Exploration of Medical Trajectories of Stroke Patients Based on Group-Based Trajectory Modeling
Abstract
:1. Introduction
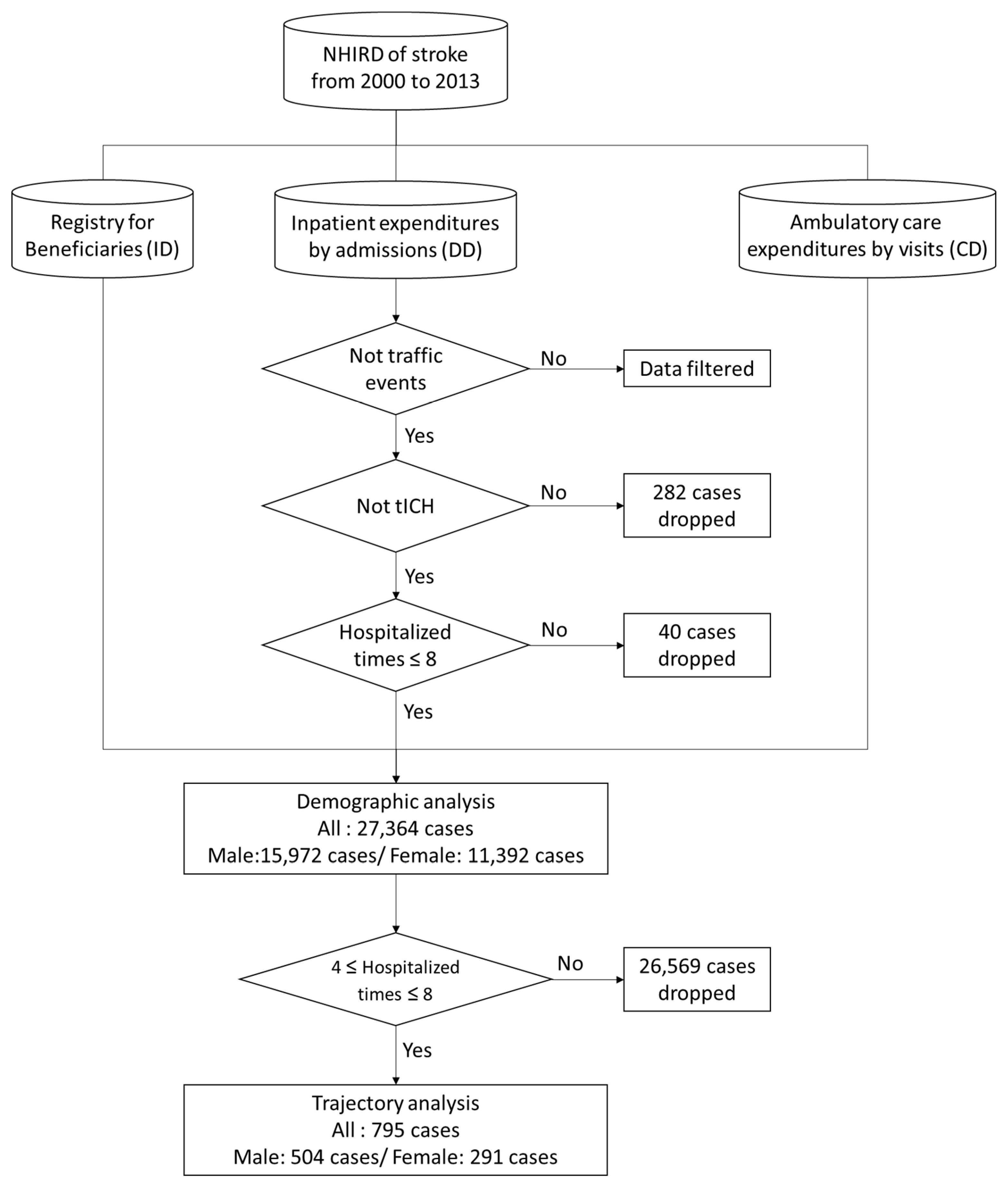
2. Materials and Methods
2.1. Data Source, Protection, and Permissions
2.2. Data Management and Statistical Analysis
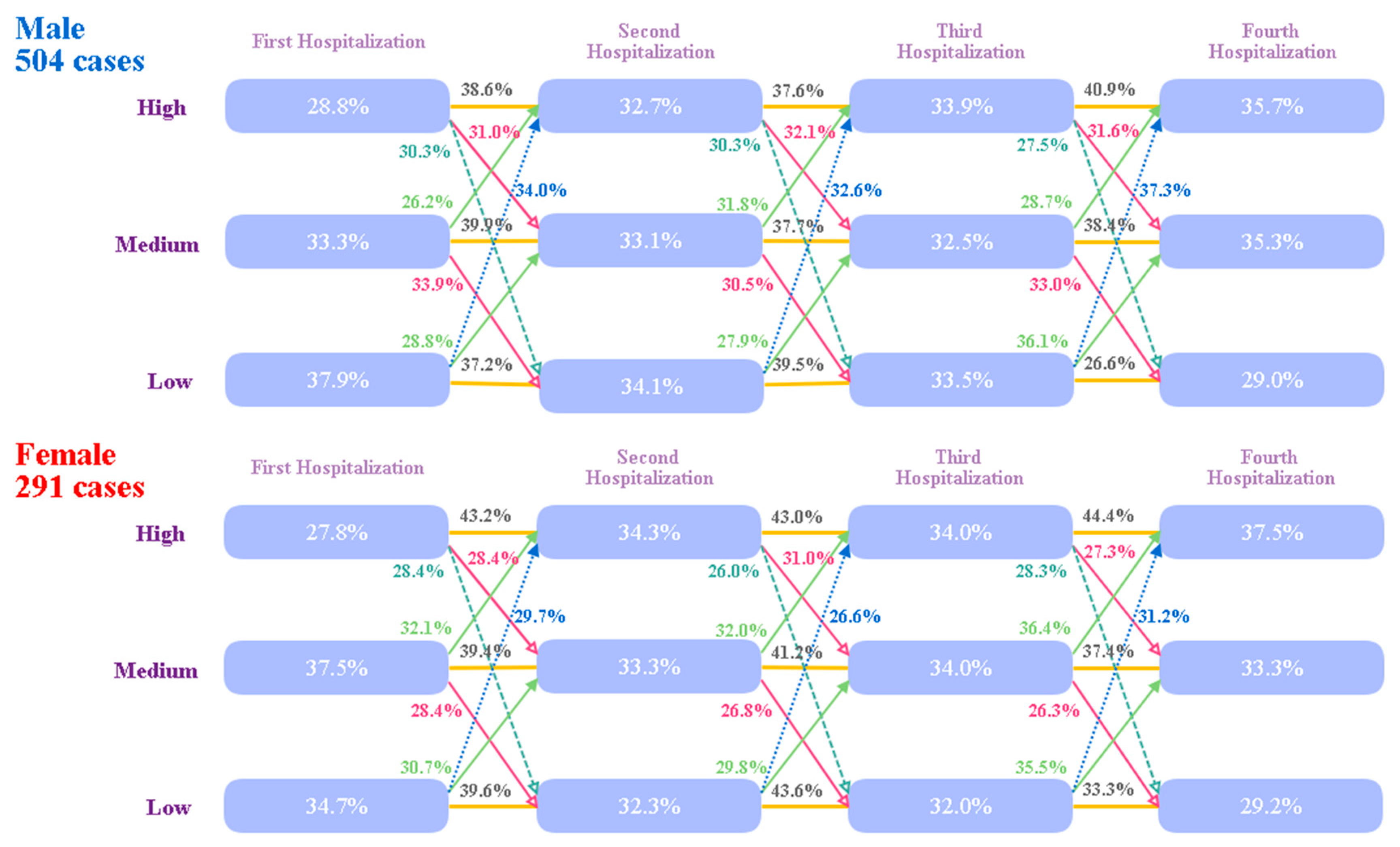
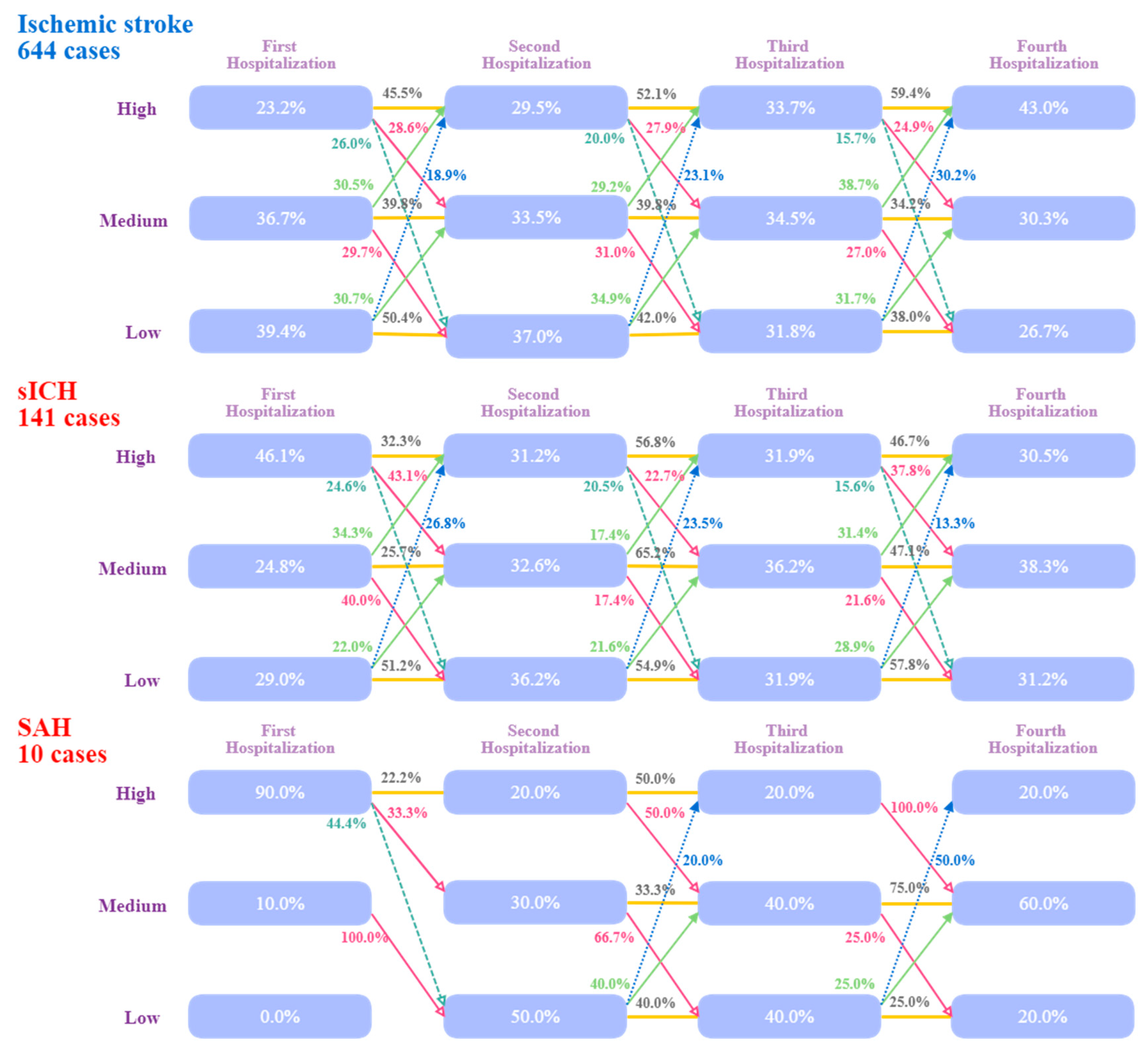
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Chen, R.; Hu, Z.; Chen, R.-L.; Zhang, D.; Xu, L.; Wang, J.; Wei, L. Socioeconomic deprivation and survival after stroke in China: A systematic literature review and a new population-based cohort study. BMJ Open 2015, 5, e005688. [Google Scholar] [CrossRef] [PubMed]
- Lahiry, S.; Levi, C.; Kim, J.; Cadilhac, D.A.; Searles, A. Economic Evaluation of a Pre-Hospital Protocol for Patients with Suspected Acute Stroke. Front. Public Health 2018, 6, 43. [Google Scholar] [CrossRef] [PubMed]
- Chan, C.; Ting, H.; Huang, H. The definition of a prolonged intensive care unit stay for spontaneous intracerebral hemorrhage patients: An application with national health insurance research database. Biomed. Res. Int. 2014, 2014, 891725. [Google Scholar] [CrossRef] [PubMed]
