Biological Age Is Associated with the Active Use of Nutrition Data
Abstract
:1. Introduction
2. Methods
2.1. Study Population
2.2. Variables
2.3. Statistical Analysis
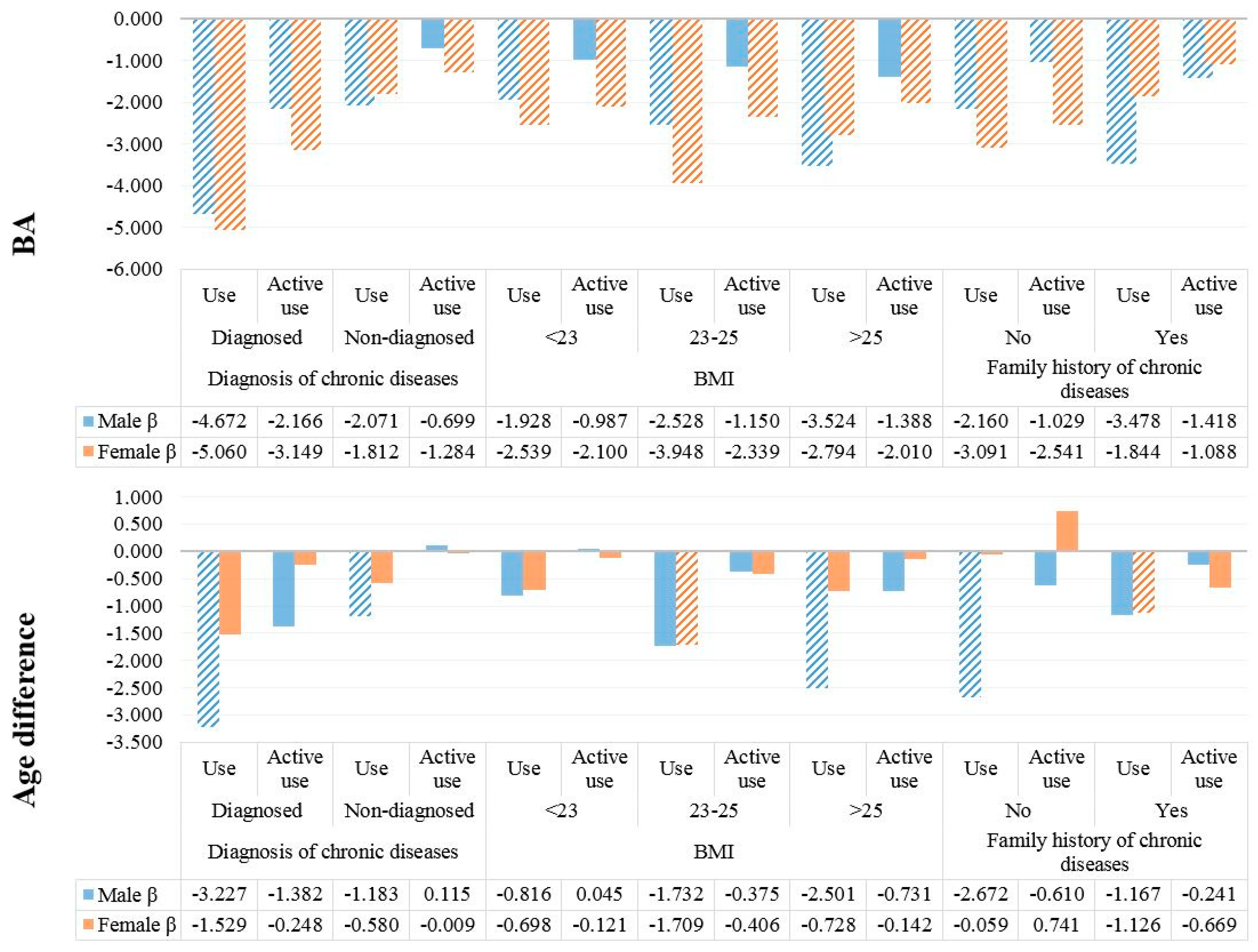
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Ingram, D.K.; Nakamura, E.; Smucny, D.; Roth, G.S.; Lane, M.A. Strategy for identifying biomarkers of aging in long-lived species. Exp. Gerontol. 2001, 36, 1025–1034. [Google Scholar] [CrossRef]
- Karasik, D.; Demissie, S.; Cupples, L.A.; Kiel, D.P. Disentangling the genetic determinants of human aging: Biological age as an alternative to the use of survival measures. J. Gerontol. Ser. A 2005, 60, 574–587. [Google Scholar] [CrossRef]
- Lorig, K.R.; Ritter, P.; Stewart, A.L.; Sobel, D.S.; Brown, B.W., Jr.; Bandura, A.; Gonzalez, V.M.; Laurent, D.D.; Holman, H.R. Chronic disease self-management program: 2-Year health status and health care utilization outcomes. Med. Care 2001, 1217–1223. [Google Scholar] [CrossRef]
- Bauer, U.E.; Briss, P.A.; Goodman, R.A.; Bowman, B.A. Prevention of chronic disease in the 21st century: Elimination of the leading preventable causes of premature death and disability in the USA. Lancet 2014, 384, 45–52. [Google Scholar] [CrossRef]
- Nakamura, E.; Moritani, T.; Kanetaka, A. Biological age versus physical fitness age. Eur. J. Appl. Physiol. Occup. Physiol. 1989, 58, 778–785. [Google Scholar] [CrossRef] [PubMed]
- Finkel, D.; Whitfield, K.; McGue, M. Genetic and environmental influences on functional age: A twin study. J. Gerontol. Ser. B 1995, 50, P104–P113. [Google Scholar] [CrossRef]
- Mitnitski, A.B.; Graham, J.E.; Mogilner, A.J.; Rockwood, K. Frailty, fitness and late-life mortality in relation to chronological and biological age. BMC Geriatr. 2002, 2, 1. [Google Scholar] [CrossRef] [Green Version]
- Fishman, L.S. Chronological versus skeletal age, an evaluation of craniofacial growth. Angle Orthod. 1979, 49, 181–189. [Google Scholar] [PubMed]
- Borkan, G.A.; Norris, A.H. Assessment of biological age using a profile of physical parameters. J. Gerontol. 1980, 35, 177–184. [Google Scholar] [CrossRef] [PubMed]
- Furukawa, T.; Inoue, M.; Kajiya, F.; Inada, H.; Takasugi, S.; Fukui, S.; Takeda, H.; Abe, H. Assessment of biological age by multiple regression analysis. J. Gerontol. 1975, 30, 422–434. [Google Scholar] [CrossRef] [PubMed]
- Post Hospers, G.; Smulders, Y.M.; Maier, A.B.; Deeg, D.J.; Muller, M. Relation between blood pressure and mortality risk in an older population: Role of chronological and biological age. J. Intern. Med. 2015, 277, 488–497. [Google Scholar] [CrossRef] [PubMed]
