Socio-Ecological Model of Correlates of Double Burden of Malnutrition in Developing Countries: A Narrative Review
Abstract
:1. Introduction
2. Materials and Methods
3. Results and Discussion
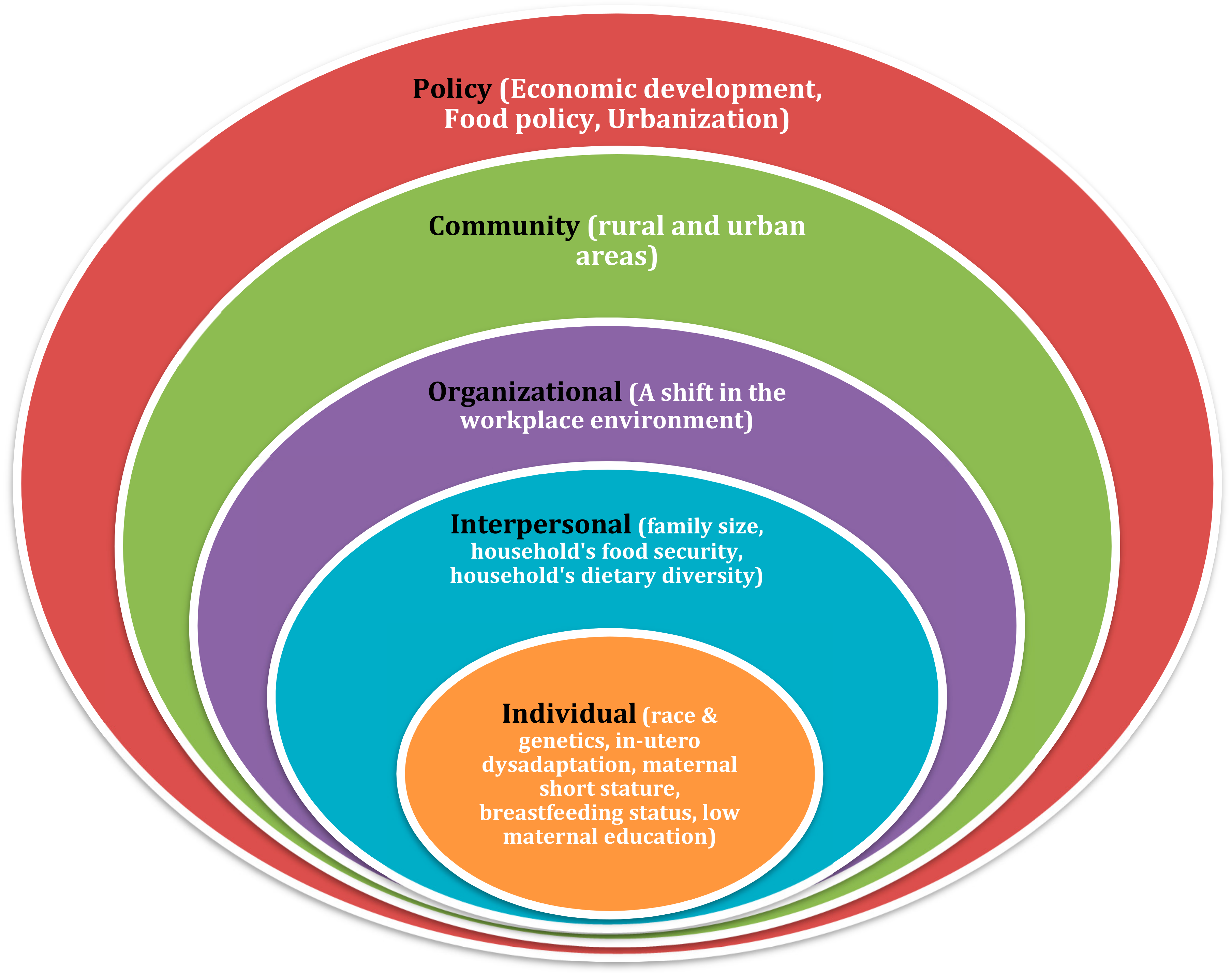
3.1. Socio-Ecological Model of Double Burden of Malnutrition
3.2. Individual Level
3.2.1. Race and Genetics
3.2.2. In Utero Dysadaptation (Barker Hypothesis)
3.2.3. Breastfeeding Status
3.2.4. Maternal Short Stature
3.2.5. Low Maternal Education
3.3. Interpersonal Level
3.3.1. Family Size
3.3.2. Household Food Security
3.3.3. Household Dietary Diversity
3.4. Organizational Level
A Shift in the Workplace Environment
3.5. Community Level
Rural and Urban Area
3.6. Policy
3.6.1. Economic Development
3.6.2. Food Policy
3.6.3. Urbanization
3.7. Potential Intervention Strategies
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Sample | Level of DBM | Correlates | Significance, Odds Ratio (OR) or 95% Confidence Interval (CI) | Key Findings | |
|---|---|---|---|---|---|
| Barquera et al., 2007 | Mexican (n = 6225) | Household level | Race and genetic (indigenous families) | The prevalence of coexistence of maternal central adiposity and child stunting (MCA) in Mexican population was higher among indigenous families | |
| Barquera et al., 2007 | Mexico (n = 6225) | Household level | Rural Area | The prevalence of coexistence of maternal central adiposity and child stunting (MCA) was higher in rural areas | |
| Bassete et al., 2014 | Argentina (n = 136) | Household level | Family Size | Household with SCOWT (stunted child and overweight mother pair) tended to have more people living in the house | |
| Bouzitou et al., 2005 | Benin (n = 148) | Community level | Household’s dietary diversity | Higher dietary diversity lowered the likelihood of double burden. | |
| Doak et al., 2005 | (n = 39,894) | Country level | Economic development | Double burden of malnutrition in a household affected mostly in countries with middle level of gross domestic product (GDP) | |
| Galiano et al., 2012 | Columbia (n = 1168) | Country level | Rural Area | The prevalence of child stunting was the highest in rural areas | |
| Ihab et al., 2013 | Malaysia (n = 223) | Household level | Household’s dietary diversity | The household’s dietary diversity of underweight child and overweight mother pairs was relatively low | |
| Jen and Brewis, 2009 | (n = 38,583) | Country level | Low Maternal Education | Analysis of Demographic Health Survey (DHS) dataset from 18 lower- and middle-income countries showed that low level of maternal education increased the likelihood of SCOWT | |
| Jehn and Brewis, 2009 | (n = 38,583) | Country level | Having more siblings in the households was also reported to be a significant predictor of SCOWT in a study involving lower and middle-income countries | ||
| Lee et al., 2010 | Guatemala (n = 2261) | Community level | Race and genetic (indigenous families) | OR = 2.0; 95%CI = 1.3-3.1 | Being an indigenous person doubled the risk of SCOWT |
| Lee et al., 2010 | Guatemala (n = 2261) | Household level | Maternal short stature | OR = 3.1; 95%CI = 2.1–4.7 | Maternal short stature is a risk factor for SCOWT |
| Lee et al., 2010 | Guatemala (n = 2261) | Country level | Family Size | OR = 1.2; 95%CI = 1.1–1.3 | Households where the mothers had a higher parity had higher likelihood of undergoing SCOM (stunted child and overweight/obese mother) |
| Lee et al., 2010 | Guatemala (n = 2261) | Household level | Working mother | OR = 1.7, 95%CI = 1.1–2.6 | Having a working mother in the household increased the risk for SCOWT in Guatemalan population |
