The Zika Virus Epidemic in Brazil: From Discovery to Future Implications
Abstract
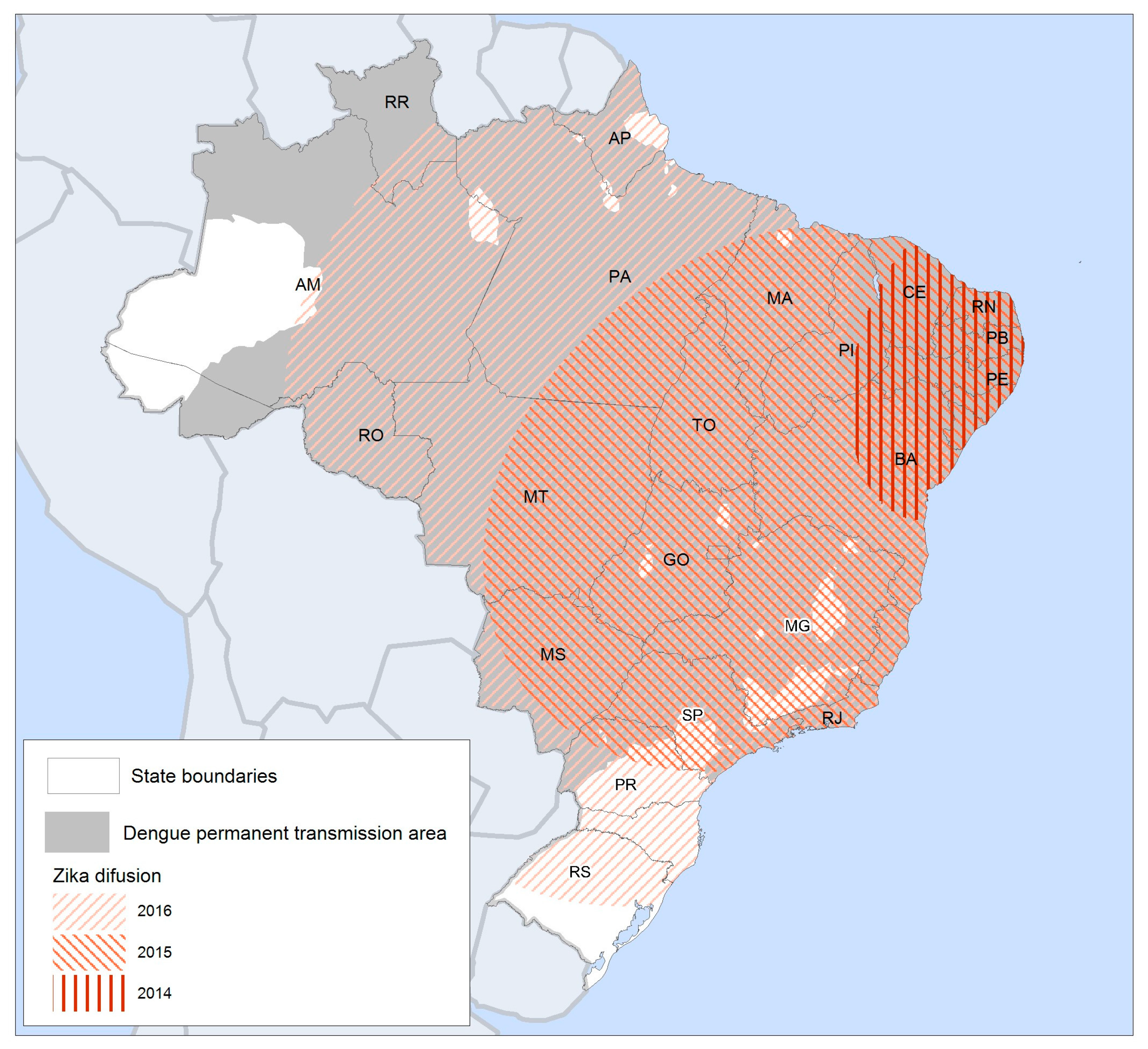
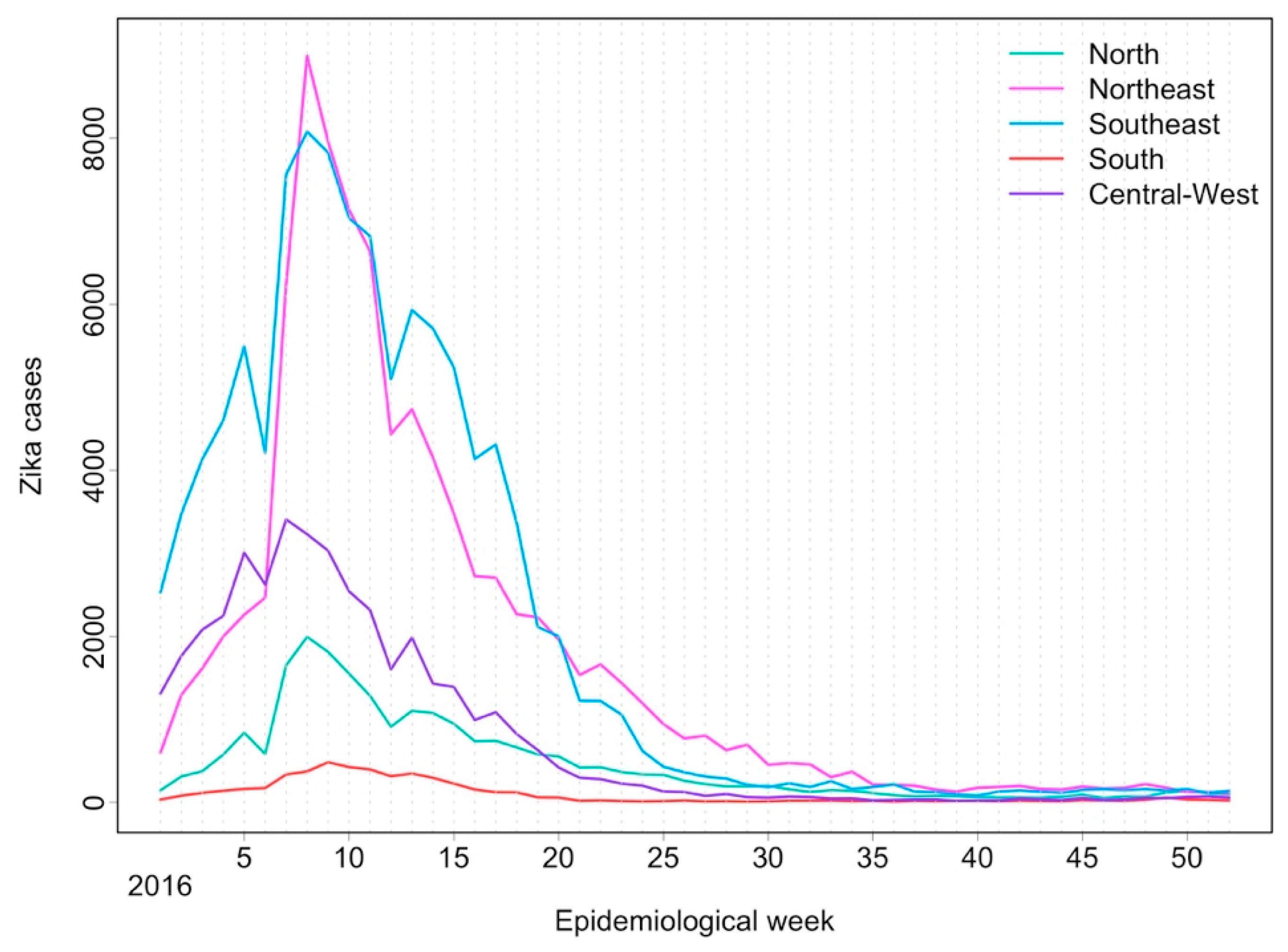
:1. Zika Virus Emergence and Spread in Brazil
2. A Public Health Emergency
2.1. Building the Evidence
2.2. Epidemiological Surveillance and Health Information Systems
3. ZIKV Transmission
3.1. Vector-Borne Transmission
3.2. Non-Vector-Borne Transmission
4. Clinical Manifestations of ZIKV
5. Control and Prevention Strategies
5.1. Vector Control
5.2. Mathematical Modelling to Guide Interventions
5.3. Birth Control
6. Social and Economic Impact
7. Knowledge Gaps
8. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Weaver, S.C.; Costa, F.; Garcia-Blanco, M.A.; Ko, A.I.; Ribeiro, G.S.; Saade, G.; Shi, P.-Y.; Vasilakis, N. Zika virus: History, emergence, biology, and prospects for control. Antivir. Res. 2016, 130, 69–80. [Google Scholar] [CrossRef] [PubMed]
- Paixão, E.S.; Barreto, F.; da Glória Teixeira, M.; da Conceição, N.; Costa, M.; Rodrigues, L.C. History, epidemiology, and clinical manifestations of Zika: A systematic review. Am. J. Public Health 2016, 106, 606–612. [Google Scholar] [CrossRef] [PubMed]
- Kindhauser, M.K.; Allen, T.; Frank, V.; Santhana, R.S.; Dye, C. Zika: The origin and spread of a mosquito-borne virus. Bull. World Health Organ. 2016, 94, 675C–686C. [Google Scholar] [CrossRef] [PubMed]
- Faria, N.R.; Azevedo, R.D.S.D.S.; Kraemer, M.U.G.; Souza, R.; Cunha, M.S.; Hill, S.C.; Thézé, J.; Bonsall, M.B.; Bowden, T.A.; Rissanen, I.; et al. Zika virus in the Americas: Early epidemiological and genetic findings. Science 2016, 352, 345–349. [Google Scholar] [CrossRef] [PubMed]
- Zanluca, C.; de Melo, V.C.A.; Mosimann, A.L.P.; dos Santos, G.I.V.; dos Santos, C.N.D.; Luz, K. First report of autochthonous transmission of Zika virus in Brazil. Mem. Inst. Oswaldo Cruz 2015, 110, 569–572. [Google Scholar] [CrossRef] [PubMed]
- Campos, G.S.; Bandeira, A.C.; Sardi, S.I. Zika virus outbreak, Bahia, Brazil. Emerg. Infect. Dis. 2015, 21, 1885–1886. [Google Scholar] [CrossRef] [PubMed]
- Ministério da Saúde. Dengue, Chikungunya e Zika. Available online: http://combateaedes.saude.gov.br/en/epidemiological-situation (accessed on 19 November 2017).
