Multidisciplinary Intervention and Acceptance and Commitment Therapy for Return-to-Work and Increased Employability among Patients with Mental Illness and/or Chronic Pain: A Randomized Controlled Trial
Abstract
:1. Introduction
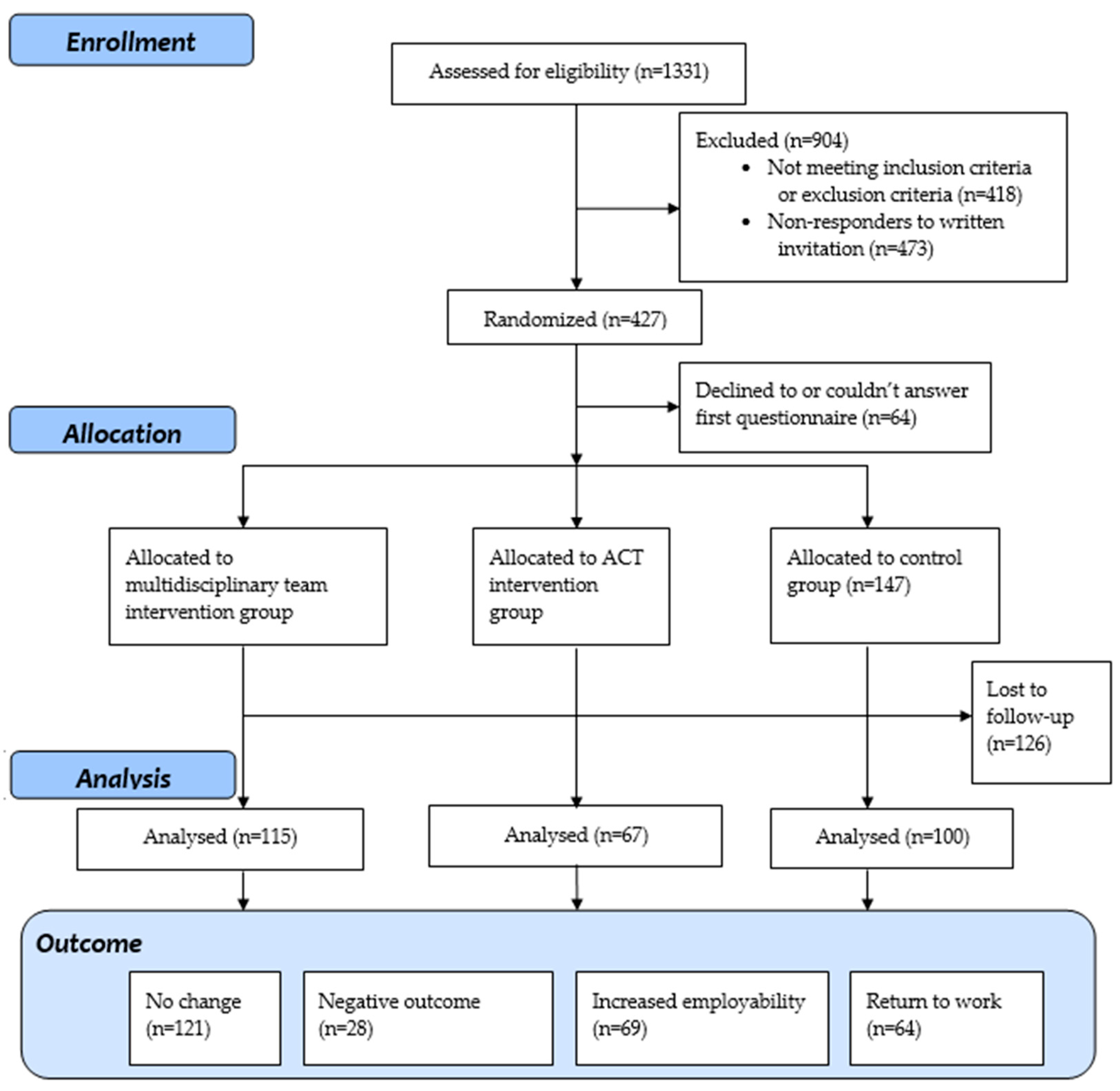
2. Materials and Methods
2.1. Subsection
2.2. Interventions
2.3. Questionnaires and Outcome Measures
2.4. Analyses
2.5. Ethical Considerations and Trial Registration
3. Results
3.1. Return-to-Work, Increased Employability, Negative Outcome, or No Change
3.2. Logistic Regression Models
3.3. Multinomial Regression Models
4. Discussion
Strengths and Limitations
5. Conclusions and Practice Implications
Author Contributions
Funding
Conflicts of Interest
References
- Henderson, M.; Harvey, S.B.; Overland, S.; Mykletun, A.; Hotopf, M. Work and common psychiatric disorders. J. R. Soc. Med. 2011, 104, 198–207. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Linder, J.; Ekholm, K.S.; Jansen, G.B.; Lundh, G.; Ekholm, J. Long-term sick leavers with difficulty in resuming work: Comparisons between psychiatric-somatic comorbidity and monodiagnosis. Int. J. Rehabil. Res. 2009, 32, 20–35. [Google Scholar] [CrossRef] [PubMed]
- Dewa, C.S.; Loong, D.; Bonato, S.; Joosen, M.C.W. The effectiveness of return-to-work interventions that incorporate work-focused problem-solving skills for workers with sickness absences related to mental disorders: A systematic literature review. BMJ Open 2015, 5, e007122. [Google Scholar] [CrossRef] [PubMed]
- Government Offices of Sweden. Regeringens Proposition 2007/08:136. En Reformerad Sjukskrivningsprocess för ökad Återgång i Arbete. [Government Proposition 2007/08: 136. A Reformed Sick Leave Process to Increase Return to Work]. Available online: https://www.riksdagen.se/sv/dokument-lagar/dokument/proposition/en-reformerad-sjukskrivningsprocess-for-okad_GV03136/html (accessed on 29 May 2018).
- Oyeflaten, I.; Lie, S.A.; Ihlebaek, C.M.; Eriksen, H.R. Multiple transitions in sick leave, disability benefits, and return to work—A 4-year follow-up of patients participating in a work-related rehabilitation program. BMC Public Health 2012, 12, 748. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marnetoft, S.U.; Selander, J. Long-term effects of early versus delayed vocational rehabilitation—A four-year follow-up. Disabil. Rehabil. 2002, 24, 741–745. [Google Scholar] [CrossRef] [PubMed]
