wang, C. Magnolin exhibits anti-inflammatory effects on chondrocytes via the NF-κB pathway for attenuating anterior cruciate ligament transection-induced osteoarthritis. Connect. Tissue Res. 2021, 62, 475–484. [Google Scholar] [CrossRef] [PubMed]
- Hajishengallis, G. Immunomicrobial pathogenesis of periodontitis: Keystones, pathobionts, and host response. Trends Immunol. 2014, 35, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Chae, B.S. Pretreatment of low-dose and super-low-dose LPS on the production of in vitro LPS-induced inflammatory mediators. Toxicol. Res. 2018, 34, 65–73. [Google Scholar] [CrossRef]
- Vergadi, E.; Vaporidi, K.; Tsatsanis, C. Regulation of endotoxin tolerance and compensatory anti-inflammatory response syndrome by non-coding RNAs. Front. Immunol. 2018, 9, 2705. [Google Scholar] [CrossRef]
- Wang, Y.; Tu, Q.; Yan, W.; Xiao, D.; Zeng, Z.; Ouyang, Y.; Huang, L.; Cai, J.; Zeng, X.; Chen, Y.-J. CXC195 suppresses proliferation and inflammatory response in LPS-induced human hepatocellular carcinoma cells via regulating TLR4-MyD88-TAK1-mediated NF-κB and MAPK pathway. Biochem. Biophys. Res. Commun. 2015, 456, 373–379. [Google Scholar] [CrossRef]
- Liu, T.; Zhang, L.; Joo, D.; Sun, S.-C. NF-κB signaling in inflammation. Signal Transduct. Target. Ther. 2017, 2, 17023. [Google Scholar] [CrossRef]
- Gao, H.; Sun, W.; Zhao, J.; Wu, X.; Lu, J.-J.; Chen, X.; Xu, Q.-M.; Khan, I.A.; Yang, S. Tanshinones and diethyl blechnics with anti-inflammatory and anti-cancer activities from Salvia miltiorrhiza Bunge (Danshen). Sci. Rep. 2016, 6, 33720. [Google Scholar] [CrossRef]
- Li, Q.; Valerio, M.S.; Kirkwood, K.L. MAPK usage in periodontal disease progression. J. Signal Transduct. 2012, 2012, 308943. [Google Scholar] [CrossRef]
- Sun, M.; Ji, Y.; Li, Z.; Chen, R.; Zhou, S.; Liu, C.; Du, M. Ginsenoside Rb3 inhibits pro-inflammatory cytokines via MAPK/AKT/NF-κB pathways and attenuates rat alveolar bone resorption in response to porphyromonas gingivalis LPS. Molecules 2020, 25, 4815. [Google Scholar] [CrossRef]
- Algate, K.; Haynes, D.; Bartold, P.; Crotti, T.; Cantley, M. The effects of tumour necrosis factor-α on bone cells involved in periodontal alveolar bone loss; osteoclasts, osteoblasts and osteocytes. J. Periodontal Res. 2016, 51, 549–566. [Google Scholar] [CrossRef] [PubMed]
- Cheng, R.; Wu, Z.; Li, M.; Shao, M.; Hu, T. Interleukin-1β is a potential therapeutic target for periodontitis: A narrative review. Int. J. Oral Sci. 2020, 12, 2. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Tang, J.; Zuo, Y.; Yu, Y.; Luo, P.; Yao, X.; Dong, Y.; Wang, P.; Liu, L.; Zhou, H. Stauntoside B inhibits macrophage activation by inhibiting NF-κB and ERK MAPK signalling. Pharmacol. Res. 2016, 111, 303–315. [Google Scholar] [CrossRef] [PubMed]
- Gomes, F.I.F.; Aragão, M.G.B.; Barbosa, F.C.B.; Bezerra, M.M.; Pinto, V.d.P.T.; Chaves, H.V. Inflammatory cytokines interleukin-1β and tumour necrosis factor-α-novel biomarkers for the detection of periodontal diseases: A literature review. J. Oral Maxillofac. Res. 2016, 7, e2. [Google Scholar] [CrossRef] [PubMed]
- Korotkova, M.; Jakobsson, P.-J. Microsomal prostaglandin e synthase-1 in rheumatic diseases. Front. Pharmacol. 2011, 1, 146. [Google Scholar] [CrossRef]
- LaRock, C.N.; Todd, J.; LaRock, D.L.; Olson, J.; O’Donoghue, A.J.; Robertson, A.A.; Cooper, M.A.; Hoffman, H.M.; Nizet, V. IL-1β is an innate immune sensor of microbial proteolysis. Sci. Immunol. 2016, 1, eaah3539. [Google Scholar] [CrossRef] [PubMed]
- Giacomelli, C.; Natali, L.; Nisi, M.; De Leo, M.; Daniele, S.; Costa, B.; Graziani, F.; Gabriele, M.; Braca, A.; Trincavelli, M.L. Negative effects of a high tumour necrosis factor-α concentration on human gingival mesenchymal stem cell trophism: The use of natural compounds as modulatory agents. Stem Cell Res. Ther. 2018, 9, 135. [Google Scholar] [CrossRef]