- Barcellos, C.; Lowe, R. Expansion of the dengue transmission area in Brazil: The role of climate and cities. Trop. Med. Int. Health 2014, 19, 159–168. [Google Scholar] [CrossRef] [PubMed]
- De Castro Catão, R.; Guimarães, R.B. Mapeamento da reemergência do dengue no Brasil–1981/82-2008. Hygeia 2011, 7, 173–185. [Google Scholar]
- Netto, E.M.; Moreira-Soto, A.; Pedroso, C.; Höser, C.; Funk, S.; Kucharski, A.J.; Rockstroh, A.; Kümmerer, B.M.; Sampaio, G.S.; Luz, E.; et al. High Zika virus seroprevalence in Salvador, Northeastern Brazil limits the potential for further outbreaks. MBio 2017, 8, e01390-17. [Google Scholar] [CrossRef] [PubMed]
- Secretaria de Vigilância em Saúde. Ministério da Saúde Monitoramento dos casos de dengue, febre de chikungunya e febre pelo vírus Zika até a semana epidemiológica 25, 2017. Bol. Epidemiol. 2017, 48, 1–10. [Google Scholar]
- Ferguson, N.M.; Cucunubá, Z.M.; Dorigatti, I.; Nedjati-Gilani, G.L.; Donnelly, C.A.; Basáñez, M.-G.; Nouvellet, P.; Lessler, J. Countering the Zika epidemic in Latin America. Science 2016, 353, 353–354. [Google Scholar] [CrossRef] [PubMed]
- Aliota, M.T.; Bassit, L.; Bradrick, S.S.; Cox, B.; Garcia-Blanco, M.A.; Gavegnano, C.; Friedrich, T.C.; Golos, T.G.; Griffin, D.E.; Haddow, A.D.; et al. Zika in the Americas, year 2: What have we learned? What gaps remain? A report from the Global Virus Network. Antivir. Res. 2017, 144, 223–246. [Google Scholar] [CrossRef] [PubMed]
- Teixeira, M.G.; Maria da Conceição, N.C.; de Oliveira, W.K.; Nunes, M.L.; Rodrigues, L.C. The epidemic of Zika virus–related microcephaly in Brazil: Detection, control, etiology, and future scenarios. Am. J. Public Health 2016, 106, 601–605. [Google Scholar] [CrossRef] [PubMed]
- Secretaria de Vigilância em Saúde. Ministério da Saúde Situação epidemiológica de ocorrência de microcefalias no Brasil, 2015. Bol. Epidemiol. 2015, 46, 1–3. [Google Scholar]
- WHO. WHO Director-General Summarizes the Outcome of the Emergency Committee Regarding Clusters of Microcephaly and Guillain-Barré Syndrome. Available online: http://www.who.int/mediacentre/news/statements/2016/emergency-committee-zika-microcephaly/en/ (accessed on 4 March 2016).
