Children’s Weight Gain and Cardiovascular Fitness Loss over the Summer
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants and Setting
2.3. Health-Related Fitness Measures
2.4. Procedures
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Janssen, I.; LeBlanc, A.G. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int. J. Beh. Nutr. Phys. Act. 2010, 7, 40. [Google Scholar] [CrossRef] [PubMed]
- Cooper, A.R.; Goodman, A.; Page, A.S.; Sherar, L.B.; Esliger, D.W.; van Sluijs, E.M.; Andersen, L.B.; Anderssen, S.; Cardon, G.; Davey, R.; et al. Objectively measured physical activity and sedentary time in youth: The International children’s accelerometry database (ICAD). Int. J. Beh. Nutr. Phys. Act. 2015, 12, 113. [Google Scholar] [CrossRef] [PubMed]
- Weaver, R.G.; Crimarco, A.; Brusseau, T.A.; Webster, C.A.; Burns, R.D.; Hannon, J.C. Accelerometry-Derived Physical Activity of First through Third Grade Children during the Segmented School Day. J. School Health 2016, 86, 726–733. [Google Scholar] [CrossRef] [PubMed]
- Brusseau, T.A.; Finkelstein, T.; Kulinna, P.H.; Pangrazi, C. Health-Related Fitness of American Indian Youth. Res. Q. Exerc. Sport 2014, 85, 257–261. [Google Scholar] [CrossRef] [PubMed]
- Huotari, P.; Nupponen, H.; Mikkelsson, L.; Laakso, L.; Kujala, U. Adolescent physical fitness and activity as predictors of adulthood activity. J. Sport Sci. 2011, 29, 1135–1141. [Google Scholar] [CrossRef] [PubMed]
- Telama, R. Tracking of physical activity from childhood to adulthood: A review. Obes. Facts. 2009, 2, 187–195. [Google Scholar] [CrossRef] [PubMed]
- Naylor, P.J.; Nettlefold, L.; Race, D.; Hoy, C.; Ashe, M.C.; Wharf Higgins, J.; McKay, H.A. Implementation of school based physical activity interventions: A systematic review. Prev. Med. 2015, 72, 95–115. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Comprehensive School Physical Activity Programs: A Guide for Schools; Department of Health and Human Services: Atlanta, GA, USA, 2013.
- Brusseau, T.A.; Hannon, J.C.; Burns, R. The effect of a comprehensive school physical activity program on physical activity and health-related fitness in children from low-income families. J. Phys. Act. Health. 2016, 13, 888–894. [Google Scholar] [CrossRef] [PubMed]
- Brusseau, T.A.; Hannon, J.C.; Fu, Y.; Fang, Y.; Nam, K.; Goodrum, S.; Burns, R.D. Trends in physical activity, health-related fitness, and gross motor skills in children during a two-year comprehensive school physical activity program. J. Sci. Med. Sport 2018, 21, 828–832. [Google Scholar] [CrossRef] [PubMed]
- Fu, Y.; Brusseau, T.A.; Hannon, J.C.; Burns, R.D. Effect of a 12-week summer break on school day physical activity and health-related fitness in low-income children from CSPAP schools. J. Env. Public Health. 2017, 2017. [Google Scholar] [CrossRef]
- Baranowski, T.; O’Connor, T.; Johnston, C.; Hughes, S.; Moreno, J.; Chen, T.A.; Meltzer, L.; Baranowski, J. School year versus summer differences in child weight gain: A narrative review. Child Obes. 2014, 10, 18–24. [Google Scholar] [CrossRef] [PubMed]
- Von Hippel, P.T.; Powell, B.; Downey, D.B.; Rowland, N.J. The effect of school on overweight in childhood: Gain in body mass index during the school year and during summer vacation. Am. J. Public Health. 2007, 97, 696–702. [Google Scholar] [CrossRef] [PubMed]
