Insights into Advanced Neurological Dysfunction Mechanisms Following DBS Surgery in Parkinson’s Patients: Neuroinflammation and Pyroptosis
Abstract
1. Introduction
2. Activation of Astrocytes and Microglia Is the Beginning of Neuroinflammation
2.1. Activation of Microglia
2.2. Activation of Astrocytes
2.3. Crosstalk between Microglia and Astrocytes
3. Neuroinflammation Occurs as the Result of Multifactorial Synergy including Astrocytes and Microglia
3.1. Astrocytes Interact with Microglia to Induce Neuroinflammation
3.2. Other Factors Acting on Neurons May Induce Downstream Inflammation
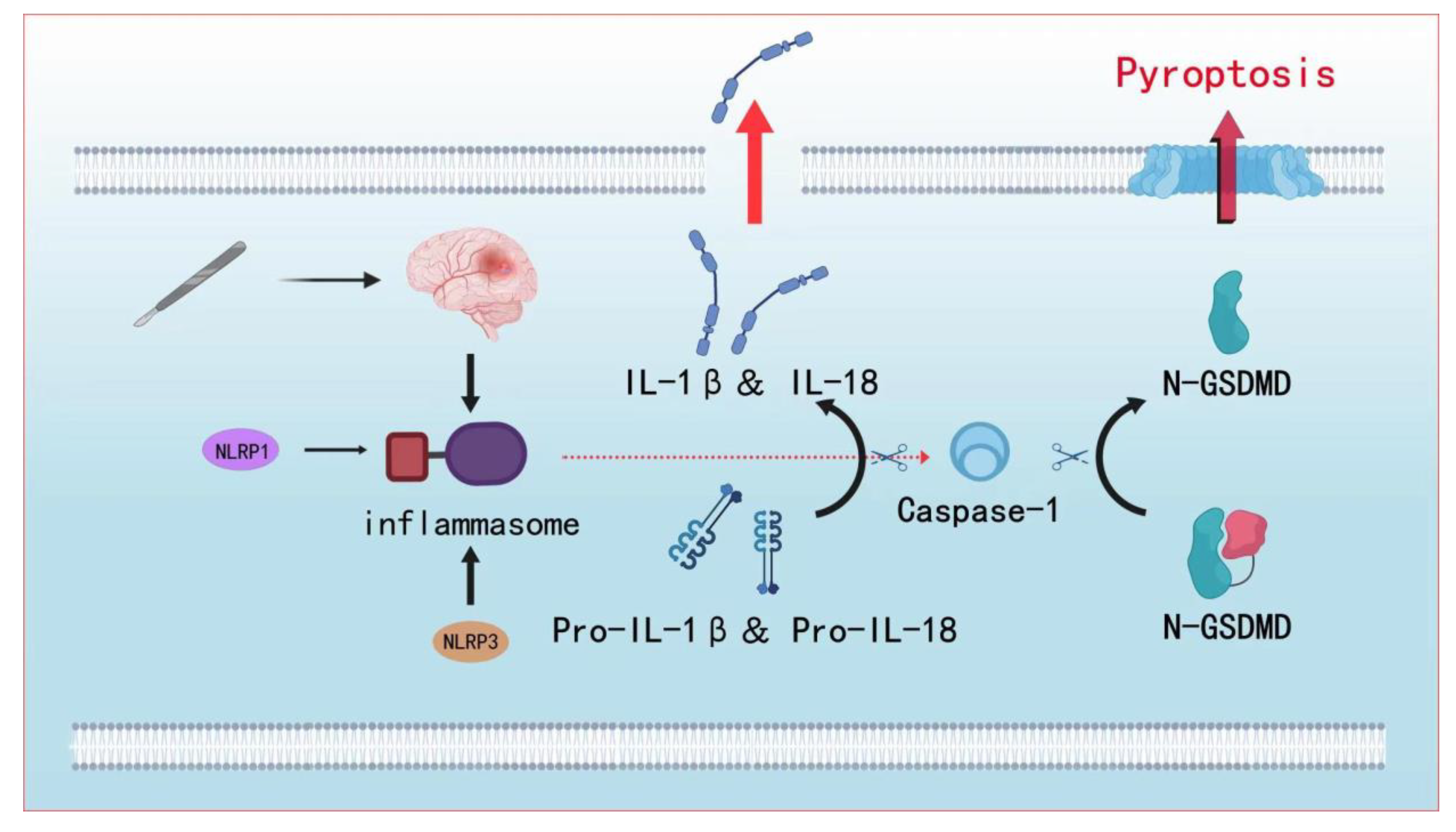
4. Neuroinflammation-Induced Pyroptosomal Formation May Promote Consciousness Disorders
4.1. Inflammasome Formation
4.2. Pyroptosis Leads to Language and Consciousness Disorders
5. Therapeutic Prospects of Neuroprotection: Targeting the Microglia–Astrocytes Interaction to Regulate Neuroinflammation
5.1. MAO-B Inhibitors
5.2. Drugs That Inhibit the Activation of Microglia and Astrocytes
5.3. Neurotrophic-Factor-Based Drugs
5.4. Iron Chelator Drugs
| Targets | Drugs | Type of Drugs | Therapeutic Effect |
|---|---|---|---|
| MAO-B | Selegiline [87] | MAO-B inhibitor | Enhances antioxidant capacity and reduces oxidative stress |
| Rasagiline [88] | |||
| Microglia or astrocyte activation | Cannabidiol [89] | Plant cannabinoids | Activates the astrocyte TRPV1-CNTF pathway to exert anti-inflammatory and neuroprotective effects |
| Dexmdetomdine [91] | α2-adrenoceptor | Upregulates the neurotrophin BDNF expression, and inhibits activated microglia and astrocytes | |
| NLY01 [95] | GLP-1R agonist | Blocks microglial activation and A1 astrocyte production | |
| Baicalein [96] | Flavonoid compound | Reduces astrocyte activation and inflammasome activation, inhibits the activation of NF-κB signaling pathway, and inhibits MAPK phosphorylation | |
| DHT [100] | Androgens | Microglia inhibit LPS activation causing inflammation induced by the TLR4-mediated NF-B and MAPK signaling pathway | |
| GDNF | Curcumin [101] | Neurotrophic factor-based drugs | Stimulation of Trk/PI3K signaling to restore neuronal regeneration and reduce the levels of tumor necrosis factor-α (TNF-α) and caspase activity, thereby increasing the levels of brain-derived neurotrophic factor (BDNF) |
| Intracellular iron | DFO [109] | Iron chelator drugs | Removal of intracellular iron, thereby reducing ROS production and reducing misfolding and aggregation of certain proteins |
| DFP [110] |
6. Hardware and Anesthesia of DBS Surgery
7. Discussion
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dorsey, E.R.; Bloem, B.R. The Parkinson Pandemic-A Call to Action. JAMA Neurol. 2018, 75, 9–10. [Google Scholar] [CrossRef]
- Ascherio, A.; Schwarzschild, M.A. The epidemiology of Parkinson’s disease: Risk factors and prevention. Lancet Neurol. 2016, 15, 1257–1272. [Google Scholar] [CrossRef] [PubMed]
- Fahn, S. The history of dopamine and levodopa in the treatment of Parkinson’s disease. Mov. Disord. 2008, 23 (Suppl. S3), S497–S508. [Google Scholar] [CrossRef] [PubMed]
- Mottaghi, S.; Buchholz, O.; Hofmann, U.G. Systematic Evaluation of DBS Parameters in the Hemi-Parkinsonian Rat Model. Front. Neurosci. 2020, 14, 561008. [Google Scholar] [CrossRef] [PubMed]
- García-Gomar, M.G.; Concha, L.; Soto-Abraham, J.; Tournier, J.D.; Aguado-Carrillo, G.; Velasco-Campos, F. Long-Term Improvement of Parkinson Disease Motor Symptoms Derived from Lesions of Prelemniscal Fiber Tract Components. Oper. Neurosurg. 2020, 19, 539–550. [Google Scholar] [CrossRef]
- Chiken, S.; Nambu, A. Mechanism of Deep Brain Stimulation: Inhibition, Excitation, or Disruption? Neuroscientist 2016, 22, 313–322. [Google Scholar] [CrossRef]
- Patel, P.D.; Patel, N.V.; Davidson, C.; Danish, S.F. The Role of MRgLITT in Overcoming the Challenges in Managing Infield Recurrence After Radiation for Brain Metastasis. Neurosurgery 2016, 79 (Suppl. S1), S40–S58. [Google Scholar] [CrossRef]
- MRgFUS-Mediated Antibody Delivery Improves Drug Uptake across the BBB. Cancer Discov. 2021, 11, 2957. [CrossRef]