- Mallet, H.-P.; Vial, A.-L.; Musso, D. Bilan de l’epidemie a virus Zika en Polynesie Francaise, 2013–2014. BISES Bull. Inf. Sanit. Epidemiol. Stat. 2015, 13, 1–5. [Google Scholar]
- Ministério da Saúde. Secretaria de Vigilância em Saúde—Ministério da Saúde monitoramento dos casos de dengue, febre de chikungunya e febre pelo vírus Zika até a semana epidemiológica 52, 2016. Bol. Epidemiol. 2017, 48, 1–11. [Google Scholar]
- Ministério da Saúde. Secretaria de Vigilância em Saúde. Protocolo de Vigilância e Resposta à Ocorrência de Microcefalia Relacionada à Infecção pelo Vírus Zika; Ministério da Saúde: Brasília, Brazil, 2015.
- Victora, C.G.; Schuler-Faccini, L.; Matijasevich, A.; Ribeiro, E.; Pessoa, A.; Barros, F.C. Microcephaly in Brazil: How to interpret reported numbers? Lancet 2016, 387, 621–624. [Google Scholar] [CrossRef]
- De Souza, W.V.; de Araújo, T.V.B.; de Albuquerque, M.F.P.M.; Braga, M.C.; de Ximenes, R.A.A.; de Miranda-Filho, D.B.; Bezerra, L.C.A.; Dimech, G.S.; de Carvalho, P.I.; de Assunção, R.S.; et al. Microcephaly in Pernambuco State, Brazil: Epidemiological characteristics and evaluation of the diagnostic accuracy of cutoff points for reporting suspected cases. Cad. Saúde Pública 2016, 32. [Google Scholar] [CrossRef]
- World Health Organization. Pyriproxyfen in Drinking-Water: Background Document for Development of WHO Guidelines for Drinking-Water Quality; WHO: Geneva, Switzerland, 2004. [Google Scholar]
- Lopez-Camelo, J.S.; Orioli, I.M.; Castilla, E. ECLAMC Final Document; ECLAMC: Buenos Aires, Argentina, 2015. [Google Scholar]
- Diniz, D. Zika virus and women. Cad. Saúde Pública 2016, 32. [Google Scholar] [CrossRef]
- RESP—Registro de Eventos em Saúde Pública. Available online: http://www.resp.saude.gov.br/microcefalia#/painel (accessed on 15 August 2017).
- Ministério da Saúde. Brasil Protocolo de Vigilancia e Resposta à Ocorrência de Microcefalia e/ou Alterações do Sistema Nervoso Central; Ministério da Saúde: Brasília, Brazil, 2016.
- PAHO/WHO. Zika—Epidemiological Report. Brazil. Available online: http://www.paho.org/hq/index.php?option=com_docman&task=doc_view&gid=35221&&Itemid=270&lang=en (accessed on 19 November 2017).
- Secretaria de Vigilância em Saúde. Ministério da Saúde Zika vírus: Perfil epidemiológico em mulheres. Bol. Epidemiol. 2016, 47, 1–7. [Google Scholar]
- Barcellos, C.; Xavier, D.R.; Pavão, A.L.; Boccolini, C.S.; Pina, M.F.; Pedroso, M.; Romero, D.; Romão, A.R. Increased hospitalizations for neuropathies as indicators of Zika virus infection, according to Health Information System Data, Brazil. Emerg. Infect. Dis. 2016, 22, 1894. [Google Scholar] [CrossRef] [PubMed]
- De Oliveira, W.K.; de França, G.V.A.; Carmo, E.H.; Duncan, B.B.; de Souza Kuchenbecker, R.; Schmidt, M.I. Infection-related microcephaly after the 2015 and 2016 Zika virus outbreaks in Brazil: A surveillance-based analysis. Lancet 2017, 390, 861–870. [Google Scholar] [CrossRef]
- Coeli, C.M. We must pay more attention to record linkage quality. Cad. Saúde Pública 2015, 31, 1349–1350. [Google Scholar] [CrossRef] [PubMed]
- King, D.A.; Peckham, C.; Waage, J.K.; Brownlie, J.; Woolhouse, M.E.J. Infectious diseases: Preparing for the future. Science 2006, 313, 1392–1393. [Google Scholar] [CrossRef] [PubMed]
- Mirza, N.; Reynolds, T.; Coletta, M.; Suda, K.; Soyiri, I.; Markle, A.; Leopold, H.; Lenert, L.; Samoff, E.; Siniscalchi, A.; et al. Steps to a sustainable public health surveillance enterprise: A commentary from the International Society for Disease Surveillance. Online J. Public Health Inform. 2013, 5, 210. [Google Scholar] [CrossRef] [PubMed]
- Grard, G.; Caron, M.; Mombo, I.M.; Nkoghe, D.; Ondo, S.M.; Jiolle, D.; Fontenille, D.; Paupy, C.; Leroy, E.M. Zika virus in Gabon (Central Africa)—2007: A new threat from Aedes albopictus? PLoS Negl. Trop. Dis. 2014, 8, e2681. [Google Scholar] [CrossRef] [PubMed]
- Chouin-Carneiro, T.; Vega-Rua, A.; Vazeille, M.; Yebakima, A.; Girod, R.; Goindin, D.; Dupont-Rouzeyrol, M.; Lourenço-de-Oliveira, R.; Failloux, A.-B. Differential susceptibilities of Aedes aegypti and Aedes albopictus from the Americas to Zika virus. PLoS Negl. Trop. Dis. 2016, 10, e0004543. [Google Scholar] [CrossRef] [PubMed]
- Smartt, C.T.; Stenn, T.M.; Chen, T.-Y.; Teixeira, M.G.; Queiroz, E.P.; Souza Dos Santos, L.; Queiroz, G.A.; Ribeiro Souza, K.; Kalabric Silva, L.; Shin, D.; et al. Evidence of Zika virus RNA fragments in Aedes albopictus (Diptera: Culicidae) field-collected eggs from Camaçari, Bahia, Brazil. J. Med. Entomol. 2017. [Google Scholar] [CrossRef] [PubMed]
- Braks, M.A.; Honório, N.A.; Lourenço-De-Oliveira, R.; Juliano, S.A.; Lounibos, L.P. Convergent habitat segregation of Aedes aegypti and Aedes albopictus (Diptera: Culicidae) in southeastern Brazil and Florida. J. Med. Entomol. 2003, 40, 785–794. [Google Scholar] [CrossRef] [PubMed]
- Honório, N.A.; Codeço, C.T.; Alves, F.C.; Magalhães, M.A.F.M.; Lourenço-De-Oliveira, R. Temporal distribution of Aedes aegypti in different districts of Rio de Janeiro, Brazil, measured by two types of traps. J. Med. Entomol. 2009, 46, 1001–1014. [Google Scholar] [CrossRef] [PubMed]
