Frailty as the Future Core Business of Public Health: Report of the Activities of the A3 Action Group of the European Innovation Partnership on Active and Healthy Ageing (EIP on AHA)
Abstract
1. Introduction
- -
- Improving health and QoL of older adults;
- -
- Improving the efficiency and sustainability of health systems;
- -
- Strengthening the competitiveness of European industry by investing in innovative products and services in the field of health and ageing [9].
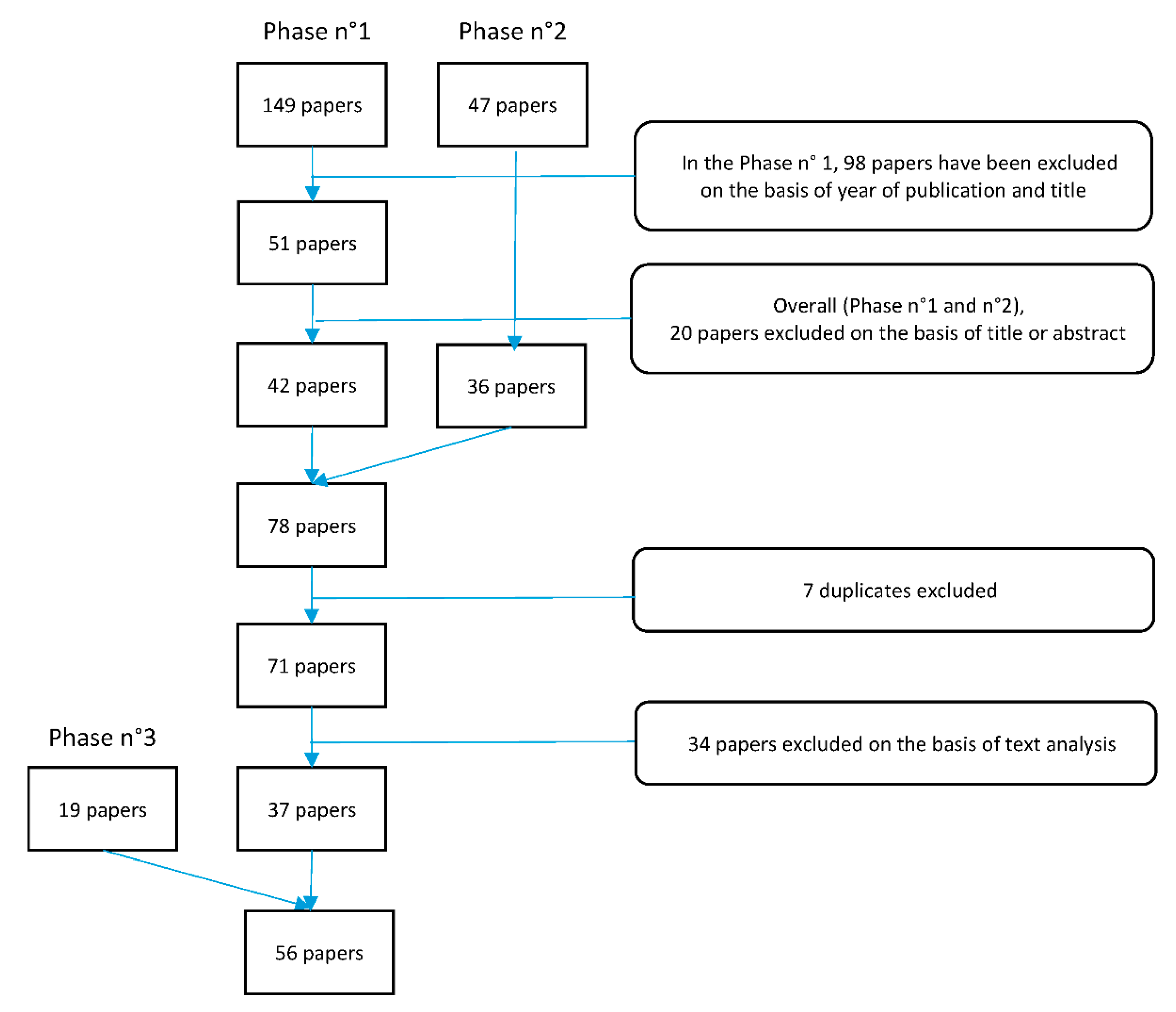
2. Methods
3. Results
- (1)
- Frailty screening tools (8/56)
- (2)
- Assessment of frailty and main associated factors at community level (30/56)
- (3)
- Intervention protocols (13/56)
- (4)
- Impact studies (5/56)
3.1. Tools to Screen Frailty in Community-Dwelling Older Adults
3.2. Assessment of Frailty and Associated Predictors at Community Level
3.2.1. The Prevalence and Predictors of Frailty
3.2.2. Frailty and Multimorbidity
3.2.3. The Caregiver Network
3.2.4. Frailty and Quality of Life
3.2.5. Frailty and Nutrition
3.2.6. Physical Ability: Mobility and Physical Activities
3.3. Interventions to Mitigate Frailty and Its Consequences
3.4. Impact Studies
- -
- Short physical performance Battery (SPPB) score improved to 1.58 to 1.36 (p < 0.001);
- -
- handgrip strength increased to 2.84 and 2.49 kilogram (p < 0.001);
- -
- functional reach rose to 4.3 and 4.52 centimetres (p < 0.001);
- -
- the number of prescriptions decreased to 1.39 and 1.09 (p < 0.001);
- -
- there was an improvement in neurocognitive battery scores [73].
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Illario, M.; De Luca, V.; Tramontano, G.; Menditto, E.; Iaccarino, G.; Bertorello, L.; Palummeri, E.; Romano, V.; Moda, G.; Maggio, M.; et al. The Italian reference sites of the European innovation partnership on active and healthy ageing: Progetto Mattone Internazionale as an enabling factor. Annali dell’Istituto Superiore di Sanità 2017, 53, 60–69. [Google Scholar] [CrossRef] [PubMed]
- International Longevity Centre. Active Ageing: A Policy Framework in Response to Longevity Revolution. Available online: http://ilcbrazil.org/portugues/wp-content/uploads/sites/4/2015/12/Active-Ageing-A-Policy-Framework-ILC-Brazil_web.pdf Accessed (accessed on 13 November 2018).
- World Health Organization. World Report about Ageing and Health. Available online: http://apps.who.int/iris/bitstream/handle/10665/186463/9789240694811_eng.pdf;jsessionid=B9A03C37671AFA933C77145A30215F30?sequence=1 (accessed on 13 November 2018).
- Fernández-Ballesteros. Active versus Healthy Aging: A Step Backwards? OAJ Gerontol. Geriatr. Med. 2017, 1, 555558. [Google Scholar]
- Domagała, A.; Arsenijevic, J.; Poscia, A. Good practices in health promotion for older people. In Health Promotion for Older People in Europe; Scholar Publishing House Ltd.: Warsaw, Poland, 2017; pp. 147–178. ISBN 978-83-7383-906-9. [Google Scholar]
- Eurostat. Statistics Explained. Healthy Life Years Statistics. Available online: http://ec.europa.eu/eurostat/statistics-explained/index.php?title=Healthy_life_years_statistics (accessed on 13 November 2018).
