Healthcare Utilization and All-Cause Premature Mortality in Hungarian Segregated Roma Settlements: Evaluation of Specific Indicators in a Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Setting
2.2. Design
2.3. Mapping Segregated Roma Settlements
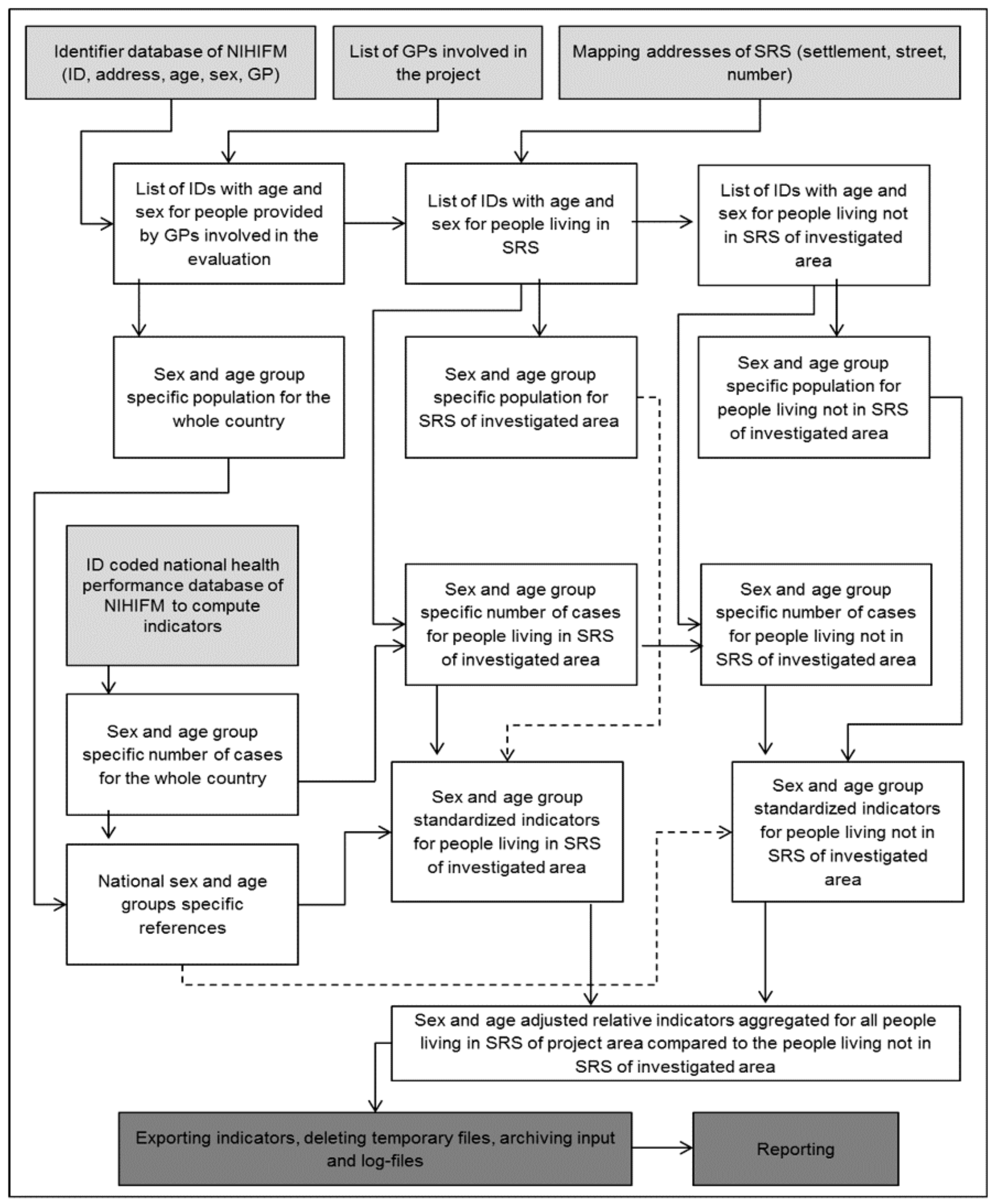
2.4. Roma Settlement Specific Version of NIHIFM’ Routine Primary Adult Care Indicators
2.5. Statistical Analysis
2.6. Ethics Approval and Consent to Participate
2.7. Availability of Data and Material
3. Results
3.1. Pathway Indicators
3.2. Performance Indicators
3.3. All-Cause Premature Mortality
4. Discussion
4.1. New Indicator Set for Segregated Roma Settlements
4.2. Main Findings and Concordance with Others’ Observations
4.3. Strengths and Limitations
4.4. Implications
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Adany, R. Roma health is global ill health. Eur. J. Public Health 2014, 24, 702–703. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- European Commission. European Commission: Communication from the Commission to the European Parliament, the Council, the European Economic and Social Committee and the Committee of the Regions. An EU Framework for National Roma Integration Strategies up to 2020; European Commission: Brussels, Belgium, 2011. [Google Scholar]
- Hajioff, S.; McKee, M. The health of the Roma people: A review of the published literature. J. Epidemiol. Community Health 2000, 54, 864–869. [Google Scholar] [CrossRef] [PubMed]
- Marmot, M. Health Inequalities in the EU—Final Report of a Consortium. European Union: European Commission Directorate-General for Health and Consumers; European Commission: Brussels, Belgium, 2013. [Google Scholar]
- European Commission. European Commission: The Commission’s Assessment of Hungary’s National Strategy; European Commission: Brussels, Belgium, 2012. [Google Scholar]
- European Commission. European Commission: Roma Health Report. Health Status of the Roma Population Data Collection in the Member States of the European Union; European Commission: Brussels, Belgium, 2014. [Google Scholar]
- Richard, L.; Furler, J.; Densley, K.; Haggerty, J.; Russell, G.; Levesque, J.F.; Gunn, J. Equity of access to primary healthcare for vulnerable populations: The IMPACT international online survey of innovations. Int. J. Equity Health 2016, 15, 64. [Google Scholar] [CrossRef] [PubMed]
- Ringold, D.; Orenstein, M.; Wilkens, E. Roma in an Expanding Europe: Breaking the Poverty Cycle; The International Bank for Reconstruction and Development/The World Bank: Washington, DC, USA, 2005. [Google Scholar]
- Kosa, K.; Adany, R. Studying vulnerable populations: Lessons from the Roma minority. Epidemiology 2007, 18, 290–299. [Google Scholar] [PubMed]
- Jakab, Z.; Juhasz, A.; Nagy, C.; Schuler, D.; Garami, M. Trends and territorial inequalities of incidence and survival of childhood leukaemia and their relations to socioeconomic status in Hungary, 1971–2015. Eur. J. Cancer Prev. 2017, 26, S183–S190. [Google Scholar] [CrossRef] [PubMed]