- Feyissa, A.M.; Tatum, W.O. Adult EEG. Handb. Clin. Neurol. 2019, 160, 103–124. [Google Scholar] [CrossRef]
- Stern, M.A.; Isbaine, F.; Qiu, D.; Riley, J.P.; Boulis, N.M.; Gross, R.E. Radiofrequency Ablation Through Previously Effective Deep Brain Stimulation Leads for Parkinson Disease: A Retrospective Series. World Neurosurg. 2020, 144, e750–e765. [Google Scholar] [CrossRef]
- Umemura, A.; Oyama, G.; Shimo, Y.; Hattori, N. Deep brain stimulation for Parkinson’s disease. Nihon Rinsho 2017, 75, 83–88. [Google Scholar]
- Maier, F.; Lewis, C.J.; Horstkoetter, N.; Eggers, C.; Kalbe, E.; Maarouf, M.; Kuhn, J.; Zurowski, M.; Moro, E.; Woopen, C.; et al. Patients’ expectations of deep brain stimulation, and subjective perceived outcome related to clinical measures in Parkinson’s disease: A mixed-method approach. J. Neurol. Neurosurg. Psychiatry 2013, 84, 1273–1281. [Google Scholar] [CrossRef] [PubMed]
- Odekerken, V.J.; Boel, J.A.; Geurtsen, G.J.; Schmand, B.A.; Dekker, I.P.; de Haan, R.J.; Schuurman, P.R.; de Bie, R.M. Neuropsychological outcome after deep brain stimulation for Parkinson disease. Neurology 2015, 84, 1355–1361. [Google Scholar] [CrossRef]
- Krack, P.; Batir, A.; Van Blercom, N.; Chabardes, S.; Fraix, V.; Ardouin, C.; Koudsie, A.; Limousin, P.D.; Benazzouz, A.; LeBas, J.F.; et al. Five-year follow-up of bilateral stimulation of the subthalamic nucleus in advanced Parkinson’s disease. N. Engl. J. Med. 2003, 349, 1925–1934. [Google Scholar] [CrossRef] [PubMed]
- Llanque, S.M.; Enriquez, M.; Cheng, A.L.; Doty, L.; Brotto, M.A.; Kelly, P.J.; Niedens, M.; Caserta, M.S.; Savage, L.M. The family series workshop: A community-based psychoeducational intervention. Am. J. Alzheimers Dis. Other Demen. 2015, 30, 573–583. [Google Scholar] [CrossRef] [PubMed]
- Funkiewiez, A.; Ardouin, C.; Caputo, E.; Krack, P.; Fraix, V.; Klinger, H.; Chabardes, S.; Foote, K.; Benabid, A.L.; Pollak, P. Long term effects of bilateral subthalamic nucleus stimulation on cognitive function, mood, and behaviour in Parkinson’s disease. J. Neurol. Neurosurg. Psychiatry 2004, 75, 834–839. [Google Scholar] [CrossRef] [PubMed]
- Ory-Magne, F.; Brefel-Courbon, C.; Simonetta-Moreau, M.; Fabre, N.; Lotterie, J.A.; Chaynes, P.; Berry, I.; Lazorthes, Y.; Rascol, O. Does ageing influence deep brain stimulation outcomes in Parkinson’s disease? Mov. Disord. 2007, 22, 1457–1463. [Google Scholar] [CrossRef]
- Prinz, M.; Jung, S.; Priller, J. Microglia Biology: One Century of Evolving Concepts. Cell 2019, 179, 292–311. [Google Scholar] [CrossRef] [PubMed]
- Blomstedt, P.; Hariz, M.I. Are complications less common in deep brain stimulation than in ablative procedures for movement disorders? Stereotact. Funct. Neurosurg. 2006, 84, 72–81. [Google Scholar] [CrossRef] [PubMed]
- Boviatsis, E.J.; Stavrinou, L.C.; Themistocleous, M.; Kouyialis, A.T.; Sakas, D.E. Surgical and hardware complications of deep brain stimulation. A seven-year experience and review of the literature. Acta Neurochir. 2010, 152, 2053–2062. [Google Scholar] [CrossRef]
- Lim, E.W.; Aarsland, D.; Ffytche, D.; Taddei, R.N.; van Wamelen, D.J.; Wan, Y.M.; Tan, E.K.; Ray Chaudhuri, K. Amyloid-β and Parkinson’s disease. J. Neurol. 2019, 266, 2605–2619. [Google Scholar] [CrossRef] [PubMed]
- Lana, D.; Ugolini, F.; Giovannini, M.G. Space-Dependent Glia-Neuron Interplay in the Hippocampus of Transgenic Models of β-Amyloid Deposition. Int. J. Mol. Sci. 2020, 21, 9441. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, R.C.; Sosa, J.C.; Gardeck, A.M.; Baez, A.S.; Lee, C.H.; Wessling-Resnick, M. Inflammation-induced iron transport and metabolism by brain microglia. J. Biol. Chem. 2018, 293, 7853–7863. [Google Scholar] [CrossRef]
- Fine, J.M.; Kosyakovsky, J.; Baillargeon, A.M.; Tokarev, J.V.; Cooner, J.M.; Svitak, A.L.; Faltesek, K.A.; Frey, W.H., 2nd; Hanson, L.R. Intranasal deferoxamine can improve memory in healthy C57 mice, suggesting a partially non-disease-specific pathway of functional neurologic improvement. Brain Behav. 2020, 10, e01536. [Google Scholar] [CrossRef]