- Roelen, C.A.; Norder, G.; Koopmans, P.C.; van Rhenen, W.; van der Klink, J.J.; Bultmann, U. Employees sick-listed with mental disorders: Who returns to work and when? J. Occup. Rehabil. 2012, 22, 409–417. [Google Scholar] [CrossRef] [PubMed]
- Cancelliere, C.; Donovan, J.; Stochkendahl, M.J.; Biscardi, M.; Ammendolia, C.; Myburgh, C.; Cassidy, J.D. Factors affecting return to work after injury or illness: Best evidence synthesis of systematic reviews. Chiropr. Man. Ther. 2016, 24, 32. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van der Klink, J.J.; Blonk, R.W.; Schene, A.H.; van Dijk, F.J. The benefits of interventions for work-related stress. Am. J. Public Health 2001, 91, 270–276. [Google Scholar] [PubMed]
- Cullen, K.L.; Irvin, E.; Collie, A.; Clay, F.; Gensby, U.; Jennings, P.A.; Hogg-Johnson, S.; Kristman, V.; Laberge, M.; McKenzie, D.; et al. Effectiveness of workplace interventions in return-to-work for musculoskeletal, pain-related and mental health conditions: An update of the evidence and messages for practitioners. J. Occup. Rehabil. 2018, 28, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Lytsy, P.; Larsson, K.; Anderzen, I. Health in women on long-term sick leave because of pain or mental illness. Int. J. Rehabil. Res. 2015, 38, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Lytsy, P.; Carlsson, L.; Anderzen, I. Effectiveness of two vocational rehabilitation programmes in women with long-term sick leave due to pain syndrome or mental illness: 1-Year follow-up of a randomized controlled trial. J. Rehabil. Med. 2017, 49, 170–177. [Google Scholar] [CrossRef] [PubMed]
- Hacker, T.; Stone, P.; MacBeth, A. Acceptance and commitment therapy—Do we know enough? Cumulative and sequential meta-analyses of randomized controlled trials. J. Affect. Disord. 2016, 190, 551–565. [Google Scholar] [CrossRef] [PubMed]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [PubMed]
- Schwarzer, R.; Jerusalem, M. Self-efficacy measurement and generalized self-efficacy scale. In Measures in Health Psychology: A User’s Portfolio; Johnston, M.W., John, S.C.W., Eds.; NFER-NELSON: Windsor, UK, 1995; pp. 33–39. [Google Scholar]
- Schwarzer, R. Everything You Wanted to Know about the General Self-Efficacy Scale but Were Afraid to Ask. Available online: http://userpage.fu-berlin.de/~health/faq_gse.pdf (accessed on 6 July 2016).
- Love, J.; Moore, C.D.; Hensing, G. Validation of the Swedish translation of the general self-efficacy scale. Qual. Life Res. 2012, 21, 1249–1253. [Google Scholar] [CrossRef] [PubMed]
