Study on the Status of Health Service Utilization among Caregivers of Left-Behind Children in Poor Rural Areas of Hunan Province: A Baseline Survey
Abstract
:1. Introduction
2. Methods
2.1. Sampling
- The village inclusion criteria: Villages with a minimum of 15 LBC (3–5 years old) living in poor households (per capita annual income <2300 RMB in 2013) with no kindergarten or care center for LBC.
- The village exclusion criteria: Villages receiving similar funding or benefits from other sources, such as charities or non-governmental organizations (NGOs).
- The CLBC inclusion criteria: Caregivers in poor households (per capita annual income <2300 RMB in 2013) with at least one LBC (3–5 years old).
- The CLBC exclusion criteria: Caregivers receiving benefits from a charity, NGO or other similar program.
2.2. Recruitment
2.3. Ethical Approval
2.4. Data Collection
2.5. Statistical Analysis
3. Results
3.1. General Characteristics of Study Population
3.2. Accessibility of Health Service
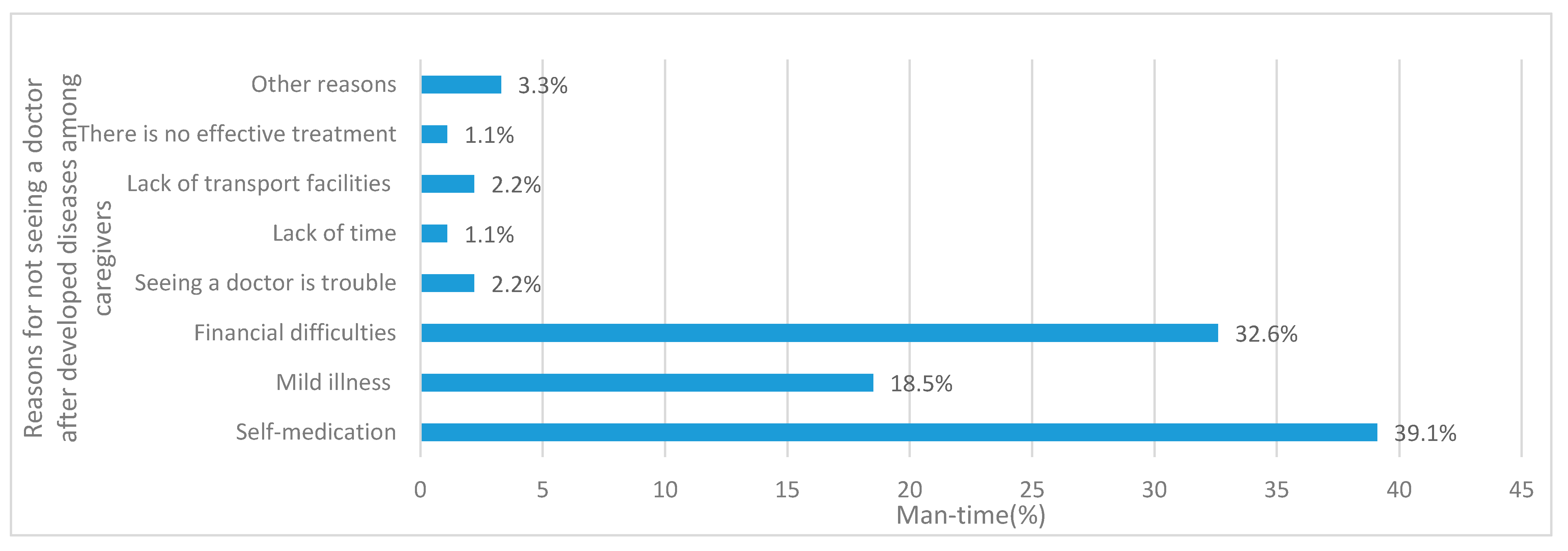
3.3. Health Service Needs
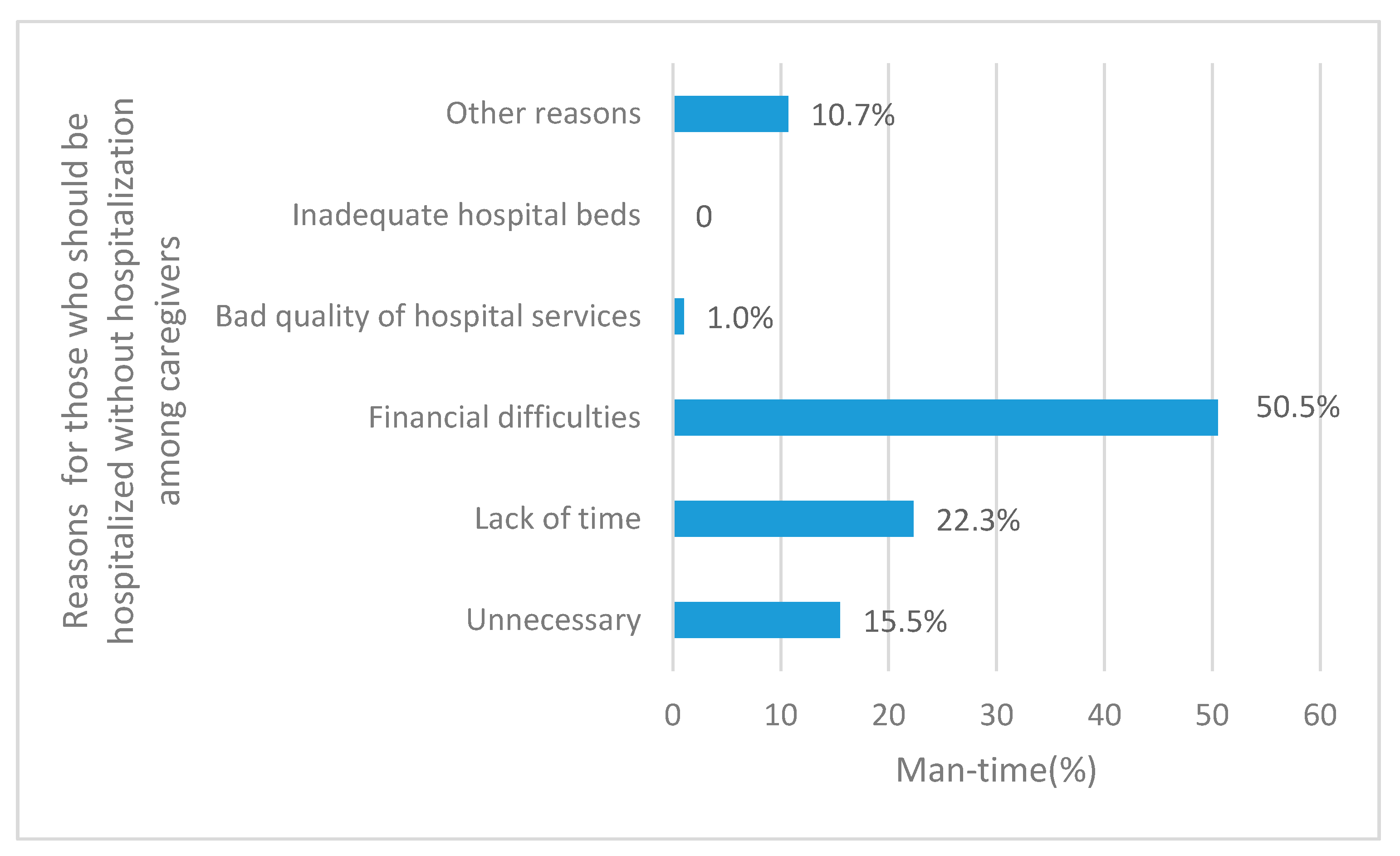
3.4. Hospitalization Rates
3.5. Participation in Basic Public Health Services among CLBCs
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| CLBC | Caregivers of left-behind children |
| LBC | Left-behind children |
| NGO | Non-governmental organizations |
| NCMS | New Cooperative Medical System |
| CCT | Conditional cash transfer |
References
- All-China Women’s Federation. Research Report on rural left-behind children and rural-urban migrant children in China. China Women’s Mov. 2013, 6, 30–34. (In Chinese) [Google Scholar]
- Niu, T.H.; Meng, Q.Y.; Wang, G.D. The study on the status of the utilization of the Health services of the Shandong province rural elders and its influencing factors. Chin. Prim. Health Care 2010, 24, 7–8. (In Chinese) [Google Scholar]
- Zhang, M.Y. The Study about Left-Behind Children Guardinas’s Social Capitals’ Influence towards Health Service Utilization in Yanbian Area; Yanbian University: Jilin, China, 2013. (In Chinese) [Google Scholar]
- Tu, D. Investigation and Analysis to the Basic Medical and Health Service Needs of the Rural Elderly with Migrant Children in Chongqing; Chongqing Medical University: Chongqing, China, 2015. (In Chinese) [Google Scholar]