- Volz, K. Conservation in the Iron Responsive Element Family. Genes 2021, 12, 1365. [Google Scholar] [CrossRef]
- Gong, L.; Tian, X.; Zhou, J.; Dong, Q.; Tan, Y.; Lu, Y.; Wu, J.; Zhao, Y.; Liu, X. Iron Dyshomeostasis Induces Binding of APP to BACE1 for Amyloid Pathology and Impairs APP/Fpn1 Complex in Microglia: Implication in Pathogenesis of Cerebral Microbleeds. Cell. Transplant. 2019, 28, 1009–1017. [Google Scholar] [CrossRef]
- Daneman, R.; Prat, A. The blood-brain barrier. Cold Spring Harb. Perspect. Biol. 2015, 7, a020412. [Google Scholar] [CrossRef]
- Li, Z.; Ni, C.; Xia, C.; Jaw, J.; Wang, Y.; Cao, Y.; Xu, M.; Guo, X. Calcineurin/nuclear factor-κB signaling mediates isoflurane-induced hippocampal neuroinflammation and subsequent cognitive impairment in aged rats. Mol. Med. Rep. 2017, 15, 201–209. [Google Scholar] [CrossRef]
- Yang, Z.; Liu, Y.; Yuan, F.; Li, Z.; Huang, S.; Shen, H.; Yuan, B. Sinomenine inhibits microglia activation and attenuates brain injury in intracerebral hemorrhage. Mol. Immunol. 2014, 60, 109–114. [Google Scholar] [CrossRef]
- Qin, Z.; Wang, P.Y.; Su, D.F.; Liu, X. miRNA-124 in Immune System and Immune Disorders. Front. Immunol. 2016, 7, 406. [Google Scholar] [CrossRef] [PubMed]
- Tang, Y.; Le, W. Differential Roles of M1 and M2 Microglia in Neurodegenerative Diseases. Mol. Neurobiol. 2016, 53, 1181–1194. [Google Scholar] [CrossRef] [PubMed]
- Bekris, L.M.; Khrestian, M.; Dyne, E.; Shao, Y.; Pillai, J.A.; Rao, S.M.; Bemiller, S.M.; Lamb, B.; Fernandez, H.H.; Leverenz, J.B. Soluble TREM2 and biomarkers of central and peripheral inflammation in neurodegenerative disease. J. Neuroimmunol. 2018, 319, 19–27. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, J.M.; Schardien, K.; Wigdahl, B.; Nonnemacher, M.R. Roles of neuropathology-associated reactive astrocytes: A systematic review. Acta Neuropathol. Commun. 2023, 11, 42. [Google Scholar] [CrossRef] [PubMed]
- Colombo, E.; Farina, C. Astrocytes: Key Regulators of Neuroinflammation. Trends Immunol. 2016, 37, 608–620. [Google Scholar] [CrossRef] [PubMed]
- Lyons, K.E.; Wilkinson, S.B.; Overman, J.; Pahwa, R. Surgical and hardware complications of subthalamic stimulation: A series of 160 procedures. Neurology 2004, 63, 612–616. [Google Scholar] [CrossRef]
- Joint, C.; Nandi, D.; Parkin, S.; Gregory, R.; Aziz, T. Hardware-related problems of deep brain stimulation. Mov. Disord. 2002, 17 (Suppl. S3), S175–S180. [Google Scholar] [CrossRef]
- Arocho-Quinones, E.V.; Pahapill, P.A. Non-Infectious Peri-Electrode Edema and Contrast Enhancement Following Deep Brain Stimulation Surgery. Neuromodulation 2016, 19, 872–876. [Google Scholar] [CrossRef] [PubMed]
- Liu, P.R.; Cao, F.; Zhang, Y.; Peng, S. Electroacupuncture reduces astrocyte number and oxidative stress in aged rats with surgery-induced cognitive dysfunction. J. Int. Med. Res. 2019, 47, 3860–3873. [Google Scholar] [CrossRef]
- Jack, C.S.; Arbour, N.; Manusow, J.; Montgrain, V.; Blain, M.; McCrea, E.; Shapiro, A.; Antel, J.P. TLR signaling tailors innate immune responses in human microglia and astrocytes. J. Immunol. 2005, 175, 4320–4330. [Google Scholar] [CrossRef]
- Scumpia, P.O.; Kelly, K.M.; Reeves, W.H.; Stevens, B.R. Double-stranded RNA signals antiviral and inflammatory programs and dysfunctional glutamate transport in TLR3-expressing astrocytes. Glia 2005, 52, 153–162. [Google Scholar] [CrossRef]
- Takeda, K.; Akira, S. Toll-like receptors. Curr. Protoc. Immunol. 2015, 109, 14.12.1–14.12.10. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.R.; Liu, J.C.; Bao, J.S.; Bai, Q.Q.; Wang, G.Q. Interaction of Microglia and Astrocytes in the Neurovascular Unit. Front. Immunol. 2020, 11, 1024. [Google Scholar] [CrossRef]
- Wang, Y.; Wang, S.; Zhang, W.; Liu, J.; Yang, Z.; Liu, C. Notch1 participates in the activation of autophagy in the hippocampus of type I diabetic mice. Neurochem. Int. 2021, 150, 105156. [Google Scholar] [CrossRef]