- Van der Klink, J.J.; Blonk, R.W.; Schene, A.H.; van Dijk, F.J. Reducing long term sickness absence by an activating intervention in adjustment disorders: A cluster randomised controlled design. Occup. Environ. Med. 2003, 60, 429–437. [Google Scholar] [CrossRef] [PubMed]
- Franche, R.-L.; Cullen, K.; Clarke, J.; Irvin, E.; Sinclair, S.; Frank, J. Workplace-based return-to-work interventions: A systematic review of the quantitative literature. J. Occup. Rehabil. 2005, 15, 607–631. [Google Scholar] [CrossRef] [PubMed]
- Brouwers, E.P.; Tiemens, B.G.; Terluin, B.; Verhaak, P.F. Effectiveness of an intervention to reduce sickness absence in patients with emotional distress or minor mental disorders: A randomized controlled effectiveness trial. Gen. Hosp. Psychiatry 2006, 28, 223–229. [Google Scholar] [CrossRef] [PubMed]
- Van Rhenen, W.; Blonk, R.W.; Schaufeli, W.B.; van Dijk, F.J. Can sickness absence be reduced by stress reduction programs: On the effectiveness of two approaches. Int. Arch. Occup. Environ. Health 2007, 80, 505–515. [Google Scholar] [CrossRef] [PubMed]
- Netterstrøm, B.; Friebel, L.; Ladegaard, Y. Effects of a multidisciplinary stress treatment programme on patient return to work rate and symptom reduction: Results from a randomised, wait-list controlled trial. Psychother. Psychosom. 2013, 82, 177–186. [Google Scholar] [CrossRef] [PubMed]
- Momsen, A.H.; Stapelfeldt, C.M.; Nielsen, C.V.; Nielsen, M.B.; Aust, B.; Rugulies, R.; Jensen, C. Effects of a randomized controlled intervention trial on return to work and health care utilization after long-term sickness absence. BMC Public Health 2016, 16, 1149. [Google Scholar] [CrossRef] [PubMed]
- Hayes, S.C.; Luoma, J.B.; Bond, F.W.; Masuda, A.; Lillis, J. Acceptance and commitment therapy: Model, processes and outcomes. Behav. Res. Ther. 2006, 44, 1–25. [Google Scholar] [CrossRef] [PubMed]
- Nieuwenhuijsen, K.; Faber, B.; Verbeek, J.H.; Neumeyer-Gromen, A.; Hees, H.L.; Verhoeven, A.C.; van der Feltz-Cornelis, C.M.; Bultmann, U. Interventions to improve return to work in depressed people. Cochrane Database Syst. Rev. 2014, 12, CD006237. [Google Scholar] [CrossRef] [PubMed]
- Vingard, E.; Alexanderson, K.; Norlund, A. Swedish council on technology assessment in health care (SBU). Chapter 9. Consequences of being on sick leave. Scand. J. Public Health Suppl. 2004, 63, 207–215. [Google Scholar] [CrossRef] [PubMed]