- Wahlin, Å.; MacDonald, S.W.; de Frias, C.M.; Nilsson, L.G.; Dixon, R.A. How do health and biological age influence chronological age and sex differences in cognitive aging: Moderating, mediating, or both? Psychol. Aging 2006, 21, 318. [Google Scholar] [CrossRef] [PubMed]
- Soriano-Tárraga, C.; Mola-Caminal, M.; Giralt-Steinhauer, E.; Ois, A.; Rodríguez-Campello, A.; Cuadrado-Godia, E.; Gómez-González, A.; Vivanco-Hidalgo, R.M.; Fernández-Cadenas, I.; Cullell, N.; et al. Biological age is better than chronological as predictor of 3-month outcome in ischemic stroke. Neurology 2017. [Google Scholar] [CrossRef] [PubMed]
- Twisk, J.; Kemper, H.; Van Mechelen, W. The relationship between physical fitness and physical activity during adolescence and cardiovascular disease risk factors at adult age. The Amsterdam Growth and Health Longitudinal Study. Int. J. Sports Med. 2002, 23, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Post, G.; Kemper, H.; Twisk, J.; Van Mechelen, W. The association between dietary patterns and cardio vascular disease risk indicators in healthy youngsters: Results covering fifteen years of longitudinal development. Eur. J. Clin. Nutr. 1997, 51, 387. [Google Scholar] [CrossRef] [PubMed]
- Park, H.-K. Nutrition policy in South Korea. Asia Pac. J. Clin. Nutr. 2008, 17, 343–345. [Google Scholar] [PubMed]
- Guthrie, J.F.; Fox, J.J.; Cleveland, L.E.; Welsh, S. Who uses nutrition labeling, and what effects does label use have on diet quality? J. Nutr. Educ. 1995, 27, 163–172. [Google Scholar] [CrossRef]
- Kim, J.Y.; Kweon, K.H.; Kim, M.J.; Park, E.-C.; Jang, S.-Y.; Kim, W.; Han, K.-T. Is nutritional labeling associated with individual health? The effects of labeling-based awareness on dyslipidemia risk in a South Korean population. Nutr. J. 2015, 15, 81. [Google Scholar] [CrossRef] [PubMed]
- Chaudhry, B.; Wang, J.; Wu, S.; Maglione, M.; Mojica, W.; Roth, E.; Morton, S.C.; Shekelle, P.G. Systematic review: Impact of health information technology on quality, efficiency, and costs of medical care. Ann. Intern. Med. 2006, 144, 742–752. [Google Scholar] [CrossRef] [PubMed]
- Kang, Y.G.; Suh, E.; Chun, H.; Kim, S.-H.; Kim, D.K.; Bae, C.-Y. Models for estimating the metabolic syndrome biological age as the new index for evaluation and management of metabolic syndrome. Clin. Interv. Aging 2017, 12, 253. [Google Scholar] [CrossRef] [PubMed]
- Dubina, T.; Mints, A.Y.; Zhuk, E. Biological age and its estimation. III. Introduction of a correction to the multiple regression model of biological age and assessment of biological age in cross-sectional and longitudinal studies. Exp. Gerontol. 1984, 19, 133–143. [Google Scholar] [CrossRef]