| Lee et al., 2012 | Guatemala (n = 2492) | Household level | Economic development | OR = 1.74; 95%CI = 1.13–2.67 | Households at the middle consumption quintile had a higher likelihood of having SCOM compared to household in the first quintile |
| Oddo at al., 2012 | Indonesia (n = 247126) | Country level | Breastfeeding status | OR = 0.84; 95% CI: 0.81–0.84 | When the child was breastfed, the odds of having MCDB (maternal child double burden) were only 0.84× compared to when the child was not being breastfed |
| Oddo at al., 2012 | Bangladesh (n = 168317) | Country level | Breastfeeding status | OR = 0.55; 95% CI: 0.52–0.58 | The protective effect of breastfeeding was even greater in Bangladeshi population where the OR of having MCDB was only 0.55 (95% CI: 0.52–0.58) |
| Oddo at al., 2012 | Indonesia (n = 247126) | Country level | Maternal short stature | 2.32× (95% CI: 2.25–2.40) | The Indonesian data showed households that had a mother short in stature increased the OR for MCDB 2.32× (95% CI: 2.25–2.40) |
| Oddo at al., 2012 | Bangladesh (n = 168317) | Country level | Maternal short stature | OR = 2.11; 95% CI: 1.96–2.26 | In Bangladeshi population maternal short stature increase the likelihood of MCDB with OR = 2.11 (95% CI: 1.96–2.26). |
| Oddo at al., 2012 | Indonesia (n = 247126) | Country level | Family Size | (OR = 1.34; 95% CI: 1.28–1.40) | Large family size also correlated with MCDB, where having more than 4 persons in the family increased the odds in Indonesia |
| Oddo at al., 2012 | Bangladesh (n = 168317) | Country level | Family Size | OR = 1.94; 95% CI: 1.77–2.12 | Large family size also correlated with MCDB, where having more than 4 persons in the family increased the odds in Bangladeshi population |
| Oddo et al., 2012 | Indonesia and Bangladesh | Country level | Rural Area | Double burden of malnutrition also occurs in rural setting | |
| Ramirez-Zea et al., 2014 | Guatemala (n = 44739) | Household level | Race and genetic (indigenous families) | Higher prevalence in SCOWT pairs in indigenous households (28.2%) than non-indigenous households (14.4%) | |
| Roemling and Qaim 2013 | Indonesia (n = 27327) | Country level | Economic development | The double burden of malnutrition arguably started among the rich population, but recently shifted toward the poorest population group in Indonesia | |
| Sekiyama et al., 2015 | Indonesia (n = 242) | Household level | Household’s dietary diversity | aOR = 0.46; 95%CI = 0.21–1.04 | When consumption of the “high-animal products” was in the highest quartile, the risk of maternal-child double burden was decreased, compared to those in the lowest quartile |
| Vaezghasemi et al., 2014 | Indonesia (n = 12048) | Household level | Economic development | At the household level, the double burden of malnutrition was more prevalent in households with a high SES | |
| Wong et al., 2015 | Malaysia (n = 160) | Household level | Maternal education | aOR = 1.7, p < 0.05 | Mother with higher education was associated with higher odds of SCOWT among indigenous people of Peninsular Malaysia |
| Wong et al., 2015 | Malaysia (n = 160) | Household level | Ethnicity | aOR = 0.1, p < 0.05 | Ethnicity was associated with double burden of malnutrition measured as underweight child and overweight/obese mother |
| Wong et al., 2015 | Malaysia (n = 160) | Household level | Number of children | aOR = 0.3, p < 0.05 | Number of children in the household associated with double burden of malnutrition measured as Underweight Child and Overweight/Obese Mother |
