How Older Adults Cope with Cognitive Complexity and Environmental Constraints during Dual-Task Walking: The Role of Executive Function Involvement
Abstract
:1. Introduction
2. Materials and Methods
2.1. Procedures
2.1.1. Cognitive Assessment in ST and DT
2.1.2. Gait Assessment in ST and DT
2.1.3. Computation of DT Effects for Cognitive and Gait Variables
2.1.4. Assessment of Covariates
2.2. Statistical Analysis
3. Results
3.1. Descriptive Statistics
3.2. Dual Task Effects on Gait Performance
3.2.1. Effects of Environmental Constraints on Gait
3.2.2. Effects of Cognitive Complexity on Gait
3.2.3. Interactive Effects of Environmental Constraints and Cognitive Demands on Gait
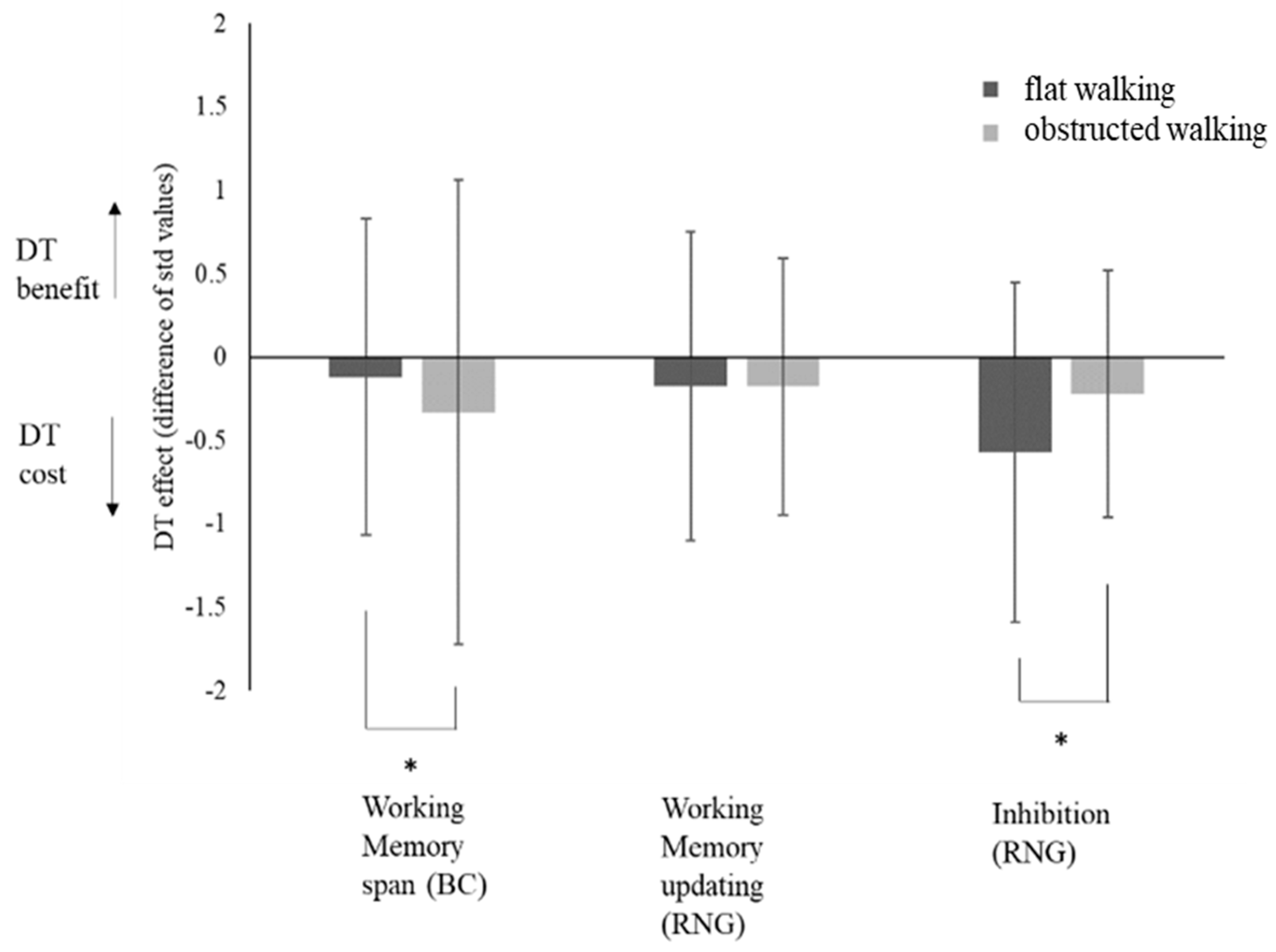
3.3. Dual-Task Effects on Cognitive Performance
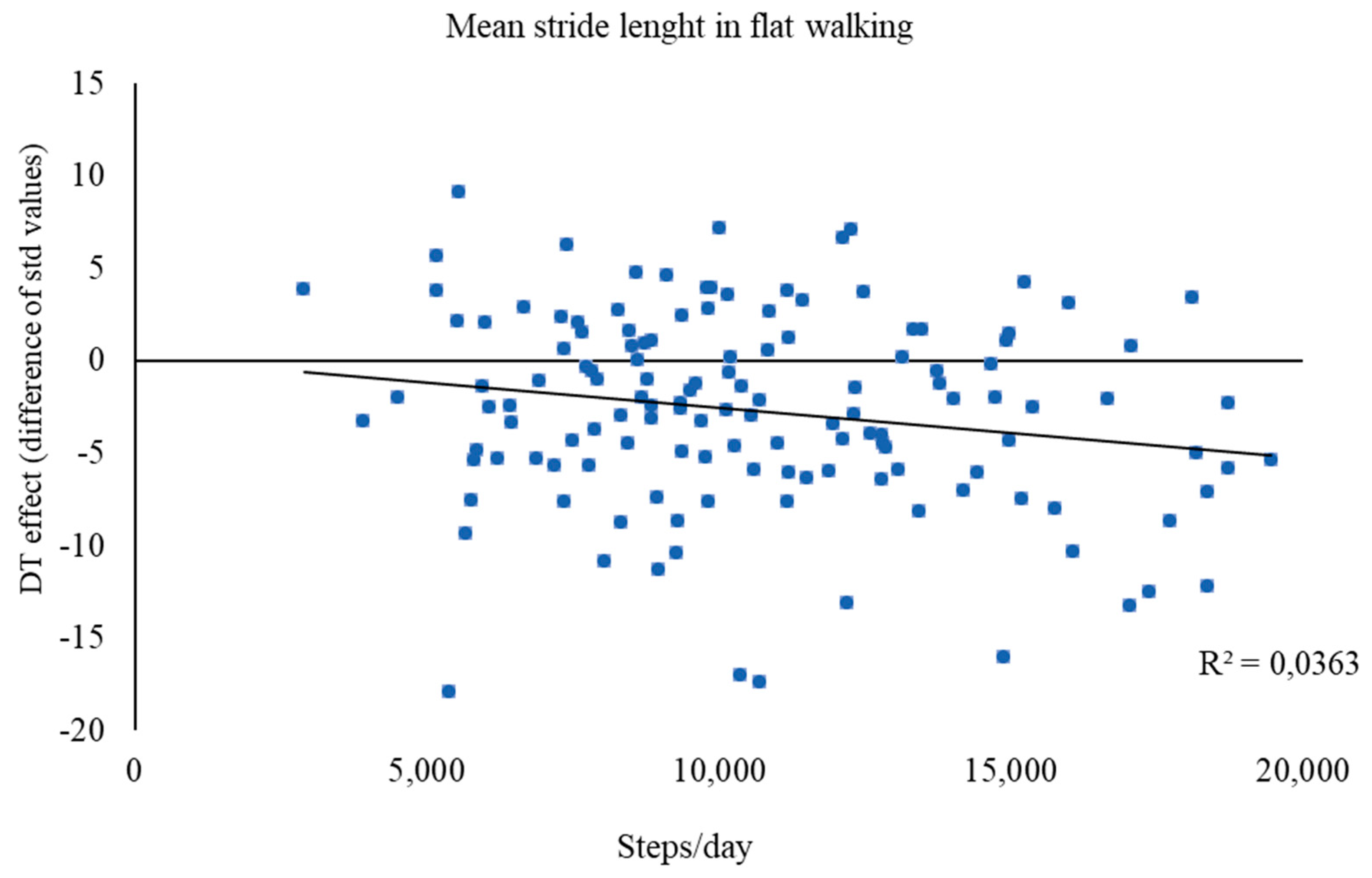
3.4. Prediction of Dual-Task Effects by Physical Activity Level
4. Discussion
4.1. Reciprocal Dual-Task Effects and Task Prioritization
4.2. Dual-Task Effects on Gait: Influence of Physical Activity
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Shumway-Cook, A.; Woollacott, M. Motor Control: Translating Research into Clinical Practice, 4th ed.; Wolters Kluwer Health/Lippincott Williams & Wilkins: Baltimore, MD, USA, 2011. [Google Scholar]
- World Health Organization. Global Action Plan on Physical Activity 2018–2030: More Active People for a Healthier World; World Health Organization: Geneva, Switzerland, 2018; Licence: CC BY-NC-SA 3.0 IGO. [Google Scholar]
- Sussman, A.; Goode, R. The Magic of Walking; Simon and Schuster: New York, NY, USA, 1967. [Google Scholar]
- World Health Organization. Steps to Health—A European Framework to Promote Physical Activity for Health; WHO Regional Office Europe: Copenhagen, Denmark, 2007. [Google Scholar]
- Campos, J.J.; Anderson, D.I.; Barbu-Roth, M.A.; Hubbard, E.M.; Hertenstein, M.J.; Witherington, D. Travel broadens the mind. Infancy 2000, 1, 149–219. [Google Scholar] [CrossRef]
- Iezzoni, L.I. When Walking Fails: Mobility Problems of Adults with Chronic Conditions; University of California Press: Los Angeles, CA, USA, 2003. [Google Scholar]
- Forte, R.; Pesce, C.; Costa Leite, J.; De Vito, G.; Gibney, E.; Tomporoski, P.D.; Boreham, C.A. Executive function moderates the role of physical fitness in determining functional ability of older individuals. Aging Clin. Exp. Res. 2013, 25, 291–298. [Google Scholar] [CrossRef] [PubMed]
- Hausdorff, J.M.; Yogev, G.; Springer, S.; Simon, E.S.; Giladi, N. Walking is more like catching than tapping: Gait in the elderly as a complex cognitive task. Exp. Brain Res. 2005, 164, 541–548. [Google Scholar] [CrossRef]
