Multi-Morbid Health Profiles and Specialty Healthcare Service Use: A Moderating Role of Poverty
Abstract
1. Introduction
- (1)
- What are the patterns of multi-morbidity (physical, mental, and substance/alcohol problems) among older adults in the United States? We expect to identify several heterogeneous groups based on their physical, mental, and behavioral health conditions.
- (2)
- What is the relationship between older adults’ multi-morbid health profiles and the patterns of use of specialty healthcare services? It is hypothesized that older adults with mental or behavioral health problems use more mental health and/or substance use services.
- (3)
- To what extent does poverty moderate the relationship between health profiles and patterns of specialty health service use? It is expected that those living in poverty have limited access to healthcare treatments despite their mental or behavioral problems.
2. Materials and Methods
2.1. Data and Sample
2.2. Measures
2.3. Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Centers for Medicare & Medicaid Services [CMS]. Chronic Conditions among Medicare Beneficiaries; CMS: Baltimore, MD, USA, 2012.
- De Nardi, M.; French, E.; Jones, J.B.; McCauley, J. Medical spending of the US elderly. Fisc. Stud. 2016, 37, 717–747. [Google Scholar] [CrossRef]
- Ward, B.W.; Schiller, J.S.; Goodman, R.A. Multiple chronic conditions among US adults: A 2012 update. Prev. Chronic Dis. 2014, 11, E62. [Google Scholar] [CrossRef] [PubMed]
- Jindai, K.; Nielson, C.M.; Vorderstrasse, B.A.; Quiñones, A.R. Multimorbidity and Functional Limitations among Adults 65 or Older, NHANES 2005–2012. Prev. Chronic Dis. 2016, 13, E151. [Google Scholar] [CrossRef]
- Hajat, C.; Stein, E.; Yach, D. Multiple Chronic Conditions: The Global State. 2017. Available online: http://www.tevapharm.com/files/docs/Teva_MCC_Report.pdf (accessed on 19 April 2019).
- Marengoni, A.; Angleman, S.; Melis, R.; Mangialasche, F.; Karp, A.; Garmen, A.; Meinow, B.; Fratiglioni, L. Aging with multimorbidity: A systematic review of the literature. Ageing Res. Rev. 2011, 10, 430–439. [Google Scholar] [CrossRef] [PubMed]
- Lapierre, S.; Erlangsen, A.; Waern, M.; De Leo, D.; Oyama, H.; Scocco, P.; Gallo, J.; Szanto, K.; Conwell, Y.; Draper, B.; et al. A systematic review of elderly suicide prevention programs. Crisis 2011, 32, 88–89. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention [CDC]. Health, United States, 2013: In Brief; CDC: Hyattsville, MD, USA, 2014.
- Babatunde, O.T.; Outlaw, K.R.; Forbes, B.; Gay, T. Revisiting baby boomers and alcohol use: Emerging treatment trends. J. Hum. Behav. Soc. Environ. 2014, 24, 597–611. [Google Scholar] [CrossRef]
- National Institute on Aging. Facts about Aging and Alcohol. Available online: https://www.nia.nih.gov/health/facts-about-aging-and-alcohol (accessed on 19 April 2019).
- Barnett, K.; Mercer, S.W.; Norbury, M.; Watt, G.; Wyke, S.; Guthrie, B. Epidemiology of multimorbidity and implications for healthcare, research, and medical education: A cross-sectional study. Lancet 2012, 380, 37–43. [Google Scholar] [CrossRef]
- Lin, W.C.; Zhang, J.; Leung, G.Y.; Clark, R.E. Chronic physical conditions in older adults with mental illness and/or substance use disorders. J. Am. Geriatr. Soc. 2011, 59, 1913–1921. [Google Scholar] [CrossRef]
- Choi, N.G.; DiNitto, D.M.; Marti, C.N. Alcohol and other substance use, mental health treatment use, and perceived unmet treatment need: Comparison between baby boomers and older adults. Am. J. Addict. 2015, 24, 299–307. [Google Scholar] [CrossRef] [PubMed]
- Salmon, J.M.; Forester, B. Substance abuse and co-occurring psychiatric disorders in older adults: A clinical case and review of the relevant literature. J. Dual Diagn. 2012, 8, 74–84. [Google Scholar] [CrossRef]
- Substance Abuse and Mental Health Services Administration [SAMHSA]. Results from the 2010 National Survey on Drug Use and Health: Mental Health Findings; NSDUH Series H-42, HHS Publication No (SMA), 11-4667; Substance Abuse and Mental Health Services Administration: Rockville, MD, USA, 2012.