- Illario, M.; Vollenbroek-Hutten, M.; Molloy, D.W.; Menditto, E.; Iaccarino, G.; Eklund, P. Active and healthy ageing and independent living. J. Aging Res. 2015, 2015, 542183. [Google Scholar] [CrossRef] [PubMed]
- García-Esquinas, E.; Rodríguez-Artalejo, F. Environmental Pollutants, Limitations in Physical Functioning, and Frailty in Older Adults. Curr. Environ. Health Rep. 2017, 4, 12–20. [Google Scholar] [CrossRef]
- European Commission. Communication from the Commission to the European Parliament, the Council, the European Economic and Social Committee and the Committee of the Regions: Europe 2020 Flagship Initiative Innovation Union. 2011. Available online: https://ec.europa.eu/research/innovation-union/pdf/innovation-union-communication_en.pdf (accessed on 13 November 2018).
- European Innovation Partnership on Active and Healthy Ageing. State of play of Action Group A1. Prescription and Adherence to Medical Plans. Available online: https://ec.europa.eu/research/innovation-union/pdf/active-healthy-ageing/a1_achievements_2015.pdf (accessed on 13 November 2018).
- European Innovation Partnership on Active and Healthy Ageing. State of Play of Action Group A2. Personalised Health Management and Falls Prevention. Available online: file:///C:/Users/med03/Downloads/ag_a2_sop.pdf (accessed on 13 November 2018).
- Cano, A.; Dargent, G.; Carriazo, A.; López-Samaniego, L.; Apostolo, J.; Campos, E.; Holland, C.; Varela-Nieto, I.; Luz Sánchez-Sánchez, M.; Illario, M.; et al. Tackling frailty and functional decline: Background of the action group A3 of the European innovation partnership for active and healthy ageing. Maturitas 2018, 115, 69–73. [Google Scholar] [CrossRef] [PubMed]
- European Innovation Partnership on Active and Healthy Ageing. State of play of Action Group B3. Replicating and Tutoring Integrated Care for Chronic Diseases, including Remote Monitoring at Regional Level. Available online: https://ec.europa.eu/research/innovation-union/pdf/active-healthy-ageing/b3_achievements_2015.pdf (accessed on 13 November 2018).
- European Innovation Partnership on Active and Healthy Ageing. State of play of Action Group C2. Development of Interoperable and Independent Living Solutions. Available online: file:///C:/Users/med03/Downloads/ag_c2_sop.pdf (accessed on 13 November 2018).
- European Innovation Partnership on Active and Healthy Ageing. State of Play of Action Group D4. Innovation for Age-Friendly Buildings, Cities and Environments. Available online: https://ec.europa.eu/research/innovation-union/pdf/active-healthy-ageing/d4_achievements_2015.pdf (accessed on 13 November 2018).
- Illario, M.; Iaccarino, G.; Piazza, O.; Menditto, E.; Coscioni, E. Proceedings of the EIP on AHA: A3 Action Group on Frailty. Transl. Med. UniSa 2015, 13, 1–3. [Google Scholar] [PubMed]
- European Innovation Partnership on Active and Healthy Ageing. Building European Commitment to Prevent and Tackle Frailty. A Decalogue on Frailty Prevention. Available online: https://ec.europa.eu/research/innovation-union/pdf/active-healthy-ageing/a3_decalogue_2015.pdf (accessed on 13 November 2018).
- Bousquet, J.; Agache, I.; Aliberti, M.R.; Angles, R.; Annesi-Maesano, I.; Anto, J.M.; Arnavielhe, S.; Asayag, E.; Bacci, E.; Bedbrook, A. Transfer of innovation on allergic rhinitis and asthma multimorbidity in the elderly (MACVIA-ARIA)—EIP on AHA Twinning Reference Site (GARD research demonstration project). Allergy 2018, 73, 77–92. [Google Scholar] [CrossRef]
- Malva, J.O.; Amado, A.; Rodrigues, A.; Mota-Pinto, A.; Cardoso, A.F.; Teixeira, A.M.; Todo-Bom, A.; Devesa, A.; Ambrósio, A.F.; Cunha, A.L. The Quadruple Helix-Based Innovation Model of Reference Sites for Active and Healthy Ageing in Europe: The Ageing@Coimbra Case Study. Front. Med. 2018, 5, 132. [Google Scholar] [CrossRef]
- European Commission. European Innovation Partnership. Available online: https://ec.europa.eu/eip/ageing/about-the-partnership_en (accessed on 29 November 2018).
- Piotrowicz, J.; Soll, A.; Kielar, U.; Zwiefka, A.; Guligowska, A.; Piglowska, M.; Kostka, T.; Kurpas, D. ICT and environmental support for patients with frailty syndrome: CAREWELL project, FOCUS project and SUNFRAIL project. Med. Sci. Pulse 2017, 1, 37–43. [Google Scholar] [CrossRef]
- Sunfrail. Available online: http://www.sunfrail.eu/ (accessed on 19 November 2018).