- Chan, C.; Ting, H.; Huang, H. The incidence, hospital expenditure, and, 30 day and 1 year mortality rates of spontaneous intracerebral hemorrhage in Taiwan. J. Clin. Neurosci. 2014, 21, 91–94. [Google Scholar] [CrossRef] [PubMed]
- Ting, H.-W.; Chan, C.-L.; Pan, R.-H.; Lai, R.K.; Chien, T.-Y. Use of Information Technologies to Explore Correlations between Climatic Factors and Spontaneous Intracerebral Hemorrhage in Different Age Groups. J. Comput. Sci. Eng. 2017, 11, 142–151. [Google Scholar] [CrossRef]
- Krishnamurthi, N.; Francis, J.; Fihn, S.D.; Meyer, C.S.; Whooley, M.A. Leading causes of cardiovascular hospitalization in 8.45 million US veterans. PLoS ONE 2018, 13, e0193996. [Google Scholar]
- Ting, H.W.; Chien, T.Y.; Lai, K.R.; Pan, R.H.; Wu, K.H.; Chen, J.M.; Chan, C.L. Differences in Spontaneous Intracerebral Hemorrhage Cases between Urban and Rural Regions of Taiwan: Big Data Analytics of Government Open Data. Int. J. Environ. Res. Public Health 2017, 14, 1548. [Google Scholar] [CrossRef]
- Thanvi, B.R.; Sprigg, N.; Munshi, S.K. Advances in spontaneous intracerebral haemorrhage. Int. J. Clin. Pract. 2012, 66, 556–564. [Google Scholar] [CrossRef]
