Understanding the Increase in Life Expectancy in Hong Kong: Contributions of Changes in Age- and Cause-Specific Mortality
Abstract
1. Introduction
2. Materials and Methods
3. Results
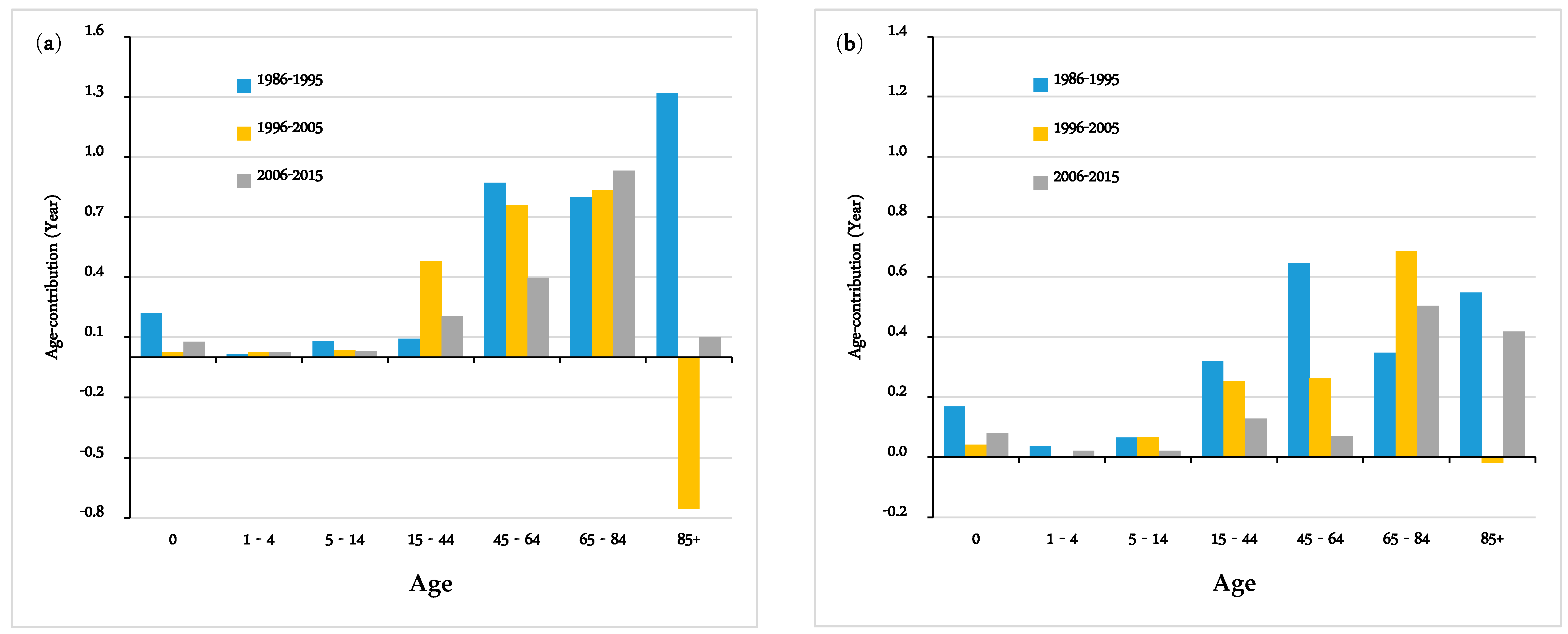
3.1. Contributions of Mortality Change by Age Group
3.2. Contributions of Mortality Change by Causes of Death
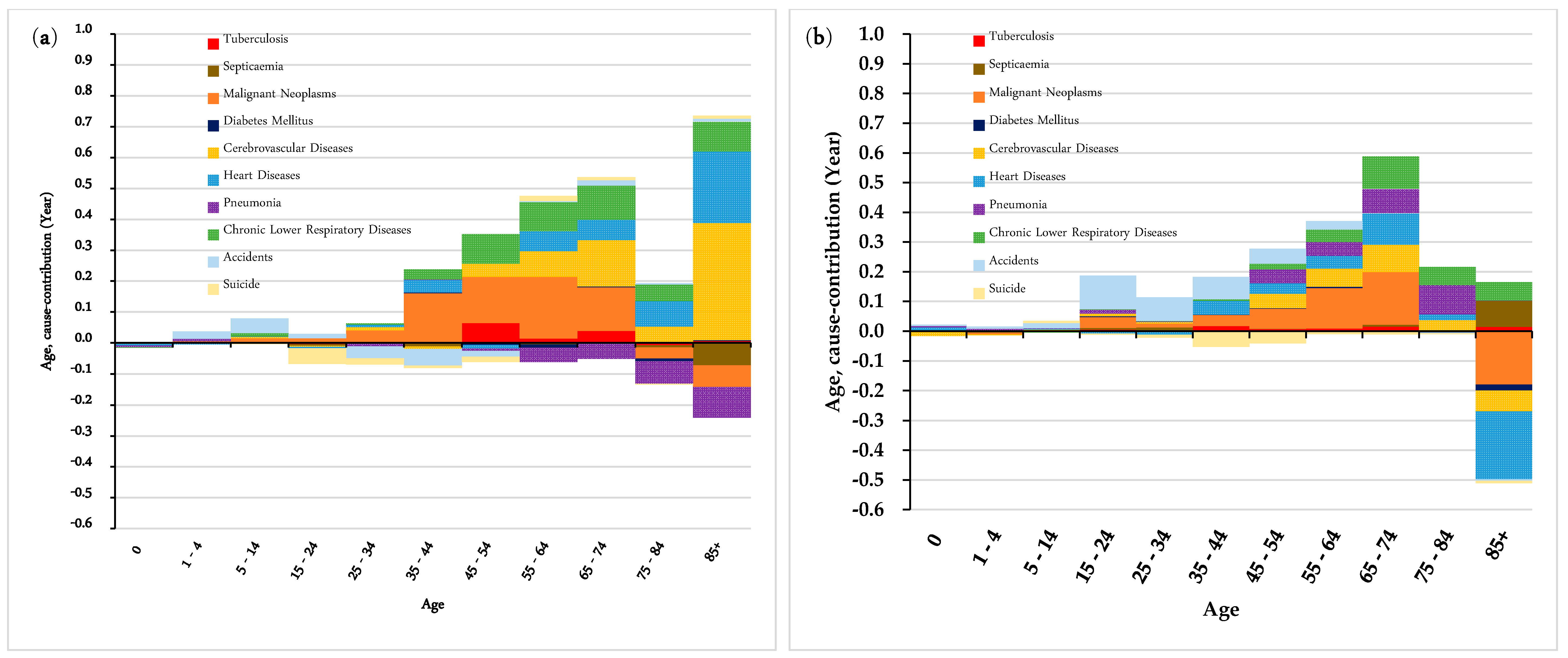
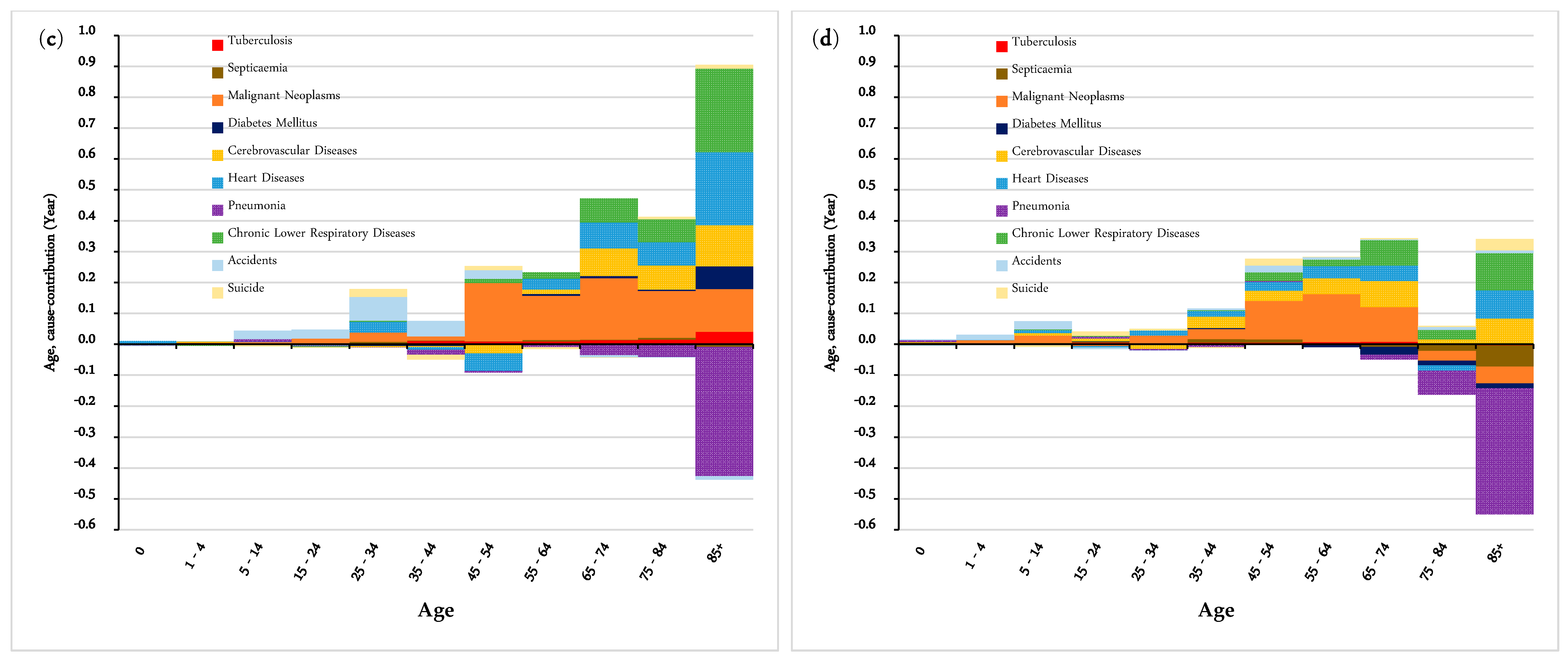
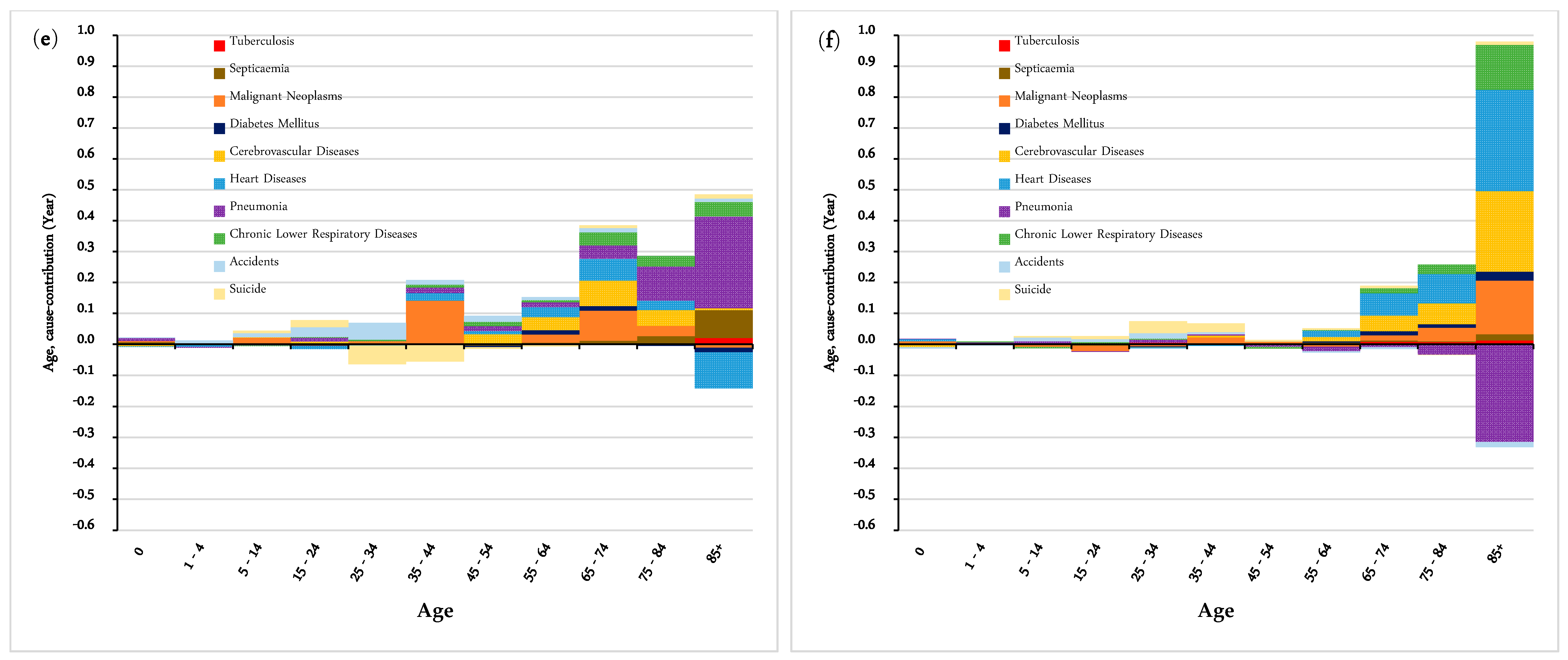
3.3. Contributions of Mortality Change by Age and Causes of Death
4. Discussion
5. Conclusions and Future Work
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A

Appendix B
| Causes of Death | ICD 9 | ICD 10 | ICD Update |
|---|---|---|---|
| (1986–2000) | (2001–2009) | (2010 Onwards) | |
| Infectious Diseases | 001–139 | A00–B99 | A00–B99 |
| Tuberculosis | 010–018, 137 | A15–A19, B90 | A15–A19, B90 |
| Septicemia | 38 | A40–A41 | A40–A41 |
| Malignant neoplasms | 140–208 | C00–C97 | C00–C97 |
| Endocrine Diseases | 240–278 | E00–E89 | E00–E89 |
| Diabetes Mellitus | 250 | E10–E14 | E10–E14 |
| Circulatory Diseases | 390–459 | I00–I97, I99 | I00–I97, I99 |
| Cerebrovascular diseases | 430–438 | I60–I69 | I60–I69 |