- Menninger, J.A. Assessment and treatment of alcoholism and substance-related disorders in the elderly. Bull. Menn. Clin. 2002, 66, 166–183. [Google Scholar] [CrossRef]
- Schüz, B.; Wurm, S.; Warner, L.M.; Tesch-Römer, C. Health and subjective well-being in later adulthood: Different health states—Different needs? Appl. Psychol. Health Well Being 2009, 1, 23–45. [Google Scholar] [CrossRef]
- Lafortune, L.; Beland, F.; Bergman, H.; Ankri, J. Health state profiles and service utilization in community-living elderly. Med. Care 2009, 47, 286–294. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.F.; Tian, W.H.; Yao, H.P. The heterogeneous health latent classes of elderly people and their socio-demographic characteristics in Taiwan. Arch. Gerontol. Geriatr. 2014, 58, 205–213. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Smith, J.; Dunkle, R.E.; Ingersoll-Dayton, B.; Antonucci, T.C. Health and social-physical environment profiles among older adults living alone: Associations with depressive symptoms. J. Gerontol. B Psychol. Sci. Soc. Sci. 2019, 74, 675–684. [Google Scholar] [CrossRef]
- Mackenzie, C.S.; Gekoski, W.L.; Knox, V.J. Age, gender, and the underutilization of mental health services: The influence of help-seeking attitudes. Aging Ment. Health 2006, 10, 574–582. [Google Scholar] [CrossRef]
- Woodward, A.T. A latent class analysis of age differences in choosing service providers to treat mental and substance use disorders. Psychiatr. Serv. 2013, 64, 1087–1094. [Google Scholar] [CrossRef]
- Park-Lee, E.; Lipari, R.N.; Hedden, S.L.; Kroutil, L.A.; Porter, J.D. Receipt of Services for Substance Use and Mental Health Issues among Adults: Results from the 2016 National Survey on Drug Use and Health; Substance Abuse and Mental Health Services Administration: Rockville, MD, USA, 2017.
- Kessler, R.C.; Berglund, P.; Demler, O.; Jin, R.; Merikangas, K.R.; Walters, E.E. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication (NCS-R). Arch. Gen. Psychiatry 2005, 62, 593–602. [Google Scholar] [CrossRef]
- Addis, M.E.; Mahalik, J.R. Men, masculinity, and the contexts of help seeking. Am. Psychol. 2003, 58, 5–14. [Google Scholar] [CrossRef]
- Uebelacker, L.A.; Wang, P.S.; Berglund, P.; Kessler, R.C. Clinical differences among patients treated for mental health problems in general medical and specialty mental health settings in the National Comorbidity Survey Replication (NCS-R). Gen. Hosp. Psychiatry 2006, 28, 387–395. [Google Scholar] [CrossRef]
- Jimenez, D.E.; Cook, B.; Bartels, S.J.; Alegría, M. Disparities in mental health service use of racial and ethnic minority elderly adults. J. Am. Geriatr. Soc. 2013, 61, 18–25. [Google Scholar] [CrossRef]
- Ojeda, V.D.; Bergstresser, S.A. Gender, race-ethnicity, and psychosocial barriers to mental healthcare: An examination of perceptions and attitudes among adults reporting unmet need. J. Health Soc. Behav. 2009, 49, 317–334. [Google Scholar] [CrossRef] [PubMed]
- Nelson, C.H.; Park, J. The nature and correlates of unmet healthcare needs in Ontario, Canada. Soc. Sci. Med. 2006, 62, 2291–2300. [Google Scholar] [CrossRef]
- Steele, L.; Dewa, C.; Lee, K. Socioeconomic status and self-reported barriers to mental health service use. Can. J. Psychiatry 2007, 52, 201–206. [Google Scholar] [CrossRef]
- Choi, N.G.; DiNitto, D.M.; Marti, C.N. Treatment use, perceived need, and barriers to seeking treatment for substance abuse and mental health problems among older adults compared to younger adults. Drug Alcohol Depend. 2014, 145, 113–120. [Google Scholar] [CrossRef]
- Gum, A.M.; Iser, L.; Petkus, A. Behavioral health service utilization and preferences of older adults receiving home-based aging services. Am. J. Geriatr. Psychiatry 2010, 18, 491–501. [Google Scholar] [CrossRef] [PubMed]
- Friedman, B.; Jiang, H.J.; Elixhauser, A.; Segal, A. Hospital inpatient costs for adults with multiple chronic conditions. Med. Care Res. Rev. 2006, 63, 327–346. [Google Scholar] [CrossRef]
- Gerteis, J.; Izrael, D.; Deitz, D.; LeRoy, L.; Ricciardi, R.; Miller, T.; Basu, J. Multiple Chronic Conditions Chartbook. 2014. Available online: https://www.ahrq.gov/sites/default/files/wysiwyg/professionals/prevention-chronic-care/decision/mcc/mccchartbook.pdf (accessed on 19 April 2019).