- Cho, B.H.; Jung, Y.H.; Kim, D.J.; Woo, B.H.; Jung, J.E.; Lee, J.H.; Choi, Y.W.; Park, H.R. Acetylshikonin suppresses invasion of Porphyromonas gingivalis-infected YD10B oral cancer cells by modulating the interleukin-8/matrix metalloproteinase axis. Mol. Med. Report. 2018, 17, 2327–2334. [Google Scholar]
- Parmar, N.K.; Nisha, K.; Guru, S.; Padmanabhan, S. Role of matrixmetalloproteinases in periodontal disease—A review. Biomed. J. Sci. Tech. Res. 2018, 2, 2099–2104. [Google Scholar]
- Birkedal-Hansen, H. Role of matrix metalloproteinases in human periodontal diseases. J. Periodontol. 1993, 64, 474–484. [Google Scholar]
- Sorsa, T.; Tjäderhane, L.; Salo, T. Matrix metalloproteinases (MMPs) in oral diseases. Oral Dis. 2004, 10, 311–318. [Google Scholar] [CrossRef]
- Popat, R.P.; Bhavsar, N.V.; Popat, P.R. Gingival crevicular fluid levels of Matrix Metalloproteinase-1 (MMP-1) and Tissue Inhibitor of Metalloproteinase-1 (TIMP-1) in periodontal health and disease. Singap. Dent. J. 2014, 35, 59–64. [Google Scholar] [CrossRef] [PubMed]
- Khuda, F.; Anuar, N.N.M.; Baharin, B.; Nasruddin, N.S.; Khuda, F.; Anuar, N.; Baharin, B.; Nasruddin, N. A mini review on the associations of matrix metalloproteinases (MMPs)-1,-8,-13 with periodontal disease. AIMS Mol. Sci. 2021, 8, 13–31. [Google Scholar] [CrossRef]
- De Morais, E.; Pinheiro, J.; Leite, R.; Santos, P.; Barboza, C.; Freitas, R. Matrix metalloproteinase-8 levels in periodontal disease patients: A systematic review. J. Periodontal Res. 2018, 53, 156–163. [Google Scholar] [CrossRef]
- Ghodpage, P.S.; Kolte, R.A.; Kolte, A.P.; Gupta, M. Influence of phase I periodontal therapy on levels of matrix metalloproteinase 1 and tissue inhibitor of metalloproteinase 1. Saudi Dent. J. 2014, 26, 171–175. [Google Scholar] [CrossRef] [PubMed]
- Escalona, L.A.; Mastromatteo-Alberga, P.; Correnti, M. Cytokine and metalloproteinases in gingival fluid from patients with chronic periodontitis. Investig. Clin. 2016, 57, 131–142. [Google Scholar]
- Meydhyono, W.; Nasution, A.H.; Ilyas, S.; Ervina, I.; Primasari, A. Evaluation of salivary matrix metallo proteinase-13 and tissue inhibitor of metalloproteinase-1 levels in patients with chronic periodontitis. Nveo-Nat. Volatiles Essent. Oils J.|Nveo 2021, 8, 4733–4742. [Google Scholar]
- Yang, Y.-H.; Li, D.-L.; Bi, X.-Y.; Sun, L.; Yu, X.-J.; Fang, H.-L.; Miao, Y.; Zhao, M.; He, X.; Liu, J.-J. Acetylcholine inhibits LPS-induced MMP-9 production and cell migration via the a7 nAChR-JAK2/STAT3 pathway in RAW264. 7 cells. Cell. Physiol. Biochem. 2015, 36, 2025–2038. [Google Scholar] [CrossRef]
- Steenport, M.; Khan, K.F.; Du, B.; Barnhard, S.E.; Dannenberg, A.J.; Falcone, D.J. Matrix metalloproteinase (MMP)-1 and MMP-3 induce macrophage MMP-9: Evidence for the role of TNF-α and cyclooxygenase-2. J. Immunol. 2009, 183, 8119–8127. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, H.-J.; Lee, S.-J.; Lee, S.-K.; Choi, B.-K.; Lee, D.-R. Magnolia kobus Extract Inhibits Periodontitis-Inducing Mediators in Porphyromonas gingivalis Lipopolysaccharide-Activated RAW 264.7 Cells. Curr. Issues Mol. Biol. 2023, 45, 538-554. https://doi.org/10.3390/cimb45010036
Lee H-J, Lee S-J, Lee S-K, Choi B-K, Lee D-R. Magnolia kobus Extract Inhibits Periodontitis-Inducing Mediators in Porphyromonas gingivalis Lipopolysaccharide-Activated RAW 264.7 Cells. Current Issues in Molecular Biology. 2023; 45(1):538-554. https://doi.org/10.3390/cimb45010036
Chicago/Turabian StyleLee, Hae-Jin, So-Jung Lee, Sung-Kwon Lee, Bong-Keun Choi, and Dong-Ryung Lee. 2023. "Magnolia kobus Extract Inhibits Periodontitis-Inducing Mediators in Porphyromonas gingivalis Lipopolysaccharide-Activated RAW 264.7 Cells" Current Issues in Molecular Biology 45, no. 1: 538-554. https://doi.org/10.3390/cimb45010036
APA StyleLee, H.-J., Lee, S.-J., Lee, S.-K., Choi, B.-K., & Lee, D.-R. (2023). Magnolia kobus Extract Inhibits Periodontitis-Inducing Mediators in Porphyromonas gingivalis Lipopolysaccharide-Activated RAW 264.7 Cells. Current Issues in Molecular Biology, 45(1), 538-554. https://doi.org/10.3390/cimb45010036