- Lambertsen, K.L.; Meldgaard, M.; Ladeby, R.; Finsen, B. A quantitative study of microglial-macrophage synthesis of tumor necrosis factor during acute and late focal cerebral ischemia in mice. J. Cereb. Blood Flow. Metab. 2005, 25, 119–135. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.H.; Oyarzabal, E.A.; Sung, Y.F.; Chu, C.H.; Wang, Q.; Chen, S.L.; Lu, R.B.; Hong, J.S. Microglial regulation of immunological and neuroprotective functions of astroglia. Glia 2015, 63, 118–131. [Google Scholar] [CrossRef] [PubMed]
- Kirkley, K.S.; Popichak, K.A.; Afzali, M.F.; Legare, M.E.; Tjalkens, R.B. Microglia amplify inflammatory activation of astrocytes in manganese neurotoxicity. J. Neuroinflammation 2017, 14, 99. [Google Scholar] [CrossRef]
- Pascual, O.; Ben Achour, S.; Rostaing, P.; Triller, A.; Bessis, A. Microglia activation triggers astrocyte-mediated modulation of excitatory neurotransmission. Proc. Natl. Acad. Sci. USA 2012, 109, E197–E205. [Google Scholar] [CrossRef]
- Xu, J.; Dong, H.; Qian, Q.; Zhang, X.; Wang, Y.; Jin, W.; Qian, Y. Astrocyte-derived CCL2 participates in surgery-induced cognitive dysfunction and neuroinflammation via evoking microglia activation. Behav. Brain Res. 2017, 332, 145–153. [Google Scholar] [CrossRef]
- Allaman, I.; Bélanger, M.; Magistretti, P.J. Astrocyte-neuron metabolic relationships: For better and for worse. Trends Neurosci. 2011, 34, 76–87. [Google Scholar] [CrossRef]
- McKimmie, C.S.; Graham, G.J. Astrocytes modulate the chemokine network in a pathogen-specific manner. Biochem. Biophys. Res. Commun. 2010, 394, 1006–1011. [Google Scholar] [CrossRef]
- Zhao, Q.; Che, X.; Zhang, H.; Fan, P.; Tan, G.; Liu, L.; Jiang, D.; Zhao, J.; Xiang, X.; Liang, Y.; et al. Thioredoxin-interacting protein links endoplasmic reticulum stress to inflammatory brain injury and apoptosis after subarachnoid haemorrhage. J. Neuroinflammation 2017, 14, 104. [Google Scholar] [CrossRef]
- Kwon, H.S.; Koh, S.H. Neuroinflammation in neurodegenerative disorders: The roles of microglia and astrocytes. Transl. Neurodegener. 2020, 9, 42. [Google Scholar] [CrossRef] [PubMed]
- Terrando, N.; Monaco, C.; Ma, D.; Foxwell, B.M.; Feldmann, M.; Maze, M. Tumor necrosis factor-alpha triggers a cytokine cascade yielding postoperative cognitive decline. Proc. Natl. Acad. Sci. USA 2010, 107, 20518–20522. [Google Scholar] [CrossRef]
- Saraswati, A.P.; Ali Hussaini, S.M.; Krishna, N.H.; Babu, B.N.; Kamal, A. Glycogen synthase kinase-3 and its inhibitors: Potential target for various therapeutic conditions. Eur. J. Med. Chem. 2018, 144, 843–858. [Google Scholar] [CrossRef] [PubMed]
- Zhang Wei, M.J. Research progress on molecular mechanism of cell pyrophosis and its relationship with disease. Pract. J. Card. Cereb. Pneumal Vasc. Dis. 2019, 27, 246–248. [Google Scholar]
- Song, N.; Liu, Z.S.; Xue, W.; Bai, Z.F.; Wang, Q.Y.; Dai, J.; Liu, X.; Huang, Y.J.; Cai, H.; Zhan, X.Y.; et al. NLRP3 Phosphorylation Is an Essential Priming Event for Inflammasome Activation. Mol. Cell. 2017, 68, 185–197.e186. [Google Scholar] [CrossRef]
- Femenía, T.; Giménez-Cassina, A.; Codeluppi, S.; Fernández-Zafra, T.; Katsu-Jiménez, Y.; Terrando, N.; Eriksson, L.I.; Gómez-Galán, M. Disrupted Neuroglial Metabolic Coupling after Peripheral Surgery. J. Neurosci. 2018, 38, 452–464. [Google Scholar] [CrossRef]
- Lv, Z.T.; Huang, J.M.; Zhang, J.M.; Zhang, J.M.; Guo, J.F.; Chen, A.M. Effect of Ulinastatin in the Treatment of Postperative Cognitive Dysfunction: Review of Current Literature. Biomed. Res. Int. 2016, 2016, 2571080. [Google Scholar] [CrossRef]
- An, P.; Xie, J.; Qiu, S.; Liu, Y.; Wang, J.; Xiu, X.; Li, L.; Tang, M. Hispidulin exhibits neuroprotective activities against cerebral ischemia reperfusion injury through suppressing NLRP3-mediated pyroptosis. Life Sci. 2019, 232, 116599. [Google Scholar] [CrossRef]
- Abbott, N.J.; Patabendige, A.A.; Dolman, D.E.; Yusof, S.R.; Begley, D.J. Structure and function of the blood-brain barrier. Neurobiol. Dis. 2010, 37, 13–25. [Google Scholar] [CrossRef]
- Huang, S.; Hu, H.; Cai, Y.H.; Hua, F. Effect of parecoxib in the treatment of postoperative cognitive dysfunction: A systematic review and meta-analysis. Medicine 2019, 98, e13812. [Google Scholar] [CrossRef]