- Xiao, Y.Z. Research on Life Quality and Health Service Utilization among the Elder Left-Behind Population in Henyang County of Hunan Province; Central South Univerty: Hunan, China, 2010. (In Chinese) [Google Scholar]
- Ren, H.L.; Qiao, H.; Huang, Y.X. Health service demand and utilization among women of childbearing age in rural areas of Ningxia. J. Ningxia Med. Univ. 2015, 37, 177–179. (In Chinese) [Google Scholar]
- Hu, Y.; Gong, L.; Chen, F.K. Investigation on health status and health care consciousness of rural married women of childbearing age. Maternal Child Health Care China 2013, 28, 1453–1456. (In Chinese) [Google Scholar]
- Gao, J.; Ni, Z.; Tian, H.W. Two-week Morbility Rate and Health Services Utilization of 830 Rural Women of Childbearing Age in Tongxin County. J. Ningxia Med. Univ. 2012, 34, 912–914. (In Chinese) [Google Scholar]
- Lin, Q.; Peymané, A.; Karla, H. Health allowance for improving the nutritional status and development of 3–5-year-old left-behind children in poor rural areas of China: Study protocol for a cluster randomised trial. Trials 2015, 16, 1–10. [Google Scholar]
- Luo, J.Y.; Li, M.L.; Zeng, R. Study on the willingness of care and related influencing factors among caregivers of those stranded children under 7 years in Chinese rural areas. Chin. J. Epidemiol. 2010, 31, 965–969. (In Chinese) [Google Scholar]
- Xu, L.; Meng, Q. The Fifth National Health Service Survey-Health services need, demand and utilization. Chin. J. Health Inform. Manag. 2014, 11, 193–194. (In Chinese) [Google Scholar]
- Jing, R.F. Acomparative Study of Medical Care Utilization of Peasants Participating in the New Cooperative Medical System in some Poverty Counties in Hunan; Peking Union Medical College: Beijing, China, 2014. (In Chinese) [Google Scholar]
- Guo, Y.C. Study on Health Services Utilition and Influencing Factors among Rural Elderly in Certral and West Poor Areas of China; Huazhong University of Science and Technology: Hubei, China, 2013. (In Chinese) [Google Scholar]
- Yang, S.W.; Lin, X.Y.; Wu, W.F. Investigation and analysis research of rural doctors team in Qiannan. China J. Qiannan Med. Coll. Natl. 2014, 27, 259–261. (In Chinese) [Google Scholar]