- Lounibos, L.P. Invasions by insect vectors of human disease. Annu. Rev. Entomol. 2002, 47, 233–266. [Google Scholar] [CrossRef] [PubMed]
- Lounibos, L.P.; Kramer, L.D. Invasiveness of Aedes aegypti and Aedes albopictus and vectorial capacity for chikungunya virus. J. Infect. Dis. 2016, 214, S453–S458. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, A.; Dash, P.K.; Singh, A.K.; Sharma, S.; Gopalan, N.; Rao, P.V.L.; Parida, M.M.; Reiter, P. Evidence of experimental vertical transmission of emerging novel ECSA genotype of chikungunya virus in Aedes aegypti. PLoS Negl. Trop. Dis. 2014, 8, e2990. [Google Scholar] [CrossRef] [PubMed]
- De Lima-Camara, T.N.; Honório, N.A.; Lourenço-de-Oliveira, R. Freqüência e distribuição espacial de Aedes aegypti e Aedes albopictus (Diptera, Culicidae) no Rio de Janeiro, Brasil Frequency and spatial distribution of Aedes aegypti and Aedes albopictus (Diptera, Culicidae). Cad. Saúde Pública 2006, 22, 2079–2084. [Google Scholar] [CrossRef] [PubMed]
- Kraemer, M.U.; Sinka, M.E.; Duda, K.A.; Mylne, A.Q.; Shearer, F.M.; Barker, C.M.; Moore, C.G.; Carvalho, R.G.; Coelho, G.E.; Van Bortel, W.; et al. The global distribution of the arbovirus vectors Aedes aegypti and Ae. albopictus. Elife 2015, 4, e08347. [Google Scholar] [CrossRef] [PubMed]
- Ferreira-de-Brito, A.; Ribeiro, I.P.; de Miranda, R.M.; Fernandes, R.S.; Campos, S.S.; da Silva, K.A.B.; de Castro, M.G.; Bonaldo, M.C.; Brasil, P.; Lourenço-de-Oliveira, R. First detection of natural infection of Aedes aegypti with Zika virus in Brazil and throughout South America. Mem. Inst. Oswaldo Cruz 2016, 111, 655–658. [Google Scholar] [CrossRef] [PubMed]
- Guerbois, M.; Fernandez-Salas, I.; Azar, S.R.; Danis-Lozano, R.; Alpuche-Aranda, C.M.; Leal, G.; Garcia-Malo, I.R.; Diaz-Gonzalez, E.E.; Casas-Martinez, M.; Rossi, S.L.; et al. Outbreak of Zika virus infection, Chiapas State, Mexico, 2015, and first confirmed transmission by Aedes aegypti mosquitoes in the Americas. J. Infect. Dis. 2016, 214, 1349–1356. [Google Scholar] [CrossRef] [PubMed]
- Ayllón, T.; de Campos, R.M.; Brasil, P.; Morone, F.C.; Câmara, D.C.P.; Meira, G.L.S.; Tannich, E.; Yamamoto, K.A.; Carvalho, M.S.; Pedro, R.S.; et al. Early evidence for Zika virus circulation among Aedes aegypti mosquitoes, Rio de Janeiro, Brazil. Emerg. Infect. Dis. 2017, 23, 1411–1412. [Google Scholar] [CrossRef] [PubMed]
- Thangamani, S.; Huang, J.; Hart, C.E.; Guzman, H.; Tesh, R.B. Vertical transmission of Zika virus in Aedes aegypti mosquitoes. Am. J. Trop. Med. Hyg. 2016, 95, 1169–1173. [Google Scholar] [CrossRef] [PubMed]
- Campos, S.S.; Fernandes, R.S.; dos Santos, A.A.C.; de Miranda, R.M.; Telleria, E.L.; Ferreira-de-Brito, A.; de Castro, M.G.; Failloux, A.-B.; Bonaldo, M.C.; Lourenço-de-Oliveira, R. Zika virus can be venereally transmitted between Aedes aegypti mosquitoes. Parasit. Vectors 2017, 10, 605. [Google Scholar] [CrossRef] [PubMed]
- Pereira-Silva, J.W.; do Nascimento, V.A.; Belchior, H.C.M.; Almeida, J.F.; Pessoa, F.A.C.; Naveca, F.G.; Ríos-Velásquez, C.M. First evidence of Zika virus venereal transmission in Aedes aegypti mosquitoes. Mem. Inst. Oswaldo Cruz 2018, 113, 56–61. [Google Scholar] [CrossRef] [PubMed]
- Göertz, G.P.; Vogels, C.B.; Geertsema, C.; Koenraadt, C.J.; Pijlman, G.P. Mosquito co-infection with Zika and chikungunya virus allows simultaneous transmission without affecting vector competence of Aedes aegypti. PLoS Negl. Trop. Dis. 2017, 11, e0005654. [Google Scholar] [CrossRef] [PubMed]
- Vazeille, M.; Mousson, L.; Martin, E.; Failloux, A.-B. Orally co-Infected Aedes albopictus from La Reunion Island, Indian Ocean, can deliver both dengue and chikungunya infectious viral particles in their saliva. PLoS Negl. Trop. Dis. 2010, 4, e706. [Google Scholar] [CrossRef] [PubMed]
- Muturi, E.J.; Bara, J. Sindbis virus interferes with dengue 4 virus replication and its potential transmission by Aedes albopictus. Parasit. Vectors 2015, 8, 65. [Google Scholar] [CrossRef] [PubMed]
- Nuckols, J.; Huang, Y.-J.; Higgs, S.; Miller, A.; Pyles, R.; Spratt, H.M.; Horne, K.; Vanlandingham, D. Evaluation of simultaneous transmission of chikungunya virus and dengue virus type 2 in infected Aedes aegypti and Aedes albopictus (Diptera: Culicidae). J. Med. Entomol. 2015, 52, 447–451. [Google Scholar] [CrossRef] [PubMed]
- Di Luca, M.; Severini, F.; Toma, L.; Boccolini, D.; Romi, R.; Remoli, M.E.; Sabbatucci, M.; Rizzo, C.; Venturi, G.; Rezza, G.; et al. Experimental studies of susceptibility of Italian Aedes albopictus to Zika virus. Eurosurveillance 2016, 21. [Google Scholar] [CrossRef] [PubMed]
- Costa-da-Silva, A.L.; Ioshino, R.S.; de Araújo, H.R.C.; Kojin, B.B.; de Andrade Zanotto, P.M.; Oliveira, D.B.L.; Melo, S.R.; Durigon, E.L.; Capurro, M.L. Laboratory strains of Aedes aegypti are competent to brazilian Zika virus. PLoS ONE 2017, 12, e0171951. [Google Scholar]