- Yogev, G.; Hausdorff, J.M.; Giladi, N. The role of executive function and attention in gait. Mov. Disord. 2008, 23, 329–472. [Google Scholar] [CrossRef]
- Seidler, R.D.; Bernard, J.A.; Burutolu, T.B.; Fling, B.W.; Gordon, M.T.; Gwin, J.T.; Kwak, Y.; Lipps, D.B. Motor control and aging: Links to age-related brain structural, functional, and biochemical effects. Neurosci. Biobehav. Rev. 2010, 34, 721–733. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Turner, G.R.; Spreng, R.N. Executive functions and neurocognitive aging: Dissociable patterns of brain activity. Neurobiol. Aging 2012, 33, e1–e13. [Google Scholar] [CrossRef] [PubMed]
- Al-Yahya, E.; Dawes, H.; Smith, L.; Dennis, A.; Howells, K.; Cockburn, J. Cognitive motor interference while walking: A systematic review and meta-analysis. Neurosci. Biobehav. Rev. 2011, 35, 715–728. [Google Scholar] [CrossRef]
- de Cássia Gomes, G.; Fuscaldi Teixeira-Salmela, L.; Silveira de Freitas, F.A.; Morais Fonseca, M.L.; de Barros Pinheiro, M.; de Carvalho Morais, V.A.; Caramelli, P. Gait performance of the elderly under dual-task conditions: Review of instruments employed and kinematic parameters. Revista Brasileira de Geriatria e Gerontologia 2016, 19, 165–182. [Google Scholar] [CrossRef] [Green Version]
- Beurskens, R.; Bock, O. Age-related deficits of dual-task walking: A review. Neural Plast. 2012, 131608. [Google Scholar] [CrossRef]
- Bridenbaugh, S.A.; Kressig, R.W. Laboratory review: The role of gait analysis in seniors’ mobility and fall prevention. Gerontology 2011, 57, 256–264. [Google Scholar] [CrossRef] [PubMed]
- Makizako, H.; Furuna, T.; Shimada, H.; Ihira, H.; Kimura, M.; Uchiyama, E.; Oddsson, L.I. Association between a history of falls and the ability to multi-task in community-dwelling older people. Aging Clin. Exp. Res. 2010, 22, 427–432. [Google Scholar] [CrossRef] [PubMed]
- Schaefer, S.; Schellenbach, M.; Lindenberger, U.; Woollacott, M. Walking in high-risk settings: Do older adults still prioritize gait when distracted by a cognitive task? Exp. Brain Res. 2015, 233, 79–88. [Google Scholar] [CrossRef] [PubMed]
- Shumway-Cook, A.; Woollacott, M.; Kerns, K.A.; Baldwin, M. The effects of two types of cognitive tasks on postural stability in older adults with and without a history of falls. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 1997, 52, M232–M240. [Google Scholar] [CrossRef] [PubMed]