| Wong et al., 2015 | Malaysia (n = 160) | Household level | Older age mother | aOR = 1.2, p < 0.05 | Having older aged mother was associated with double burden of malnutrition, measured as SCOWT |
| Wong et al., 2015 | Malaysia (n = 160) | Household level | Household income per capita | aOR = 16.8, p < 0.01 | Having household income per capita of less than $29.01 USD was associated with double burden of malnutrition measured as SCOWT |
| Mahmudiono et al., 2016 | Indonesia (n = 72) | Household level | Maternal education and behavior | Nutrition Education for Overweight/Obese Mother with Stunted Children (NEO-MOM) intervention using printed educational materials was hypothesized beneficial for maternal behavioral change | |
| Mahmudiono et al., 2017 | Indonesia (n = 768) | Household level | Household dietary diversity | OR = 0.89; 95% CI: 0.80–0.99 | Higher dietary diversity score was associated with lower likelihood of child stunting |
| Has et al., 2018 | Indonesia (n = 100) | Household level | Maternal behavior | Maternal motivation, perceived barriers, self-efficacy, and activity-related effect were influenced maternal behavior in fulfilling school-aged children nutritional food intake | |
| Mahmudiono et al., 2018 | Indonesia (n = 72) | Household level | Maternal literacy and behavior | 12-week nutrition education was significantly improved maternal self-efficacy in physical activity, fruits, vegetables and animal protein consumption, but did not significantly influence child-height gain | |
| Mahmudiono et al., 2018 | Indonesia (n = 768) | Community level | Household food insecurity | aOR = 2.798; 95% CI: 1.54–5.08 | Food insecurity was related to the double burden of malnutrition and the Household Food Insecurity Access Scale (HFIAS) category was a predictor of SCOWT |
| Mahmudiono et al., 2018 | Indonesia (n = 662) | Community level | Maternal literacy, dietary diversity, and food security | Household with double burden of malnutrition have relatively lower nutrition literacy, dietary diversity, and food security. Household with normal mom and child had the highest score in food security followed by OWT (overweight mother, normal child), SC (normal mom, stunted child), and lastly SCOWT | |
| Sudewi et al., 2018 | Indonesia (n = 7) | Household level | Maternal parenting style | The lack of maternal knowledge about children eating behavior was associated with children future eating disorders. Children started their eating disorders at the of 2-6 months and worsen by the aged 12 months | |
| Adi et al., 2019 | Indonesia (n = 199) | Community level | Health workers nutrition literacy | Good understanding, well-organized documents availability, and the regulation conformity by health workers were significantly correlated with exclusive breastfeeding regulation. Thus, with great breastfeeding regulation is a key factor to prevent stunting children. | |
| Diana et al., 2019 | Indonesia (n = 330) | Community level | Maternal knowledge and behavior | More than half mother had moderate knowledge about exclusive breastfeeding. There was correlation between knowledge and attitude with breastfeeding practice | |
| Mahmudiono et al., 2019 | Indonesia (n = 55) | Household level | Household dietary diversity | OR = 5.49; 95% CI: 1.32–22.93 | Children living in a poor dietary diversity household had 5-times higher risk of being stunting |
| SEM Level | Targets/Settings | Intervention Strategies |
|---|---|---|