- Paez, K.A.; Zhao, L.; Hwang, W. Rising out-of-pocket spending for chronic conditions: A ten-year trend. Health Aff. 2009, 28, 15–25. [Google Scholar] [CrossRef]
- Kim, J.L.; Cho, J.; Park, S.; Park, E.C. Depression symptom and professional mental health service use. BMC Psychiatry 2015, 15, 261. [Google Scholar] [CrossRef]
- Andersen, R.M. Revisiting the behavioral model and access to medical care: Does it matter? J. Health Soc. Behav. 1995, 36, 1–10. [Google Scholar] [CrossRef]
- Pearlin, L.I. The life course and the stress process: Some conceptual comparisons. J. Gerontol. B Psychol. Sci. Soc. Sci. 2010, 65B, 207–215. [Google Scholar] [CrossRef]
- Ferraro, K.F.; Shippee, T.P.; Schafer, M.H. Cumulative inequality theory for research on aging and the life course. In Handbook of Theories of Aging, 2nd ed.; Bengtson, V.L., Gans, D., Putney, N.M., Silverstein, M., Eds.; Springer: New York, NY, USA, 2009; pp. 413–433. [Google Scholar]
- Hedden, S.; Gfroerer, J.; Barker, P.; Smith, S.; Pemberton, M.R.; Saavedra, L.M.; Forman-Hoffmann, V.L.; Ringeisen, H.; Novak, S.P. Comparison of NSDUH Mental Health Data and Methods with Other Data Sources; Substance Abuse and Mental Health Services Administration: Rockville, MD, USA, 2012.
- US Department of Health and Human Services. Multiple Chronic Conditions-A Strategic Framework: Optimum Health and Quality of Life for Individuals with Multiple Chronic Conditions; US Department of Health and Human Services: Washington, DC, USA, 2010.
- Üstün, T.B.; Kostanjsek, N.; Chatterji, S.; Rehm, J. Measuring Health and Disability: Manual for WHO Disability Assessment Schedule (WHODAS 2.0); World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Kessler, R.C.; Barker, P.R.; Colpe, L.J.; Epstein, J.F.; Gfroerer, J.C.; Hiripi, E.; Howes, M.J.; Normand, S.L.; Mandersheid, R.W.; Walters, E.E.; et al. Screening for serious mental illness in the general population. Arch. Gen. Psychiatry 2003, 60, 184–189. [Google Scholar] [CrossRef]
- Frohlich, L.; Swenson, K.; Wolf, S.; Mccartney, S.; Hauan, S. Financial Condition and Healthcare Burdens of People in Deep Poverty. Available online: https://aspe.hhs.gov/basic-report/financial-condition-and-health-care-burdens-people-deep-poverty (accessed on 19 April 2019).
- Kwon, E.; Park, S.; McBride, T.D. Health insurance and poverty in trajectories of out-of-pocket expenditure among low-income middle-aged adults. Health Serv. Res. 2018, 53, 4332–4352. [Google Scholar] [CrossRef]
- Center for Behavioral Health Statistics and Quality. 2013 National Survey on Drug Use and Health Public Use File Codebook; Substance Abuse and Mental Health Service Administration [SAMHSA]: Rockville, MD, USA, 2014.
- Collins, L.M.; Lanza, S.T. Latent Class and Latent Transition Analysis: With Applications in the Social, Behavioral, and Health Sciences; John Wiley & Sons: Hoboken, NJ, USA, 2010. [Google Scholar]
- Muthén, L.K.; Muthén, B.O. Mplus User’s Guide, 7th ed.; Muthén & Muthén: Los Angeles, CA, USA, 2012. [Google Scholar]
- Starkweather, J.; Moske, A.K. Multinomial Logistic Regression. Available online: http://www.unt.edu/rss/class/Jon/Benchmarks/MLR_JDS_Aug2011.pdf (accessed on 19 April 2019).