- Kelly, V.E.; Janke, A.A.; Shumway-Cook, A. Effects of instructed focus and task difficulty on concurrent walking and cognitive task performance in healthy young adults. Exp. Brain Res. 2010, 207, 65–73. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, K.Z.; Lindenberger, U.; Freund, A.M.; Baltes, P.B. Walking while memorizing: Age-related differences in compensatory behavior. Psychol. Sci. 2001, 12, 230–237. [Google Scholar] [CrossRef]
- Sun, R.; Shea, J.B. Probing attention prioritization during dual task step initiation: A novel method. Exp. Brain Res. 2016, 234, 1047–1056. [Google Scholar] [CrossRef]
- Yogev-Seligmann, G.; Hausdorff, J.M.; Giladi, N. Do we always prioritize balance when walking? Towards an integrated model of task prioritization. Mov. Disord. 2012, 27, 765–770. [Google Scholar] [CrossRef]
- Smith, E.; Cusack, T.; Cunningham, C.; Blake, C. The influence of a cognitive dual task on the gait parameters of healthy older adults: A systematic review and meta-analysis. J. Aging Phys. Act. 2017, 25, 671–686. [Google Scholar] [CrossRef] [PubMed]
- Chu, Y.H.; Tang, P.F.; Peng, Y.C.; Chen, H.Y. Meta-analysis of type and complexity of a secondary task during walking on the prediction of elderly falls. Geriatr. Gerontol. Intl. 2013, 13, 289–297. [Google Scholar] [CrossRef]
- Huxhold, O.; Li, S.-C.; Schmiedek, F.; Lindenberger, U. Dual tasking postural control. Aging and the effects of cognitive demand in conjunction with focus of attention. Brain Res. Bull. 2006, 69, 294–305. [Google Scholar] [CrossRef]
- Lövdén, M.; Schaefer, S.; Pohlmeyer, A.E.; Lindenberger, U. Walking variability and working-memory load in aging: A dual-process account relating cognitive control to motor control performance. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2008, 63, P121–P128. [Google Scholar] [CrossRef] [PubMed]
- Brustio, P.R.; Magistro, D.; Zecca, M.; Rabaglietti, E.; Liubicich, M. Age-related decrements in dual-task performance: Comparison of different mobility and cognitive tasks. A cross sectional study. PLoS ONE 2017, 12, e0181698. [Google Scholar] [CrossRef] [PubMed]
- Plummer-D’Amato, P.; Brancato, B.; Dantowitz, M.; Birken, S.; Bonke, C.; Furey, E. Effects of gait and cognitive task difficulty on cognitive-motor interference in aging. J. Aging Res. 2012, 583894. [Google Scholar] [CrossRef] [PubMed]
- Beauchet, O.; Annweiler, C.; Montero-Odasso, M.; Fantino, B.; Herrmann, F.R.; Allali, G. Gait control: A specific subdomain of executive function? J. Neuroeng. Rehabil. 2012, 9, 12. [Google Scholar] [CrossRef] [PubMed]