- Yang, L.; Liu, J.; Qi, G.; Li, Y.; Liu, Y. The middle-term outcome of carotid endarterectomy and stenting for treatment of ischemic stroke in Chinese patients. Sci. Rep. 2018, 8, 4697. [Google Scholar] [CrossRef] [Green Version]
- Li, H.W.; Yang, M.C.; Chung, K.P. Predictors for readmission of acute ischemic stroke in Taiwan. J. Formos. Med. Assoc. 2011, 110, 627–633. [Google Scholar] [CrossRef] [Green Version]
- Tshikwela, M.L.; Longo-Mbenza, B. Spontaneous intracerebral hemorrhage: Clinical and computed tomography findings in predicting in-hospital mortality in Central Africans. J. Neurosci. Rural Pract. 2012, 3, 115–120. [Google Scholar] [PubMed]
- Martini, S.R.; Flaherty, M.L.; Brown, W.M.; Haverbusch, M.; Comeau, M.E.; Sauerbeck, L.R.; Kissela, B.M.; Deka, R.; Kleindorfer, D.O.; Moomaw, C.J.; et al. Risk factors for intracerebral hemorrhage differ according to hemorrhage location. Neurology 2012, 79, 2275–2282. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, V.; Moshier, E.; Leng, S.; Barlogie, B.; Cho, H.J.; Jagannath, S.; Madduri, D.; Mazumdar, M.; Parekh, S.; Chari, A. Risk stratification of smoldering multiple myeloma: Predictive value of free light chains and group-based trajectory modeling. Blood Adv. 2018, 2, 1470–1479. [Google Scholar] [CrossRef] [PubMed]