- Thorpe, J.M.; Thorpe, C.T.; Kennelty, K.A.; Pandhi, N. Patterns of perceived barriers to medical care in older adults: A latent class analysis. BMC Health Serv. Res. 2011, 11, 181. [Google Scholar] [CrossRef]
- Lanza, S.T.; Rhoades, B.L. Latent class analysis: An alternative perspective on subgroup analysis in prevention and treatment. Prev. Sci. 2013, 14, 157–168. [Google Scholar] [CrossRef]
- North, C.S.; Brown, E.S.; Pollio, D.E. E Expanded conceptualization of multimorbidity to encompass substance use disorders and other psychiatric illness. Ann. Clin. Psychiatry 2016, 28, 182–188. [Google Scholar] [PubMed]
- Han, B.H.L.; Moore, A.A.; Sherman, S.E.; Palamar, J.J. Prevalence and correlates of binge drinking among older adults with multimorbidity. Drug Alcohol Depend. 2018, 187, 48–54. [Google Scholar] [CrossRef] [PubMed]
- Galenkamp, H.; Braam, A.W.; Huisman, M.; Deeg, D.J. Somatic multimorbidity and self-rated health in the older population. J. Gerontol. B Psychol. Sci. Soc. Sci. 2011, 66, 380–386. [Google Scholar] [CrossRef]
- Kadam, U.T.; Croft, P.R. Clinical multimorbidity and physical function in older adults: A record and health status linkage study in general practice. Fam. Pract. 2007, 24, 412–419. [Google Scholar] [CrossRef] [PubMed]
- Newman, A.B.; Boudreau, R.M.; Naydeck, B.L.; Fried, L.F.; Harris, T.B. A physiologic index of comorbidity: Relationship to mortality and disability. J. Gerontol. A Biol. Sci. Med. Sci. 2008, 63, 603–609. [Google Scholar] [CrossRef]
- Scott, K.M.; Von Korff, M.; Alonso, J.; Angermeyer, M.; Bromet, E.J.; Bruffaerts, R.; de Girolamo, G.; de Graaf, R.; Fernandez, A.; Gureje, O.; et al. Age patterns in the prevalence of DSM-IV depressive/anxiety disorders with and without physical co-morbidity. Psychol. Med. 2008, 38, 1659–1669. [Google Scholar] [CrossRef]
- Naylor, C.; Parsonage, M.; McDaid, D.; Knapp, M.; Fossey, M.; Galea, A. Long-Term Conditions and Mental Health: The Cost of Co-Morbidities; The King’s Fund: London, UK, 2012. [Google Scholar]
- Blazer, D.G.; Wu, L.T. The epidemiology of at-risk and binge drinking among middle-aged and elderly community adults: National Survey on Drug Use and Health. Am. J. Psychiatry 2009, 166, 1162–1169. [Google Scholar] [CrossRef] [PubMed]
- Fiske, A.; Wetherell, J.L.; Gatz, M. Depression in older adults. Annu. Rev. Clin. Psychol. 2008, 5, 363–389. [Google Scholar] [CrossRef]
- Kuerbis, A.; Sacco, P.; Blazer, D.G.; Moore, A.A. Substance abuse among older adults. Clin. Geriatr. Med. 2014, 30, 629–654. [Google Scholar] [CrossRef]