- Guedes, D.R.; Paiva, M.H.; Donato, M.M.; Barbosa, P.P.; Krokovsky, L.; dos Rocha, S.W.S.; Saraiva, K.L.; Crespo, M.M.; Rezende, T.M.; Wallau, G.L.; et al. Zika virus replication in the mosquito Culex quinquefasciatus in Brazil. Emerg. Microbes Infect. 2017, 6, e69. [Google Scholar] [CrossRef] [PubMed]
- Guo, X.; Li, C.; Deng, Y.; Xing, D.; Liu, Q.; Wu, Q.; Sun, A.; Dong, Y.; Cao, W.; Qin, C.; et al. Culex pipiens quinquefasciatus: A potential vector to transmit Zika virus. Emerg. Microbes Infect. 2016, 5, e102. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, R.S.; Campos, S.S.; Ferreira-de-Brito, A.; De Miranda, R.M.; da Silva, K.A.B.; De Castro, M.G.; Raphael, L.M.; Brasil, P.; Failloux, A.-B.; Bonaldo, M.C.; et al. Culex quinquefasciatus from Rio de Janeiro is not competent to transmit the local Zika virus. PLoS Negl. Trop. Dis. 2016, 10, e0004993. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.-J.S.; Ayers, V.B.; Lyons, A.C.; Unlu, I.; Alto, B.W.; Cohnstaedt, L.W.; Higgs, S.; Vanlandingham, D.L. Culex species mosquitoes and Zika virus. Vector-Borne Zoonotic Dis. 2016, 16, 673–676. [Google Scholar] [CrossRef] [PubMed]
- Amraoui, F.; Atyame-Nten, C.; Vega-Rúa, A.; Lourenço-De-Oliveira, R.; Vazeille, M.; Failloux, A.B. Culex mosquitoes are experimentally unable to transmit Zika virus. Eurosurveillance 2016, 21. [Google Scholar] [CrossRef] [PubMed]
- Hall-Mendelin, S.; Pyke, A.T.; Moore, P.R.; Mackay, I.M.; McMahon, J.L.; Ritchie, S.A.; Taylor, C.T.; Moore, F.A.; van den Hurk, A.F. Assessment of local mosquito species incriminates Aedes aegypti as the potential vector of Zika virus in Australia. PLoS Negl. Trop. Dis. 2016, 10, e0004959. [Google Scholar] [CrossRef] [PubMed]
- Roundy, C.M.; Azar, S.R.; Brault, A.C.; Ebel, G.D.; Failloux, A.-B.; Fernandez-Salas, I.; Kitron, U.; Kramer, L.D.; Lourenço-de-Oliveira, R.; Osorio, J.E.; et al. Lack of evidence for Zika virus transmission by Culex mosquitoes. Emerg. Microbes Infect. 2017, 6, e90. [Google Scholar] [CrossRef] [PubMed]
- Ayres, C.; Guedes, D.; Paiva, M.; Donato, M.; Barbosa, P.; Krokovsky, L.; Rocha, S.; Saraiva, K.; Crespo, M.; Rezende, T.; et al. Response to: ‘Lack of evidence for Zika virus transmission by Culex mosquitoes’. Emerg. Microbes Infect. 2017, 6, e91. [Google Scholar] [CrossRef] [PubMed]
- Diallo, D.; Sall, A.A.; Diagne, C.T.; Faye, O.; Faye, O.; Ba, Y.; Hanley, K.A.; Buenemann, M.; Weaver, S.C.; Diallo, M. Zika virus emergence in mosquitoes in southeastern Senegal, 2011. PLoS ONE 2014, 9, e109442. [Google Scholar] [CrossRef] [PubMed]
- Althouse, B.M.; Vasilakis, N.; Sall, A.A.; Diallo, M.; Weaver, S.C.; Hanley, K.A. Potential for Zika virus to establish a sylvatic transmission cycle in the Americas. PLoS Negl. Trop. Dis. 2016, 10, e0005055. [Google Scholar] [CrossRef] [PubMed]
- Cornet, M.; Robin, Y.; Chateau, R.; Hème, G.; Adam, C.; Valade, M.; Le Gonidec, G.; Jan, C.; Renaudet, J.; Dieng, P.L.; et al. Isolements d’arbovirus au Sénégal oriental apartir de moustiques (1972–1977) et notes sur l’épidémiologie des virus transmis par les Aedes, en particulier du virus amaril. Ent. Méd. Parasitol. ORSTOM 1979, 17, 149–163. [Google Scholar]
- Favoretto, S.; Araujo, D.; Oliveira, D.; Duarte, N.; Mesquita, F.; Zanotto, P.; Durigon, E. First detection of Zika virus in neotropical primates in Brazil: A possible new reservoir. bioRxiv 2016. [Google Scholar] [CrossRef]
- Vorou, R. Zika virus, vectors, reservoirs, amplifying hosts, and their potential to spread worldwide: What we know and what we should investigate urgently. Int. J. Infect. Dis. 2016, 48, 85–90. [Google Scholar] [CrossRef] [PubMed]
- Musso, D.; Cao-Lormeau, V.M.; Gubler, D.J. Zika virus: Following the path of dengue and chikungunya? Lancet 2015, 386, 243–244. [Google Scholar] [CrossRef]
- Murray, K.O.; Gorchakov, R.; Carlson, A.R.; Berry, R.; Lai, L.; Natrajan, M.; Garcia, M.N.; Correa, A.; Patel, S.M.; Aagaard, K.; et al. Prolonged detection of Zika virus in vaginal secretions and whole blood. Emerg. Infect. Dis. 2017, 23, 99. [Google Scholar] [CrossRef] [PubMed]
- Baud, D.; Gubler, D.J.; Schaub, B.; Lanteri, M.C.; Musso, D. An update on Zika virus infection. Lancet 2017. [Google Scholar] [CrossRef]
- Paz-Bailey, G.; Rosenberg, E.S.; Doyle, K.; Munoz-Jordan, J.; Santiago, G.A.; Klein, L.; Perez-Padilla, J.; Medina, F.A.; Waterman, S.H.; Gubern, C.G.; et al. Persistence of Zika virus in body fluids—Preliminary report. N. Engl. J. Med. 2017. [Google Scholar] [CrossRef] [PubMed]
- Cavalcanti, M.G.; Cabral-Castro, M.J.; Gonçalves, J.L.; Santana, L.S.; Pimenta, E.S.; Peralta, J.M. Zika virus shedding in human milk during lactation: An unlikely source of infection? Int. J. Infect. Dis. 2017, 57, 70–72. [Google Scholar] [CrossRef] [PubMed]
- Sotelo, J.R.; Sotelo, A.B.; Sotelo, F.J.; Doi, A.M.; Pinho, J.R.; de Cassia Oliveira, R.; Bezerra, A.M.; Deutsch, A.D.; Villas-Boas, L.S.; Felix, A.C.; et al. Persistence of Zika virus in breast milk after infection in late stage of pregnancy. Emerg. Infect. Dis. 2017, 23, 854. [Google Scholar] [CrossRef] [PubMed]