| Heart Diseases | |||
| Respiratory Diseases | 460–519 | J00–J98 | J00–J98 |
| Pneumonia | 480–486 | J12–J18 | J12–J18 |
| Chronic Lower Respiratory Diseases | 490–494,496 | J40–J47 | J40–J47 |
| Digestive Diseases | 520–579 | K00–K92 | K00–K92 |
| Genitourinary Diseases | 580–629 | N00–N99 | N00–N99 |
| External Causes | E800–E999 | V01–Y89 | V01–Y89 |
| Accidents | E800–E949 | V01–X59 | V01–X59 |
| Y40–Y86 | Y40–Y86 | ||
| Y88–Y89 | Y88–Y89 | ||
| Suicide | E950–E959 | X60–X84 | X60–X84 |
References
- Zhang, Z.; Yu, H.; Wang, C. Differences in life expectancy between household and non-household populations in Shanghai, 2000–2010. Chin. J. Popul. Sci. 2015, 23–34. [Google Scholar]
- Hiam, L.; Harrison, D.; McKee, M.; Dorling, D. Why is life expectancy in England and Wales ‘stalling’? J. Epidemiol. Community Health 2018, 72, 404–408. [Google Scholar] [CrossRef]
- Vaupel, J.W. How change in age-specific mortality affects life expectancy. Popul. Stud. 1986, 40, 147–157. [Google Scholar] [CrossRef] [PubMed]
- Conti, S.; Farchi, G.; Masocco, M.; Toccaceli, V.; Vichi, M. The impact of the major causes of death on life expectancy in Italy. Int. J. Epidemiol. 1999, 28, 905–910. [Google Scholar] [CrossRef] [PubMed]