- Boruzs, K.; Juhasz, A.; Nagy, C.; Adany, R.; Biro, K. Relationship between Statin Utilization and Socioeconomic Deprivation in Hungary. Front. Pharmacol. 2016, 7, 66. [Google Scholar] [CrossRef] [PubMed]
- Nagy, C.; Juhasz, A.; Beale, L.; Paldy, A. Mortality amenable to health care and its relation to socio-economic status in Hungary, 2004–2008. Eur. J. Public Health 2012, 22, 620–624. [Google Scholar] [CrossRef] [PubMed]
- Sebestyen, A.; Toth, F.; Sandor, J.; Nyarady, J.; Boncz, I. Correlation between risk factors and subsequent surgical management following internal fixation of intracapsular femoral neck fractures in patients under the age of 60 years. Eur. J. Trauma Emerg. Surg. 2011, 37, 503–510. [Google Scholar] [CrossRef] [PubMed]
- Kosa, I.; Nemes, A.; Belicza, E.; Kiraly, F.; Vassanyi, I. Regional differences in the utilisation of coronary angiography as initial investigation for the evaluation of patients with suspected coronary artery disease. Int. J. Cardiol. 2013, 168, 5012–5015. [Google Scholar] [CrossRef] [PubMed]
- Kosa, K.; Darago, L.; Adany, R. Environmental survey of segregated habitats of Roma in Hungary: A way to be empowering and reliable in minority research. Eur. J. Public Health 2011, 21, 463–468. [Google Scholar] [CrossRef] [PubMed]
- Sandor, J.; Kosa, Z.; Boruzs, K.; Boros, J.; Tokaji, I.; McKee, M.; Adany, R. The decade of Roma Inclusion: Did it make a difference to health and use of health care services? Int. J. Public Health 2017, 62, 803–815. [Google Scholar] [CrossRef] [PubMed]
- Adany, R.; Kosa, K.; Sandor, J.; Papp, M.; Furjes, G. General practitioners’ cluster: A model to reorient primary health care to public health services. Eur. J. Public Health 2013, 23, 529–530. [Google Scholar] [CrossRef] [PubMed]
- Jakab, Z. Public health, primary care and the ‘cluster’ model. Eur. J. Public Health 2013, 23, 528. [Google Scholar] [CrossRef] [PubMed]
- Sandor, J.; Kosa, K.; Papp, M.; Furjes, G.; Korosi, L.; Jakovljevic, M.; Adany, R. Capitation-Based Financing Hampers the Provision of Preventive Services in Primary Health Care. Front. Public Health 2016, 4, 200. [Google Scholar] [CrossRef] [PubMed]
- Sandor, J.; Nagy, A.; Foldvari, A.; Szabo, E.; Csenteri, O.; Vincze, F.; Sipos, V.; Kovacs, N.; Palinkas, A.; Papp, M.; et al. Delivery of cardio-metabolic preventive services to Hungarian Roma of different socio-economic strata. Fam. Pract. 2017, 34, 83–89. [Google Scholar] [CrossRef] [PubMed]
- Kosa, Z.; Szeles, G.; Kardos, L.; Kosa, K.; Nemeth, R.; Orszagh, S.; Fesus, G.; McKee, M.; Adany, R.; Voko, Z. A comparative health survey of the inhabitants of Roma settlements in Hungary. Am. J. Public Health 2007, 97, 853–859. [Google Scholar] [CrossRef] [PubMed]
- Kosa, Z.; Moravcsik-Kornyicki, A.; Dioszegi, J.; Roberts, B.; Szabo, Z.; Sandor, J.; Adany, R. Prevalence of metabolic syndrome among Roma: A comparative health examination survey in Hungary. Eur. J. Public Health 2015, 25, 299–304. [Google Scholar] [CrossRef] [PubMed]
- Ádány, R. (Ed.) Operations Manual for GPs Cluster on Public Health Services in Primary Health Care. Version 5. 2013. Available online: https://nepegeszseg.hu/Swiss/SH.8.1_operations_manual_version5.pdf (accessed on 24 August 2018).