- Brazendale, K.; Beets, M.W.; Weaver, R.G.; Pate, R.R.; Turner-McGrievy, G.M.; Kaczynski, A.T.; Chandler, J.L.; Bohnert, A.; von Hippel, P.T. Understanding differences between summer vs. school obesogenic behaviors of children: The structured days hypothesis. Int. J. Beh. Nutr. Phys. Act. 2017, 14, 100. [Google Scholar] [CrossRef] [PubMed]
- Brusseau, T.A. The intricacies of children’s physical activity. J. Hum. Kin. 2015, 47, 269–275. [Google Scholar] [CrossRef] [PubMed]
- Welk, G.; Meredith, M.D. Fitnessgram and Activitygram Test Administration Manual-Updated 4th Edition; Human Kinetics: Champaign, IL, USA, 2010. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Routledge: London, UK, 1988. [Google Scholar]
- Khambalia, A.Z.; Dickinson, S.; Hardy, L.; Gill, T.A.; Baur, L.A. A Synthesis of Existing Systematic Reviews and Meta-Analyses of School-Based Behavioural Interventions for Controlling and Preventing Obesity. Obes. Rev. 2012, 13, 214–233. [Google Scholar] [CrossRef] [PubMed]
- Pratt, C.A.; Loria, C.M.; Arteaga, S.S.; Nicastro, H.L.; Lopez-Class, M.; de Jesus, J.M.; Srinivas, P.; Maric-Bilkan, C.; Schwartz Longacre, L.; Boyington, J.E.A.; et al. A systematic review of obesity disparities research. Am. J. Prev. Med. 2017, 53, 113–122. [Google Scholar] [CrossRef] [PubMed]
- Weaver, R.G.; Beets, M.W.; Perry, M.; Hunt, E.; Brazendale, K.; Decker, L.; Turner-McGrievy, G.; Pate, R.; Youngstedt, S.D.; Saelens, B.E.; et al. Changes in Children’s Sleep and Physical Activity During a One-week versus a Three-week Break from School: A natural experiment. Sleep 2018. [Google Scholar] [CrossRef]
- Chen, T.A.; Baranowski, T.; Moreno, J.P.; O’Connor, T.M.; Hughes, S.O.; Baranowski, J.; Woehler, D.; Kimbro, R.T.; Johnston, C.A. Obesity status trajectory groups among elementary school children. BMC Public Health 2016, 16, 526. [Google Scholar] [CrossRef]
- Sallis, J.F.; McKenzie, T.L.; Alcaraz, J.E.; Kolody, B.; Faucette, N.; Hovell, M.F. The effects of a 2-year physical education program (SPARK) on physical activity and fitness in elementary school students. Sports, play and active recreation for kids. Am. J. Public Health 1997, 87, 1328–1334. [Google Scholar] [CrossRef]
- Treviño, R.P.; Fogt, D.L.; Wyatt, T.J.; Leal-Vasquez, L.; Sosa, E.; Woods, C. Diabetes risk, low fitness, and energy insufficiency levels among children from poor families. J. Am. Diet Assoc. 2008, 108, 1846–1853. [Google Scholar] [CrossRef]
- O’Loughlin, J.; Paradis, G.; Kishchuk, N.; Barnett, T.; Renaud, L. Prevalence and correlates of physical activity behaviors among elementary schoolchildren in multiethnic, low income, inner-city neighborhoods in Montreal, Canada. Ann. Epi. 1999, 9, 397–407. [Google Scholar] [CrossRef]
- Brazendale, K.; Beets, M.W.; Weaver, R.G.; Chandler, J.L.; Randel, A.B.; Turner-McGrievy, G.M.; Moore, J.B.; Huberty, J.L.; Ward, D.S. Children’s moderate to vigorous physical activity attending summer day camps. Am. J. Prev. Med. 2017, 53, 78–84. [Google Scholar] [CrossRef] [PubMed]
- Park, K.S.; Lee, M.G. Effects of summer school participation and psychosocial outcomes on changes in body composition and physical fitness during summer break. J. Exerc. Nutr. Biochem. 2015, 19, 81–90. [Google Scholar] [CrossRef] [PubMed]
- American Camp Association. Camp Trends: Tuition. 2018. Available online: https://www.acacamps.org/press-room/camp-trends/tuition (accessed on 2 October 2018).