- Shkolnikov, V.; McKee, M.; Leon, D.A. Changes in life expectancy in Russia in the mid-1990s. Lancet 2001, 357, 917–921. [Google Scholar] [CrossRef]
- Gómez-Redondo, R.; Boe, C. Decomposition analysis of Spanish life expectancy at birth: Evolution and changes in the components by sex and age. Demogr. Res. 2005, 13, 521–546. [Google Scholar] [CrossRef]
- Klenk, J.; Rapp, K.; Büchele, G.; Keil, U.; Weiland, S.K. Increasing life expectancy in Germany: Quantitative contributions from changes in age-and disease-specific mortality. Eur. J. Public Health 2007, 17, 587–592. [Google Scholar] [CrossRef]
- HKCSD. Women and Men in Hong Kong Key Statistics 2018; Census and Statistics Department, HKSAR Government: Hong Kong, China, 2018.
- Law, C.K.; Yip, P.S.F. Healthy life expectancy in Hong Kong special administrative region of China. Bull. World Health Organ. 2003, 81, 43–47. [Google Scholar] [PubMed]
- Cheung, K.S.L.; Yip, P.S.F. Trends in healthy life expectancy in Hong Kong SAR 1996–2008. Eur. J. Ageing 2010, 7, 257–269. [Google Scholar] [CrossRef]