- Government of Hungary. National Social Inclusion Strategy and the Government Action Plan on Its Implementation between 2015 and 2017; Government of Hungary: Budapest, Hungary, 2015. [Google Scholar]
- Jackson, C.; Bedford, H.; Cheater, F.M.; Condon, L.; Emslie, C.; Ireland, L.; Kemsley, P.; Kerr, S.; Lewis, H.J.; Mytton, J.; et al. Needles, Jabs and Jags: A qualitative exploration of barriers and facilitators to child and adult immunisation uptake among Gypsies, Travellers and Roma. BMC Public Health 2017, 17, 254. [Google Scholar] [CrossRef] [PubMed]
- Sudzinova, A.; Nagyova, I.; Studencan, M.; Rosenberger, J.; Skodova, Z.; Vargova, H.; Middel, B.; Reijneveld, S.A.; van Dijk, J.P. Roma coronary heart disease patients have more medical risk factors and greater severity of coronary heart disease than non-Roma. Int. J Public Health 2013, 58, 409–415. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sudzinova, A.; Nagyova, I.; Rosenberger, J.; Studencan, M.; Vargova, H.; Middel, B.; van Dijk, J.P.; Reijneveld, S.A. Seven years’ mortality in Roma and non-Roma patients after coronary angiography. Eur. J. Public Health 2015, 25, 765–769. [Google Scholar] [CrossRef] [PubMed]
- Ekuklu, G.; Berberoglu, U.; Eskiocak, M.; Saltik, A. Utilization of primary health care services by Turkish gypsies and members of the general population at Muradiye Health Unit District in Edirne, Turkey. Yonsei Med. J. 2003, 44, 414–423. [Google Scholar] [CrossRef] [PubMed]
- Colombini, M.; Rechel, B.; Mayhew, S.H. Access of Roma to sexual and reproductive health services: Qualitative findings from Albania, Bulgaria and Macedonia. Glob. Public Health 2012, 7, 522–534. [Google Scholar] [CrossRef] [PubMed]
- Carrasco-Garrido, P.; Lopez de Andres, A.; Hernandez Barrera, V.; Jimenez-Trujillo, I.; Jimenez-Garcia, R. Health status of Roma women in Spain. Eur. J. Public Health 2011, 21, 793–798. [Google Scholar] [CrossRef] [PubMed]
- Hull, S.; Mathur, R.; Boomla, K.; Chowdhury, T.A.; Dreyer, G.; Alazawi, W.; Robson, J. Research into practice: Understanding ethnic differences in healthcare usage and outcomes in general practice. Br. J. Gen. Pract. 2014, 64, 653–655. [Google Scholar] [CrossRef] [PubMed]
- Badrick, E.; Hull, S.; Mathur, R.; Shajahan, S.; Boomla, K.; Bremner, S.; Robson, J. Health equity audits in general practice: A strategy to reduce health inequalities. Primary Health Care Res. Dev. 2014, 15, 80–95. [Google Scholar] [CrossRef] [PubMed]
- Lin, S.S.; Kelsey, J.L. Use of race and ethnicity in epidemiologic research: Concepts, methodological issues, and suggestions for research. Epidemiol. Rev. 2000, 22, 187–202. [Google Scholar] [CrossRef] [PubMed]
- Hull, S.A.; Mathur, R.; Badrick, E.; Robson, J.; Boomla, K. Recording ethnicity in primary care: Assessing the methods and impact. Br. J. Gen. Pract. 2011, 61, e290–e294. [Google Scholar] [CrossRef] [PubMed]