- Cipriani, K.; Richardson, C.; Roberts, G. Family and community involvement in the comprehensive school physical activity program. JOPERD 2012, 83, 20–26. [Google Scholar] [CrossRef]
- Van Sluijs, E.M.F.; Mcminn, A.M.; Griffin, S.J. Effectiveness of interventions to promote physical activity in children and adolescents: Systematic review of controlled trials. Brit. Med. J. 2007, 335, 703–707. [Google Scholar] [CrossRef] [PubMed]
- Beets, M.W.; Okely, A.; Weaver, R.G.; Webster, C.; Lubans, D.; Brusseau, T.; Carson, R.; Cliff, D.P. The theory of expanded, extended, and enhanced opportunities for youth physical activity promotion. Int. J. Beh. Nutr. Phys. Act. 2016, 13, 120. [Google Scholar] [CrossRef] [PubMed]
- Foley, L.; Mhurchu, C.N.; Marsh, S.; Epstein, L.H.; Olds, T.; Dewes, O.; Heke, I.; Jiang, Y.; Maddison, R. Screen time weight-loss intervention targeting children at home (SWITCH): Process evaluation of a randomised controlled trial intervention. BMC Public Health 2016, 16, 439. [Google Scholar] [CrossRef]
- Cooper, H.; Valentine, J.C.; Charlton, K.; Melson, A. The effects of modified school calendars on student achievement and on school and community attitudes. Rev. Educ. Res. 2003, 73, 1–52. [Google Scholar] [CrossRef]
- Wu, A.D.; Stone, J.E. Does year-round schooling affect the outcome and growth of California’s API scores? J. Educ. Res. Policy Stud. 2010, 10, 79–97. [Google Scholar]

| Sample | Body Mass Index (kg/m2) | PACER Laps |
|---|---|---|
| Total (n = 404) | 18.6 (3.8) | 23.9 (15.2) |
| Females (n = 203) | 18.4 (3.2) | 22.6 (14.7) |
| Males (n = 201) | 18.7 (4.1) | 25.3 * (16.4) |
| Grade 1 (n = 91) | 17.9 (3.2) | 18.3 (8.1) |
| Grade 2 (n = 102) | 18.1 (3.5) | 20.1 (11.2) |