- Obiero, C.W.; Ndiaye, A.G.W.; Sciré, A.S.; Kaunyangi, B.M.; Marchetti, E.; Gone, A.M.; Schütte, L.D.; Riccucci, D.; Auerbach, J.; Saul, A.; et al. A Phase 2a Randomized Study to Evaluate the Safety and Immunogenicity of the 1790GAHB Generalized Modules for Membrane Antigen Vaccine against Shigella sonnei Administered Intramuscularly to Adults from a Shigellosis-Endemic Country. Front. Immunol. 2017, 8, 1884. [Google Scholar] [CrossRef]
- Tang, Y.S.; Zhao, Y.H.; Zhong, Y.; Li, X.Z.; Pu, J.X.; Luo, Y.C.; Zhou, Q.L. Neferine inhibits LPS-ATP-induced endothelial cell pyroptosis via regulation of ROS/NLRP3/Caspase-1 signaling pathway. Inflamm. Res. 2019, 68, 727–738. [Google Scholar] [CrossRef] [PubMed]
- Cookson, B.T.; Brennan, M.A. Pro-inflammatory programmed cell death. Trends Microbiol. 2001, 9, 113–114. [Google Scholar] [CrossRef] [PubMed]
- LaRock, C.N.; Cookson, B.T. Burning down the house: Cellular actions during pyroptosis. PLoS Pathog. 2013, 9, e1003793. [Google Scholar] [CrossRef]
- Vande Walle, L.; Lamkanfi, M. Pyroptosis. Curr. Biol. 2016, 26, R568–R572. [Google Scholar] [CrossRef] [PubMed]
- Zychlinsky, A.; Prevost, M.C.; Sansonetti, P.J. Shigella flexneri induces apoptosis in infected macrophages. Nature 1992, 358, 167–169. [Google Scholar] [CrossRef] [PubMed]
- McKenzie, B.A.; Dixit, V.M.; Power, C. Fiery Cell Death: Pyroptosis in the Central Nervous System. Trends Neurosci. 2020, 43, 55–73. [Google Scholar] [CrossRef]
- Lénárt, N.; Brough, D.; Dénes, Á. Inflammasomes link vascular disease with neuroinflammation and brain disorders. J. Cereb. Blood Flow. Metab. 2016, 36, 1668–1685. [Google Scholar] [CrossRef] [PubMed]
- Yan, Y. Effect of N-acetylcysteine on Cognitive Function and Nuclear Factor Erythroid 2 Related Factor 2/Heme Oxygenase-1 Pathway in Mouse Models of Postoperative Cognitive Dysfunction. Acta Acad. Med. Sin. 2019, 41, 529–535. [Google Scholar] [CrossRef]
- Lee, B.L.; Mirrashidi, K.M.; Stowe, I.B.; Kummerfeld, S.K.; Watanabe, C.; Haley, B.; Cuellar, T.L.; Reichelt, M.; Kayagaki, N. ASC- and caspase-8-dependent apoptotic pathway diverges from the NLRC4 inflammasome in macrophages. Sci. Rep. 2018, 8, 3788. [Google Scholar] [CrossRef] [PubMed]
- Xue, Y.; Enosi Tuipulotu, D.; Tan, W.H.; Kay, C.; Man, S.M. Emerging Activators and Regulators of Inflammasomes and Pyroptosis. Trends Immunol. 2019, 40, 1035–1052. [Google Scholar] [CrossRef] [PubMed]
- Rathinam, V.A.; Fitzgerald, K.A. Inflammasome Complexes: Emerging Mechanisms and Effector Functions. Cell. 2016, 165, 792–800. [Google Scholar] [CrossRef] [PubMed]
- Broz, P. Immunology: Caspase target drives pyroptosis. Nature 2015, 526, 642–643. [Google Scholar] [CrossRef] [PubMed]
- Shi, J.; Zhao, Y.; Wang, K.; Shi, X.; Wang, Y.; Huang, H.; Zhuang, Y.; Cai, T.; Wang, F.; Shao, F. Cleavage of GSDMD by inflammatory caspases determines pyroptotic cell death. Nature 2015, 526, 660–665. [Google Scholar] [CrossRef]
- Liu, D.; Dong, Z.; Xiang, F.; Liu, H.; Wang, Y.; Wang, Q.; Rao, J. Dendrobium Alkaloids Promote Neural Function After Cerebral Ischemia-Reperfusion Injury Through Inhibiting Pyroptosis Induced Neuronal Death in both In Vivo and In Vitro Models. Neurochem. Res. 2020, 45, 437–454. [Google Scholar] [CrossRef] [PubMed]
- Biederer, T.; Kaeser, P.S.; Blanpied, T.A. Transcellular Nanoalignment of Synaptic Function. Neuron 2017, 96, 680–696. [Google Scholar] [CrossRef] [PubMed]
- Xu, L.; Qiu, X.; Wang, S.; Wang, Q.; Zhao, X.L. NMDA Receptor Antagonist MK801 Protects Against 1-Bromopropane-Induced Cognitive Dysfunction. Neurosci. Bull. 2019, 35, 347–361. [Google Scholar] [CrossRef]
- Licht, T.; Sasson, E.; Bell, B.; Grunewald, M.; Kumar, S.; Kreisel, T.; Ben-Zvi, A.; Keshet, E. Hippocampal neural stem cells facilitate access from circulation via apical cytoplasmic processes. eLife 2020, 9, e52134. [Google Scholar] [CrossRef] [PubMed]
- Parvathenani, L.K.; Tertyshnikova, S.; Greco, C.R.; Roberts, S.B.; Robertson, B.; Posmantur, R. P2X7 mediates superoxide production in primary microglia and is up-regulated in a transgenic mouse model of Alzheimer’s disease. J. Biol. Chem. 2003, 278, 13309–13317. [Google Scholar] [CrossRef]