- Mok, C.C.; Kwok, C.L.; Ho, L.Y.; Chan, P.T.; Yip, P.S.F. Life expectancy, standardized mortality ratios, and causes of death in six rheumatic diseases in Hong Kong, China. Arthritis Rheum. 2011, 63, 1182–1189. [Google Scholar] [CrossRef]
- Mok, C.C.; Kwok, R.C.; Yip, P.S.F. Effect of renal disease on the standardized mortality ratio and life expectancy of patients with systemic lupus erythematosus. Arthritis Rheum. 2013, 65, 2154–2160. [Google Scholar] [CrossRef] [PubMed]
- Arriaga, E.E. Measuring and explaining the change in life expectancies. Demography 1984, 21, 83–96. [Google Scholar] [CrossRef] [PubMed]
- Arriaga, E.E. Changing Trends in Mortality Decline during the Last Decades. In Differential Mortality: Methodological Issues and Biosocial Factors; Clarendon Press: Oxford, UK, 1989; pp. 105–129. [Google Scholar]
- Kannisto, V.; Lauritsen, J.; Thatcher, A.R.; Vaupel, J.W. Reductions in mortality at advanced ages: Several decades of evidence from 27 countries. Popul. Dev. Rev. 1994, 20, 793–810. [Google Scholar] [CrossRef]
- Cheung, S.L.K.; Robine, J.M.; Tu, E.J.C.; Caselli, G. Three dimensions of the survival curve: Horizontalization, verticalization, and longevity extension. Demography 2005, 42, 243–258. [Google Scholar] [CrossRef] [PubMed]