- He, H.M.; Wu, S.J.; Yao, C.Q. Investigation of farmers’ health records management and cognition. China Health Serv. Manag. 2009, 249, 187–189. (In Chinese) [Google Scholar]
- Ma, H.Q.; Chen, Z.C. Patterns of Inter-provincial Migration in China:Evidence from the Sixth Population Census. Popul. Res. 2012, 36, 87–99. (In Chinese) [Google Scholar]
- Joseph, E.S. Economics of the Public Sector, 3rd ed.; W.W. Norton & Company: New York, NY, USA, 2000; p. 25. [Google Scholar]
- Ren, G. The key of the sustainable development of the New Rural Cooperative Medical Scheme: Institutional change and demand management. China Prim. Health Care 2012, 26, 17–18. (In Chinese) [Google Scholar]
- Liu, Y.J. Enlightenment of Thailand’s “30 baht plan” on medical insurance in China. Health Econ. Res. 2011, 286, 45–47. (In Chinese) [Google Scholar]
- Tang, L.X.; Zhao, L.Y.; Li, X.Y. International experience of conditional cash transfer payment for poverty alleviation program. Guizhou Soc. Sci. 2012, 272, 87–93. (In Chinese) [Google Scholar]
- Hu, X.J.; Yu, M. Analyzing the mode of Conditional Cash Transfers for demander of health services. China Health Serv. Manag. 2014, 213, 487–489. (In Chinese) [Google Scholar]
| Fenghuang County (n = 254) | Pingjiang County (n = 264) | Total (n = 518) | |
|---|---|---|---|
| Family size | |||
| ≤3 | 2 (0.8%) | 2 (0.8%) | 4 (0.8%) |
| 4–7 | 172 (67.7%) | 190 (72.0%) | 362 (69.9%) |
| 8–11 | 73 (28.7%) | 67 (25.4%) | 140 (27.0%) |
| ≥12 | 7 (2.8%) | 5 (1.9%) | 12 (2.3%) |
| Housing type | |||
| Thatched cottage/shack | 37 (14.6%) | 4 (1.5%) | 41 (7.9%) |
| Earth wall room | 75 (29.5%) | 19 (7.2%) | 94 (18.1%) |
| Brick bungalows | 73 (28.7%) | 103 (39.0%) | 176 (34.0%) |
| Two floor cottages | 69 (27.2%) | 138 (52.3%) | 207 (40.0%) |
| Access to tap water | 104 (40.9%) | 30 (11.4%) | 134 (25.9%) |
| Age (year) | |||
| 20–39 | 47 (18.5%) | 13 (4.9%) | 60 (11.6%) |
| 40–59 | 91 (35.8%) | 152 (57.6%) | 243 (46.9%) |
| ≥60 | 116 (45.7%) | 99 (37.5%) | 215 (41.5%) |
| Gender | |||
| Male | 81 (31.9%) | 94 (35.6%) | 175 (33.8%) |
| Female | 173 (68.2%) | 170 (64.4%) | 343 (66.2%) |