- Nagin, D.S. Group-Based Trajectory Modeling: An Overview. Ann. Nutr. Metab. 2014, 65, 205–210. [Google Scholar] [CrossRef] [PubMed]
- Reynaud, E.; Plancoulaine, S.; Annesi-Maesano, I.; Bernard, J.; Botton, J.; Dargent-Molina, P.; De Lauzon-Guillain, B.; Ducimetière, P.; De Agostini, M.; Foliguet, B.; et al. Night-waking and behavior in preschoolers: A developmental trajectory approach. Sleep Med. 2018, 43, 90–95. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.F.; Liu, J.C.; Huang, H.C.; Chuang, S.Y.; Chen, C.I.; Lin, K.C. Longitudinal transition trajectory of gouty arthritis and its comorbidities: A population-based study. Rheumatol. Int. 2017, 37, 313–322. [Google Scholar] [CrossRef] [PubMed]
- Institutes N: Introduction to the National Health Insurance Research Database (NHIRD), Taiwan. Available online: http://nhird.nhri.org.tw/en/index.htm (accessed on 1 December 2013).
- Chien, T.-Y.; Ting, H.-W.; Chan, C.-L.; Yang, N.-P.; Pan, R.-H.; Lai, K.R.; Hung, S.-I. Does the Short-Term Effect of Air Pollution Influence the Incidence of Spontaneous Intracerebral Hemorrhage in Different Patient Groups? Big Data Analysis in Taiwan. Int. J. Environ. Res. Public Health 2017, 14, 1547. [Google Scholar] [CrossRef]