- Onder, G.; Cesari, M.; Maggio, M.; Palmer, K. Defining a care pathway for patients with multimorbidity or frailty. Eur. J. Intern. Med. 2017, 38, 1–2. [Google Scholar] [CrossRef]
- Weathers, E.; O’Caoimh, R.; O’Sullivan, R.; Paúl, C.; Orfilia, F.; Clarnette, R.; Fitzgerald, C.; Svendrovski, A.; Cornally, N.; Leahy-Warren, P.; et al. The inter-rater reliability of the Risk Instrument for Screening in the Community. Br. J. Community Nurs. 2016, 21, 469–475. [Google Scholar] [CrossRef] [PubMed]
- O’Caoimh, R.; FitzGerald, C.; Cronin, U.; Svendrovski, A.; Gao, Y.; Healy, E.; O’Connell, E.; O’Keeffe, G.; O’Herlihy, E.; Weathers, E.; et al. Which part of a short, global risk assessment, the Risk Instrument for Screening in the Community, predicts adverse healthcare outcomes? J. Aging Res. 2015, 2015, 256414. [Google Scholar] [CrossRef] [PubMed]
- Capanna, A.; Scarcella, P.; Gilardi, F.; Mancinelli, S.; Palombi, L.; Marazzi, M.C.; Riccardi, F.; Liotta, G. Sensitivity and Specificity of a Short Questionnaire to Screen Frailty in the Community-Dwelling Older Population. Adv. Aging Res. 2018, 7, 52–63. [Google Scholar] [CrossRef]
- Gilardi, F.; Capanna, A.; Ferraro, M.; Scarcella, P.; Marazzi, M.C.; Palombi, L.; Liotta, G. Frailty screening and assessment tools: A review of characteristics and use in Public Health. Ann. Ig. 2018, 30, 128–139. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Laso, Á.; O’Caoimh, R.; Galluzzo, L.; Carcaillon-Bentana, L.; Beltzer, N.; Macijauskiene, J.; Albaina Bacaicoa, O.; Ciutan, M.; Hendry, A.; Lopez-Samaniego, L.; et al. Population screening, monitoring and surveillance for frailty: Three systematic reviews and a grey literature review. Annali dell’Istituto Superiore di Sanità 2018, 54, 253–262. [Google Scholar] [CrossRef] [PubMed]
- Apóstolo, J.; Cooke, R.; Bobrowicz-Campos, E.; Santana, S.; Marcucci, M.; Cano, A.; Vollenbroek-Hutten, M.; Germini, F.; Holland, C. Predicting risk and outcomes for frail older adults: An umbrella review of frailty screening tools. JBI Database Syst. Rev. Implement Rep. 2017, 15, 1154–1208. [Google Scholar] [CrossRef]
- Liotta, G.; O’Caoimh, R.; Gilardi, F.; Proietti, M.G.; Rocco, G.; Alvaro, R.; Scarcella, P.; Molloy, D.W.; Orlando, S.; Mancinelli, S.; et al. Assessment of frailty in community-dwelling older adults residents in the Lazio region (Italy): A model to plan regional community-based services. Arch. Gerontol. Geriatr. 2017, 68, 1–7. [Google Scholar] [CrossRef]
- Gilardi, F.; Scarcella, P.; Proietti, M.G.; Capobianco, G.; Rocco, G.; Capanna, A.; Mancinelli, S.; Marazzi, M.C.; Palombi, L.; Liotta, G. Frailty as a predictor of mortality and hospital services use in older adults: A cluster analysis in a cohort study. Eur. J. Public Health 2018, 28, 842–846. [Google Scholar] [CrossRef]
- Doménech-Abella, J.; Mundó, J.; Moneta, M.V.; Perales, J.; Ayuso-Mateos, J.L.; Miret, M.; Haro, J.M.; Olaya, B. The impact of socioeconomic status on the association between biomedical and psychosocial well-being and all-cause mortality in older Spanish adults. Soc. Psychiatry Psychiatr. Epidemiol. 2018, 53, 259–268. [Google Scholar] [CrossRef]
- Teixeira, L.; Azevedo, M.J.; Alves, S.; Pires, C.L.; Paúl, C. Perception of Risk of adverse outcomes of older people: Comparison between nursing homes, day centres and home care services. Qual. Ageing Older Adults 2017, 18, 212–220. [Google Scholar] [CrossRef]
- Olaya, B.; Moneta, M.V.; Caballero, F.F.; Tyrovolas, S.; Bayes, I.; Ayuso-Mateos, J.L.; Haro, J.M. Latent class analysis of multimorbidity patterns and associated outcomes in Spanish older adults: A prospective cohort study. BMC Geriatr. 2017, 17, 186. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, A.M.; Gregório, M.J.; Sousa, R.D.; Dias, S.S.; Santos, M.J.; Mendes, J.M.; Coelho, P.S.; Branco, J.C.; Canhão, H. Challenges of Ageing in Portugal: Data from the EpiDoC Cohort. Acta Med. Port. 2018, 31, 80–93. [Google Scholar] [CrossRef] [PubMed]
- Tomás, C.C.; Oliveira, E.; Sousa, D.; Uba-Chupel, M.; Furtado, G.; Rocha, C.; Teixeira, A.; Ferreira, P.; Alves, C.; Gisin, S.; et al. Proceedings of the 3rd IPLeiria’s International Health Congress: Leiria, Portugal. 6–7 May 2016. BMC Health Serv. Res. 2016, 16 (Suppl. 3), 200. [Google Scholar] [CrossRef] [PubMed]
- Garin, N.; Koyanagi, A.; Chatterji, S.; Tyrovolas, S.; Olaya, B.; Leonardi, M.; Lara, E.; Koskinen, S.; Tobiasz-Adamczyk, B.; Ayuso-Mateos, J.L.; et al. Global Multimorbidity Patterns: A Cross-Sectional, Population-Based, Multi-Country Study. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2015, 71, 205–214. [Google Scholar] [CrossRef] [PubMed]
- D’Avanzo, B.; Shaw, R.; Riva, S.; Apostolo, J.; Bobrowicz-Campos, E.; Kurpas, D.; Bujnowska-Fedak, M.; Holland, C. Stakeholders’ views and experiences of care and interventions for addressing frailty and pre-frailty: A meta-synthesis of qualitative evidence. PLoS ONE 2017, 12, e0180127. [Google Scholar] [CrossRef] [PubMed]
- Orfila, F.; Coma-Solé, M.; Cabanas, M.; Cegri-Lombardo, F.; Moleras-Serra, A.; Pujol-Ribera, E. Family caregiver mistreatment of the elderly: Prevalence of risk and associated factors. BMC Public Health 2018, 18, 167. [Google Scholar] [CrossRef]
- O’Caoimh, R.; Cornally, N.; Svendrovski, A.; Weathers, E.; FitzGerald, C.; Healy, E.; O’Connell, E.; O’Keeffe, G.; O’Herlihy, E.; Gao, Y.; et al. Measuring the Effect of Carers on Patients’ Risk of Adverse Healthcare Outcomes Using the Caregiver Network Score. J. Frailty Aging 2016, 5, 104–110. [Google Scholar] [CrossRef]
- Gwyther, H.; Shaw, R.; Jaime Dauden, E.A.; D’Avanzo, B.; Kurpas, D.; Bujnowska-Fedak, M.; Kujawa, T.; Marcucci, M.; Cano, A.; Holland, C. Understanding frailty: A qualitative study of European healthcare policy-makers’ approaches to frailty screening and management. BMJ Open 2018, 8, e018653corr1. [Google Scholar] [CrossRef]
- Amanzio, M.; Palermo, S.; Zucca, M.; Rosato, R.; Rubino, E.; Leotta, D.; Bartoli, M.; Rainero, I. Neuropsychological Correlates of Pre-Frailty in Neurocognitive Disorders: A Possible Role for Metacognitive Dysfunction and Mood Changes. Front. Med. 2017, 4, 199. [Google Scholar] [CrossRef]