- Avraam, D.; Arnold, S.; Jones, D.; Vasiev, B. Time-evolution of age-dependent mortality patterns in mathematical model of heterogeneous human population. Exp. Gerontol. 2014, 60, 18–30. [Google Scholar] [CrossRef] [PubMed]
- Yoshinaga, K.; Une, H. Contributions of mortality changes by age group and selected causes of death to the increase in Japanese life expectancy at birth from 1950 to 2000. Eur. J. Epidemiol. 2005, 20, 49–57. [Google Scholar] [CrossRef] [PubMed]
- Yanagishita, M.; Guralnik, J.M. Changing mortality patterns that led life expectancy in Japan to surpass Sweden’s: 1972–1982. Demography 1988, 25, 611–624. [Google Scholar] [CrossRef]
- Kong, X.; Yang, Y.; Gao, J.; Guan, J.; Liu, Y.; Wang, R.; Xing, B.; Li, Y.; Ma, W. Overview of the health care system in Hong Kong and its referential significance to mainland China. J. Chin. Med. Assoc. 2015, 78, 569–573. [Google Scholar] [CrossRef]
- Department of Health, the Government of the Hong Kong Special Administrative Region. Strategy and Action Plan to Prevent and Control Non-communicable Diseases in Hong Kong. Available online: https://www. dh.gov.hk/english/pub_rec/pub_rec.html (accessed on 1 November 2018).