- Tran, D.T.; Jorm, L.R.; Havard, A.; Harris, M.F.; Comino, E.J. Variation in the use of primary care services for diabetes management according to country of birth and geography among older Australians. Prim. Care Diabetes 2016, 10, 66–74. [Google Scholar] [CrossRef] [PubMed]
- Smylie, J.; Firestone, M. Back to the basics: Identifying and addressing underlying challenges in achieving high quality and relevant health statistics for indigenous populations in Canada. Stat. J. IAOS 2015, 31, 67–87. [Google Scholar] [PubMed]
- Levesque, J.F.; Harris, M.F.; Russell, G. Patient-centred access to health care: Conceptualising access at the interface of health systems and populations. Int. J. Equity Health 2013, 12, 18. [Google Scholar] [CrossRef] [PubMed]

| Indicator Type | Indicator Name |
|---|---|
| pathway indicators | number of GP appointments per person per year |
| proportion of subjects receiving outpatient care per year | |
| number of interventions in outpatient care per person per year | |
| reimbursement for interventions in outpatient care per person per year | |
| proportion of subjects hospitalized per year | |
| duration of hospitalization in inpatient care per person per year | |
| reimbursement for inpatient care per person per year | |
| proportion of subjects having an imaging examination per year | |
| total number of imaging examinations per person per year | |
| reimbursement for imaging examination in outpatient care per person per year | |
| performance indicators | proportion of patients above 65 years of age vaccinated against influenza within the last 12 months |
| proportion of patients aged 40–54 years with treated hypertension (taking antihypertensive medication at least four times within 12 months) | |
| proportion of patients aged 55–69 years with treated hypertension (taking antihypertensive medication at least four times within 12 months) | |
| proportion of patients having a serum creatinine test within the last 12 months among treated hypertensive patients (taking antihypertensive drugs at least four times within the last 12 months) | |
| proportion of patients having a lipid status assessment within the last 12 months among treated hypertensive and/or treated diabetes patients (taking antihypertensive medication at least four times within 12 months and/or taking ATC code A10 drugs at least four times within the last 12 months) | |
| proportion of patients taking beta-blocker medication at least four times within 12 months relative to the total number of acute myocardial infarction (MI) and/or coronary artery bypass surgery (CABG) and/or percutaneous coronary intervention (PTCA) patients | |
| proportion of patients among treated diabetes patients having a hemoglobin A1c test within the last 12 months (taking ATC code A10 drugs at least four times within the last 12 months) | |
| proportion of patients among treated diabetes patients examined by ophthalmologist within the last 12 months (taking ATC code A10 drugs at least four times within the last 12 months) | |
| proportion of patients aged 40–54 years with treated diabetes mellitus (taking ATC code A10 drugs at least four times within 12 months) | |