- Raggi, A.; Corso, B.; Minicuci, N.; Quintas, R.; Sattin, D.; De Torres, L.; Chatterji, S.; Frisoni, G.B.; Haro, J.M.; Koskinen, S.; et al. Determinants of Quality of Life in Ageing Populations: Results from a Cross-Sectional Study in Finland, Poland and Spain. PLoS ONE 2016, 11, e0159293. [Google Scholar] [CrossRef]
- Lara, E.; Koyanagi, A.; Caballero, F.; Domènech-Abella, J.; Miret, M.; Olaya, B.; Rico-Uribe, L.; Ayuso-Mateos, J.L.; Haro, J.M. Cognitive reserve is associated with quality of life: A population-based study. Exp. Gerontol. 2017, 87, 67–73. [Google Scholar] [CrossRef] [PubMed]
- Gwyther, H.; Bobrowicz-Campos, E.; Apóstolo, L.A.J.; Marcucci, M.; Cano, A.; Holland, C. A realist review to understand the efficacy and outcomes of interventions designed to minimise, reverse or prevent the progression of frailty. Health Psychol. Rev. 2018, 12, 382–404. [Google Scholar] [CrossRef] [PubMed]
- De Sousa, R.D.; Rodrigues, A.M.; Gregório, M.J.; Branco, J.D.C.; Gouveia, M.J.; Canhão, H.; Dias, S.S. Anxiety and Depression in the Portuguese Older Adults: Prevalence and Associated Factors. Front. Med. 2017, 4, 196. [Google Scholar] [CrossRef] [PubMed]
- Tobiasz-Adamczyk, B.; Galas, A.; Zawisza, K.; Chatterji, S.; Haro, J.M.; Ayuso-Mateos, J.L.; Koskinen, S.; Leonardi, M. Gender-related differences in the multi-pathway effect of social determinants on quality of life in older age-the COURAGE in Europe project. Qual. Life Res. 2017, 26, 1865–1878. [Google Scholar] [CrossRef] [PubMed]
- Rapacciuolo, A.; Perrone Filardi, P.; Cuomo, R.; Mauriello, V.; Quarto, M.; Kisslinger, A.; Savarese, G.; Illario, M.; Tramontano, D. The Impact of Social and Cultural Engagement and Dieting on Well-Being and Resilience in a Group of Residents in the Metropolitan Area of Naples. J. Aging Res. 2016, 2016, 4768420. [Google Scholar] [CrossRef] [PubMed]
- Rico-Uribe, L.A.; Caballero, F.F.; Olaya, B.; Tobiasz-Adamczyk, B.; Koskinen, S.; Leonardi, M.; Haro, J.M.; Chatterji, S.; Ayuso-Mateos, J.L.; Miret, M. Loneliness, Social Networks, and Health: A Cross-Sectional Study in Three Countries. PLoS ONE 2016, 11, e0145264. [Google Scholar] [CrossRef] [PubMed]
- Domènech-Abella, J.; Lara, E.; Rubio-Valera, M.; Olaya, B.; Moneta, M.V.; Rico-Uribe, L.A.; Ayuso-Mateos, J.L.; Mundó, J.; Haro, J.M. Loneliness and depression in the elderly: The role of social network. Soc. Psychiatry Psychiatr. Epidemiol. 2017, 52, 381–390. [Google Scholar] [CrossRef]
- Santos, D.; Abad, F.J.; Miret, M.; Chatterji, S.; Olaya, B.; Zawisza, K.; Koskinen, S.; Leonardi, M.; Haro, J.M.; Ayuso-Mateos, J.L.; et al. Measurement invariance of the WHOQOL-AGE questionnaire across three European countries. Qual. Life Res. 2018, 27, 1015–1025. [Google Scholar] [CrossRef]
- Fernandes, S.G.; Rodrigues, A.M.; Nunes, C.; Santos, O.; Gregório, M.J.; de Sousa, R.D.; Dias, S.; Canhão, H. Food Insecurity in Older Adults: Results from the Epidemiology of Chronic Diseases Cohort Study 3. Front. Med. 2018, 5, 203. [Google Scholar] [CrossRef]
- Coto Montes, A.; Boga, J.A.; Bermejo Millo, C.; Rubio González, A.; Potes Ochoa, Y.; Vega Naredo, I.; Martínez Reig, M.; Romero Rizos, L.; Sánchez Jurado, P.M.; Solano, J.J.; et al. Potential early biomarkers of sarcopenia among independent older adults. Maturitas 2017, 104, 117–122. [Google Scholar] [CrossRef]
- Potes, Y.; de Luxán-Delgado, B.; Rodriguez-González, S.; Guimarães, M.R.M.; Solano, J.J.; Fernández-Fernández, M.; Bermúdez, M.; Boga, J.A.; Vega-Naredo, I.; Coto-Montes, A. Overweight in elderly people induces impaired autophagy in skeletal muscle. Free Radic. Biol. Med. 2017, 110, 31–41. [Google Scholar] [CrossRef] [PubMed]
- Coto-Montes, A.; Boga, J.A.; Tan, D.X.; Reiter, R.J. Melatonin as a Potential Agent in the Treatment of Sarcopenia. Int. J. Mol. Sci. 2016, 17, 1771. [Google Scholar] [CrossRef] [PubMed]
- Olaya, B.; Moneta, M.V.; Doménech-Abella, J.; Miret, M.; Bayes, I.; Ayuso-Mateos, J.L.; Haro, J.M. Mobility Difficulties, Physical Activity, and All-cause Mortality Risk in a Nationally representative Sample of Older Adults. J. Gerontol. A Biol. Sci. Med. Sci. 2018, 73, 1272–1279. [Google Scholar] [CrossRef] [PubMed]
- Tomás, M.T.; Galán-Mercant, A.; Carnero, E.A.; Fernandes, B. Functional Capacity and Levels of Physical Activity in Aging: A 3-Year Follow-up. Front. Med. 2018, 4, 244. [Google Scholar] [CrossRef] [PubMed]
- Loyen, A.; Clarke-Cornwell, A.M.; Anderssen, S.A.; Hagströmer, M.; Sardinha, L.B.; Sundquist, K.; Ekelund, U.; Steene-Johannessen, J.; Baptista, F.; Hansen, B.H.; et al. Sedentary Time and Physical Activity Surveillance Through Accelerometer Pooling in Four European Countries. Sports Med. 2017, 47, 1421–1435. [Google Scholar] [CrossRef] [PubMed]
- Santos, D.A.; Júdice, P.B.; Magalhães, J.P.; Correia, I.R.; Silva, A.M.; Baptista, F.; Sardinha, L.B. Patterns of accelerometer-derived sedentary time across the lifespan. J. Sports Sci. 2018, 36, 2809–2817. [Google Scholar] [CrossRef]
- Pereira, C.; Fernandes, J.; Raimundo, A.; Biehl-Printes, C.; Marmeleira, J.; Tomas-Carus, P. Increased Physical Activity and Fitness above the 50(th) Percentile Avoid the Threat of Older Adults Becoming Institutionalized: A Cross-sectional Pilot Study. Rejuvenation Res. 2016, 19, 13–20. [Google Scholar] [CrossRef]
- Cano, A.; Kurpas, D.; Bujnowska-Fedak, M.M.; Santana, S.; Holland, C.; Marcucci, M.; Gonzalez-Segura, A.; Vollenbroek-Hutten, M.; D’Avanzo, B.; Nobili, A.; et al. FOCUS: Frailty Management Optimisation through EIPAHA Commitments and Utilisation of Stakeholders’ Input—An innovative European Project in elderly care. Fam. Med. Prim. Care Rev. 2016, 18, 373–376. [Google Scholar] [CrossRef]
- Apóstolo, J.; Cooke, R.; Bobrowicz-Campos, E.; Santana, S.; Marcucci, M.; Cano, A.; Vollenbroek-Hutten, M.; Germini, F.; D’Avanzo, B.; Gwyther, H.; et al. Corrigendum: Effectiveness of interventions to prevent pre-frailty and frailty progression in older adults: A systematic review. JBI Database Syst. Rev. Implement Rep. 2018, 16, 1282–1283. [Google Scholar] [CrossRef]
- FrailSafe. Available online: https://frailsafe-project.eu/ (accessed on 14 November 2018).