- Soklaridis, S.; Ammendolia, C.; Cassidy, D. Looking upstream to understand low back pain and return to work: Psychosocial factors as the product of system issues. Soc. Sci. Med. 2010, 71, 1557–1566. [Google Scholar] [CrossRef] [PubMed]
- Gehlert, S.; Sohmer, D.; Sacks, T.; Mininger, C.; McClintock, M.; Olopade, O. Targeting health disparities: A model linking upstream determinants to downstream interventions: Knowing about the interaction of societal factors and disease can enable targeted interventions to reduce health disparities. Health Aff. 2008, 27, 339–349. [Google Scholar] [CrossRef] [PubMed]
- Salmi, P.; Svedberg, P.; Hagberg, J.; Lundh, G.; Linder, J.; Alexanderson, K. Outcome of multidisciplinary investigations of long-term sickness absentees. Disabil. Rehabil. 2009, 31, 131–137. [Google Scholar] [CrossRef] [PubMed]
| Variable | Group/Measure | MDT Group | ACT Group | Control Group | Total |
|---|---|---|---|---|---|
| Sex | Female | 90.4 | 100.0 | 93.9 | 93.9 |
| Male | 9.6 | 0.0 | 6.1 | 6.1 | |
| Age, years | Mean (SD) | 49.9 (8.5) | 47.8 (7.8) | 48.0 (8.3) | 48.7 (8.3) |
| Education | Compulsory school | 22.2 | 14.7 | 21.1 | 20.1 |
| Secondary school or equal | 48.9 | 44.0 | 46.5 | 46.9 | |
| University | 28.9 | 41.3 | 32.5 | 33.0 | |
| HADS a | Anxiety, mean (SD) | 10.9 (5.0) | 10.1 (4.9) | 11.1 (5.3) | 10.8 (5.1) |
| Depression, mean (SD) | 9.5 (4.7) | 8.5 (4.2) | 9.1 (5.1) | 9.1 (4.7) | |
| SE b | SE, mean | 2.3 (0.7) | 2.4 (0.7) | 2.3 (0.7) | 2.3 (0.7) |
| Employment contract | Employed | 66.3 | 57.8 | 61.9 | 62.8 |
| Not employed | 33.7 | 42.2 | 38.1 | 37.2 | |
| Extent of sick leave | Full-time | 55.7 | 53.9 | 55.2 | 55.1 |
| Part-time | 44.3 | 46.1 | 44.8 | 44.9 | |
| Years with income replacement | Mean (SD) | 8.1 (3.3) | 7.6 (3.1) | 7.5 (3.2) | 7.8 (3.2) |
| Dosage of intervention | Sessions with psychologist, mean (SD) | 4.7 (6.4) | 8.0 (6.0) | 0.0 (0.0) | 3.9 (5.9) |
| Sessions with MD c. OT d. PT e and SW f, mean (SD) | 4.4 (5.4) | 0.0 (0.0) | 0.0 (0.0) | 1.8 (4.1) | |
| Total sessions in the project, mean (SD) | 9.1 (8.4) | 8.0 (6.0) | 0.0 (0.0) | 5.7 (7.4) |
| Outcome | MDT Group | ACT Group | Control Group | Overall |
|---|---|---|---|---|
| RTW (%) | 31.3 ** | 17.9 ** | 16.0 ** | 22.7 |
| Increased employability (%) | 27.0 ** | 35.8 ** | 14.0 ** | 24.5 |
| Negative outcome (%) | 4.3 ** | 9.0 ** | 17.0 ** | 9.9 |
| No change (%) | 37.4 ** | 37.3 ** | 53.0 ** | 42.9 |
| Variable | Group/Measure | Crude OR (95% CI) | Model 1 OR (95% CI) | Model 2 OR (95% CI) |
|---|---|---|---|---|
| Intervention group | Group | |||
| Control (ref.) | 1 | 1 | 1 | |