- Lin, K.B.; Lai, K.R.; Yang, N.P.; Wu, K.S.; Ting, H.W.; Pan, R.H.; Chan, C.L. Trends and outcomes in the utilization of laparoscopic appendectomies in a low-income population in Taiwan from 2003 to 2011. Int. J. Equity Health 2015, 14, 100. [Google Scholar] [CrossRef]
- Chan, C.L.; You, H.J.; Huang, H.T.; Ting, H.W. Using an integrated COC index and multilevel measurements to verify the care outcome of patients with multiple chronic conditions. BMC Health Serv. Res. 2012, 12, 405. [Google Scholar] [CrossRef]
- Lin, K.B.; Lai, K.R.; Yang, N.P.; Chan, C.L.; Liu, Y.H.; Pan, R.H.; Huang, C.H. Epidemiology and socioeconomic features of appendicitis in Taiwan: A 12-year population-based study. World J. Emerg. Surg. 2015, 10, 42. [Google Scholar] [CrossRef]
- Pan, R.-H.; Chang, N.-T.; Chu, D.; Hsu, K.-F.; Hsu, Y.-N.; Hsu, J.-C.; Tseng, L.-Y.; Yang, N.-P. Epidemiology of Orthopedic Fractures and Other Injuries among Inpatients Admitted due to Traffic Accidents: A 10-Year Nationwide Survey in Taiwan. Sci. World J. 2014, 2014, 637872. [Google Scholar] [CrossRef] [PubMed]
- Innovation Center for Big Data and Digital Convergence, Yuan Ze University. Available online: http://www.innobic.yzu.edu.tw/ (accessed on 10 August 2017).