- Bherer, L.; Erickson, K.I.; Liu-Ambrose, T. A review of the effects of physical activity and exercise on cognitive and brain functions in older adults. J. Aging Res. 2013, 657508. [Google Scholar] [CrossRef]
- Northey, J.M.; Cherbuin, N.; Pumpa, K.L.; Smee, D.J.; Rattray, B. Exercise interventions for cognitive function in adults older than 50: A systematic review with meta-analysis. Br. J. Sports Med. 2018, 52, 154–160. [Google Scholar] [CrossRef] [PubMed]
- Plummer, P.; Zukowski, L.A.; Giuliani, C.; Hall, A.M.; Zurakowski, D. Effects of physical exercise interventions on gait-related dual-task interference in older adults: A systematic review and meta-analysis. Gerontology 2015, 62, 94–117. [Google Scholar] [CrossRef] [PubMed]
- Blondell, S.J.; Hammersley-Mather, R.; Veerman, J.L. Does physical activity prevent cognitive decline and dementia? A systematic review and meta-analysis of longitudinal studies. BMC Public Health 2014, 14, 510. [Google Scholar] [CrossRef]
- Engeroff, T.; Ingmann, T.; Banzer, W. Physical activity throughout the adult life span and domain-specific cognitive function in old age: A systematic review of cross-sectional and longitudinal data. Sports Med. 2018, 48, 1405–1436. [Google Scholar] [CrossRef] [PubMed]
- Bootsman, N.J.M.; Skinner, T.L.; Lal, R.; Glindemann, D.; Lagasca, C.; Peeters, G.M.E.E.G. The relationship between physical activity, physical performance and psycho-cognitive functioning in older adults living in residential aged care facilities. J. Sci. Med. Sport 2018, 21, 173–178. [Google Scholar] [CrossRef]
- Audiffren, M.; Tomporowski, P.D.; Zagrodnik, J. Acute aerobic exercise and information processing: Modulation of executive control in a Random Number Generation task. Acta Psychol. 2009, 132, 85–95. [Google Scholar] [CrossRef] [PubMed]
- Miyake, A.; Friedman, N.P.; Emerson, M.J.; Witzki, A.H.; Howerter, A.; Wager, T.D. The unity and diversity of executive functions and their contributions to complex “Frontal Lobe” tasks: A latent variable analysis. Cogn. Psychol. 2000, 41, 49–100. [Google Scholar] [CrossRef] [PubMed]
- Brown, L.A.; McKenzie, N.C.; Doan, J.B. Age-dependent differences in the attentional demands of obstacle negotiation. J. Gerontol. Ser. A 2005, 60, 924–927. [Google Scholar] [CrossRef]
- Kimand, H.D.; Brunt, D. The effect of a dual-task on obstacle crossing in healthy elderly and young adults. Arch. Phys. Med. Rehabil. 2007, 88, 1309–1313. [Google Scholar] [CrossRef]