| Ethnicity | |||
| Han | 65 (25.6%) | 260 (98.5%) | 325 (62.7%) |
| Miao and other minorities | 189 (74.4%) | 4 (1.5%) | 193 (37.3%) |
| Education level | |||
| No formal education | 99 (39.0%) | 56 (21.2%) | 155 (29.9%) |
| Primary school | 101 (39.7%) | 150 (56.8%) | 251 (48.4%) |
| Junior middle school | 44 (17.3%) | 48 (18.2%) | 92 (17.8%) |
| High school and others | 10 (3.9%) | 10 (3.8%) | 20 (3.9%) |
| Occupation | |||
| Farmer | 241 (94.9%) | 256 (97.0%) | 497 (95.9%) |
| Living conditions | |||
| Living with their spouses | 59 (23.2%) | 79 (29.9%) | 138 (26.6%) |
| Living with their spouses and children | 171 (67.3%) | 148 (56.1%) | 319 (61.6%) |
| Widowed and living with their children | 21 (8.3%) | 27 (10.2%) | 48 (9.3%) |
| Widowed and living alone | 3 (1.2%) | 10 (3.8%) | 13 (2.5%) |
| Annual per capita income Quartile (RMB) | |||
| <¥695 (Bottom) | 84 (33.1%) | 45 (17.0%) | 129 (24.9%) |
| ¥695–1512 (3rd ) | 63 (24.8%) | 67 (25.4%) | 130 (25.1%) |
| ¥1513–2561 (2nd) | 56 (22.0%) | 74 (28.0%) | 130 (25.1%) |
| ≥¥2562 (Top) | 51 (20.1%) | 78 (29.5%) | 129 (24.9%) |
| Relation to LBC * | |||
| Father or Mother | 53 (20.9%) | 23 (8.7%) | 76 (14.7%) |
| Grandparents | 200 (78.7%) | 230 (87.1%) | 430 (83.0%) |
| Others | 1 (0.4%) | 11 (4.2%) | 12 (2.3%) |
| Bedridden patient at home | |||
| None | 215 (84.6%) | 206 (78.0%) | 421 (81.3%) |
| One | 36 (14.2%) | 50 (18.9%) | 86 (16.6%) |
| Two and more | 3 (1.2%) | 8 (3.0%) | 11 (2.1%) |
| Number of 3–5 years old LBC | |||
| 1 | 193 (76.0%) | 208 (78.8%) | 401 (77.4%) |
| 2–3 | 55 (21.7%) | 53 (20.1%) | 108 (20.8%) |
| More than 3 | 3 (1.2%) | 2 (0.8%) | 5 (1.0%) |
| Number of participants who had missing data | 3 (1.2%) | 1 0.4%) | 4 (0.8%) |
| Number of LBC | |||
| 1 | 79 (31.1%) | 83 (31.4%) | 162 (31.3%) |
| 2–3 | 139 (54.7%) | 160 (60.6%) | 299 (57.7%) |
| More than 3 | 32 (12.6%) | 19 (7.2%) | 51 (9.8%) |
| Number of participants who had missing data | 4 (1.6%) | 2 (0.8%) | 6 (1.2%) |
| Enrolled in the NCMS ** | 242 (95.3%) | 257 (97.3%) | 499 (96.3%) |
| Fenghuang County (n = 81) | Pingjiang County (n = 106) | Total (n = 187) | p | |
|---|---|---|---|---|
| Two-week prevalence | 81 (31.9%) | 106 (40.2%) | 187 (36.1%) | 0.055 |