- Karwowski, M.P.; Nelson, J.M.; Staples, J.E.; Fischer, M.; Fleming-Dutra, K.E.; Villanueva, J.; Powers, A.M.; Mead, P.; Honein, M.A.; Moore, C.A.; et al. Zika virus disease: A CDC update for pediatric health care providers. Pediatrics 2016, 137, e20160621. [Google Scholar] [CrossRef] [PubMed]
- Motta, I.J.; Spencer, B.R.; Cordeiro da Silva, S.G.; Arruda, M.B.; Dobbin, J.A.; Gonzaga, Y.B.; Arcuri, I.P.; Tavares, R.C.; Atta, E.H.; Fernandes, R.F.; et al. Evidence for transmission of Zika virus by platelet transfusion. N. Engl. J. Med. 2016, 375, 1101–1103. [Google Scholar] [CrossRef] [PubMed]
- Oehler, E.; Watrin, L.; Larre, P.; Leparc-Goffart, I.; Lastère, S.; Valour, F.; Baudouin, L.; Mallet, H.P.; Musso, D.; Ghawche, F. Zika virus infection complicated by Guillain-Barré syndrome—Case report, French Polynesia, December 2013. Eurosurveillance 2014, 19, 20720. [Google Scholar] [CrossRef] [PubMed]
- Possas, C.; Brasil, P.; Marzochi, M.C.; Tanuri, A.; Martins, R.M.; Marques, E.T.; Bonaldo, M.C.; Ferreira, A.G.; Lourenço-de-Oliveira, R.; Nogueira, R.M.R.; et al. Zika puzzle in Brazil: Peculiar conditions of viral introduction and dissemination—A Review. Mem. Inst. Oswaldo Cruz 2017, 112, 319–327. [Google Scholar] [CrossRef] [PubMed]
- CDC. Congenital Zika Syndrome & Other Birth Defects. Available online: https://www.cdc.gov/pregnancy/zika/testing-follow-up/zika-syndrome-birth-defects.html (accessed on 22 December 2017).
- Mlakar, J.; Korva, M.; Tul, N.; Popović, M.; Poljšak-Prijatelj, M.; Mraz, J.; Kolenc, M.; Resman Rus, K.; Vesnaver Vipotnik, T.; Fabjan Vodušek, V.; et al. Zika virus associated with microcephaly. N. Engl. J. Med. 2016. [Google Scholar] [CrossRef] [PubMed]
- Brasil, P.; Pereira, J.P., Jr.; Moreira, M.E.; Ribeiro Nogueira, R.M.; Damasceno, L.; Wakimoto, M.; Rabello, R.S.; Valderramos, S.G.; Halai, U.-A.; Salles, T.S.; et al. Zika virus infection in pregnant women in Rio de Janeiro. N. Engl. J. Med. 2016, 2016, 2321–2334. [Google Scholar] [CrossRef] [PubMed]
- De Araújo, T.V.B.; Rodrigues, L.C.; de Alencar Ximenes, R.A.; de Barros Miranda-Filho, D.; Montarroyos, U.R.; de Melo, A.P.L.; Valongueiro, S.; Souza, W.V.; Braga, C.; Brandão Filho, S.P.; et al. Association between Zika virus infection and microcephaly in Brazil, January to May, 2016: Preliminary report of a case-control study. Lancet Infect. Dis. 2016, 16, 1356–1363. [Google Scholar] [CrossRef]
- Yuan, L.; Huang, X.-Y.; Liu, Z.-Y.; Zhang, F.; Zhu, X.-L.; Yu, J.-Y.; Ji, X.; Xu, Y.-P.; Li, G.; Li, C.; et al. A single mutation in the prM protein of Zika virus contributes to fetal microcephaly. Science 2017, 358, 933–936. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, S.A.; Jamieson, D.J.; Honein, M.A.; Petersen, L.R. Zika virus and birth defects—Reviewing the evidence for causality. N. Engl. J. Med. 2016, 2016, 1981–1987. [Google Scholar] [CrossRef] [PubMed]
- Broutet, N.; Krauer, F.; Riesen, M.; Khalakdina, A.; Almiron, M.; Aldighieri, S.; Espinal, M.; Low, N.; Dye, C. Zika virus as a cause of neurologic disorders. N. Engl. J. Med. 2016, 374, 1506–1509. [Google Scholar] [CrossRef] [PubMed]
- Shapiro-Mendoza, C.K. Pregnancy outcomes after maternal Zika virus infection during pregnancy—US Territories, 1 January 2016–25 April 2017. MMWR Morb. Mortal. Wkly. Rep. 2017, 66, 615–621. [Google Scholar] [CrossRef] [PubMed]
- Maciel-de-Freitas, R.; Aguiar, R.; Bruno, R.V.; Guimarães, M.C.; Lourenço-de-Oliveira, R.; Sorgine, M.H.; Struchiner, C.J.; Valle, D.; O’Neill, S.L.; Moreira, L.A. Why do we need alternative tools to control mosquito-borne diseases in Latin America? Mem. Inst. Oswaldo Cruz 2012, 107, 828–829. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.-J.S.; Higgs, S.; Vanlandingham, D.L. Biological control strategies for mosquito vectors of arboviruses. Insects 2017, 8, 21. [Google Scholar] [CrossRef] [PubMed]
- Codeço, C.T.; Lima, A.W.S.; Araújo, S.C.; Lima, J.B.P.; Maciel-de-Freitas, R.; Honório, N.A.; Galardo, A.K.R.; Braga, I.A.; Coelho, G.E.; Valle, D. Surveillance of Aedes aegypti: Comparison of house index with four alternative traps. PLoS Negl. Trop. Dis. 2015, 9, e0003475. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, M.S.; Honorio, N.A.; Garcia, L.M.T.; de Carvalho, L.C.S. Aedes aegypti control in urban areas: A systemic approach to a complex dynamic. PLoS Negl. Trop. Dis. 2017, 11, e0005632. [Google Scholar] [CrossRef] [PubMed]
- Tauil, P.L. Aspectos críticos do controle do dengue no Brasil. Cad. Saúde Pública 2002, 18, 867–871. [Google Scholar] [CrossRef] [PubMed]
- Regis, L.N.; Acioli, R.V.; Silveira, J.C.; Melo-Santos, M.A.V.; Souza, W.V.; Ribeiro, C.M.N.; da Silva, J.C.S.; Monteiro, A.M.V.; Oliveira, C.M.F.; Barbosa, R.M.R.; et al. Sustained reduction of the dengue vector population resulting from an integrated control strategy applied in two brazilian cities. PLoS ONE 2013, 8, e067682. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, D.O.; Costa-da-Silva, A.L.; Lees, R.S.; Capurro, M.L. Two step male release strategy using transgenic mosquito lines to control transmission of vector-borne diseases. Acta Trop. 2014, 132, S170–S177. [Google Scholar] [CrossRef] [PubMed]