| Individual | Pregnant and lactating women | Empower women especially pregnant and lactating women though nutrition education on healthy eating, exclusive breastfeeding and serving size [37,39,88,91]. Promoting the importance of nutrition in 1000 days of early life to break the cycle of intergenerational malnutrition [90] |
| Mother | Improve women education achievement and behavioral change [65] | |
| Interpersonal | Household | Promote family planning program |
| Improve dietary diversity in the household [40] Decrease inequalities in household’s food distribution [38,94] | ||
| Organizational | Workplace environment | Promote physical activity in the work place [94,95,96] |
| Housewife | Create peer group of housewives to reduce excess sedentary time | |
| Community | Rural area | Lobby government to emphasize rural development as a strategy for poverty reduction [88] Provide culturally accepted nutrition education to the indigenous population living in rural area |
| Urban area | Advocate the local city government to increase parks and recreational space [74] | |
| Policy | Food policy | Advocate to the government towards taxation for unhealthy food policy [15,82] |
| Urbanization | Lobby government to emphasize rural development as a strategy for poverty reduction [88] |
References
- Bhurosy, T.; Jeewon, R. Overweight and Obesity Epidemic in Developing Countries: A Problem with Diet, Physical Activity, or Socioeconomic Status? Sci. World J. 2014. [Google Scholar] [CrossRef] [PubMed]
- Finucane, M.M.; Stevens, G.A.; Cowan, M.J.; Danaei, G.; Lin, J.K.; Paciorek, C.J.; Singh, G.M.; Gutierrez, H.R.; Lu, Y.; Bahalim, A.N.; et al. National, Regional, and Global Trends in Body-Mass Index since 1980: Systematic Analysis of Health Examination Surveys and Epidemiological Studies with 960 Country-Years and 9·1 Million Participants. Lancet 2011, 377, 557–567. [Google Scholar] [CrossRef]
- WHO. Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/ obesity-and-overweight (accessed on 20 July 2019).
- Swinburn, B.A.; Sacks, G.; Hall, K.D.; McPherson, K.; Finegood, D.T.; Moodie, M.L.; Gortmaker, S.L. The Global Obesity Pandemic: Shaped by Global Drivers and Local Environments. Lancet 2011, 378, 804–814. [Google Scholar] [CrossRef]
- Ogden, C.L.; Carroll, M.D.; Kit, B.K.; Flegal, K.M. Prevalence of Childhood and Adult Obesity in the United States, 2011–2012. JAMA 2014, 311, 806. [Google Scholar] [CrossRef] [PubMed]
- Dietz, W.H. The Response of the US Centers for Disease Control and Prevention to the Obesity Epidemic. Annu. Rev. Public Health 2015, 36, 575–596. [Google Scholar] [CrossRef] [Green Version]
- Martorell, R.; Khan, L.K.; Hughes, M.L.; Grummer-Strawn, L.M. Obesity in Women from Developing Countries. Eur. J. Clin. Nutr. 2000, 54, 247–252. [Google Scholar] [CrossRef] [PubMed]
- Bredenkamp, C.; Buisman, L.R.; Van de Poel, E. Persistent Inequalities in Child Undernutrition: Evidence from 80 Countries, from 1990 to Today. Int. J. Epidemiol. 2014, 43, 1328–1335. [Google Scholar] [CrossRef]
- Restrepo-Méndez, M.C.; Barros, A.J.D.; Black, R.E.; Victora, C.G. Time Trends in Socio-Economic Inequalities in Stunting Prevalence: Analyses of Repeated National Surveys. Public Health Nutr. 2014, 18, 2097–2104. [Google Scholar] [CrossRef]
- United Nations Children’s Fund; World Health Organization; World Bank Group. Improving Child Nutrition: Levels and Trends in Child Malnutrition: UNICEF-WHO-The World Bank Joint Child Malnutrition Estimates; WHO: Geneva, Switzerland, 2013. [Google Scholar]
- UNICEF. Malnutrition in Children–UNICEF DATA. Available online: https://data.unicef.org/topic/nutrition/malnutrition/ (accessed on 21 July 2019).