- Wu, C.-Y.; Chen, Y.-J.; Ho, H.J.; Hsu, Y.-C.; Kuo, K.N.; Wu, M.-S.; Lin, J.-T. Association between nucleoside analogues and risk of hepatitis B virus–related hepatocellular carcinoma recurrence following liver resection. JAMA 2012, 308, 1906–1913. [Google Scholar] [CrossRef] [PubMed]
- Nagin, D.S.; Jones, B.L.; Passos, V.L.; Tremblay, R.E. Group-based multi-trajectory modeling. Stat. Methods Med. Res. 2018, 27, 2015–2023. [Google Scholar] [CrossRef] [PubMed]
- Koellhoffer, E.C.; McCullough, L.D. The effects of estrogen in ischemic stroke. Transl. Stroke Res. 2013, 4, 390–401. [Google Scholar] [CrossRef] [PubMed]
- Roy-O’Reilly, M.; McCullough, L.D. Sex differences in stroke: The contribution of coagulation. Exp. Neurol. 2014, 259, 16–27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Beal, C.C. Women’s Interpretation of and Cognitive and Behavioral Responses to the Symptoms of Acute Ischemic Stroke. J. Neurosci. Nurs. 2014, 46, 256–266. [Google Scholar] [CrossRef] [PubMed]
- Scarborough, J.E.; Pappas, T.N.; Bennett, K.M.; Lagoo-Deenadayalan, S. Failure-to-pursue rescue: Explaining excess mortality in elderly emergency general surgical patients with preexisting “do-not-resuscitate” orders. Ann. Surg. 2012, 256, 453–461. [Google Scholar] [CrossRef]
- Silvennoinen, K.; Meretoja, A.; Strbian, D.; Putaala, J.; Kaste, M.; Tatlisumak, T. Do-not-resuscitate (DNR) orders in patients with intracerebral hemorrhage. Int. J. Stroke 2014, 9, 53–58. [Google Scholar] [CrossRef] [PubMed]
- de Decker, L.; Annweiler, C.; Launay, C.; Fantino, B.; Beauchet, O. Do not resuscitate orders and aging: Impact of multimorbidity on the decision-making process. J. Nutr. Health Aging 2014, 18, 330–335. [Google Scholar] [CrossRef]
| Admission Times (n) | # Patients | Percentage | # Patients (n ≤ Admission Times ≤ 8) |
|---|---|---|---|
| 1 | 20,392 | 74.41% | 27,364 |
| 2 | 4772 | 17.41% | 6972 |
| 3 | 1405 | 5.13% | 2200 |
| 4 | 497 | 1.81% | 795 |
| 5 | 183 | 0.67% | 298 |
| 6 | 68 | 0.25% | 115 |
| 7 | 28 | 0.10% | 47 |
| 8 | 19 | 0.07% | 19 |
| 9 | 14 | 0.05% | |
| 10 | 7 | 0.03% | |
| >10 | 19 | 0.07% | |
| Total | 27,404 | ||
| First Hospitalization | Second Hospitalization | Third Hospitalization | Fourth Hospitalization | |||||
|---|---|---|---|---|---|---|---|---|
| All | Death | All | Death | All | Death | All | Death | |
| § Case numbers (%) | 27,364 | 1924 (7.0%) | 6972 | 428 (6.1%) | 2200 | 138 (6.3%) | 795 | 49 (6.2%) |
| Male | 15,972 | 1100 (6.9%) | 4130 | 224 (5.0%) | 1351 | 82 (6.1%) | 504 | 36 (7.1%) |
| Female | 11,392 | 824 (7.2%) | 2842 | 204 (7.2%) | 849 | 56 (6.6%) | 291 | 13 (4.5%) |