- Reis-Castro, L. Genetically modified insects as a public health tool: Discussing the different bio-objectification within genetic strategies. Croat. Med. J. 2012, 53, 635. [Google Scholar] [CrossRef] [PubMed]
- Moreira, L.A.; Iturbe-Ormaetxe, I.; Jeffery, J.A.; Lu, G.; Pyke, A.T.; Hedges, L.M.; Rocha, B.C.; Hall-Mendelin, S.; Day, A.; Riegler, M.; et al. A Wolbachia symbiont in Aedes aegypti limits infection with dengue, chikungunya, and Plasmodium. Cell 2009, 139, 1268–1278. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, A.; Montgomery, B.; Popovici, J.; Iturbe-Ormaetxe, I.; Johnson, P.; Muzzi, F.; Greenfield, M.; Durkan, M.; Leong, Y.; Dong, Y.; et al. Successful establishment of Wolbachia in Aedes populations to suppress dengue transmission. Nature 2011, 476, 454–457. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, D.O.; McKemey, A.R.; Garziera, L.; Lacroix, R.; Donnelly, C.A.; Alphey, L.; Malavasi, A.; Capurro, M.L. Suppression of a field population of Aedes aegypti in Brazil by sustained release of transgenic male mosquitoes. PLoS Negl. Trop. Dis. 2015, 9, e0003864. [Google Scholar] [CrossRef] [PubMed]
- Abad-Franch, F.; Zamora-Perea, E.; Ferraz, G.; Padilla-Torres, S.D.; Luz, S.L. Mosquito-disseminated pyriproxyfen yields high breeding-site coverage and boosts juvenile mosquito mortality at the neighborhood scale. PLoS Negl. Trop. Dis. 2015, 9, e0003702. [Google Scholar] [CrossRef] [PubMed]
- Abad-Franch, F.; Zamora-Perea, E.; Luz, S.L. Mosquito-disseminated insecticide for citywide vector control and its potential to block arbovirus epidemics: Entomological observations and modeling results from Amazonian Brazil. PLoS Med. 2017, 14, e1002213. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Sun, K.; Chinazzi, M.; Piontti, A.P.; Dean, N.E.; Rojas, D.P.; Merler, S.; Mistry, D.; Poletti, P.; Rossi, L.; et al. Spread of Zika virus in the Americas. Proc. Natl. Acad. Sci. USA 2017, 114, E4334–E4343. [Google Scholar] [CrossRef] [PubMed]
- Bogoch, I.I.; Brady, O.J.; Kraemer, M.; German, M.; Creatore, M.I.; Kulkarni, M.A.; Brownstein, J.S.; Mekaru, S.R.; Hay, S.I.; Groot, E.; et al. Anticipating the international spread of Zika virus from Brazil. Lancet 2016, 387, 335–336. [Google Scholar] [CrossRef]
- Perkins, T.A.; Siraj, A.S.; Ruktanonchai, C.W.; Kraemer, M.U.; Tatem, A.J. Model-based projections of Zika virus infections in childbearing women in the Americas. Nat. Microbiol. 2016, 1, 16126. [Google Scholar] [CrossRef] [PubMed]
- Lessler, J.; Chaisson, L.H.; Kucirka, L.M.; Bi, Q.; Grantz, K.; Salje, H.; Carcelen, A.C.; Ott, C.T.; Sheffield, J.S.; Ferguson, N.M.; et al. Assessing the global threat from Zika virus. Science 2016, 353, aaf8160. [Google Scholar] [CrossRef] [PubMed]
- Colón-González, F.D.J.; Peres, C.; São Bernardo, C.; Hunter, P.; Lake, I. After the epidemic: Zika virus projections for Latin America and the Caribbean. PLoS Negl. Trop. Dis. 2017. [Google Scholar] [CrossRef] [PubMed]
- Muñoz, Á.G.; Thomson, M.C.; Stewart-Ibarra, A.M.; Vecchi, G.A.; Chourio, X.; Nájera, P.; Moran, Z.; Yang, X. Could the recent Zika epidemic have been predicted? Front. Microbiol. 2017, 8, 1291. [Google Scholar] [CrossRef] [PubMed]
- Lowe, R.; Barcellos, C.; Coelho, C.A.; Bailey, T.C.; Coelho, G.E.; Graham, R.; Jupp, T.; Ramalho, W.M.; Carvalho, M.S.; Stephenson, D.B.; et al. Dengue outlook for the World Cup in Brazil: An early warning model framework driven by real-time seasonal climate forecasts. Lancet Infect. Dis. 2014, 14, 619–626. [Google Scholar] [CrossRef]
- Lowe, R.; Coelho, C.A.; Barcellos, C.; Carvalho, M.S.; Catao, R.D.C.; Coelho, G.E.; Ramalho, W.M.; Bailey, T.C.; Stephenson, D.B.; Rodo, X. Evaluating probabilistic dengue risk forecasts from a prototype early warning system for Brazil. Elife 2016, 5, e11285. [Google Scholar] [CrossRef] [PubMed]
- Lowe, R.; Stewart-Ibarra, A.M.; Petrova, D.; García-Díez, M.; Borbor-Cordova, M.J.; Mejía, R.; Regato, M.; Rodó, X. Climate services for health: Predicting the evolution of the 2016 dengue season in Machala, Ecuador. Lancet Planet. Health 2017, 1, e142–e151. [Google Scholar] [CrossRef]
- Perkins, T.A. Retracing Zika’s footsteps across the Americas with computational modeling. Proc. Natl. Acad. Sci. USA 2017, 114, 5558–5560. [Google Scholar] [CrossRef] [PubMed]
- Asher, J.; Barker, C.; Chen, G.; Cummings, D.; Chinazzi, M.; Daniel-Wayman, S.; Fischer, M.; Ferguson, N.; Follman, D.; Halloran, M.E.; et al. Preliminary results of models to predict areas in the Americas with increased likelihood of Zika virus transmission in 2017. bioRxiv 2017, 187591. [Google Scholar] [CrossRef]
- CDC Zika Virus: Health Effects and Risks. Available online: https://www.cdc.gov/zika/healtheffects/index.html (accessed on 11 October 2017).
- Ministério da Saúde. Secretaria de Atenção à Saúde. Protocolo de Atenção à Saúde e Resposta à Ocorrência de Microcefalia Relacionada à Infecção pelo Vírus Zika; Ministério da Saúde: Brasília, Brazil, 2016.