| MDTa group | 3.26 ** (1.85–5.74) | 4.22 ** (2.18–8.15) | 4.62 ** (2.27–9.41) | |
| ACTb group | 2.71 ** (1.42–5.16) | 2.42 * (1.17–4.97) | 2.35 * (1.07–5.19) | |
| Demographic | Age | 0.96 * (0.94–0.99) | 0.96 * (0.92 - 0.99) | 0.96 * (0.93–1.00) |
| Education level | ||||
| Compulsory school | 1 | 1 | 1 | |
| Secondary school-equal | 1.87 (0.91–3.82) | 1.60 (0.74–3.46) | 1.98 (0.85–4.58) | |
| University | 1.24 (0.58–2.66) | 1.23 (0.55–2.77) | 1.28 (0.53–3.11) | |
| Health and work related factors | HADSc, Anxiety | 0.99 (0.94–1.04) | 1.05 (0.96–1.14) | |
| HADSc Depression | 0.97 (0.92–1.02) | 0.97 (0.89–1.06) | ||
| Self-efficacy (<2.30) | 1 | 1 | ||
| Self-efficacy (≥2.30) | 1.76 * (1.07–2.89) | 2.75 ** (1.33–5.72) | ||
| Employment contract | ||||
| Not employed | 1 | 1 | ||
| Employed | 0.70 (0.42–1.15) | 0.78 (0.38–1.61) | ||
| Extent of sick leave | ||||
| Full time | 1 | 1 | ||
| Part time | 0.67 (0.42–1.07) | 0.56 (0.29–1.10) | ||
| Years with income replacement | 0.97 (0.90–1.05) | 0.97 (0.88- 1.06) | ||
| Nagelkerke r2 | 14.0% | 24.1% |
| Variable | Return to Work or Change in System Position | ||||||
|---|---|---|---|---|---|---|---|
| Negative Outcome | Increased Employability | Return to Work | |||||
| Crude OR (95% CI) | Adjusted OR (95% CI) | Crude OR (95% CI) | Adjusted OR (95% CI) | Crude OR (95% CI) | Adjusted OR (95% CI) | ||
| Intervention group | Group | ||||||
| Control (ref.) | 1 | 1 | 1 | 1 | 1 | 1 | |
| MDTa group | 0.36 (0.12–1.06) | 0.19 * (0.05–0.72) | 2.73 ** (1.29–5.77) | 4.24 ** (1.60–11.26) | 2.77 ** (1.36–5.66) | 3.31 ** (1.39–7.87) | |
| ACTb group | 0.75 (0.26–2.13) | 0.36 (0.10–1.35) | 3.63 ** (1.61–8.19) | 3.22 * (1.13–9.15) | 1.56 (0.66–3.86) | 1.36 (0.48–3.86) | |
| Demographic | Age | 0.99 (0.94–1.04) | 0.94 (0.88–1.01) | 0.95 ** (0.92–0.99) | 0.94 * (0.90–0.99) | 0.97 (0.93–1.01) | 0.96 (0.92–1.01) |
| Education level | |||||||
| Compulsory school | 1 | 1 | 1 | 1 | 1 | 1 | |
| Secondary school or equal | 1.41 (0.40–4.91) | 0.76 (0.16–3.57) | 3.78 * (1.31–10.92) | 4.52 * (1.29–15.87) | 1.16 (0.49–2.77) | 1.08 (0.40–2.89) | |
| University | 1.44 (0.40–5.22) | 0.61 (0.13–2.98) | 1.79 (0.57–5.64) | 2.24 (0.58–8.71) | 1.10 (0.45–2.74) | 0.85 (0.30–2.39) | |
| Health and work-related factors | HADSc, Anxiety | 0.93 (0.85–1.01) | 0.92 (0.80–1.06) | 0.99 (0.93–1.06) | 1.02 (0.92–1.14) | 0.96 (0.90–1.02) | 1.05 (0.94–1.16) |
| HADSc, Depression | 0.93 (0.85–1.02) | 1.14 (0.96–1.35) | 0.96 (0.90–1.02) | 0.98 (0.87–1.10) | 0.96 (0.89–1.02) | 1.01 (0.90–1.13) | |