- Food and Agriculture Organization of The United Nations. The Double Burden of Malnutrition Case Studies from Six Developing Countries; Food and Agriculture Organization of The United Nations: Rome, Italy, 2006. [Google Scholar]
- Tzioumis, E.; Adair, L.S. Childhood Dual Burden of Under- and Overnutrition in Low- and Middle-InCome Countries: A Critical Review. Food Nutr. Bull. 2014, 35, 230–243. [Google Scholar] [CrossRef]
- Gartner, A.; El Ati, J.; Traissac, P.; Bour, A.; Berger, J.; Landais, E.; El Hsaïni, H.; Ben Rayana, C.; Delpeuch, F. A Double Burden of Overall or Central Adiposity and Anemia or Iron Deficiency Is Prevalent but with Little Socioeconomic Patterning among Moroccan and Tunisian Urban Women. J. Nutr. 2014, 144, 87–97. [Google Scholar] [CrossRef]
- Kroker-Lobos, M.F.; Pedroza-Tobías, A.; Pedraza, L.S.; Rivera, J.A. The Double Burden of Undernutrition and Excess Body Weight in Mexico. Am. J. Clin. Nutr. 2014, 100, 1652S–1658S. [Google Scholar] [CrossRef] [PubMed]
- Dieffenbach, S.; Stein, A.D. Stunted Child/Overweight Mother Pairs Represent a Statistical Artifact, Not a Distinct Entity. J. Nutr. 2012, 142, 771–773. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Houser, R.F.; Must, A.; de Fulladolsa, P.P.; Bermudez, O.I. Socioeconomic Disparities and the Familial Coexistence of Child Stunting and Maternal Overweight in Guatemala. Econ. Hum. Biol. 2012, 10, 232–241. [Google Scholar] [CrossRef] [PubMed]
- Ramirez-Zea, M.; Kroker-Lobos, M.F.; Close-Fernandez, R.; Kanter, R. The Double Burden of Malnutrition in Indigenous and Nonindigenous Guatemalan Populations. Am. J. Clin. Nutr. 2014, 100, 1644S–1651S. [Google Scholar] [CrossRef] [PubMed]
- Oddo, V.M.; Rah, J.H.; Semba, R.D.; Sun, K.; Akhter, N.; Sari, M.; de Pee, S.; Moench-Pfanner, R.; Bloem, M.; Kraemer, K. Predictors of Maternal and Child Double Burden of Malnutrition in Rural Indonesia and Bangladesh. Am. J. Clin. Nutr. 2012, 95, 951–958. [Google Scholar] [CrossRef] [PubMed]
- Lee, G.; Gutierrez, C.; Jones, A.; Castro, N.; Cevallos, W.; Eisenberg, J. Double Burden of Malnutrition in Rural Ecuador: Adult Overweight and Child Stunting Co-Occur at the Community but Not the Household Level (P10-075-19). Curr. Dev. Nutr. 2019, 3. [Google Scholar] [CrossRef]
- Labadarios, D.; Mchiza, Z.; Steyn, N.P.; Gericke, G.; Maunder, E.; Davids, Y.; Parker, W. Food Security in South Africa: A Review of National Surveys. Bull. World Health Organ. 2011, 89, 891–899. [Google Scholar] [CrossRef]
- Doak, C.M.; Adair, L.S.; Bentley, M.; Monteiro, C.; Popkin, B.M. The Dual Burden Household and the Nutrition Transition Paradox. Int. J. Obes. 2005, 29, 129–136. [Google Scholar] [CrossRef]
- Wang, H.; Du, S.; Zhai, F.; Popkin, B.M. Trends in the Distribution of Body Mass Index among Chinese Adults, Aged 20–45 Years (1989–2000). Int. J. Obes. 2007, 31, 272–278. [Google Scholar] [CrossRef]
- Manyanga, T.; El-sayed, H.; Doku, D.T.; Randall, J.R. The Prevalence of Underweight, Overweight, Obesity and Associated Risk Factors among School-Going Adolescents in Seven African Countries. BMC Public Health 2014, 14, 887. [Google Scholar] [CrossRef]
- Kavle, J.A.; Flax, V.L.; Abdelmegeid, A.; Salah, F.; Hafez, S.; Ramzy, M.; Hamed, D.; Saleh, G.; Galloway, R. Factors Associated with Early Growth in Egyptian Infants: Implications for Addressing the Dual Burden of Malnutrition. Matern. Child Nutr. 2016, 12, 139–151. [Google Scholar] [CrossRef] [PubMed]
- Le Nguyen, B.K.; Le Thi, H.; Thuy, N.T.; Huu, C.N.; Do, T.T.; Deurenberg, P.; Khouw, I. Double Burden of Undernutrition and Overnutrition in Vietnam in 2011: Results of the SEANUTS Study in 0.5–11-Year-Old Children. Br. J. Nutr. 2013, 110, S45–S56. [Google Scholar] [CrossRef] [PubMed]
- Rojroongwasinkul, N.; Kijboonchoo, K.; Wimonpeerapattana, W.; Purttiponthanee, S.; Yamborisut, U.; Boonpraderm, A.; Kunapan, P.; Thasanasuwan, W.; Khouw, I. SEANUTS: The Nutritional Status and Dietary Intakes of 0.5–12-Year-Old Thai Children. Br. J. Nutr. 2013, 25, 36–44. [Google Scholar] [CrossRef]
- Sandjaja, S.; Budiman, B.; Harahap, H.; Ernawati, F.; Soekatri, M.; Widodo, Y.; Sumedi, E.; Rustan, E.; Sofia, G.; Syarief, S.N.; et al. Food Consumption and Nutritional and Biochemical Status of 0.5–12-Year-Old Indonesian Children: The SEANUTS Study. Br. J. Nutr. 2013, 110, S11–S20. [Google Scholar] [CrossRef] [PubMed]