- PROMISS. Nutrition for Healthy Ageing. Available online: www.PROMISS-VU.eu (accessed on 14 November 2018).
- Wijnhoven, H.A.H.; Elstgeest, L.E.M.; de Vet, H.C.W.; Nicolaou, M.; Snijder, M.B.; Visser, M. Development and validation of a short food questionnaire to screen for low protein intake in community-dwelling older adults: The Protein Screener 55+ (Pro55+). PLoS ONE 2018, 13, e0196406. [Google Scholar] [CrossRef]
- Ramalho, F.; Carnide, F.; Santos-Rocha, R.; André, H.I.; Moniz-Pereira, V.; Machado, M.L.; Veloso, A.P. Community-Based Exercise Intervention for Gait and Functional Fitness Improvement in an Older Population: Study Protocol. J Aging Phys. Act. 2017, 25, 84–93. [Google Scholar] [CrossRef] [PubMed]
- Carnide, F.; Baptista, F.; Moura, A.; Sofia, B.D.; Moura, A.; Langberg, H.; Mosbech Jensen, A.; del Pozo, F. Frailty, Falls, and Functional loss Education: The 3Fights@Edu MOOC perspective. In Proceedings of the 2016 1st International Conference on Technology and Innovation in Sports, Health and Wellbeing (TISHW), Vila Real, Portugal, 1–3 December 2016; Available online: https://ieeexplore.ieee.org/stamp/stamp.jsp?tp=&arnumber=7847784 (accessed on 14 November 2018).
- Dias, S.B.; Konstantinidis, E.; Diniz, J.A.; Bamidis, P.; Charisis, V.; Hadjidimitriou, S.; Stadtschnitzer, M.; Fagerberg, P.; Ioakeimidis, I.; Dimitropoulos, K.; et al. Serious Games as a means for holistically supporting Parkinson’s Disease patients: The i-PROGNOSIS Personalized Game Suite framework. In Proceedings of the 9th International Conference on Virtual Worlds and Games for Serious Applications (VS-Games), Athens, Greece, 6–8 September 2017; pp. 237–244. [Google Scholar] [CrossRef]
- Illario, M.; Maione, A.S.; Rusciano, M.R.; Goossens, E.; Rauter, A.; Braz, N.; Jager-Wittenaar, H.; Di Somma, C.; Crola, C.; Soprano, M.; et al. NutriLive: An Integrated Nutritional Approach as a Sustainable Tool to Prevent Malnutrition in Older People and Promote Active and Healthy Ageing—The EIP-AHA Nutrition Action Group. Adv. Public Health 2016, 2016, 5678782. [Google Scholar] [CrossRef]
- Arcopinto, M.; Cataldi, M.; De Luca, V.; Orlando, V.; Simeone, G.; D’Assante, R.; Postiglione, A.; Guida, A.; Trama, U.; Illario, M.; et al. Implementing an ICT-Based Polypharmacy Management Program in Italy. Transl. Med. UniSa 2017, 16, 24–29. [Google Scholar] [PubMed]
- Vuolo, L.; Barrea, L.; Savanelli, M.C.; Savastano, S.; Rubino, M.; Scarano, E.; Soprano, M.; Illario, M.; Colao, A.; Di Somma, C. Nutrition and Osteoporosis: Preliminary data of Campania Region of European PERsonalised ICT Supported Service for Independent Living and Active Ageing. Transl. Med. UniSa 2016, 13, 13–18. [Google Scholar] [PubMed]
- Barrea, L.; Muscogiuri, G.; Di Somma, C.; Tramontano, G.; De Luca, V.; Illario, M.; Colao, A.; Savastano, S. Association between Mediterranean diet and hand grip strength in older adult women. Clin. Nutr. 2018. [Google Scholar] [CrossRef]
- Health Directorate, Lazio Region; Department of Epidemiology, Lazio Regional Health Service, ASL Rome 1. The Regional Plan for Prevention of Heat Wave Related Effects. Available online: https://www.salutelazio.it/notizie-dalla-regione-lazio/-/asset_publisher/3IMUBGWmAz07/content/ondate-calore?inheritRedirect=false&redirect=https%3A%2F%2Fwww.salutelazio.it%2Fnotizie-dalla-regione-lazio%3Fp_p_id%3D101_INSTANCE_3IMUBGWmAz07%26p_p_lifecycle%3D0%26p_p_state%3Dnormal%26p_p_mode%3Dview%26p_p_col_id%3Dcolumn-1%26p_p_col_pos%3D1%26p_p_col_count%3D2 (accessed on 19 November 2018).
- Romera-Liebana, L.; Orfila, F.; Segura, J.M.; Real, J.; Fabra, M.L.; Möller, M.; Lancho, S.; Ramirez, A.; Marti, N.; Cullell, M.; et al. Effects of a Primary Care-Based Multifactorial Intervention on Physical and Cognitive Function in Frail, Elderly Individuals: A Randomized Controlled Trial. J. Gerontol. A Biol. Sci. Med. Sci. 2018, 73, 1668–1674. [Google Scholar] [CrossRef]
- Behm, L.; Eklund, K.; Wilhelmson, K.; Zidén, L.; Gustafsson, S.; Falk, K.; Dahlin-Ivanoff, S. Health Promotion Can Postpone Frailty: Results from the RCT Elderly Persons in the Risk Zone. Public Health Nurs. 2016, 33, 303–315. [Google Scholar] [CrossRef]
- Liotta, G.; Inzerilli, M.C.; Palombi, L.; Madaro, O.; Orlando, S.; Scarcella, P.; Betti, D.; Marazzi, M.C. Social Interventions to Prevent Heat-Related Mortality in the Older Adult in Rome, Italy: A Quasi-Experimental Study. Int. J. Environ. Res. Public Health 2018, 15, E715. [Google Scholar] [CrossRef]
- Liotta, G.; Inzerilli, M.C.; Palombi, L.; Bianchini, A.; Di Gennaro, L.; Madaro, O.; Marazzi, M.C. Impact of social care on Hospital Admissions in a sample of community-dwelling older adults: Results of a quasi-experimental study. Ann. Ig. 2018, 30, 378–386. [Google Scholar] [CrossRef]
- O’Caoimh, R.; Gao, Y.; Svendrovski, A.; Healy, E.; O’Connell, E.; O’Keeffe, G.; Cronin, U.; O’Herlihy, E.; Cornally, N.; Molloy, D.W. Screening for markers of frailty and perceived risk of adverse outcomes using the Risk Instrument for Screening in the Community (RISC). BMC Geriatr. 2014, 14, 104. [Google Scholar] [CrossRef]
- O’Caoimh, R.; Cornally, N.; Weathers, E.; O’Sullivan, R.; Fitzgerald, C.; Orfila, F.; Clarnette, R.; Paúl, C.; Molloy, D.W. Risk prediction in the community: A systematic review of case-finding instruments that predict adverse healthcare outcomes in community-dwelling older adults. Maturitas 2015, 82, 3–21. [Google Scholar] [CrossRef] [PubMed]
- Cesari, M.; Prince, M.; Thiyagarajan, J.A.; De Carvalho, I.A.; Bernabei, R.; Chan, P.; Gutierrez-Robledo, L.M.; Michel, J.P.; Morley, J.E.; Ong, P.; et al. Frailty: An emerging public health priority. J. Am. Med. Dir. Assoc. 2016, 17, 188–192. [Google Scholar] [CrossRef] [PubMed]
- Puts, M.T.E.; Toubasi, S.; Andrew, M.K.; Ashe, M.C.; Ploeg, J.; Atkinson, E.; Ayala, A.P.; Roy, A.; Monforte, M.R.; Bergman, H.; et al. Interventions to prevent or reduce the level of frailty in community-dwelling older adults: A scoping review of the literature and international policies. Age Ageing 2017, 46, 383–392. [Google Scholar] [CrossRef] [PubMed]
- Feng, Z.; Lugtenberg, M.; Franse, C.; Fang, X.; Hu, S.; Jin, C.; Raat, H. Risk factors and protective factors associated with incident or increase of frailty among community-dwelling older adults: A systematic review of longitudinal studies. PLoS ONE 2017, 12, e0178383. [Google Scholar] [CrossRef] [PubMed]
- O’Caoimh, R.; Galluzzo, L.; Rodriguez-Laso, A.; Van der Heyden, J.; Ranhoff, A.H.; Carcaillon-Bentata, L.; Beltzer, N.; Kennelly, S.; Liew, A. Transitions and trajectories in frailty states over time: A systematic review of the European Joint Action ADVANTAGE. Annali dell’Istituto Superiore di Sanità 2018, 54, 246–252. [Google Scholar] [PubMed]