- Variyam, J.N.; Cawley, J. Nutrition Labels and Obesity; National Bureau of Economic Research: Cambridge, MA, USA, 2006. [Google Scholar]
- Post, R.E.; Mainous, A.G., III; Diaz, V.A.; Matheson, E.M.; Everett, C.J. Use of the nutrition facts label in chronic disease management: Results from the National Health and Nutrition Examination Survey. J. Am. Diet. Assoc. 2010, 110, 628–632. [Google Scholar] [CrossRef] [PubMed]
- Goggins, W.B.; Woo, J.; Sham, A.; Ho, S.C. Frailty index as a measure of biological age in a Chinese population. J. Gerontol. Ser. A 2005, 60, 1046–1051. [Google Scholar] [CrossRef]
- Rose, N. In search of certainty: Risk management in a biological age. J. Public Ment. Health 2005, 4, 14–22. [Google Scholar] [CrossRef]

| Variable | Males | Females | ||
|---|---|---|---|---|
| Frequency | % | Frequency | % | |
| Use of nutrition data | ||||
| Active use | 1127 | 12.8 | 4010 | 27.5 |
| Use | 5844 | 58.8 | 7298 | 49.3 |
| Nonuse | 4038 | 28.5 | 4597 | 23.2 |
| Age (years) | ||||
| <30 | 1274 | 20.0 | 1818 | 17.2 |
| 30–39 | 1777 | 20.1 | 2947 | 20.1 |
| 40–49 | 1911 | 21.2 | 2957 | 21.8 |
| 50–59 | 2117 | 19.3 | 3262 | 19.4 |
| ≥60 | 3930 | 19.4 | 4921 | 21.4 |
| Education level | ||||
| Less than high school | 6187 | 48.7 | 10,408 | 60.6 |
| Bachelor’s degree | 4159 | 45.3 | 5043 | 36.4 |
| Master’s degree or higher | 663 | 6.0 | 454 | 3.1 |
| Economic status | ||||
| Unemployed | 2922 | 23.1 | 8118 | 48.2 |
| Employed | 8087 | 76.9 | 7787 | 51.8 |
| Household income | ||||
| Low | 1939 | 13.2 | 3077 | 16.4 |
| Medium to low | 2813 | 25.6 | 4089 | 26.6 |
| Medium to high | 3113 | 31.0 | 4327 | 28.7 |
| High | 3144 | 30.2 | 4412 | 28.3 |
| BMI (kg/m2) | ||||
| <23 | 4172 | 37.5 | 7802 | 51.7 |
| 23–25 | 2852 | 25.4 | 3465 | 20.7 |
| >25 | 3985 | 37.1 | 4638 | 27.6 |
| Chronic disease | ||||
| Diagnosed | 3482 | 23.3 | 4694 | 23.8 |
| Not diagnosed | 7527 | 76.7 | 11,211 | 76.2 |
| Aerobic exercise status | ||||
| Yes | 3501 | 35.1 | 4070 | 27.7 |
| No | 7508 | 64.9 | 11,835 | 72.3 |
| Smoking status | ||||
| Smoker | 4114 | 41.4 | 754 | 5.7 |
| Ex-smoker | 4638 | 35.8 | 822 | 6.0 |
| Nonsmoker | 2257 | 22.8 | 14,329 | 88.3 |
| Alcohol intake | ||||
| Less than twice a week | 9023 | 79.7 | 15,305 | 95.4 |
| More than twice a week | 1986 | 20.3 | 600 | 4.6 |
| Family history of chronic disease | ||||
| No | 7373 | 65.1 | 10,042 | 62.0 |
| Yes | 3636 | 34.9 | 5863 | 38.0 |
| Survey year | ||||
| 2010 | 2085 | 16.8 | 2951 | 16.8 |
| 2011 | 2031 | 17.2 | 2999 | 17.8 |