| proportion of patients aged 55–69 years with treated diabetes mellitus (taking ATC code A10 drugs at least four times within 12 months) | |
| per capita amount of purchased antibiotics prescribed by the GP, in the previous 12 months | |
| participation rate of mammography in the previous 24 months among 45- to 65-year-old women | |
| participation rate of cervical cytology in the previous 36 months among 25- to 65-year-old women | |
| all-cause premature mortality | mortality rate for adults 18–64 years old who had not changed GMPs in the five years prior to the investigated year |
| Indicators | Crude Rates in the Sample, N (%) | SRS | Non-SRS | RR [95% CI] | ||
|---|---|---|---|---|---|---|
| N | Standardized Rates [95% CI] | N | Standardized Rates [95% CI] | |||
| number of GP appointments (appointments per capita per year) | 454,257 (8.31) | 22,322 | 1.144 [1.129–1.159] | 431,935 | 0.994 [0.991–0.996] | 1.152 [1.136–1.167] |
| number of subjects receiving outpatient care at least once a year (%) | 40,255 (73.62) | 2059 | 0.97 [0.929–1.012] | 38,196 | 1.002 [0.992–1.012] | 0.968 [0.926–1.012] |
| number of interventions in outpatient care a year (interventions per capita) | 1,834,015 (33.54) | 76,715 | 0.897 [0.891–0.904] | 1,757,300 | 1.005 [1.004–1.007] | 0.893 [0.886–0.899] |
| reimbursement in outpatient care a year (EURO per capita) | 2,011,662 (36.79) | 87,311 | 0.924 [0.918–0.930] | 1,924,351 | 1.004 [1.002–1.005] | 0.920 [0.914–0.927] |
| number of subjects having imaging examination at least once a year (%) | 28,629 (52.36) | 1556 | 1.061 [1.009–1.115] | 27,073 | 0.997 [0.985–1.009] | 1.064 [1.011–1.120] |
| number of imaging examinations a year (examinations per capita) | 1,076,117 (19.68) | 44,413 | 0.899 [0.891–0.908] | 1,031,704 | 1.005 [1.003–1.007] | 0.895 [0.887–0.904] |
| reimbursement for imaging examination a year (EURO per capita) | 703,974 (12.87) | 34,139 | 1.034 [1.023–1.046] | 669,835 | 0.998 [0.996–1.001] | 1.036 [1.025–1.047] |
| number of subjects being hospitalized at least once a year (%) | 9007 (16.47) | 522 | 1.269 [1.165–1.383] | 8,485 | 0.987 [0.966–1.008] | 1.286 [1.177–1.405] |
| duration of hospitalization a year (days per capita) | 142,475 (2.61) | 58,265 | 1.162 [1.132–1.192] | 136,649 | 0.994 [0.989–0.999] | 1.168 [1.138–1.200] |
| reimbursement in inpatient care a year (EURO per capita) | 7,554,882 (138.16) | 299,580 | 1.058 [1.054–1.061] | 7,255,301 | 0.9977 [0.9970–0.9984] | 1.060 [1.057–1.064] |
| Indicators | Crude Rates in the Sample, N (%) | SRS | Non-SRS | RR [95% CI] | ||
|---|---|---|---|---|---|---|
| N | Standardized Rates [95% CI] | N | Standardized Rates [95% CI] | |||
| influenza vaccination, above 65 years of age | 2523 (23.22) | 29 | 0.679 [0.472–0.977] | 2494 | 1.006 [0.967–1.046] | 0.675 [0.468–0.973] |
| prevalence of hypertension, 40–54 years | 3461 (25.57) | 200 | 0.999 [0.870–1.148] | 3261 | 1.000 [0.966–1.035] | 0.999 [0.866–1.153] |