- Godde, B.; Voelcker-Rehage, C. More automation and less cognitive control of imagined walking movements in high- versus low-fit older adults. Front. Aging Neurosci. 2010, 2, 139. [Google Scholar] [CrossRef]
- Osness, W.H.; Adrian, M.; Clark, B. Functional Fitness Assessment for Adults Over 60 Years, 2nd ed.; Kendall/Hunt: Dubuque, IA, USA, 1996. [Google Scholar]
- Ware, J.; Kosiniski, M.; Keller, S. SF-12. How to Score the SF-12 Physical and Mental Health Summary Scale, 3rd ed.; Quality Metric Incorporated: Lincoln, RI, USA, 1998; p. 97. [Google Scholar]
- MacPherson, S.E.; Cox, S.R.; Dickie, D.A.; Karama, S.; Starr, J.M.; Evans, A.C.; Bastin, M.E.; Wardlaw, J.M.; Deary, I.J. Processing speed and the relationship between Trail Making Test-B performance, cortical thinning and white matter microstructure in older adults. Cortex 2017, 95, 92–103. [Google Scholar] [CrossRef] [PubMed]
- Reitan, R.M. Validity of the trail making test as an indicator of organic brain damage. Percept. Mot. Skills 1958, 8, 271–276. [Google Scholar] [CrossRef]
- Falbo, S.; Condello, G.; Capranica, L.; Forte, R.; Pesce, C. Effects of physical-cognitive dual task training on executive function and gait performance in older adults: A randomized controlled trial. Biomed. Res. Int. 2016, 5812092. [Google Scholar] [CrossRef]
- Borg, G. Borg’s Perceived Exertion and Pain Scales; Human Kinetics: Champaign, IL, USA, 1998. [Google Scholar]
- Groslambert, A.; Mahon, A.D. Perceived exertion: Influence of age and cognitive development. Sports Med. 2006, 36, 911–928. [Google Scholar] [CrossRef]
- Berryman, N.; Bherer, L.; Nadeau, S.; Lauzière, S.; Lehr, L.; Bobeuf, F.; Lussier, M.; Kergoat, M.J.; Vu, T.T.; Bosquet, L. Multiple roads lead to Rome: Combined high-intensity aerobic and strength training vs. gross motor activities leads to equivalent improvement in executive functions in a. cohort of healthy older adults. AGE 2014, 36, 9710. [Google Scholar] [CrossRef] [PubMed]
- Baddeley, A.D. Working Memory; Oxford University Press: New York, NY, USA, 1986. [Google Scholar]
- Towse, J.N.; Cheshire, A. Random number generation and working memory. Eur. J. Cogn. Psychol. 2007, 19, 374–394. [Google Scholar] [CrossRef] [Green Version]
- Albinet, C.; Tomporowski, P.D.; Beasman, K. Aging and concurrent task performance: Cognitive demand and motor control. Educ. Gerontol. 2006, 32, 689–706. [Google Scholar] [CrossRef]
- Neill, D.; Towse, J. RGCalc. Quantifying Order in Response Sequences. Available online: https://www.lancaster.ac.uk/staff/towse/rgcpage.html (accessed on 2 May 2019).