- Rodríguez-Artalejo, F.; Rodríguez-Mañas, L. The frailty syndrome in the public health agenda. J. Epidemiol. Community Health 2014, 68, 703–704. [Google Scholar] [CrossRef] [PubMed]
- O’Caoimh, R.; Galluzzo, L.; Rodríguez-Laso, Á.; Van der Heyden, J.; Ranhoff, A.H.; Lamprini-Koula, M.; Ciutan, M.; López-Samaniego, L.; Carcaillon-Bentata, L.; Kennelly, S.; et al. Prevalence of frailty at population level in European ADVANTAGE Joint Action Member States: A systematic review and meta-analysis. Annali dell’Istituto Superiore di Sanità 2018, 54, 226–239. [Google Scholar]

| Article (Ref. Number) | Tool Description | Way of Administration | Developer | The Tool Has Been Tested (a), Implemented (b), or Validated (c) | Country Where It Has Been Tested/Validated |
|---|---|---|---|---|---|
| SUNFRAIL Tool [22] | 9 items exploring socioeconomic domain, Psycho-Physical status, functional capacity | Social and/or Health care personnel | SUNFRAIL EU project | (a) | Italy |
| The Risk Instrument for Screening in the Community (RISC) [24] | 32 items exploring domains of physical condition, mental health, functional status, community support, housing, social relationships | Public Health nurses | COLLAGE * | (a), (b), (c) | Ireland, Spain, Portugal, Australia |
| Short Functional Geriatric Evaluation (SFGE) [26] | 13-items exploring socioeconomic domain, Psycho-Physical status, functional capacity | Personnel with secondary school diploma | University of Rome “Tor Vergata” | (a), (b), (c) (for predicting the Use of Hospital Services) | Italy |
| First Authors and Ref. Number | Study Design | Sample Size | Sample Age | Instrument(s) | Main Outcomes | Country | Follow Up |
|---|---|---|---|---|---|---|---|
| The Prevalence and Predictors of Frailty | |||||||
| Liotta [28] | Cross sectional | 1331, females 54.2% | Over 64 years | Functional Geriatric Evaluation | A total of 21.5% of frail individuals, 31.8% among the over-74 years; factors associated to Frailty: more than one neurologic disease, disability, low education, living alone, being older than 84 years. | Italy | NA |
| Gilardi [29] | Observational longitudinal cohort study | 1280, females 54.4% | Over 64 years | Functional Geriatric Evaluation | Mortality rate: 1.8%, 10.1% and 19.1% among robust, frail and very frail respectively; UHS rate was 957.4 for frail/pre-frail and 594.5 for robust. Factors associated to highest UHS rate: disability, lack of social resources, psychological/psychiatric impairment, physical impairment, lack of home care. | Italy | 1 year |
| Domenech-Abella [30] | Longitudinal survey | 2783, females 54.6% | Over 50 years | Set of instruments | Psychosocial and biomedical well-being as well as Socioeconomic Status (SES) had a role in the prediction of mortality: adults who had lower levels of psychosocial SA were more prone to die, independently of SES; significant interaction was observed between biomedical SA and SES (p = 0.046). | Spain | 3 years |
| Teixeira [31] | Cross sectional | 224, females 69.6% | Over 64 years | Risk Instrument for Screening in the Community | The 64.4% of the clients of home care services and day center services was at risk of hospitalization; over the 50% of the clients of home care services and day center services was at risk of death; the 73.3% of the clients of day centers was at risk of institutionalization. | Portugal | NA |
| Frailty and Multimorbidity (see also [28,29,31]) | |||||||
| Olaya [32] | Longitudinal survey | 3541, females 54.5% | Over 50 years | Set of instruments | Patients with showed an increased percentage of hospital admissions 16.8% vs. 30.1% or 44.5), and medical visits in the last 12 months (3.04 vs. 5.55 or 7.02). | Spain | 3 years |
| Rodrigues [33] | Cross sectional | 2393, females 55.8% | Over 65 years | Set of instruments | Multimorbidity prevalence: 78.3% of the adults aged 65–69 years and 83.4% among the over-80 years. 25.8% of the sample was hospitalized in the last year. | Portugal | NA |
| Teixeira [34] | Cross sectional | 4470, females 58.7% | Over 64 years | Risk Instrument for Screening in the Community | The perceived risk of death increased with the increase of severity of medical concerns (OR: 1.6 for mild severity; 9.7 for moderate severity; 48.6 for severe) and the decrease ability of caregiver to manage (OR: 4.5 for “can manage”; 65.3 for “cannot manage”). | Portugal | NA |
| Garin [35] | Cross-sectional | 41,909, females 52.3% | Over 50 years | Questionnaire to gather information on health and well-being | Multimorbidity prevalence increases with age. The factors that show higher odds for multimorbidity are: higher age, female, lower education, separated/divorced/widowed and rural inhabitance. Multimorbidity patterns identified across countries: Cardio-respiratory, metabolic, mental-articular and respiratory pattern. | Finland, Poland, Spain, China, Ghana, India, Russia, Mexico, South Africa | NA |
| The Caregiver Network (see also [34]) | |||||||
| D’Avanzo [36] | Meta-synthesis of qualitative evidence | 45 studies | Older adults, caregivers | A bottom-up approach involving formal and informal caregivers is needed to approach frailty as a malleable and preventable condition. | Western countries | NA | |
| Orfila [37] | Cross sectional | 829, females 82.8% | Caregivers | Set of instruments | Prevalence of abuse risk by the caregiver 33.4%; factors associated: caregiver burden (OR = 2.75; 95% CI: 1.74–4.33), caregiver anxiety (OR = 2.06; 95% CI: 1.40–3.02), caregiver perception of aggressive behavior in the care recipient (OR = 7.24; 95% CI: 4.99–10.51), and a bad previous relationship (OR = 4.66; 95% CI: 1.25–17.4). | Spain | NA |
| O’Caoimh [38] | Observational prospective cohort study | 803, females 64% | Over 65 years | Risk Instrument for Screening in the Community | Risk of institutionalization is associated to the caregivers’ difficulty in managing medical issues (OR = 3.8; 2.22–6.86); the caregivers’ difficulties are not associated with higher risk of death/hospitalization. | Ireland | 1 year |
| Gwyther [39] | Thematic analysis of semi structured qualitative interviews | 7 | Health care policy makers | Ad Hoc | ‘Knowledge gap’, around frailty and awareness of the malleability of frailty. Frailty should be recognized as a clinical syndrome and managed by integrating social and health care. Need for a culture shift to overcome the silos approach in providing care. | UK, Italy, Spain, Poland, representatives of EU | NA |
| Frailty and Quality of Life (QoL) | |||||||