- Burden of Hospitalized Pneumonia in Hong Kong: A Population-Based Estimation from 2011–15. Available online: https://hub.hku.hk/handle/10722/263645 (accessed on 25 March 2019).
- Wu, X.; Law, C.K.; Yip, P.S.F. A Projection of Future Hospitalisation Needs in a Rapidly Ageing Society: A Hong Kong Experience. Int. J. Environ. Res. Public Health 2019, 16, 473. [Google Scholar] [CrossRef]
- WHO. Global Status Report on Noncommunicable Diseases; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Dans, A.; Ng, N.; Varghese, C.; Tai, E.S.; Firestone, R.; Bonita, R. The rise of chronic non-communicable diseases in southeast Asia: Time for action. Lancet 2011, 377, 680–689. [Google Scholar] [CrossRef]
- Beaglehole, R.; Yach, D. Globalisation and the prevention and control of non-communicable disease: The neglected chronic diseases of adults. Lancet 2003, 362, 903–908. [Google Scholar] [CrossRef]
- Danaei, G.; Ding, E.L.; Mozaffarian, D.; Taylor, B.; Rehm, J.; Murray, C.J.; Ezzati, M. The preventable causes of death in the United States: Comparative risk assessment of dietary, lifestyle, and metabolic risk factors. PLoS Med. 2009, 6. [Google Scholar] [CrossRef] [PubMed]
- Ikeda, N.; Inoue, M.; Iso, H.; Ikeda, S.; Satoh, T.; Noda, M.; Mizoue, T.; Imano, H.; Saito, E.; Katanoda, K. Adult mortality attributable to preventable risk factors for non-communicable diseases and injuries in Japan: A comparative risk assessment. PLoS Med. 2012, 9, e1001160. [Google Scholar] [CrossRef] [PubMed]
- Lee, I.M.; Shiroma, E.J.; Lobelo, F.; Puska, P.; Blair, S.N.; Katzmarzyk, P.T.; The Lancet Physical Activity Series Working Group. Effect of physical inactivity on major non-communicable diseases worldwide: An analysis of burden of disease and life expectancy. Lancet 2012, 380, 219–229. [Google Scholar] [CrossRef]
- Di Cesare, M.; Khang, Y.H.; Asaria, P.; Blakely, T.; Cowan, M.J.; Farzadfar, F.; Guerrero, R.; Ikeda, N.; Kyobutungi, C.; Msyamboza, K.P. Inequalities in non-communicable diseases and effective responses. Lancet 2013, 381, 585–597. [Google Scholar] [CrossRef]
- Yap, F.H.; Ho, P.L.; Lam, K.F.; Chan, P.K.; Cheng, Y.H.; Peiris, J.S. Excess hospital admissions for pneumonia, chronic obstructive pulmonary disease, and heart failure during influenza seasons in Hong Kong. J. Med. Virol. 2004, 73, 617–623. [Google Scholar] [CrossRef] [PubMed]
| Causes of Death | 1986 | 1995 | 2005 | 2015 | ||||
|---|---|---|---|---|---|---|---|---|