- Roll, J.M.; Kennedy, J.; Tran, M.; Howell, D. Disparities in unmet need for mental health services in the United States, 1997–2010. Psychiatr. Serv. 2013, 64, 80–82. [Google Scholar] [CrossRef] [PubMed]
- Keyes, C.L. Promoting and protecting mental health as flourishing: A complementary strategy for improving national mental health. Am. Psychol. 2007, 62, 95–108. [Google Scholar] [CrossRef]
- Prince, M.; Patel, V.; Saxena, S.; Maj, M.; Maselko, J.; Phillips, M.R.; Rahman, A. No health without mental health. Lancet 2007, 370, 859–877. [Google Scholar] [CrossRef]
- Gould, C.E.; O’Hara, R.; Goldstein, M.K.; Beaudreau, S.A. Multimorbidity is associated with anxiety in older adults in the health and retirement study. Int. J. Geriatr. Psychiatry 2013, 31, 1105–1115. [Google Scholar] [CrossRef] [PubMed]
- Lynch, J.W.; Kaplan, G.A.; Shema, S.J. Cumulative impact of sustained economic hardship on physical, cognitive, psychological, and social functioning. N. Engl. J. Med. 1997, 337, 1889–1895. [Google Scholar] [CrossRef] [PubMed]
- Muntaner, C.; Eaton, W.W.; Diala, C.; Kessler, R.C.; Sorlie, P.D. Social class, assets, organizational control and the prevalence of common groups of psychiatric disorders. Soc. Sci. Med. 1998, 47, 2043–2053. [Google Scholar] [CrossRef]
- Lorant, V.; Deliège, D.; Eaton, W.; Robert, A.; Philippot, P.; Ansseau, M. Socioeconomic inequalities in depression: A meta-analysis. Am. J. Epidemiol. 2003, 157, 98–112. [Google Scholar] [CrossRef] [PubMed]
- Morello-Frosch, R.; Zuk, M.; Jerrett, M.; Shamasunder, B.; Kyle, A.D. Understanding the cumulative impacts of inequalities in environmental health: Implications for policy. Health Aff. 2011, 30, 879–887. [Google Scholar] [CrossRef] [PubMed]
- Chow, J.C.; Jaffee, K.; Snowden, L. Racial/ethnic disparities in the use of mental health services in poverty areas. Am. J. Public Health 2003, 93, 792–797. [Google Scholar] [CrossRef]
- Baird, K.E. Recent trends in the probability of high out-of-pocket medical expenses in the United States. SAGE Open Med. 2016, 4. [Google Scholar] [CrossRef]
- Sommers, B.D.; Oellerich, D. The poverty-reducing effect of Medicaid. J. Health Econ. 2013, 32, 816–832. [Google Scholar] [CrossRef]
- Wilson, M.G.; Lavis, J.N.; Gauvin, F.P. Designing integrated approaches to support people with multimorbidity: Key messages from systematic reviews, health system leaders and citizens. Healthc. Policy 2016, 12, 91–104. [Google Scholar] [CrossRef][Green Version]
- Yao, L.; Robert, S.A. The contributions of race, individual socioeconomic status, and neighborhood socioeconomic context on the self-rated health trajectories and mortality of older adults. Res. Aging 2008, 30, 251–273. [Google Scholar] [CrossRef]