- Middleton, A.; Fritz, S.L.; Lusardi, M. Walking speed: The functional vital sign. J. Aging Phys. Act. 2015, 23, 314–322. [Google Scholar] [CrossRef] [PubMed]
- Strauss, E.; Sherman, E.M.; Spreen, O. Trail Making Test. In A Compendium of Neuropsychological Tests. Administration, Norms, and Commentary, 3rd ed.; Strauss, E., Sherman, E.M.S., Spreen, O., Eds.; Oxford University Press: New York, NY, USA, 2006; pp. 655–6773. [Google Scholar]
- Fernández, A.L.; Marcopulos, B.A. A comparison of normative data for the Trail Making Test from several countries: Equivalence of norms and considerations for interpretation. Scand. J. Psychol. 2008, 49, 239–246. [Google Scholar] [CrossRef] [PubMed]
- Office of Public Health Assessment. Health Status in Utah: The Medical Outcomes Study SF-12 (2001 Utah Health Status Survey Report); Utah Department of Health: Salt Lake City, UT, USA, 2004. [Google Scholar]
- Hausdorff, J.M. Gait variability: Methods, modeling and meaning. J. Neuroeng. Rehabil. 2005, 2, 19. [Google Scholar] [CrossRef] [PubMed]
- Kelly, V.E.; Eusterbrock, A.J.; Shumway-Cook, A. Factors influencing dynamic prioritization during dual-task walking in healthy young adults. Gait Posture 2013, 37, 131–134. [Google Scholar] [CrossRef] [Green Version]
- Fritz, S.; Lusardi, M. White Paper: “Walking Speed: The Sixth Vital Sign”. J. Geriatr. Phys. Ther. 2009, 3, 2–5. [Google Scholar] [CrossRef]
- Cesari, M.; Kritchevsky, S.B.; Penninx, B.W.; Nicklas, B.J.; Simonsick, E.M.; Newman, A.B.; Tylavsky, F.A.; Brach, J.S.; Satterfield, S.; Bauer, D.C.; et al. Prognostic value of usual gait speed in well-functioning older people--results from the Health, Aging and Body Composition Study. J. Am. Geriatr. Soc. 2005, 53, 1675–1680. [Google Scholar] [CrossRef]
- Quach, L.; Galica, A.M.; Jones, R.N.; Procter-Gary, E.; Manor, B.; Hannan, M.T.; Lipisitz, L.A. The non-linear relationship between gait speed and falls: The maintenance of balance, independent living, intellect, and zest in the elderly of Boston study. J. Am. Geriatr. Soc. 2011, 59, 1069–1073. [Google Scholar] [CrossRef]
- Abellan van Kann, G.; Rolland, Y.; Andrieu, S.; Beauchet, O.; Bonnefoy, M.; Cesari, M.; Donini, L.M.; Gillette Guyonnet, S.; Inzitari, M.; Nourhashemi, F.; et al. Gait speed at usual pace as a predictor of adverse outcomes in community dwelling older people an International Academy on Nutrition and Aging (IANA) Task Force. J. Nutr. Health Aging 2009, 13, 881–889. [Google Scholar] [CrossRef]
- Hortobagy, T.; Lesinski, M.; Gabler, M.; VanSwearingen, J.M.; Malatesta, D.; Granacher, U. Effects of three types of exercise interventions on healthy old adults’ gait speed: A systematic review and meta-analysis. Sports Med. 2015, 45, 1627–1643. [Google Scholar] [CrossRef] [PubMed]
- Wollesen, B.; Voelcker-Rehage, C. Training effects on motor–cognitive dual-task performance in older adults. Eur. Rev. Aging Phys. Act. 2014, 11, 5–24. [Google Scholar] [CrossRef]
- Chang, Y.K.; Labban, J.D.; Gapin, J.I.; Etnier, J.L. The effects of acute exercise on cognitive performance: A meta-analysis. Brain Res. 2012, 1453, 87–101. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Forte, R.; Boreham, C.A.; De Vito, G.; Ditroilo, M.; Pesce, C. Measures of static postural control moderate the association of strength and power with functional dynamic balance. Aging Clin. Exp. Res. 2014, 26, 645–653. [Google Scholar] [CrossRef] [PubMed]