| Males | Females | Males | Females | Males | Females | Males | Females | |
| All causes | 507.3 | 428.6 | 577.9 | 443.3 | 661.1 | 485.1 | 757.9 | 530.2 |
| Infectious Diseases | 17.2 | 10.8 | 20.3 | 15.4 | 18.1 | 13.8 | 20.1 | 14.9 |
| Tuberculosis | 11.1 | 3.8 | 10.9 | 3.4 | 6.3 | 1.8 | 3.9 | 0.7 |
| Septicaemia | 4.8 | 6.7 | 8.9 | 11.8 | 10.2 | 10.9 | 12.4 | 11.8 |
| Other Infectious Diseases | 1.3 | 0.3 | 0.6 | 0.2 | 1.7 | 1.1 | 3.8 | 2.4 |
| Malignant Neoplasms | 172.4 | 117.1 | 196.0 | 119.7 | 230.2 | 136.6 | 247.4 | 151.5 |
| Endocrine Diseases | 3.6 | 5.9 | 6.0 | 10.4 | 8.9 | 11.6 | 8.5 | 8.2 |
| Diabetes Mellitus | 3.3 | 5.4 | 5.5 | 9.7 | 7.5 | 10.0 | 7.0 | 6.4 |
| Other Endocrine Diseases | 0.2 | 0.5 | 0.5 | 0.7 | 1.4 | 1.5 | 1.5 | 1.8 |
| Circulatory Diseases | 134.8 | 136.4 | 143.9 | 140.3 | 157.4 | 145.0 | 159.2 | 119.0 |
| Cerebrovascular Diseases | 49.4 | 58.7 | 49.8 | 58.3 | 51.3 | 50.4 | 49.1 | 40.6 |
| Heart Diseases | 64.8 | 59.5 | 75.6 | 65.8 | 86.4 | 75.0 | 90.4 | 63.9 |
| Other Circulatory Diseases | 20.6 | 18.2 | 18.4 | 16.2 | 19.7 | 19.6 | 19.8 | 14.5 |
| Respiratory Diseases | 82.5 | 65.3 | 108.9 | 81.0 | 128.2 | 83.1 | 177.5 | 116.9 |
| Pneumonia | 28.9 | 28.3 | 55.7 | 52.7 | 70.3 | 57.2 | 124.9 | 96.3 |
| Chronic Lower Respiratory Diseases | 45.4 | 27.9 | 45.5 | 22.2 | 49.7 | 19.0 | 36.9 | 9.7 |
| Other Respiratory Diseases | 8.2 | 9.1 | 7.7 | 6.2 | 8.2 | 6.9 | 15.8 | 10.9 |
| Digestive System | 23.0 | 15.1 | 26.4 | 19.5 | 24.0 | 18.3 | 26.1 | 17.4 |
| Genitourinary System | 18.5 | 25.5 | 16.8 | 20.8 | 24.2 | 28.8 | 31.3 | 30.8 |
| External Causes | 34.9 | 21.5 | 37.2 | 17.1 | 38.4 | 19.1 | 35.3 | 17.3 |
| Accidents | 17.3 | 8.5 | 18.5 | 6.5 | 16.1 | 6.4 | 17.1 | 8.4 |
| Suicide | 13.5 | 10.4 | 16.1 | 9.7 | 18.9 | 10.9 | 17.4 | 8.6 |
| Other External Causes | 4.0 | 2.6 | 2.6 | 0.9 | 3.4 | 1.8 | 0.8 | 0.4 |
| Causes of Death | Males | Females | ||||
|---|---|---|---|---|---|---|
| 1986–1995 | 1996–2005 | 2006–2015 | 1986–1995 | 1996–2005 | 2006–2015 | |
| All Causes | 3.392 | 1.404 | 1.770 | 2.132 | 1.292 | 1.242 |
| Infectious Diseases | 0.041 | 0.150 | 0.078 | −0.033 | 0.150 | 0.038 |
| Tuberculosis | 0.116 | 0.073 | 0.098 | 0.031 | 0.037 | 0.037 |
| Septicaemia | −0.107 | 0.099 | 0.019 | −0.074 | 0.129 | 0.031 |
| Other Infectious Diseases | 0.033 | −0.022 | −0.039 | 0.010 | −0.016 | −0.030 |
| Malignant Neoplasms | 0.613 | 0.279 | 0.887 | 0.391 | 0.312 | 0.226 |