- Gellert, P.; von Berenberg, P.; Zahn, T.; Neuwirth, J.; Kuhlmey, A.; Dräger, D. Multimorbidity profiles in German centenarians: A latent class analysis of health insurance data. J. Aging Health 2017. [Google Scholar] [CrossRef]
- Reiss-Brennan, B. Mental health integration: Normalizing team care. J. Prim. Care Community Health 2014, 5, 55–60. [Google Scholar] [CrossRef] [PubMed]
- Gum, A.M.; Schonfeld, L.; Tyler, S.; Fishleder, S.; Guerra, L. One-visit behavioral intervention for older primary care patients with mild to moderate depressive symptoms. South. Med. J. 2016, 109, 442–447. [Google Scholar] [CrossRef]
- Reiss-Brennan, B.; Brunisholz, K.D.; Dredge, C.; Briot, P.; Grazier, K.; Wilcox, A.; Savitz, L.; James, B. Association of integrated team-based care with healthcare quality, utilization, and cost. JAMA 2016, 316, 826–834. [Google Scholar] [CrossRef] [PubMed]
- King, D.E.; Matheson, E.; Chirina, S.; Shankar, A.; Broman-Fulks, J. The status of baby boomers’ health in the United States: The healthiest generation? JAMA Intern. Med. 2013, 173, 385–386. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez, J.M.; Alegria, M.; Prihoda, T.J.; Copeland, L.A.; Zeber, J.E. How the relationship of attitudes toward mental health treatment and service use differs by age, gender, ethnicity/race and education. Soc. Psychiatry Psychiatr. Epidemiol. 2011, 46, 45–57. [Google Scholar] [CrossRef] [PubMed]
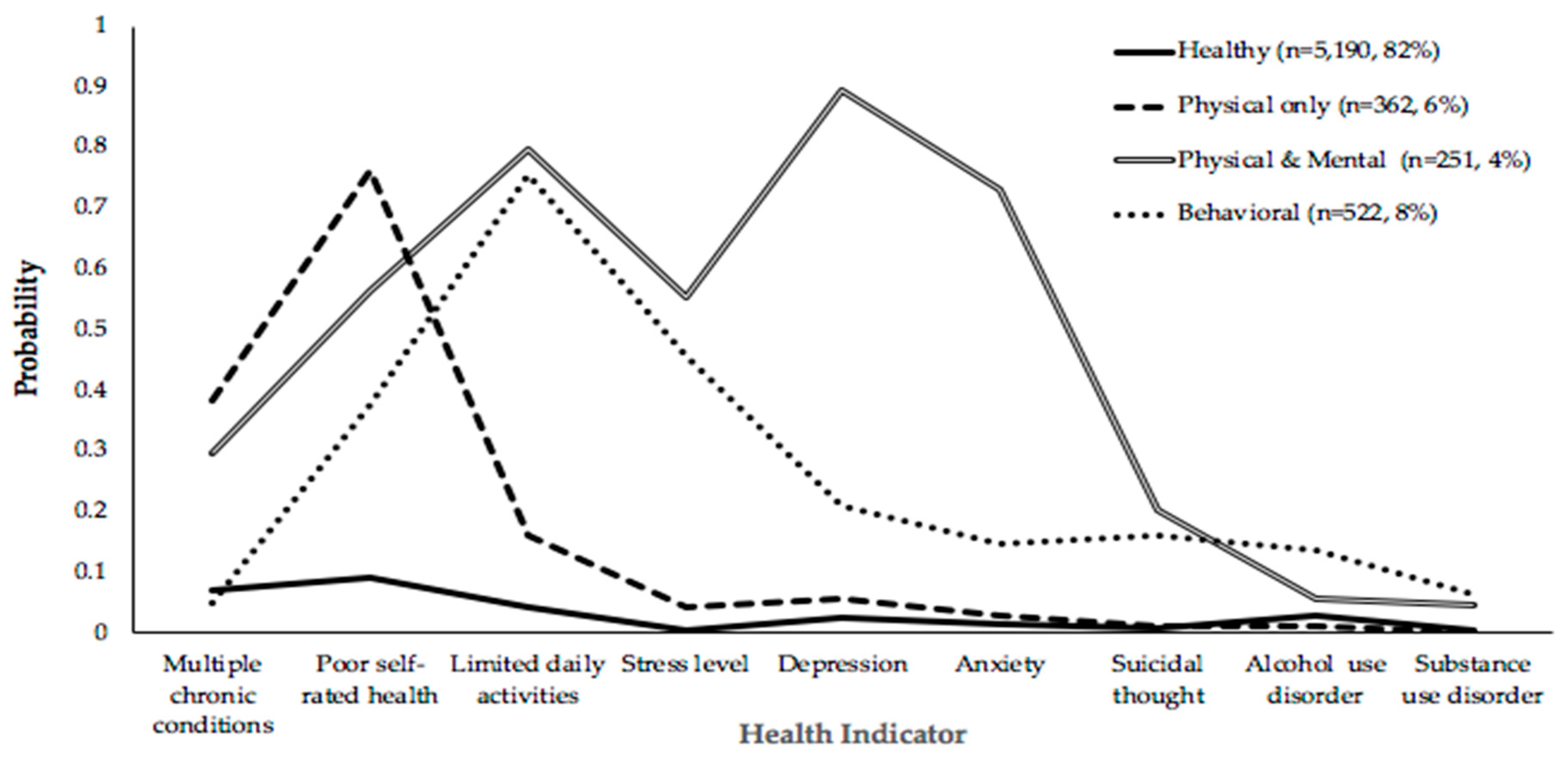
| Class 2 | Class 3 | Class 4 | Class 5 | |||||
|---|---|---|---|---|---|---|---|---|
| BIC | 27,868.128 | 27,789.460 | 27,736.929 | 27,743.495 | ||||
| Entropy | 0.86 | 0.92 | 0.76 | 0.79 | ||||
| LMR LR test (p value) | <0.001 | <0.001 | 0.001 | 0.004 | ||||
| Class Counts and Proportions | 740 | 0.12 | 671 | 0.11 | 251 | 0.04 | 172 | 0.03 |
| 5585 | 0.88 | 671 | 0.11 | 5190 | 0.82 | 356 | 0.06 | |
| 1004 | 0.16 | 522 | 0.08 | 5183 | 0.82 | |||
| 362 | 0.06 | 253 | 0.04 | |||||
| 361 | 0.06 | |||||||
| Physical Only | Physical and Mental | Behavioral | |||||||
|---|---|---|---|---|---|---|---|---|---|
| RRR | 95% Cl | p | RRR | 95% Cl | p | RRR | 95% Cl | p | |
| Age group (ref: 50–64) | |||||||||
| 65 and over | 0.26 | [0.19, 0.37] | <0.001 | 0.41 | [0.33, 0.51] | <0.001 | 1.48 | [1.17, 1.87] | 0.001 |
| Race (ref: White) | |||||||||
| Black | 0.18 | [0.09, 0.37] | <0.001 | 0.76 | [0.56, 1.03] | 0.076 | 1.61 | [1.18, 2.18] | 0.002 |
| Hispanic | 0.91 | [0.59, 1.42] | 0.685 | 0.75 | [0.53, 1.06] | 0.109 | 1.15 | [0.80, 1.66] | 0.456 |