| Amanzio [40] | Cross sectional | 60, females 63.3% | Over 50 years | Set of instruments | Frailty is associated to action monitoring and monetary gain (cognitive domain), depression and disinhibition (behavioral domain). | Italy | NA |
| Raggi [41] | Cross sectional | 5639, females 51.2% | Over 18 years | WHOQOL-AGE | The model explained 45% of the Quality of Life variation: The biggest variation was related to social and demographic variables (22.5%), followed by chronic condition (4.6%). | Finland, Poland and Spain | NA |
| Lara [42] | Cross sectional | 1973, females 56% | Over 50 years | Set of instruments | Cognitive Reserve was associated with higher QoL and this association was mediated by disability, which explained about half of the association, and depression and cognition that explained 6–10% of this association. | Spain | NA |
| Gwyther [43] | Review | Healthcare interventions were successful when they were (1) sufficiently different from usual care; (2) based on health psychology; (3) offering choice over intervention elements; (4) organized in group settings; (5) multi-component (exercise, cognitive, nutrition, social). | NA | NA | |||
| de Sousa [44] | Cross sectional | 1680, females 54% | Over 64 years | Set of instruments | The estimated prevalence of anxiety was 9.6% and depression is 11.8%. Anxiety and depression were associated to higher levels of physical disability (OR = 3.10; 96% CI: 2.12–4.52; OR = 3.08, 95% CI: 2.29–4.14) and lower levels of quality of life (OR = 0.03, 95% CI: 0.01–0.09; OR = 0.03, 95% CI: 0.01–0.06), respectively. | Portugal | NA |
| Tobiasz-Adamczyk [45] | Cross sectional | 5099, females 58.6% | Over 50 years | WHOQOL-AGE | Males benefited more (in QoL) from social networks and social support, and women from social participation. Gender-related differences (in QoL) were associated with social networks in the group of 80+, for social support in the 50–64 and 65–79 years, and for social participation in the 65–79 years. | Finland, Poland and Spain | NA |
| Raparacciuolo [46] | Cross sectional | 571, females 50% | Over 60 years | Set of instruments | Better Resilience and Psychological Well-Being are associated to social participation to cultural activities. Participating subjects are more likely to adhere to diet/nutritional regimen. | Italy | NA |
| Rico-Uribe [47] | Cross sectional | 10,800, females 57.4% | Over 18 years | UCLA Loneliness Scale | Loneliness increases in over-79 population; higher age, the presence of depression and a higher score on loneliness were associated with a worse health status. | Finland, Poland and Spain | NA |
| Domenech-Abella [48] | Cross sectional | 3535, females 45.9% | Over 50 years | Set of instruments | Feelings of loneliness or depression were reported in the 13% and 12.1% of the sample, respectively. They were associated with the size and the quality of the network as well as with the, frequency of contact. Small social network was observed among the adults with depression and feelings of loneliness. | Spain | NA |
| Santos [49] | Cross sectional | 9987 | Over 18 years | WHOQOL-AGE | Respondents from Finland, Poland, and Spain attribute the same meaning to the latent construct studied, showing the reliability of the used tool. | Finland, Poland and Spain | NA |
| Fernandes [50] | Cross sectional | 1885, females 55.5% | Over 64 years | Set of instruments | A total of 23% of older adult reported to be food insecure; factors associated with food insecurity were gender (to be female) older age, financial difficulties lower education, living in the Azores and Madeira, stopping medication and medical visits, higher multimorbidity. | Portugal | 3 years |
| Physical Ability: Mobility and Physical Activities | |||||||
| Coto-Montes [51] | Cross sectional | 200, females 58% | Over 69 years | Set of instruments | Lipid peroxidation were associated with sarcopenia in independent older adults. The prevalence of sarcopenia was 35.3% in women and 13.1% in men. It was associated with older age, functional impairment, risk of malnutrition and use of digestive system drugs. Sarcopenia was also associated with pre-frailty and depressed mood. | Spain | NA |
| Potes [52] | Observational longitudinal cohort study | 39, no data about gender | Over 70 years | Set of instruments | Overweight induces a progressive protein breakdown reflected as a progressive withdrawal of anabolism against the promoted catabolic state leading to muscle wasting. | Spain | NA |
| Coto-Montes [53] | Review | Melatonin may be beneficial in attenuating, reducing or preventing each of the symptoms that characterize sarcopenia. | NA | NA | |||
| Olaya [54] | Longitudinal study | 2074, females 54.4% | Over 60 years | Set of instruments | High levels of physical activity were associated with a 51% lower risk of dying, compared with moderate physical activity. Mortality dropped by 2% for each unit increase in mobility functioning | Spain | 3 years |
| Tomàs [55] | Longitudinal study | 43, females 72.1% | Over 60 years | Battery of tests | The 6-MWT is a predictor of other functional capacities; type II diabetes influences the 6-MWT. | Portugal | 3 years |
| Loyen [56] | Cross sectional | 9509, females 55.5% | Over 20 years | Accelerometer data and socio-demographic data | 23% experienced more than 10 h of sedentary time/day, and 72% did not meet the physical activity recommendations. Factors associated were older age and higher weight. | England, Portugal, Norway, Sweden | NA |
| Santos [57] | Cross sectional | 4575, females 58.6% | Accelerometer data and socio-demographic data | Sedentary time is more than 60% of older adults’ wear time. | Portugal | NA | |
| Pereira [58] | Cross-sectional | 381 | Over 75 years | Set of instruments | Institutionalization increased by 1.6% for each additional year of age. Each additional 100 MET-min/week expended on physical active decrease by 2%; Each additional meter walked in the aerobic endure test decrease by 0.9%; Each fewer unit in BMI by 24.8%. | Portugal | NA |
| Article (Ref. Number) | Name of the Intervention/Project | Aims | Target Groups | Tools/Assessment | Type of Intervention |
|---|---|---|---|---|---|
| Cano [59] | FOCUS | Contribute to the reduction of burden created by frailty by reviewing innovative practices. |
|
|
|
| www.frailsafe-project.eu. [61] | FrailSafe | Quantify frailty and eventually prevent it by analysing physiological, cognitive, behavioural and social parameters in real-time. | Older person | NA | NA |