| Two-week clinic visiting | 44 (54.3%) | 65 (61.3%) | 109 (58.3%) | 0.371 |
| Presenting symptoms(man-time) | 0.877 | |||
| Fever/Headache/Cough | 36 (39.6%) | 48 (37.2%) | 84 (38.2%) | |
| Abdominal pain/ Diarrhea | 3 (3.3%) | 7 (5.4%) | 10 (4.5%) | |
| Chest pain/Flustered/Palpitations | 8 (8.8%) | 14 (10.9%) | 22 (10.0%) | |
| Trauma | 1 (1.1%) | 3 (2.3%) | 4 (1.8%) | |
| Others | 43 (47.3%) | 57 (44.2%) | 100 (45.5%) | |
| Types of symptoms | 0.597 | |||
| One | 64 (79.0%) | 78 (73.6%) | 142 (75.9%) | |
| Two | 14 (17.3%) | 20 (18.9%) | 34 (18.2%) | |
| Three or more | 2 (2.5%) | 7 (6.6%) | 9 (4.8%) | |
| Number of participants who had missing data | 1 (1.2%) | 1 (0.9%) | 2 (1.1%) | |
| Is the activity affected? | 0.556 | |||
| No | 48 (59.3%) | 55 (51.9%) | 103 (55.1%) | |
| Partly restricted | 30 (37.0%) | 47 (44.3%) | 77 (41.2%) | |
| Needed to be on bed rest | 3 (3.7%) | 4 (3.8%) | 7 (3.7%) |
| Fenghuang County (n = 44) | Pingjiang County (n = 65) | Total (n = 109) | p | |
|---|---|---|---|---|
| Village clinics | 21 (47.7%) | 31 (47.7%) | 52 (47.7%) | 0.881 |
| Township hospitals | 14 (31.8%) | 17 (26.2%) | 31 (28.4%) | |
| County hospitals | 6 (13.6%) | 11 (16.9%) | 17 (15.6%) | |
| City hospitals and above | 3 (6.8%) | 6 (9.2%) | 9 (8.3%) |
| Fenghuang County (n = 254) | Pingjiang County (n = 264) | Total (n = 518) | p | |
|---|---|---|---|---|
| Hospitalized times in 2014 | 0.035 | |||
| None | 209 (82.3%) | 192 (72.7%) | 401 (77.4%) | |
| One or two times | 40 (15.7%) | 64 (24.2%) | 104 (20.1%) | |
| Three times or more | 5 (2.0%) | 8 (3.0%) | 13 (2.5%) | |
| Total hospital stays in 2014 | 0.940 | |||
| Less than or equal to five days | 9 (20.0%) | 16 (22.2%) | 25 (21.4%) | |
| Between six and ten days | 19 (42.2%) | 28 (38.9%) | 47 (40.2%) | |
| More than ten days | 17 (37.8%) | 28 (38.9%) | 45 (38.5%) | |
| Number of participants who were recommended for hospitalization by a doctor | 76 (29.9%) | 124 (47.0%) | 200 (38.6%) | <0.001 |
| Non-hospitalization for those who needed | 31 (40.8%) | 52 (41.9%) | 83 (41.5%) | 0.87 |
| Fenghuang County (n = 254) | Pingjiang County (n = 264) | Total (n = 518) | p | |
|---|---|---|---|---|
| Have established health records in town hospital | ||||