| prevalence of hypertension, 55–69 years | 6938 (55.99) | 200 | 0.916 [0.798–1.053] | 6738 | 1.003 [0.979–1.027] | 0.914 [0.794–1.052] |
| Serum-creatinine assessment, hypertension | 10447 (60.99) | 309 | 0.964 [0.863–1.078] | 10,138 | 1.001 [0.982–1.021] | 0.963 [0.860–1.079] |
| lipid status check-up, hypertension and/or diabetes | 9666 (54.73) | 324 | 1.067 [0.957–1.189] | 9342 | 0.998 [0.978–1.018] | 1.069 [0.957–1.194] |
| beta–blocker, ischemic heart diseases | 523 (51.73) | 23 | 1.049 [0.697–1.579] | 500 | 0.998 [0.914–1.089] | 1.052 [0.692–1.597] |
| HbA1c check-up, diabetes | 2674 (73.64) | 82 | 0.817 [0.658–1.015] | 2592 | 1.007 [0.969–1.047] | 0.811 [0.651–1.011] |
| ophthalmologic check-up, diabetes | 1313 (36.16) | 34 | 0.701 [0.501–0.982] | 1279 | 1.011 [0.958–1.068] | 0.693 [0.493–0.975] |
| prevalence of diabetes, 40–54 years | 618 (4.57) | 40 | 1.123 [0.824–1.531] | 578 | 0.992 [0.915–1.077] | 1.132 [0.821–1.559] |
| prevalence of diabetes, 55–69 years | 1241 (10.01) | 36 | 0.929 [0.670–1.287] | 1205 | 1.002 [0.947–1.061] | 0.927 [0.665–1.291] |
| treatment with antibiotics | 13371 (24.49) | 570 | 0.791 [0.728–0.858] | 12,801 | 1.012 [0.995–1.030] | 0.781 [0.718–0.850] |
| mammography, 45–64 years | 4451 (47.96) | 76 | 0.392 [0.313–0.490] | 4375 | 1.028 [0.998–1.059] | 0.381 [0.304–0.478] |
| cervix cytology, 25–64 years | 7365 (40.22) | 428 | 0.959 [0.873–1.055] | 6937 | 1.003 [0.979–1.027] | 0.957 [0.868–1.055] |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sándor, J.; Pálinkás, A.; Vincze, F.; Kovács, N.; Sipos, V.; Kőrösi, L.; Falusi, Z.; Pál, L.; Fürjes, G.; Papp, M.; et al. Healthcare Utilization and All-Cause Premature Mortality in Hungarian Segregated Roma Settlements: Evaluation of Specific Indicators in a Cross-Sectional Study. Int. J. Environ. Res. Public Health 2018, 15, 1835. https://doi.org/10.3390/ijerph15091835
Sándor J, Pálinkás A, Vincze F, Kovács N, Sipos V, Kőrösi L, Falusi Z, Pál L, Fürjes G, Papp M, et al. Healthcare Utilization and All-Cause Premature Mortality in Hungarian Segregated Roma Settlements: Evaluation of Specific Indicators in a Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2018; 15(9):1835. https://doi.org/10.3390/ijerph15091835
Chicago/Turabian StyleSándor, János, Anita Pálinkás, Ferenc Vincze, Nóra Kovács, Valéria Sipos, László Kőrösi, Zsófia Falusi, László Pál, Gergely Fürjes, Magor Papp, and et al. 2018. "Healthcare Utilization and All-Cause Premature Mortality in Hungarian Segregated Roma Settlements: Evaluation of Specific Indicators in a Cross-Sectional Study" International Journal of Environmental Research and Public Health 15, no. 9: 1835. https://doi.org/10.3390/ijerph15091835
APA StyleSándor, J., Pálinkás, A., Vincze, F., Kovács, N., Sipos, V., Kőrösi, L., Falusi, Z., Pál, L., Fürjes, G., Papp, M., & Ádány, R. (2018). Healthcare Utilization and All-Cause Premature Mortality in Hungarian Segregated Roma Settlements: Evaluation of Specific Indicators in a Cross-Sectional Study. International Journal of Environmental Research and Public Health, 15(9), 1835. https://doi.org/10.3390/ijerph15091835