| Ischemic stroke | 20,731 | 937 (4.5%) | 5579 | 345 (6.2%) | 1782 | 101 (5.7%) | 644 | 40 (6.2%) |
| sICH | 5758 | 802 (13.9%) | 1263 | 76 (6.0%) | 385 | 33 (8.6%) | 141 | 9 (6.4%) |
| SAH | 875 | 185 (21.1%) | 130 | 7 (5.4%) | 33 | 4 (12.1%) | 10 | 0 (0.0%) |
| ₸ Mean age (years) | 64.9 *** | 64.6 *** | 67.3 *** | 69.7 * | 68.1 *** | 68.8 *** | 67.7 *** | 70.8 |
| (SD) | (13.3) | (15.1) | (12.2) | (12.2) | (11.8) | (11.5) | (11.6) | (11.5) |
| Male | 63.1 | 62.1 | 66.0 | 67.8 | 66.5 | 66.4 | 66.9 | 71.7 |
| (SD) | (13.1) | (14.6) | (12.2) | (12.0) | (11.6) | (11.5) | (11.5) | (10.2) |
| Female | 67.1 | 67.1 | 69.6 | 71.8 | 69.8 | 73.4 | 69.9 | 71.1 |
| (SD) | (13.1) | (15.1) | (11.9) | (12.2) | (11.7) | (10.9) | (11.9) | (12.7) |
| Ischemic stroke | 66.9 | 70.6 | 68.9 | 72.2 | 69.6 | 68.6 | 69.3 | 73.5 |
| (SD) | (11.8) | (12.0) | (10.9) | (9.6) | (10.4) | (11.5) | (10.3) | (7.9) |
| sICH | 58.9 | 59.0 | 61.2 | 60.2 | 61.3 | 67.3 | 61.3 | 56.7 |
| (SD) | (15.2) | (15.4) | (14.5) | (15.9) | (14.6) | (10.6) | (14.5) | (17.2) |
| SAH | 54.7 | 57.2 | 56.9 | 56.3 | 59.0 | 77.8 | 56.6 | X |
| (SD) | (14.7) | (13.1) | (15.0) | (8.7) | (13.6) | (18.4) | (8.7) | X |
| Length of hospital stay (days)(SD) | 10.6 (8.5) | 10.7 (10.0) | 11.0 (8.6) | 11.5 * (10.1) | 11.6 (8.7) | 11.4 (10.3) | 12.2 (9.3) | 10.1 (9.0) |
| Male | 10.4 | 10.6 | 11.0 | 11.3 | 11.7 | 11.8 | 12.5 | 11.1 |
| (SD) | (8.5) | (10.2) | (8.8) | (10.5) | (8.8) | (10.6) | (9.9) | (11.5) |
| Female | 10.9 | 11.0 | 11.1 | 11.6 | 11.6 | 11.0 | 11.7 | 7.8 |
| (SD) | (8.5) | (9.6) | (8.5) | (9.4) | (8.7) | (10.0) | (8.6) | (6.6) |
| Ischemic stroke | 9.1 | 10.5 | 10.4 | 11.0 | 11.1 | 11.3 | 11.7 | 9.5 |
| (SD) | (6.7) | (8.2) | (7.9) | (9.2) | (8.3) | (10.4) | (8.7) | (7.1) |
| sICH | 16.5 | 11.3 | 14.3 | 10.5 | 14.2 | 14.1 | 16.0 | 17.6 |
| (SD) | (13.5) | (12.5) | (11.7) | (10.4) | (10.4) | (12.2) | (14.3) | (18.9) |
| SAH | 17.0 | 9.6 | 13.0 | 14.0 | 13.7 | ₸ 117.5 | 13.7 | X |
| (SD) | (13.8) | (11.0) | (11.1) | (12.8) | (13.3) | (201.6) | (8.8) | X |
| § Medical expenditure | 1806 | 2945 | 1677 | 2594 | 1662 | 2117 | 1703 | 1961 |
| (SD) | (1838) | (2295) | (1556) | (1932) | (1472) | (1691) | (1504) | (1804) |
| Male | 1751 | 2887 | 1656 | 2392 | 1645 | 2046 | 1745 | 2167 |
| (SD) | (1784) | (2247) | (1565) | (1884) | (1485) | (1711) | (1623) | (1879) |
| Female | 1883 | 3058 | 1708 | 2805 | 1688 | 2203 | 1647 | 1500 |
| (SD) | (1908) | (2395) | (1544) | (1965) | (1455) | (1683) | (1345) | (1832) |
| Ischemic stroke | 1293 | 2166 | 1534 | 2464 | 1588 | 2236 | 1665 | 2047 |
| (SD) | (1061) | (1389) | (1379) | (1780) | (1384) | (1784) | (1498) | (1871) |