- Skvarc, D.R.; Berk, M.; Byrne, L.K.; Dean, O.M.; Dodd, S.; Lewis, M.; Marriott, A.; Moore, E.M.; Morris, G.; Page, R.S.; et al. Post-Operative Cognitive Dysfunction: An exploration of the inflammatory hypothesis and novel therapies. Neurosci. Biobehav. Rev. 2018, 84, 116–133. [Google Scholar] [CrossRef] [PubMed]
- Chamorro, Á.; Lo, E.H.; Renú, A.; van Leyen, K.; Lyden, P.D. The future of neuroprotection in stroke. J. Neurol. Neurosurg. Psychiatry 2021, 92, 129–135. [Google Scholar] [CrossRef] [PubMed]
- Carradori, S.; D’Ascenzio, M.; Chimenti, P.; Secci, D.; Bolasco, A. Selective MAO-B inhibitors: A lesson from natural products. Mol. Divers. 2014, 18, 219–243. [Google Scholar] [CrossRef] [PubMed]
- Riederer, P.; Sofic, E.; Rausch, W.D.; Schmidt, B.; Reynolds, G.P.; Jellinger, K.; Youdim, M.B. Transition metals, ferritin, glutathione, and ascorbic acid in parkinsonian brains. J. Neurochem. 1989, 52, 515–520. [Google Scholar] [CrossRef]
- Mandel, S.; Grünblatt, E.; Riederer, P.; Gerlach, M.; Levites, Y.; Youdim, M.B. Neuroprotective strategies in Parkinson’s disease: An update on progress. CNS Drugs 2003, 17, 729–762. [Google Scholar] [CrossRef]
- Olanow, C.W.; Jankovic, J. Neuroprotective therapy in Parkinson’s disease and motor complications: A search for a pathogenesis-targeted, disease-modifying strategy. Mov. Disord. 2005, 20 (Suppl. S11), S3–S10. [Google Scholar] [CrossRef]
- Magyar, K. The pharmacology of selegiline. Int. Rev. Neurobiol. 2011, 100, 65–84. [Google Scholar] [CrossRef]
- Rascol, O.; Brooks, D.J.; Melamed, E.; Oertel, W.; Poewe, W.; Stocchi, F.; Tolosa, E. Rasagiline as an adjunct to levodopa in patients with Parkinson’s disease and motor fluctuations (LARGO, Lasting effect in Adjunct therapy with Rasagiline Given Once daily, study): A randomised, double-blind, parallel-group trial. Lancet 2005, 365, 947–954. [Google Scholar] [CrossRef]
- Mechoulam, R.; Panikashvili, D.; Shohami, E. Cannabinoids and brain injury: Therapeutic implications. Trends Mol. Med. 2002, 8, 58–61. [Google Scholar] [CrossRef]
- Giuliano, C.; Francavilla, M.; Ongari, G.; Petese, A.; Ghezzi, C.; Rossini, N.; Blandini, F.; Cerri, S. Neuroprotective and Symptomatic Effects of Cannabidiol in an Animal Model of Parkinson’s Disease. Int. J. Mol. Sci. 2021, 22, 8920. [Google Scholar] [CrossRef]
- Tasbihgou, S.R.; Barends, C.R.M.; Absalom, A.R. The role of dexmedetomidine in neurosurgery. Best. Pract. Res. Clin. Anaesthesiol. 2021, 35, 221–229. [Google Scholar] [CrossRef]
- Degos, V.; Charpentier, T.L.; Chhor, V.; Brissaud, O.; Lebon, S.; Schwendimann, L.; Bednareck, N.; Passemard, S.; Mantz, J.; Gressens, P. Neuroprotective effects of dexmedetomidine against glutamate agonist-induced neuronal cell death are related to increased astrocyte brain-derived neurotrophic factor expression. Anesthesiology 2013, 118, 1123–1132. [Google Scholar] [CrossRef]
- Xie, C.; Wang, Z.; Tang, J.; Shi, Z.; He, Z. The effect of dexmedetomidine post-treatment on the inflammatory response of astrocyte induced by lipopolysaccharide. Cell. Biochem. Biophys. 2015, 71, 407–412. [Google Scholar] [CrossRef] [PubMed]
- Yun, S.P.; Kam, T.I.; Panicker, N.; Kim, S.; Oh, Y.; Park, J.S.; Kwon, S.H.; Park, Y.J.; Karuppagounder, S.S.; Park, H.; et al. Block of A1 astrocyte conversion by microglia is neuroprotective in models of Parkinson’s disease. Nat. Med. 2018, 24, 931–938. [Google Scholar] [CrossRef] [PubMed]
- Teramoto, S.; Miyamoto, N.; Yatomi, K.; Tanaka, Y.; Oishi, H.; Arai, H.; Hattori, N.; Urabe, T. Exendin-4, a glucagon-like peptide-1 receptor agonist, provides neuroprotection in mice transient focal cerebral ischemia. J. Cereb. Blood Flow. Metab. 2011, 31, 1696–1705. [Google Scholar] [CrossRef] [PubMed]
- Yu, M.; Qi, B.; Xiaoxiang, W.; Xu, J.; Liu, X. Baicalein increases cisplatin sensitivity of A549 lung adenocarcinoma cells via PI3K/Akt/NF-κB pathway. Biomed. Pharmacother. 2017, 90, 677–685. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.; Park, H.R.; Ji, S.T.; Lee, Y.; Lee, J. Baicalein attenuates astroglial activation in the 1-methyl-4-phenyl-1,2,3,4-tetrahydropyridine-induced Parkinson’s disease model by downregulating the activations of nuclear factor-κB, ERK, and JNK. J. Neurosci. Res. 2014, 92, 130–139. [Google Scholar] [CrossRef]