- Abdullah, A. The Double Burden of Undernutrition and over Nutrition in Developing Countries: An Update. Curr. Obes. Rep. 2015, 4, 337–349. [Google Scholar] [CrossRef]
- Barquera, S.; Peterson, K.E.; Must, A.; Rogers, B.L.; Flores, M.; Houser, R.; Monterrubio, E.; Rivera-Dommarco, J.A. Coexistence of Maternal Central Adiposity and Child Stunting in Mexico. Int. J. Obes. 2007, 31, 601–607. [Google Scholar] [CrossRef] [PubMed]
- Bassett, D.R.; Howley, E.T. Limiting Factors for Maximum Oxygen Uptake and Determinants of Endurance Performance. Med. Sci. Sport. Exerc. 2000, 32, 70–84. [Google Scholar] [CrossRef]
- Freire, W.B.; Silva-Jaramillo, K.M.; Ramírez-Luzuriaga, M.J.; Belmont, P.; Waters, W.F. The Double Burden of Undernutrition and Excess Body Weight in Ecuador. Am. J. Clin. Nutr. 2014, 100, 1636S–1643S. [Google Scholar] [CrossRef]
- Sarmiento, O.L.; Parra, D.C.; González, S.A.; González-Casanova, I.; Forero, A.Y.; Garcia, J. The Dual Burden of Malnutrition in Colombia. Am. J. Clin. Nutr. 2014, 100, 1628S–1635S. [Google Scholar] [CrossRef]
- Conde, W.L.; Monteiro, C.A. Nutrition Transition and Double Burden of Undernutrition and Excess of Weight in Brazil. Am. J. Clin. Nutr. 2014, 100, 1617S–1622S. [Google Scholar] [CrossRef]
- Atalah, E.; Amigo, H.; Bustos, P. Does Chile’s Nutritional Situation Constitute a Double Burden? Am. J. Clin. Nutr. 2014, 100, 1623S–1627S. [Google Scholar] [CrossRef] [PubMed]
- Ihab, A.N.; Rohana, A.J.; Manan, W.M.W.; Suriati, W.N.W.; Zalilah, M.S.; Rusli, A.M. The Coexistence of Dual Form of Malnutrition in a Sample of Rural Malaysia. Int. J. Prev. Med. 2013, 4, 690–699. [Google Scholar] [PubMed]
- Wong, C.Y.; Zalilah, M.S.; Chua, E.Y.; Norhasmah, S.; Chin, Y.S.; Siti Nur’Asyura, A. Double-Burden of Malnutrition among the Indigenous Peoples (Orang Asli) of Peninsular Malaysia. BMC Public Health 2015, 15, 680. [Google Scholar] [CrossRef] [PubMed]
- Roemling, C.; Qaim, M. Dual Burden Households and Intra-Household Nutritional Inequality in Indonesia. Econ. Hum. Biol. 2013, 11, 563–573. [Google Scholar] [CrossRef] [PubMed]
- Vaezghasemi, M.; Öhman, A.; Eriksson, M.; Hakimi, M.; Weinehall, L.; Kusnanto, H.; Ng, N. The Effect of Gender and Social Capital on the Dual Burden of Malnutrition: A Multilevel Study in Indonesia. PLoS ONE 2014, 9, e103849. [Google Scholar] [CrossRef]
- Sekiyama, M.; Jiang, H.W.; Gunawan, B.; Dewanti, L.; Honda, R.; Shimizu-Furusawa, H.; Abdoellah, O.S.; Watanabe, C. Double Burden of Malnutrition in Rural West Java: Household-Level Analysis for Father-Child and Mother-Child Pairs and the Association with Dietary Intake. Nutrients 2015, 7, 8376–8391. [Google Scholar] [CrossRef]
- Mahmudiono, T.; Nindya, T.; Andrias, D.; Megatsari, H.; Rosenkranz, R.; Mahmudiono, T.; Nindya, T.S.; Andrias, D.R.; Megatsari, H.; Rosenkranz, R.R. Household Food Insecurity as a Predictor of Stunted Children and Overweight/Obese Mothers (SCOWT) in Urban Indonesia. Nutrients 2018, 10, 535. [Google Scholar] [CrossRef]
- Bronfenbrenner, U. Toward an Experimental Ecology of Human Development. Am. Psychol. 1977, 32, 513. [Google Scholar] [CrossRef]
- Voisin, D.R.; DiClemente, R.J.; Salazar, L.F.; Crosby, R.A.; Yarber, W.L. Ecological Factors Associated with STD Risk Behaviors among Detained Female Adolescents. Soc. Work 2006, 51, 71–79. [Google Scholar] [CrossRef]
- Atilola, O. Child Mental-Health Policy Development in Sub-Saharan Africa: Broadening the Perspectives Using Bronfenbrenner’s Ecological Model. Health Promot. Int. 2017, 32, 380–391. [Google Scholar] [CrossRef]
- Kellou, N.; Sandalinas, F.; Copin, N.; Simon, C. Prevention of Unhealthy Weight in Children by Promoting Physical Activity Using a Socio-Ecological Approach: What Can We Learn from Intervention Studies? Diabetes Metab. 2014, 40, 258–271. [Google Scholar] [CrossRef]
- Robinson, T. Applying the Socio-Ecological Model to Improving Fruit and Vegetable Intake Among Low-Income African Americans. J. Community Health 2008, 33, 395–406. [Google Scholar] [CrossRef] [PubMed]
- National Cancer Institute. Theory at a Glance: A Guide for Health Promotion Practice; Lulu: Morrisville, NC, USA, 2014.