| 2012 | 1827 | 16.7 | 2781 | 16.9 |
| 2013 | 1738 | 16.6 | 2474 | 16.2 |
| 2014 | 1594 | 15.9 | 2322 | 15.6 |
| 2015 | 1734 | 16.8 | 2378 | 16.6 |
| Stress level | ||||
| Low | 8633 | 76.3 | 11,597 | 71.4 |
| High | 2376 | 23.7 | 4308 | 28.6 |
| Subjective health status | ||||
| Good | 3988 | 38.0 | 4629 | 30.0 |
| Normal | 5312 | 48.1 | 7882 | 50.2 |
| Bad | 1709 | 13.8 | 3394 | 19.8 |
| Average daily energy intake † | 2472 | 13.7 | 1740 | 7.7 |
| Total | 11,009 | 100.0 | 15,905 | 100.0 |
| Variable | Males | Females | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BA | Difference (BA–CA) | BA | Difference (BA–CA) | |||||||||
| Mean | SD | p-Value | Mean | SD | p-Value | Mean | SD | p-Value | Mean | SD | p-Value | |
| Use of Nutrition Data | ||||||||||||
| Active use | 44.34 | 20.81 | <0.0001 | 3.15 | 13.82 | 0.0128 | 43.31 | 18.25 | <0.0001 | 2.48 | 13.19 | 0.0371 |
| Use | 49.74 | 21.17 | 3.55 | 14.50 | 49.80 | 20.59 | 3.71 | 13.63 | ||||
| Nonuse | 64.66 | 18.26 | 3.12 | 14.87 | 70.11 | 18.52 | 5.86 | 14.74 | ||||
| Variable | Males | Females | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BA | Difference (BA–CA) | BA | Difference (BA–CA) | |||||||||
| β | SE | p-Value | β | SE | p-Value | β | SE | p-Value | β | SE | p-Value | |
| Use of Nutrition Data | ||||||||||||
| Active use | −2.646 | 0.573 | <0.0001 | −1.695 | 0.559 | 0.0025 | −2.787 | 0.374 | <0.0001 | −0.817 | 0.365 | 0.0256 |
| Use | −1.181 | 0.397 | 0.003 | −0.360 | 0.386 | 0.3519 | −2.161 | 0.338 | <0.0001 | −0.201 | 0.326 | 0.5385 |
| Nonuse | Ref | - | - | Ref | - | - | ||||||
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Han, K.-T.; Kim, D.W.; Kim, S.J.; Kim, S.J. Biological Age Is Associated with the Active Use of Nutrition Data. Int. J. Environ. Res. Public Health 2018, 15, 2431. https://doi.org/10.3390/ijerph15112431
Han K-T, Kim DW, Kim SJ, Kim SJ. Biological Age Is Associated with the Active Use of Nutrition Data. International Journal of Environmental Research and Public Health. 2018; 15(11):2431. https://doi.org/10.3390/ijerph15112431
Chicago/Turabian StyleHan, Kyu-Tae, Dong Wook Kim, Seung Ju Kim, and Sun Jung Kim. 2018. "Biological Age Is Associated with the Active Use of Nutrition Data" International Journal of Environmental Research and Public Health 15, no. 11: 2431. https://doi.org/10.3390/ijerph15112431
APA StyleHan, K.-T., Kim, D. W., Kim, S. J., & Kim, S. J. (2018). Biological Age Is Associated with the Active Use of Nutrition Data. International Journal of Environmental Research and Public Health, 15(11), 2431. https://doi.org/10.3390/ijerph15112431