- Cheng, Y.; He, G.; Mu, X.; Zhang, T.; Li, X.; Hu, J.; Xu, B.; Du, G. Neuroprotective effect of baicalein against MPTP neurotoxicity: Behavioral, biochemical and immunohistochemical profile. Neurosci. Lett. 2008, 441, 16–20. [Google Scholar] [CrossRef]
- He, X.; Wei, Z.; Zhou, E.; Chen, L.; Kou, J.; Wang, J.; Yang, Z. Baicalein attenuates inflammatory responses by suppressing TLR4 mediated NF-κB and MAPK signaling pathways in LPS-induced mastitis in mice. Int. Immunopharmacol. 2015, 28, 470–476. [Google Scholar] [CrossRef]
- Giatti, S.; Rigolio, R.; Romano, S.; Mitro, N.; Viviani, B.; Cavaletti, G.; Caruso, D.; Garcia-Segura, L.M.; Melcangi, R.C. Dihydrotestosterone as a Protective Agent in Chronic Experimental Autoimmune Encephalomyelitis. Neuroendocrinology 2015, 101, 296–308. [Google Scholar] [CrossRef]
- Djaldetti, R.; Melamed, E. New drugs in the future treatment of Parkinson’s disease. J. Neurol. 2002, 249 (Suppl. S2), Ii30–Ii35. [Google Scholar] [CrossRef] [PubMed]
- Schapira, A.H. Progress in neuroprotection in Parkinson’s disease. Eur. J. Neurol. 2008, 15 (Suppl. S1), 5–13. [Google Scholar] [CrossRef]
- White, C.M.; Pasupuleti, V.; Roman, Y.M.; Li, Y.; Hernandez, A.V. Oral turmeric/curcumin effects on inflammatory markers in chronic inflammatory diseases: A systematic review and meta-analysis of randomized controlled trials. Pharmacol. Res. 2019, 146, 104280. [Google Scholar] [CrossRef]
- Abrahams, S.; Haylett, W.L.; Johnson, G.; Carr, J.A.; Bardien, S. Antioxidant effects of curcumin in models of neurodegeneration, aging, oxidative and nitrosative stress: A review. Neuroscience 2019, 406, 1–21. [Google Scholar] [CrossRef]
- Baj, T.; Seth, R. Role of Curcumin in Regulation of TNF-α Mediated Brain Inflammatory Responses. Recent. Pat. Inflamm. Allergy Drug. Discov. 2018, 12, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Sian-Hülsmann, J.; Mandel, S.; Youdim, M.B.; Riederer, P. The relevance of iron in the pathogenesis of Parkinson’s disease. J. Neurochem. 2011, 118, 939–957. [Google Scholar] [CrossRef] [PubMed]
- Ward, R.J.; Dexter, D.; Florence, A.; Aouad, F.; Hider, R.; Jenner, P.; Crichton, R.R. Brain iron in the ferrocene-loaded rat: Its chelation and influence on dopamine metabolism. Biochem. Pharmacol. 1995, 49, 1821–1826. [Google Scholar] [CrossRef]
- Dexter, D.T.; Ward, R.J.; Florence, A.; Jenner, P.; Crichton, R.R. Effects of desferrithiocin and its derivatives on peripheral iron and striatal dopamine and 5-hydroxytryptamine metabolism in the ferrocene-loaded rat. Biochem. Pharmacol. 1999, 58, 151–155. [Google Scholar] [CrossRef]
- Porter, J.B. Deferoxamine pharmacokinetics. Semin. Hematol. 2001, 38, 63–68. [Google Scholar] [CrossRef]
- Hider, R.C.; Hoffbrand, A.V. The Role of Deferiprone in Iron Chelation. N. Engl. J. Med. 2018, 379, 2140–2150. [Google Scholar] [CrossRef]
- Li, J.; Zhang, W.; Mei, S.; Qiao, L.; Wang, Y.; Zhang, X.; Li, J.; Hu, Y.; Jia, X.; Zhang, Y. Prevention and Treatment of Hardware-Related Infections in Deep Brain Stimulation Surgeries: A Retrospective and Historical Controlled Study. Front. Hum. Neurosci. 2021, 15, 707816. [Google Scholar] [CrossRef] [PubMed]
- Osawa, M.; Shingu, K.; Murakawa, M.; Adachi, T.; Kurata, J.; Seo, N.; Murayama, T.; Nakao, S.; Mori, K. Effects of sevoflurane on central nervous system electrical activity in cats. Anesth. Analg. 1994, 79, 52–57. [Google Scholar] [CrossRef] [PubMed]
- Hutchison, W.D.; Lang, A.E.; Dostrovsky, J.O.; Lozano, A.M. Pallidal neuronal activity: Implications for models of dystonia. Ann. Neurol. 2003, 53, 480–488. [Google Scholar] [CrossRef]
- Holewijn, R.A.; Verbaan, D.; van den Munckhof, P.M.; Bot, M.; Geurtsen, G.J.; Dijk, J.M.; Odekerken, V.J.; Beudel, M.; de Bie, R.M.A.; Schuurman, P.R. General Anesthesia vs Local Anesthesia in Microelectrode Recording-Guided Deep-Brain Stimulation for Parkinson Disease: The GALAXY Randomized Clinical Trial. JAMA Neurol. 2021, 78, 1212–1219. [Google Scholar] [CrossRef]