- Li, K.Z.H.; Krampe, R.T.; Bondar, A. An ecological approach to studying aging and dual-task performance. In Cognitive Limitations in Aging and Psychopathology; Engle, R.W., Sedek, G., Hecker, U.V., McIntosh, D.N., Eds.; Cambridge University Press: New York, NY, USA, 2005; pp. 190–218. [Google Scholar]
- Williams, D.M.; Matthews, C.E.; Rutt, C.; Napolitano, M.A.; Marcus, B.H. Interventions to increase walking behavior. Med. Sci. Sports Exerc. 2008, 40, S567–S573. [Google Scholar] [CrossRef]
- Tudor-Locke, C.; Craig, C.L.; Aoyagi, Y.; Bell, R.C.; Croteau, K.A.; Ewald, B.; Gardner, A.W.; Hatano, Y.; Matsudo, S.M.; Blair, S.N.; et al. How many steps/day are enough? For older adults and special populations. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 80. [Google Scholar] [CrossRef] [PubMed]
- Roberson, D.N., Jr.; Babic, V. Remedy for modernity: Experiences of walkers and hikers on Medvednica Mountain. Leis. Stud. 2009, 28, 105–112. [Google Scholar] [CrossRef]
- Cassarino, M.; Setti, A. Environment as ‘Brain Training’: A review of geographical and physical environmental influences on cognitive ageing. Ageing Res. Rev. 2015, 23, 167–182. [Google Scholar] [CrossRef]
- Ohly, H.; White, M.P.; Wheeler, B.W.; Bethel, A.; Ukoumunne, O.C.; Nikolaou, V.; Garside, R. Attention Restoration Theory: A systematic review of the attention restoration potential of exposure to natural environments. J. Toxicol. Environ. Health Part B 2016, 19, 305–343. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Gender Female (n) Male (n) | 72 (54%) 63 (46%) |
| Height (cm) | 165.0 ± 90.0 |
| Body mass (kg) | 72.4 ±12.6 |
| BMI (kg/h2) | 26.5 ± 3.5 |
| Daily steps (mean ± SD) | 10,669 ± 3671 |
| Educational level <High school (n) High school (n) College (n) | 35 (26%) 66 (49%) 34 (25%) |
| Drugs (mean ± SD) | 2.8 ± 2.7 |
| Diseases (mean ± SD) | 2.4 ± 2.3 |
| Retirement Yes (n) No (n) | 99 (73%) 36 (27%) |
| Smoking No (n) In the past (n) Yes (n) | 69 (51%) 49 (36%) 17 (13%) |
| Alcohol No (n) Occasionally (n) | 50 (37%) 85 (63%) |
| SF-12 PCS (pts) MCS (pts) | 52.2 ± 7.1 51.5 ± 9.1 |
| Delta Trail Making (s) | 49.0 ± 40.6 |
| Environmental Constraints on Walking | Cognitive Task Demands | |||
| Single Tasking | Low | High | Low | High |
| (1) Flat walking | (2) Obstructed walking | (3) Backward counting | (4) Random number generation | |
| Environmental Constraint | Cognitive Demands | |||
| Dual Tasking | Low–Low | Low–High | High–Low | High–High |
| (5) Flat walking with BC | (6) Flat walking with RNG | (7) Obstructed walking with BC | (8) Obstructed walking with RNG | |
| Working Memory Updating | |
|---|---|
| Redundancy | Index reflecting the unbalance of response alternative frequencies in a sequence of generated numbers based on the theoretical frequencies of each digit |
| Coupon | Index of the mean number of responses given before all the alternative responses are used |
| Mean Repetition Gap | Index of the average quantity of digits between successive occurrences of the same number calculated for all digits throughout the whole sequence |
| Inhibition | |