| sICH | 3846 | 4164 | 2265 | 3188 | 1972 | 2031 | 1929 | 1424 |
| (SD) | (3776) | (3886) | (2273) | (2783) | (1792) | (1825) | (1717) | (1338) |
| SAH | 7636 | 4932 | 3117 | 8423 | 2180 | 1896 | 1626 | X |
| (SD) | (6373) | (4471) | (3064) | (9799) | (2506) | (2000) | (853) | X |
| § | Interval 1 to 2 | § Interval 2 to 3 | § Interval 3 to 4 |
|---|---|---|---|
| Mean days between two admissions | 522.8 (598.3) | 364.6 (426.1) | 316.5 (370.6) |
| Male (SD) | 536.7 (597.5) | 356.7 (393.4) | 336.1 (317.5) |
| Female (SD) | 543.5 (599.6) | 428.6 (484.7) | 328.2 (371.5) |
| Ischemic stroke (SD) | 556.2 (602.1) | 385.4 (423.3) | 335.1 (370.4) |
| sICH (SD) | 473.9 (564.4) | 363.4 (438.7) | 333.8 (378.2) |
| SAH (SD) | 474.5 (614.4) | 423.3 (398.7) | 188.6 (119.3) |
| Mean OPD visits (SD) | 45.1 (50.5) | 68.9 (70.4) | 56.7 (60.3) |
| Male (SD) | 42.3 (47.1) | 63.3 (65.6) | 54.6 (58.9) |
| Female (SD) | 49.6 (55.5) | 78.0 (77.8) | 60.4 (63.3) |
| Ischemic stroke (SD) | 46.5 (50.9) | 69.1 (70.7) | 56.5 (59.8) |
| sICH (SD) | 39.7 (49.1) | 69.4 (71.2) | 57.7 (64.2) |
| SAH (SD) | 39.0 (48.1) | 56.9 (55.1) | 82.4 (90.0) |
| Mean days to OPD visit after hospital discharge (SD) | 4.8 (3.1) | 5.4 (3.8) | 5.7 (4.6) |
| Male (SD) | 4.8 (3.0) | 5.4 (3.9) | 5.6 (4.4) |
| Female (SD) | 4.8 (3.1) | 5.5 (3.9) | 5.7 (4.7) |
| Ischemic stroke (SD) | 4.7 (2.9) | 5.2 (3.5) | 5.4 (4.2) |
| sICH (SD) | 5.5 (4.8) | 6.0 (5.0) | 6.1 (5.2) |
| SAH (SD) | 7.4 (7.0) | 7.7 (7.1) | 10.2 (8.5) |
| ¶ Mean OPD cost per visit (SD) | 31 (26) | 34 (28) | 37 (30) |
| Male (SD) | 31 (26) | 35 (28) | 36 (36) |
| Female (SD) | 31 (26) | 34 (27) | 38 (31) |
| Ischemic stroke (SD) | 31 (26) | 34 (28) | 36 (29) |
| sICH (SD) | 32 (26) | 35 (28) | 40 (32) |
| SAH (SD) | 25 (20) | 31 (26) | 40 (30) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chien, T.-Y.; Lee, M.-L.; Wu, W.-L.; Ting, H.-W. Exploration of Medical Trajectories of Stroke Patients Based on Group-Based Trajectory Modeling. Int. J. Environ. Res. Public Health 2019, 16, 3472. https://doi.org/10.3390/ijerph16183472
Chien T-Y, Lee M-L, Wu W-L, Ting H-W. Exploration of Medical Trajectories of Stroke Patients Based on Group-Based Trajectory Modeling. International Journal of Environmental Research and Public Health. 2019; 16(18):3472. https://doi.org/10.3390/ijerph16183472
Chicago/Turabian StyleChien, Ting-Ying, Mei-Lien Lee, Wan-Ling Wu, and Hsien-Wei Ting. 2019. "Exploration of Medical Trajectories of Stroke Patients Based on Group-Based Trajectory Modeling" International Journal of Environmental Research and Public Health 16, no. 18: 3472. https://doi.org/10.3390/ijerph16183472