| Grade 3 (n = 97) | 19.2 † (4.1) | 25.1 † (14.5) |
| Grade 4 (n = 114) | 19.5 †† (4.4) | 24.4 † (14.2) |
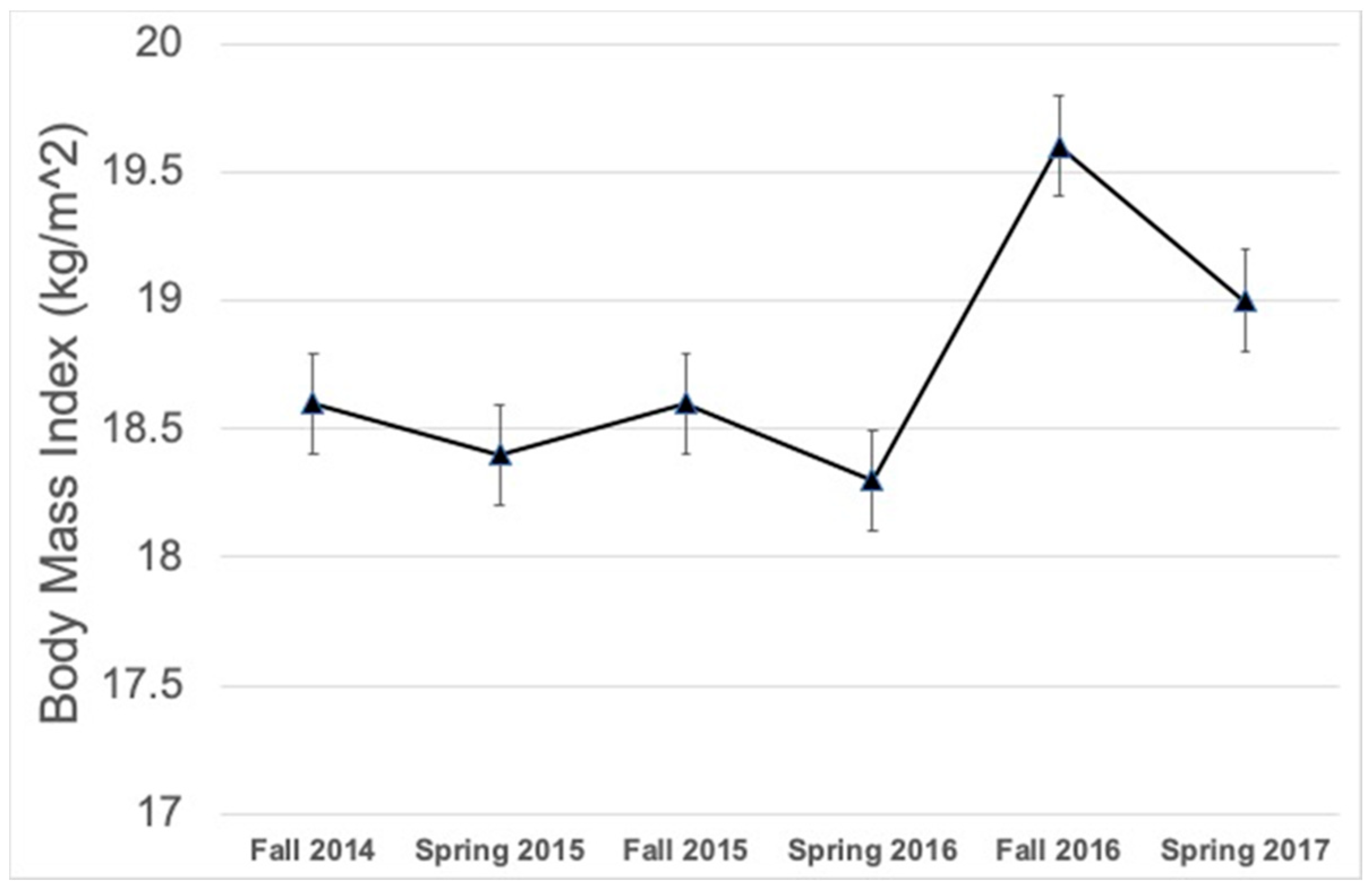
| Outcome | Time Level | b-Coefficient | 95% Confidence Interval | p-Value |
|---|---|---|---|---|
| BMI (kg/m2) | Spring 2015 | −0.2 | −0.11, 0.7 | 0.111 |
| Fall 2015 | 0.1 | −0.48, 0.47 | 0.958 | |
| Spring 2016 | −1.0 | −1.9, −0.1 | 0.028 | |
| Fall 2016 | 1.3 | 0.2, 2.4 | <0.001 | |
| Spring 2017 | 0.4 | −0.52, 1.5 | 0.351 | |
| PACER (Laps) | Spring 2015 | 3.3 | 1.8, 4.8 | <0.001 |
| Fall 2015 | −0.5 | −1.9, 0.9 | 0.515 | |
| Spring 2016 | 2.4 | 0.1, 4.6 | 0.040 | |
| Fall 2016 | −1.6 | −3.3, 0.2 | 0.073 | |
| Spring 2017 | 4.8 | 1.7, 7.9 | 0.002 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brusseau, T.A.; Burns, R.D. Children’s Weight Gain and Cardiovascular Fitness Loss over the Summer. Int. J. Environ. Res. Public Health 2018, 15, 2770. https://doi.org/10.3390/ijerph15122770
Brusseau TA, Burns RD. Children’s Weight Gain and Cardiovascular Fitness Loss over the Summer. International Journal of Environmental Research and Public Health. 2018; 15(12):2770. https://doi.org/10.3390/ijerph15122770
Chicago/Turabian StyleBrusseau, Timothy A., and Ryan D. Burns. 2018. "Children’s Weight Gain and Cardiovascular Fitness Loss over the Summer" International Journal of Environmental Research and Public Health 15, no. 12: 2770. https://doi.org/10.3390/ijerph15122770
APA StyleBrusseau, T. A., & Burns, R. D. (2018). Children’s Weight Gain and Cardiovascular Fitness Loss over the Summer. International Journal of Environmental Research and Public Health, 15(12), 2770. https://doi.org/10.3390/ijerph15122770