| Other | 1.24 | [0.69, 2.24] | 0.468 | 1.59 | [1.04, 2.42] | 0.030 | 1.63 | [0.99, 2.70] | 0.056 |
| Gender (ref: Male) | |||||||||
| Female | 1.83 | [1.38, 2.41] | <0.001 | 1.34 | [1.11, 1.62] | 0.003 | 1.07 | [0.85, 1.33] | 0.573 |
| Marital status (ref: Others) | |||||||||
| Married | 0.40 | [0.29, 0.56] | <0.001 | 0.48 | [0.38, 0.62] | <0.001 | 0.64 | [0.49, 0.84] | 0.001 |
| Education (ref: Less than high school) | |||||||||
| High school | 0.83 | [0.54, 1.27] | 0.388 | 0.75 | [0.57, 0.99] | 0.045 | 0.62 | [0.46, 0.84] | 0.002 |
| College | 1.01 | [0.65, 1.55] | 0.978 | 0.60 | [0.44, 0.81] | 0.001 | 0.70 | [0.51, 0.96] | 0.029 |
| Above college | 0.78 | [0.49, 1.23] | 0.282 | 0.60 | [0.44, 0.82] | 0.002 | 0.33 | [0.22, 0.48] | <0.001 |
| Insurance (ref: Not covered) | |||||||||
| Covered | 0.39 | [0.23, 0.65] | <0.001 | 0.69 | [0.51, 0.96] | 0.025 | 0.90 | [0.60, 1.35] | 0.605 |
| Poverty (ref: Not in poverty) | |||||||||
| In poverty | 3.15 | [2.19, 4.52] | <0.001 | 2.10 | [1.16, 2.74] | <0.001 | 1.69 | [1.23, 2.30] | 0.001 |
| Household composition (ref: Living alone) | |||||||||
| Living with other family members | 1.49 | [1.05, 2.12] | 0.025 | 1.02 | [0.80, 1.31] | 0.864 | 1.43 | [1.06, 1.95] | 0.020 |
| Constant | 0.73 | [0.08, 0.36] | 0.31 | [0.19, 0.51] | 0.09 | [0.05, 0.16] | |||
| Mental Health Treatment | Substance Use Treatment | Both Treatments | |||||||
|---|---|---|---|---|---|---|---|---|---|
| RRR | 95% Cl | p | RRR | 95% Cl | p | RRR | 95% Cl | p | |
| Health condition profiles (ref: Healthy) | |||||||||
| Physical and mental health problem | 88.55 | [53.37, 146.9] | <0.001 | 3.01 | [0.87, 10.47] | 0.083 | 249.41 | [118.4, 525.3] | <0.001 |
| Behavioral health problem | 13.43 | [10.42, 17.33] | <0.001 | 3.56 | [2.30, 5.52] | <0.001 | 40.42 | [22.94, 71.24] | <0.001 |
| Physical health problem | 3.21 | [2.27, 4.53] | <0.001 | 1.08 | [0.57, 2.05] | 0.815 | 5.79 | [2.30, 14.59] | <0.001 |
| Age group (ref: 50–64) | |||||||||
| 65 and over | 0.53 | [0.44, 0.64] | <0.001 | 0.42 | [0.31, 0.57] | <0.001 | 0.43 | [0.26, 0.71] | 0.001 |
| Race (ref: White) | |||||||||
| Black | 0.39 | [0.28, 0.55] | <0.001 | 1.03 | [0.71, 1.50] | 0.872 | 1.01 | [0.56, 1.83] | 0.970 |
| Hispanic | 0.35 | [0.24, 0.52] | <0.001 | 0.69 | [0.42, 1.14] | 0.146 | 0.69 | [0.35, 1.36] | 0.286 |
| Other | 0.55 | [0.44, 0.64] | 0.015 | 1.22 | [0.66, 2.24] | 0.523 | 1.50 | [0.70, 3.21] | 0.294 |
| Gender (ref: Male) | |||||||||
| Female | 1.85 | [1.54, 2.22] | <0.001 | 0.24 | [0.18, 0.32] | <0.001 | 0.71 | [0.48, 1.04] | 0.081 |
| Marital status (ref: Others) | |||||||||