- Lee, J.; Houser, R.F.; Must, A.; de Fulladolsa, P.P.; Bermudez, O.I. Disentangling Nutritional Factors and Household Characteristics Related to Child Stunting and Maternal Overweight in Guatemala. Econ. Hum. Biol. 2010, 8, 188–196. [Google Scholar] [CrossRef] [PubMed]
- WHO Expert Consultation. Appropriate Body-Mass Index for Asian Populations and Its Implications for Policy and Intervention Strategies. Lancet 2004, 363, 157–163. [Google Scholar] [CrossRef]
- Low, S.; Chin, M.C.; Ma, S.; Heng, D.; Deurenberg-Yap, M. Rationale for Redefining Obesity in Asians. Ann. Acad. Med. Singap. 2009, 38, 66–69. [Google Scholar] [PubMed]
- Rasmussen, K.M. The “Fetal Origins” Hypothesis: Challenges and Opportunities for Maternal and Child Nutrition. Annu. Rev. Nutr. 2001, 21, 73–95. [Google Scholar] [CrossRef] [PubMed]
- Barker, D.J.P. Human Growth and Chronic Disease: A Memorial to Jim Tanner. Ann. Hum. Biol. 2012, 39, 335–341. [Google Scholar] [CrossRef]
- Ornoy, A. Prenatal Origin of Obesity and Their Complications: Gestational Diabetes, Maternal Overweight and the Paradoxical Effects of Fetal Growth Restriction and Macrosomia. Reprod. Toxicol. 2011, 32, 205–212. [Google Scholar] [CrossRef]
- Rivera, J.A.; Pedraza, L.S.; Martorell, R.; Gil, A. Introduction to the Double Burden of Undernutrition and Excess Weight in Latin America. Am. J. Clin. Nutr. 2014, 100, 1613S–1616S. [Google Scholar] [CrossRef]
- Holt, R.I.G. Fetal Programming of the Growth Hormone-Insulin-like Growth Factor Axis. Trends Endocrinol. Metab. 2002, 13, 392–397. [Google Scholar] [CrossRef]
- Chomtho, S. Breastfeeding to Prevent Double Burden of Malnutrition. Southeast Asian J. Trop. Med. Public Health 2014, 45, 132–136. [Google Scholar] [PubMed]
- Ferreira, H.S.; Moura, F.A.; Cabral Júnior, C.R.; Florêncio, T.M.M.T.; Vieira, R.C.; de Assunção, M.L. Short Stature of Mothers from an Area Endemic for Undernutrition Is Associated with Obesity, Hypertension and Stunted Children: A Population-Based Study in the Semi-Arid Region of Alagoas, Northeast Brazil. Br. J. Nutr. 2009, 101, 1239. [Google Scholar] [CrossRef] [PubMed]
- Adi, A.C.; Diana, R.; Devy, S.R.; Qomaruddin, M.B.; Damayanti, N.A.; Putri, N.K. The Correlation between Regulation Understanding by Inter-Professional First 1000 Days of Life Health Workers and the Acceleration of Toddler Stunting Prevention. Indian J. Public Health Res. Dev. 2019, 10, 911. [Google Scholar] [CrossRef]
- Diana, R.; Adi, A.C. Mother’s Knowledge, Attitude, and Practice of Exclusive Breastfeeding. Indian J. Public Health Res. Dev. 2019, 10, 887. [Google Scholar] [CrossRef]
- Felisbino-Mendes, M.S.; Villamor, E.; Velasquez-Melendez, G. Association of Maternal and Child Nutritional Status in Brazil: A Population Based Cross-Sectional Study. PLoS ONE 2014, 9, e87486. [Google Scholar] [CrossRef] [PubMed]
- Varela-Silva, M.I.; Azcorra, H.; Dickinson, F.; Bogin, B.; Frisancho, A.R. Influence of Maternal Stature, Pregnancy Age, and Infant Birth Weight on Growth during Childhood in Yucatan, Mexico: A Test of the Intergenerational Effects Hypothesis. Am. J. Hum. Biol. 2009, 21, 657–663. [Google Scholar] [CrossRef] [PubMed]
- Bove, I.; Miranda, T.; Campoy, C.; Uauy, R.; Napol, M. Stunting, Overweight and Child Development Impairment Go Hand in Hand as Key Problems of Early Infancy: Uruguayan Case. Early Hum. Dev. 2012, 88, 747–751. [Google Scholar] [CrossRef]