| Yes | 83 (32.7%) | 99 (37.5%) | 182 (35.1%) | 0.428 |
| No | 101 (39.7%) | 103 (39.0%) | 204 (39.4%) | |
| Unclear | 70 (27.6%) | 62 (23.5%) | 132 (25.5%) | |
| Received free health examination in local health institutions in 2014 | ||||
| Yes | 129 (50.8%) | 133 (50.4%) | 262 (50.6%) | 0.793 |
| No/Forgot | 125 (49.2%) | 131 (49.6%) | 256 (49.4%) | |
| Received health education organized by local health institutions in 2014 | ||||
| None | 229 (90.1%) | 192 (72.7%) | 421 (81.3%) | <0.001 |
| One or two times | 18 (7.1%) | 56 (21.2%) | 74 (14.3%) | |
| Three times or more | 7 (2.8%) | 16 (6.1%) | 23 (4.4%) | |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ji, M.; Zhang, Y.; Zou, J.; Yuan, T.; Tang, A.; Deng, J.; Yang, L.; Li, M.; Chen, J.; Qin, H.; et al. Study on the Status of Health Service Utilization among Caregivers of Left-Behind Children in Poor Rural Areas of Hunan Province: A Baseline Survey. Int. J. Environ. Res. Public Health 2017, 14, 910. https://doi.org/10.3390/ijerph14080910
Ji M, Zhang Y, Zou J, Yuan T, Tang A, Deng J, Yang L, Li M, Chen J, Qin H, et al. Study on the Status of Health Service Utilization among Caregivers of Left-Behind Children in Poor Rural Areas of Hunan Province: A Baseline Survey. International Journal of Environmental Research and Public Health. 2017; 14(8):910. https://doi.org/10.3390/ijerph14080910
Chicago/Turabian StyleJi, Meimei, Yefu Zhang, Jiaojiao Zou, Tong Yuan, Amber Tang, Jing Deng, Lina Yang, Mingzhi Li, Jihua Chen, Hong Qin, and et al. 2017. "Study on the Status of Health Service Utilization among Caregivers of Left-Behind Children in Poor Rural Areas of Hunan Province: A Baseline Survey" International Journal of Environmental Research and Public Health 14, no. 8: 910. https://doi.org/10.3390/ijerph14080910
APA StyleJi, M., Zhang, Y., Zou, J., Yuan, T., Tang, A., Deng, J., Yang, L., Li, M., Chen, J., Qin, H., & Lin, Q. (2017). Study on the Status of Health Service Utilization among Caregivers of Left-Behind Children in Poor Rural Areas of Hunan Province: A Baseline Survey. International Journal of Environmental Research and Public Health, 14(8), 910. https://doi.org/10.3390/ijerph14080910