| Self-efficacy (<2.30) | 1 | 1 | 1 | 1 | 1 | 1 | |
| Self-efficacy (≥2.30) | 1.99 (0.84–4.73) | 1.81 (0.52–6.34) | 1.74 (0.93–3.25) | 2.71* (1.07–6.91) | 2.35 * (1.22–4.50) | 3.31 ** (1.34–8.15) | |
| Employment contract | |||||||
| Not employed | 1 | 1 | 1 | 1 | 1 | 1 | |
| Have work | 3.96 * (1.13–13.93) | 1.66 (0.32–8.70 | 0.52 * (0.28–0.95) | 0.64 (0.27–1.54) | 1.55 (0.78–3.11) | 1.09 (0.44–2.71) | |
| Extent of sick leave | |||||||
| Full time | 1 | 1 | 1 | 1 | 1 | 1 | |
| Part time | 15.65 ** (3.55–68.94) | 34.57 ** (3.84–311.31) | 0.56 (0.30–1.05) | 0.44 (0.17–1.02) | 1.65 (0.89–3.05) | 1.42 (0.62–3.21) | |
| Years, with income replacement | 1.07 (0.94–1.22) | 1.07 (0.89–1.29) | 0.99 (0.90–1.09) | 0.99 (0.89–1.12) | 0.98 (0.89–1.07) | 0.96 (0.85–1.07) | |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Berglund, E.; Anderzén, I.; Andersén, Å.; Carlsson, L.; Gustavsson, C.; Wallman, T.; Lytsy, P. Multidisciplinary Intervention and Acceptance and Commitment Therapy for Return-to-Work and Increased Employability among Patients with Mental Illness and/or Chronic Pain: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2018, 15, 2424. https://doi.org/10.3390/ijerph15112424
Berglund E, Anderzén I, Andersén Å, Carlsson L, Gustavsson C, Wallman T, Lytsy P. Multidisciplinary Intervention and Acceptance and Commitment Therapy for Return-to-Work and Increased Employability among Patients with Mental Illness and/or Chronic Pain: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health. 2018; 15(11):2424. https://doi.org/10.3390/ijerph15112424
Chicago/Turabian StyleBerglund, Erik, Ingrid Anderzén, Åsa Andersén, Lars Carlsson, Catharina Gustavsson, Thorne Wallman, and Per Lytsy. 2018. "Multidisciplinary Intervention and Acceptance and Commitment Therapy for Return-to-Work and Increased Employability among Patients with Mental Illness and/or Chronic Pain: A Randomized Controlled Trial" International Journal of Environmental Research and Public Health 15, no. 11: 2424. https://doi.org/10.3390/ijerph15112424
APA StyleBerglund, E., Anderzén, I., Andersén, Å., Carlsson, L., Gustavsson, C., Wallman, T., & Lytsy, P. (2018). Multidisciplinary Intervention and Acceptance and Commitment Therapy for Return-to-Work and Increased Employability among Patients with Mental Illness and/or Chronic Pain: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health, 15(11), 2424. https://doi.org/10.3390/ijerph15112424