- Liu, Z.; He, S.; Li, L. General Anesthesia versus Local Anesthesia for Deep Brain Stimulation in Parkinson’s Disease: A Meta-Analysis. Stereotact. Funct. Neurosurg. 2019, 97, 381–390. [Google Scholar] [CrossRef]
- Dorsey, E.R.; Sherer, T.; Okun, M.S.; Bloem, B.R. The Emerging Evidence of the Parkinson Pandemic. J. Parkinsons Dis. 2018, 8, S3–S8. [Google Scholar] [CrossRef] [PubMed]
- Habets, J.G.V.; Heijmans, M.; Kuijf, M.L.; Janssen, M.L.F.; Temel, Y.; Kubben, P.L. An update on adaptive deep brain stimulation in Parkinson’s disease. Mov. Disord. 2018, 33, 1834–1843. [Google Scholar] [CrossRef] [PubMed]
- Brozova, H.; Barnaure, I.; Ruzicka, E.; Stochl, J.; Alterman, R.; Tagliati, M. Short- and Long-Term Effects of DBS on Gait in Parkinson’s Disease. Front. Neurol. 2021, 12, 688760. [Google Scholar] [CrossRef]
- Honkanen, E.A.; Korpela, J.; Pekkonen, E.; Kaasinen, V.; Reich, M.M.; Joutsa, J. Reappearance of Symptoms after GPi-DBS Discontinuation in Cervical Dystonia. Mov. Disord. Clin. Pract. 2021, 8, 406–411. [Google Scholar] [CrossRef]
- Lewis, C.J.; Maier, F.; Horstkötter, N.; Eggers, C.; Visser-Vandewalle, V.; Moro, E.; Zurowski, M.; Kuhn, J.; Woopen, C.; Timmermann, L. The impact of subthalamic deep brain stimulation on caregivers of Parkinson’s disease patients: An exploratory study. J. Neurol. 2015, 262, 337–345. [Google Scholar] [CrossRef]
- Aldridge, D.; Theodoros, D.; Angwin, A.; Vogel, A.P. Speech outcomes in Parkinson’s disease after subthalamic nucleus deep brain stimulation: A systematic review. Parkinsonism Relat. Disord. 2016, 33, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Tripoliti, E.; Zrinzo, L.; Martinez-Torres, I.; Frost, E.; Pinto, S.; Foltynie, T.; Holl, E.; Petersen, E.; Roughton, M.; Hariz, M.I.; et al. Effects of subthalamic stimulation on speech of consecutive patients with Parkinson disease. Neurology 2011, 76, 80–86. [Google Scholar] [CrossRef]
- Okun, M.S.; Fernandez, H.H.; Wu, S.S.; Kirsch-Darrow, L.; Bowers, D.; Bova, F.; Suelter, M.; Jacobson, C.E.t.; Wang, X.; Gordon, C.W., Jr.; et al. Cognition and mood in Parkinson’s disease in subthalamic nucleus versus globus pallidus interna deep brain stimulation: The COMPARE trial. Ann. Neurol. 2009, 65, 586–595. [Google Scholar] [CrossRef]
- Fasano, A.; Romito, L.M.; Daniele, A.; Piano, C.; Zinno, M.; Bentivoglio, A.R.; Albanese, A. Motor and cognitive outcome in patients with Parkinson’s disease 8 years after subthalamic implants. Brain 2010, 133, 2664–2676. [Google Scholar] [CrossRef] [PubMed]
- Evered, L.A.; Silbert, B.S. Postoperative Cognitive Dysfunction and Noncardiac Surgery. Anesth. Analg. 2018, 127, 496–505. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Meng, H.; Wei, J.-H.; Yu, P.-Z.; Ren, J.-X.; Tang, M.-Y.; Sun, J.-Y.; Yan, X.-Y.; Su, J. Insights into Advanced Neurological Dysfunction Mechanisms Following DBS Surgery in Parkinson’s Patients: Neuroinflammation and Pyroptosis. Curr. Issues Mol. Biol. 2023, 45, 4480-4494. https://doi.org/10.3390/cimb45050284
Meng H, Wei J-H, Yu P-Z, Ren J-X, Tang M-Y, Sun J-Y, Yan X-Y, Su J. Insights into Advanced Neurological Dysfunction Mechanisms Following DBS Surgery in Parkinson’s Patients: Neuroinflammation and Pyroptosis. Current Issues in Molecular Biology. 2023; 45(5):4480-4494. https://doi.org/10.3390/cimb45050284
Chicago/Turabian StyleMeng, Hao, Jia-Hang Wei, Peng-Zheng Yu, Jia-Xin Ren, Meng-Yao Tang, Jun-Yi Sun, Xiao-Yu Yan, and Jing Su. 2023. "Insights into Advanced Neurological Dysfunction Mechanisms Following DBS Surgery in Parkinson’s Patients: Neuroinflammation and Pyroptosis" Current Issues in Molecular Biology 45, no. 5: 4480-4494. https://doi.org/10.3390/cimb45050284
APA StyleMeng, H., Wei, J.-H., Yu, P.-Z., Ren, J.-X., Tang, M.-Y., Sun, J.-Y., Yan, X.-Y., & Su, J. (2023). Insights into Advanced Neurological Dysfunction Mechanisms Following DBS Surgery in Parkinson’s Patients: Neuroinflammation and Pyroptosis. Current Issues in Molecular Biology, 45(5), 4480-4494. https://doi.org/10.3390/cimb45050284