- Coelho, F.C.; Armstrong, M.; Saraceni, V.; Lemos, C. Can Zika account for the missing babies? Front. Public Health 2017, 5, 317. [Google Scholar] [CrossRef] [PubMed]
- Marteleto, L.J.; Weitzman, A.; Coutinho, R.Z.; Valongueiro Alves, S. Women’s reproductive intentions and behaviors during the Zika epidemic in Brazil. Popul. Dev. Rev. 2017, 43, 199–227. [Google Scholar] [CrossRef]
- Human Rights Watch. Neglected and Unprotected: The Impact of the Zika Outbreak on Women and Girls in Northeastern Brazil. Available online: https://www.hrw.org/report/2017/07/12/neglected-and-unprotected/impact-zika-outbreak-women-and-girls-northeastern-brazil (accessed on 5 November 2017).
- Aiken, A.R.; Scott, J.G.; Gomperts, R.; Trussell, J.; Worrell, M.; Aiken, C.E. Requests for abortion in Latin America related to concern about Zika virus exposure. N. Engl. J. Med. 2016, 375, 396–398. [Google Scholar] [CrossRef] [PubMed]
- Darney, B.G.; Aiken, A.R.A.; Küng, S. Access to Contraception in the Context of Zika: Health System challenges and responses. Obstet. Gynecol. 2017, 129, 638–642. [Google Scholar] [CrossRef] [PubMed]
- Baum, P.; Fiastro, A.; Kunselman, S.; Vega, C.; Ricardo, C.; Galli, B.; Nascimento, M.; Baum, P.; Fiastro, A.; Kunselman, S.; et al. Ensuring a rights-based health sector response to women affected by Zika. Cad. Saúde Pública 2016, 32. [Google Scholar] [CrossRef]
- Officer, A.; Posarac, A. World Report on Disability; World Health Organ: Geneva, Switzerland, 2011. [Google Scholar]
- Banks, L.M.; Polack, S. The Economic Costs of Exclusion and Gains of Inclusion of People with Disabilities; London School of Hygiene and Tropical Medicine: London, UK, 2013. [Google Scholar]
- Kuper, H.; Nyapera, V.; Evans, J.; Munyendo, D.; Zuurmond, M.; Frison, S.; Mwenda, V.; Otieno, D.; Kisia, J. Malnutrition and childhood disability in Turkana, Kenya: Results from a case-control study. PLoS ONE 2015, 10, e0144926. [Google Scholar] [CrossRef] [PubMed]
- Jones, L.; Bellis, M.A.; Wood, S.; Hughes, K.; McCoy, E.; Eckley, L.; Bates, G.; Mikton, C.; Shakespeare, T.; Officer, A. Prevalence and risk of violence against children with disabilities: A systematic review and meta-analysis of observational studies. Lancet 2012, 380, 899–907. [Google Scholar] [CrossRef]
- Kuper, H.; Monteath-van Dok, A.; Wing, K.; Danquah, L.; Evans, J.; Zuurmond, M.; Gallinetti, J. The impact of disability on the lives of children; cross-sectional data including 8900 children with disabilities and 898,834 children without disabilities across 30 countries. PLoS ONE 2014, 9, e107300. [Google Scholar] [CrossRef] [PubMed]
- Griffith, G.M.; Hastings, R.P. ‘He’s hard work, but he’s worth it’. The experience of caregivers of individuals with intellectual disabilities and challenging behaviour: A meta-synthesis of qualitative research. J. Appl. Res. Intellect. Disabil. 2014, 27, 401–419. [Google Scholar] [CrossRef] [PubMed]
- Nam, S.-J.; Park, E.-Y. Relationship between caregiving burden and depression in caregivers of individuals with intellectual disabilities in Korea. J. Ment. Health 2017, 26, 50–56. [Google Scholar] [CrossRef] [PubMed]
- UNDP. A Socio-Economic Impact Assessment of the Zika Virus in Latin America and the Caribbean: With a Focus on Brazil, Colombia and Suriname. Available online: http://www.undp.org/content/undp/en/home/librarypage/hiv-aids/a-socio-economic-impact-assessment-of-the-zika-virus-in-latin-am.html (accessed on 19 November 2017).
- PAHO. PAHO Statement on Zika Virus Transmission and Prevention; Pan American Health Organization: Washington, DC, USA, 2016. [Google Scholar]
- WHO. INFANT Feeding in Areas of Zika Virus Transmission—Summary of Rapid Advice Guideline. Available online: http://apps.who.int/iris/bitstream/10665/204473/1/WHO_ZIKV_MOC_16.5_eng.pdf?ua=1 (accessed on 21 October 2017).
- UN General Assembly. Convention on the Rights of Persons with Disabilities. Available online: https://treaties.un.org/doc/source/docs/A_RES_61_106-E.pdf (accessed on 6 January 2018).
- WHO. Fifth Meeting of the Emergency Committee under the International Health Regulations (2005) Regarding Microcephaly, Other Neurological Disorders and Zika Virus. Available online: http://www.who.int/mediacentre/news/statements/2016/zika-fifth-ec/en/ (accessed on 22 November 2017).
- Ministério da Saúde. Ministério da Saúde Declara Fim da Emergência Nacional para Zika. Available online: http://www.brasil.gov.br/saude/2017/05/ministerio-da-saude-declara-fim-da-emergencia-nacional-para-zika (accessed on 9 November 2017).



© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lowe, R.; Barcellos, C.; Brasil, P.; Cruz, O.G.; Honório, N.A.; Kuper, H.; Carvalho, M.S. The Zika Virus Epidemic in Brazil: From Discovery to Future Implications. Int. J. Environ. Res. Public Health 2018, 15, 96. https://doi.org/10.3390/ijerph15010096
Lowe R, Barcellos C, Brasil P, Cruz OG, Honório NA, Kuper H, Carvalho MS. The Zika Virus Epidemic in Brazil: From Discovery to Future Implications. International Journal of Environmental Research and Public Health. 2018; 15(1):96. https://doi.org/10.3390/ijerph15010096
Chicago/Turabian StyleLowe, Rachel, Christovam Barcellos, Patrícia Brasil, Oswaldo G. Cruz, Nildimar Alves Honório, Hannah Kuper, and Marilia Sá Carvalho. 2018. "The Zika Virus Epidemic in Brazil: From Discovery to Future Implications" International Journal of Environmental Research and Public Health 15, no. 1: 96. https://doi.org/10.3390/ijerph15010096
APA StyleLowe, R., Barcellos, C., Brasil, P., Cruz, O. G., Honório, N. A., Kuper, H., & Carvalho, M. S. (2018). The Zika Virus Epidemic in Brazil: From Discovery to Future Implications. International Journal of Environmental Research and Public Health, 15(1), 96. https://doi.org/10.3390/ijerph15010096