| Wijnhoven [63] | Prevention of Malnutrition In Senior Subject (PROMISS) | prevent protein malnutrition in community dwelling older adults in Europe. | Community-dwelling adults aged 55 years and older. | Protein screener questionnaire: it consists of questions on weight and height, and the consumption several foods selected because of their impact on protein malnutrition. | Data from 1348 older men and women (LASA study) were used to develop the questionnaire and data from 563 older man and women (HELIUS study) were used for external validation |
| Ramalho [64] | Community-based exercise intervention for gait and functional fitness improvement in an older population. | Evaluate at 0, 12, 24, 36 weeks if a periodic community program will have significantly results in the improvement of gait and functional fitness parameters | A total of 191 people. Inclusion criteria: ≥65 years old people; community dwelling living; understand the Portuguese language. |
| The intervention: posture control, balance (static and dynamic), strength and agility of lower limbs and aerobic capacity for 36 weeks, twice a week, for 50 minutes each session. The control group will be composed by older people that will receive standard care. |
| Carnide [65] | 3Fights@Edu | Promote functional capacity and independent living by empowering elderly people and their families to understand the aging process | Older adults and their families. | Massive Open Online Courses (MOOCs) providing information on ageing changes to help older adults to take decisions about Risk and actions | Three hours course (3 sessions of 1 hour) run over one week, available three times per year Provision of online materials and discussion forums |
| Dias [66] | H2020 i-PROGNOSIS project | Mitigate frailty by acting on Parkinson’s Disease (PD) symptoms in a personalized and gamified environment. | Patients with Parkinson’s Disease. | Targeting intelligent intervention in PD area, the Personalised Game Suite (PGS) integrates different serious games in a unified platform, namely:
| Intervention platform with the integration of Serious Games to assist physical exercise, handwriting, diet improvement, and better control of emotions of PD patients. |
| Illario [67] | NutriLive | Promote a nutritional approach for prevention of functional decline and frailty across the whole European continent. | Inclusion criteria: ≥65 years citizens
|
| An ICT platform will be set up and promoted during popular events, such as food blogger competitions on specific needs, |
| Arcopinto [68] | ICT-based polypharmacy management program | Give to each patient a personalized therapy that balances benefits and harms. | Older adults | Comprehensive Geriatric Assessment plus Computerized prescription support system | NA |
| Vuolo e Barrea [69,70] | PERSSILAA (PERsonalised ICT Supported Services for Independent Living and Active Ageing) | Develope remote service modules for:
| A total of 350 over >65 years’ citizens Exclusion criteria: evident frailty, dependency in ADL, moderate to advanced dementia. |
| Health promotion and Education in community dwelling older adults |
| Health Directorate, Lazio Region [71] | The heat prevention plan of Lazio Region | Mitigate mortality during heat waves in frail elderly population. | The ≥65 years community dwellings with medium-high or high susceptibility to heat waves. | Susceptibility score associated to the risk of dying during heat waves, based on administrative healthcare databases or GPs clinical evaluation. | GP’s active surveillance (phone calls, home visits, other home-based treatment) during heat waves; information to patients and families during summer. |
| Article (Ref. Number) | Study Design | Sample Size | Instrumental | Outcomes | Follow Up | Measure of Impact | State |
|---|---|---|---|---|---|---|---|
| Romera-Liebana [72] | RCT | A total of 347 participants Aged over 65 |
|
| At 3 and 18 months | Results at 3 and 18 months respectively:
| Spain |
| Behm et al. [73] | RCT | A total of 459 persons aged over 80. |
|
| 2 years | Postponing the progression of frailty measured as tiredness in daily activities up to 1 year. | |
| Liotta [74] | Retrospective cohort study | Aged > 74 years old. A total of 6481 cases, 5724 controls | Participants to Long Live the Elderly (LLE) program | Mortality | June to September 2015 | Reduction of heat-related mortality of about 13% during summer 2015 | Italy |
| Liotta [75] | CT with historical controls | Aged ≥ 75 years old. 207 LLE program A total of 308 controls | Short Functional Geriatric Evaluation (SFGE) | Hospitalisation Mortality | Six months | Percentage of hospitalisation is 9.1% and 8.3% in the controls and in the cases respectively. LLE program reduce of about 10% the acute hospital admission rate. | Italy |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liotta, G.; Ussai, S.; Illario, M.; O’Caoimh, R.; Cano, A.; Holland, C.; Roller-Winsberger, R.; Capanna, A.; Grecuccio, C.; Ferraro, M.; et al. Frailty as the Future Core Business of Public Health: Report of the Activities of the A3 Action Group of the European Innovation Partnership on Active and Healthy Ageing (EIP on AHA). Int. J. Environ. Res. Public Health 2018, 15, 2843. https://doi.org/10.3390/ijerph15122843
Liotta G, Ussai S, Illario M, O’Caoimh R, Cano A, Holland C, Roller-Winsberger R, Capanna A, Grecuccio C, Ferraro M, et al. Frailty as the Future Core Business of Public Health: Report of the Activities of the A3 Action Group of the European Innovation Partnership on Active and Healthy Ageing (EIP on AHA). International Journal of Environmental Research and Public Health. 2018; 15(12):2843. https://doi.org/10.3390/ijerph15122843
Chicago/Turabian StyleLiotta, Giuseppe, Silvia Ussai, Maddalena Illario, Rónán O’Caoimh, Antonio Cano, Carol Holland, Regina Roller-Winsberger, Alessandra Capanna, Chiara Grecuccio, Mariacarmela Ferraro, and et al. 2018. "Frailty as the Future Core Business of Public Health: Report of the Activities of the A3 Action Group of the European Innovation Partnership on Active and Healthy Ageing (EIP on AHA)" International Journal of Environmental Research and Public Health 15, no. 12: 2843. https://doi.org/10.3390/ijerph15122843
APA StyleLiotta, G., Ussai, S., Illario, M., O’Caoimh, R., Cano, A., Holland, C., Roller-Winsberger, R., Capanna, A., Grecuccio, C., Ferraro, M., Paradiso, F., Ambrosone, C., Morucci, L., Scarcella, P., De Luca, V., & Palombi, L. (2018). Frailty as the Future Core Business of Public Health: Report of the Activities of the A3 Action Group of the European Innovation Partnership on Active and Healthy Ageing (EIP on AHA). International Journal of Environmental Research and Public Health, 15(12), 2843. https://doi.org/10.3390/ijerph15122843