| Endocrine Diseases | −0.033 | −0.020 | 0.071 | −0.059 | −0.009 | 0.066 |
| Diabetes Mellitus | −0.018 | −0.017 | 0.076 | −0.058 | 0.003 | 0.053 |
| Other Endocrine Diseases | −0.015 | −0.003 | −0.005 | 0.000 | −0.012 | 0.013 |
| Circulatory Diseases | 1.452 | 0.202 | 0.832 | 0.675 | 0.192 | 1.069 |
| Cerebrovascular Diseases | 0.709 | 0.166 | 0.278 | 0.312 | 0.218 | 0.392 |
| Heart Diseases | 0.471 | 0.022 | 0.411 | 0.231 | 0.031 | 0.520 |
| Other Circulatory Diseases | 0.272 | 0.015 | 0.143 | 0.131 | −0.056 | 0.157 |
| Respiratory Diseases | 0.455 | 0.631 | −0.166 | −0.037 | 0.695 | −0.225 |
| Pneumonia | −0.277 | 0.302 | −0.528 | −0.502 | 0.519 | −0.351 |
| Chronic Lower Respiratory Diseases | 0.498 | 0.300 | 0.458 | 0.291 | 0.159 | 0.197 |
| Other Respiratory Diseases | 0.235 | 0.029 | −0.096 | 0.174 | 0.017 | −0.071 |
| Digestive System | 0.092 | 0.217 | 0.117 | −0.039 | 0.083 | 0.124 |
| Genitourinary System | 0.362 | −0.032 | 0.075 | 0.314 | −0.066 | 0.121 |
| External Causes | 0.017 | 0.269 | 0.229 | 0.241 | 0.135 | 0.146 |
| Accidents | 0.012 | 0.364 | 0.188 | 0.093 | 0.179 | 0.015 |
| Suicide | −0.067 | −0.125 | 0.028 | 0.078 | −0.073 | 0.108 |
| Other External Causes | 0.072 | 0.030 | 0.013 | 0.070 | 0.029 | 0.022 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zheng, Y.; Chang, Q.; Yip, P.S.F. Understanding the Increase in Life Expectancy in Hong Kong: Contributions of Changes in Age- and Cause-Specific Mortality. Int. J. Environ. Res. Public Health 2019, 16, 1959. https://doi.org/10.3390/ijerph16111959
Zheng Y, Chang Q, Yip PSF. Understanding the Increase in Life Expectancy in Hong Kong: Contributions of Changes in Age- and Cause-Specific Mortality. International Journal of Environmental Research and Public Health. 2019; 16(11):1959. https://doi.org/10.3390/ijerph16111959
Chicago/Turabian StyleZheng, Yan, Qingsong Chang, and Paul Siu Fai Yip. 2019. "Understanding the Increase in Life Expectancy in Hong Kong: Contributions of Changes in Age- and Cause-Specific Mortality" International Journal of Environmental Research and Public Health 16, no. 11: 1959. https://doi.org/10.3390/ijerph16111959
APA StyleZheng, Y., Chang, Q., & Yip, P. S. F. (2019). Understanding the Increase in Life Expectancy in Hong Kong: Contributions of Changes in Age- and Cause-Specific Mortality. International Journal of Environmental Research and Public Health, 16(11), 1959. https://doi.org/10.3390/ijerph16111959