| Married | 0.96 | [0.76, 1.22] | 0.738 | 0.42 | [0.30, 0.58] | <0.001 | 0.79 | [0.48, 1.31] | 0.364 |
| Education (ref: Less than high school) | |||||||||
| High school | 1.04 | [0.77, 1.41] | 0.807 | 1.03 | [0.70, 1.51] | 0.899 | 0.84 | [0.46, 1.54] | 0.581 |
| College | 1.30 | [0.95, 1.78] | 0.102 | 0.99 | [0.66, 1.49] | 0.959 | 1.62 | [0.90, 2.92] | 0.111 |
| Above college | 1.80 | [1.31, 2.46] | <0.001 | 0.59 | [0.37, 0.93] | 0.023 | 1.25 | [0.65, 2.41] | 0.504 |
| Insurance (ref: Not covered) | |||||||||
| Covered | 0.47 | [0.32, 0.68] | <0.001 | 0.77 | [0.51, 1.16] | 0.203 | 0.74 | [0.39, 1.39] | 0.349 |
| Poverty (ref: Not in poverty) | |||||||||
| In poverty | 1.62 | [1.08, 2.42] | 0.020 | 1.31 | [0.85, 2.03] | 0.219 | 3.86 | [1.62, 9.19] | 0.002 |
| Household composition (ref: Living alone) | |||||||||
| Living with other family members | 0.79 | [0.61, 1.02] | 0.077 | 0.78 | [0.56, 1.09] | 0.151 | 0.56 | [0.34, 0.92] | 0.022 |
| Interaction effect (ref: Not in poverty × healthy group) | |||||||||
| Poverty × Physical and mental health problem | 0.46 | [0.17, 1.24] | 0.126 | - | - | 1.000 | 0.20 | [0.05, 0.80] | 0.023 |
| Poverty × Behavior health problem | 0.66 | [0.35, 1.23] | 0.194 | 0.65 | [0.26, 1.61] | 0.351 | 0.31 | [0.11, 0.93] | 0.037 |
| Poverty × Physical health problem | 0.33 | [0.12, 0.90] | 0.030 | 0.66 | [0,16, 2.67] | 0.559 | 0.13 | [0.01, 1.31] | 0.083 |
| Constant | 0.18 | [0.10, 0.30] | 0.31 | [0.16, 0.59] | 0.02 | [0.01, 0.05] | |||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kwon, I.; Shin, O.; Park, S.; Kwon, G. Multi-Morbid Health Profiles and Specialty Healthcare Service Use: A Moderating Role of Poverty. Int. J. Environ. Res. Public Health 2019, 16, 1956. https://doi.org/10.3390/ijerph16111956
Kwon I, Shin O, Park S, Kwon G. Multi-Morbid Health Profiles and Specialty Healthcare Service Use: A Moderating Role of Poverty. International Journal of Environmental Research and Public Health. 2019; 16(11):1956. https://doi.org/10.3390/ijerph16111956
Chicago/Turabian StyleKwon, Ilan, Oejin Shin, Sojung Park, and Goeun Kwon. 2019. "Multi-Morbid Health Profiles and Specialty Healthcare Service Use: A Moderating Role of Poverty" International Journal of Environmental Research and Public Health 16, no. 11: 1956. https://doi.org/10.3390/ijerph16111956
APA StyleKwon, I., Shin, O., Park, S., & Kwon, G. (2019). Multi-Morbid Health Profiles and Specialty Healthcare Service Use: A Moderating Role of Poverty. International Journal of Environmental Research and Public Health, 16(11), 1956. https://doi.org/10.3390/ijerph16111956