| Turning Point Index | Index of the similarity between the real frequencies of changes between ascending and descending series of numbers and their theoretical frequency in random responses |
| Runs | Index of variability of the number of digits in successive ascending or descending runs |
| Adjacency | Index of the relative frequency of pairs of adjacent ascending or descending numbers |
| Single Task | Dual TaskBC | Dual TaskRNG | DTEBC % | DTERNG % | ||
|---|---|---|---|---|---|---|
| Flat walking | Mean Speed (m/s) | 1.35 ± 0.19 | 1.38 ± 0.22 | 1.13 ± 0.28 | 2.83 ± 12.64 | −16.44 ± 16.30 |
| CV Speed (sd/mean × 100) | 3.53 ± 1.20 | 4.27 ± 2.36 | 6.19 ± 5.83 | 29.65 ± 79.40 | 88.96 ± 198.80 | |
| Mean Stride length (m) | 0.85 ± 0.08 | 0.86 ± 0.08 | 0.79 ± 0.08 | 1.69 ± 6.13 | −7.07 ± 6.39 | |
| CV Stride length (sd/mean × 100) | 2.98 ± 1.44 | 3.85 ± 2.59 | 3.69 ± 1.56 | 39.69 ± 94.82 | 33.85 ± 58.61 | |
| Ostacle walking | Mean Speed (m/s) | 1.15 ± 0.16 | 1.19 ± 0.19 | 1.04 ± 0.21 | 3.56 ± 11.13 | −9.17 ± 12.31 |
| CV Speed (sd/mean × 100) | 12.59 ± 4.30 | 13.23 ± 5.31 | 13.06 ± 4.53 | 11.42 ± 74.16 | 7.75 ± 31.31 | |
| Mean Stride length (m) | 0.84 ± 0.07 | 0.85 ± 0.07 | 0.82 ± 0.08 | 1.65 ± 5.84 | −3.18 ± 5.19 | |
| CV Stride length (sd/mean × 100) | 9.60 ± 7.38 | 8.48 ± 2.72 | 8.70 ± 2.19 | −0.66 ± 43.70 | 1.02 ± 35.93 |
| Single Task | Dual Taskflat | Dual Taskobstacle | DTEflat | DTEobstacle | |
|---|---|---|---|---|---|
| Working Memory span (std score) | 0.15 ± 1.17 | 0.03 ± 0.90 | −0.18 ± 0.89 | −0.12 ± 0.95 | −0.33 ± 1.39 |
| Working Memory updating (std score) | 0.12 ± 0.74 | −0.057 ± 0.91 | -0.06 ± 0.70 | −0.17 ± 0.93 | −0.18 ± 0.77 |
| Inhibition (std score) | 0.26 ± 0.51 | −0.31 ± 0.99 | 0.44 ± 0.56 | −0.57 ± 1.02 | 0.22 ± 0.74 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Forte, R.; Pesce, C.; Di Baldassarre, A.; Shea, J.; Voelcker-Rehage, C.; Capranica, L.; Condello, G. How Older Adults Cope with Cognitive Complexity and Environmental Constraints during Dual-Task Walking: The Role of Executive Function Involvement. Int. J. Environ. Res. Public Health 2019, 16, 1835. https://doi.org/10.3390/ijerph16101835
Forte R, Pesce C, Di Baldassarre A, Shea J, Voelcker-Rehage C, Capranica L, Condello G. How Older Adults Cope with Cognitive Complexity and Environmental Constraints during Dual-Task Walking: The Role of Executive Function Involvement. International Journal of Environmental Research and Public Health. 2019; 16(10):1835. https://doi.org/10.3390/ijerph16101835
Chicago/Turabian StyleForte, Roberta, Caterina Pesce, Angela Di Baldassarre, John Shea, Claudia Voelcker-Rehage, Laura Capranica, and Giancarlo Condello. 2019. "How Older Adults Cope with Cognitive Complexity and Environmental Constraints during Dual-Task Walking: The Role of Executive Function Involvement" International Journal of Environmental Research and Public Health 16, no. 10: 1835. https://doi.org/10.3390/ijerph16101835
APA StyleForte, R., Pesce, C., Di Baldassarre, A., Shea, J., Voelcker-Rehage, C., Capranica, L., & Condello, G. (2019). How Older Adults Cope with Cognitive Complexity and Environmental Constraints during Dual-Task Walking: The Role of Executive Function Involvement. International Journal of Environmental Research and Public Health, 16(10), 1835. https://doi.org/10.3390/ijerph16101835