- Sudewi, N.P.; Soedirham, O.; Suryawan, A. Parenting Style Based on the Mother’s Personal Mastery and the Mother-Child Attachment in Relation to Child Feeding Disoders: A Qualitative Study. Indian J. Public Health Res. Dev. 2018, 9, 1777. [Google Scholar] [CrossRef]
- Has, E.M.M.; Prahasiwi, D.F.; Wahyuni, S.D.; Nursalam, F.E. Mothers’ Behaviour Regarding School-Aged Children’s Nutrition: In Indonesia. Indian J. Public Health Res. Dev. 2018, 9, 317. [Google Scholar] [CrossRef]
- Mahmudiono, T.; Al Mamun, A.; Nindya, T.S.; Andrias, D.R.; Megatsari, H.; Rosenkranz, R.R. The Effectiveness of Nutrition Education for Overweight/Obese Mother with Stunted Children (NEO-MOM) in Reducing the Double Burden of Malnutrition. Nutrients 2018, 10, 1910. [Google Scholar] [CrossRef]
- Vazir, S.; Engle, P.; Balakrishna, N.; Griffiths, P.L.; Johnson, S.L.; Creed-Kanashiro, H.; Fernandez Rao, S.; Shroff, M.R.; Bentley, M.E. Cluster-Randomized Trial on Complementary and Responsive Feeding Education to Caregivers Found Improved Dietary Intake, Growth and Development among Rural Indian Toddlers. Matern. Child Nutr. 2013, 9, 99–117. [Google Scholar] [CrossRef] [PubMed]
- Navarro, J.I.; Sigulem, D.M.; Ferraro, A.A.; Polanco, J.J.; Barros, A.J. The Double Task of Preventing Malnutrition and Overweight: A Quasi-Experimental Community-Based Trial. BMC Public Health 2013, 13, 212. [Google Scholar] [CrossRef] [PubMed]
- Mahmudiono, T.; Susila Nindya, T.; Ririn Andrias, D.; Megatsari, H.; Rachmah, Q.; Rosenkranz, R.R. Comparison of Maternal Nutrition Literacy, Dietary Diversity, and Food Security among Households with and without Double Burden of Malnutrition in Surabaya, Indonesia. Malays. J. Nutr. 2018, 24, 359–370. [Google Scholar]
- Jehn, M.; Brewis, A. Paradoxical Malnutrition in Mother-Child Pairs: Untangling the Phenomenon of Over- and Under-Nutrition in Underdeveloped Economies. Econ. Hum. Biol. 2009, 7, 28–35. [Google Scholar] [CrossRef] [PubMed]
- Chua, E.Y.; Zalilah, M.S.; Chin, Y.S.; Norhasmah, S. Dietary Diversity Is Associated with Nutritional Status of Orang Asli Children in Krau Wildlife Reserve, Pahang. Malays. J. Nutr. 2012, 18, 1–13. [Google Scholar]
- Bouzitou, G.D.N.; Fayomi, B.; Delisle, H. Child Malnutrition and Maternal Overweight in Same Households in Poor Urban Areas of Benin. Sante 2015, 15, 263–270. [Google Scholar]
- Mahmudiono, T.; Andadari, D.P.P.S.; Segalita, C. Dietary Diversity in Agricultural and Coastal Area as Potential Source for the Prevention of Child Stunting in Sidoarjo District. Indian J. Public Heal. Res. Dev. 2019, 10, 696. [Google Scholar] [CrossRef]
- Mahmudiono, T.; Sumarmi, S.; Rosenkranz, R.R. Household Dietary Diversity and Child Stunting in East Java, Indonesia. Asia Pac. J. Clin. Nutr. 2017, 26, 317–325. [Google Scholar]
- Lee, R.E.; McAlexander, K.; Banda, J. Reversing the Obesogenic Environment; Human Kinetics: Champaign, IL, USA, 2011. [Google Scholar]
- Caleyachetty, R.; Rudnicka, A.R.; Echouffo-Tcheugui, J.B.; Siegel, K.R.; Richards, N.; Whincup, P.H. Prevalence of Overweight, Obesity and Thinness in 9–10 Year Old Children in Mauritius. Glob. Health 2012, 8, 28. [Google Scholar] [CrossRef]
- Khambalia, A.Z.; Lim, S.S.; Gill, T.; Bulgiba, A.M. Prevalence and Sociodemographic Factors of Malnutrition among Children in Malaysia. Food Nutr. Bull. 2012, 33, 31–42. [Google Scholar] [CrossRef] [Green Version]
- Horiuchi, Y.; Kusama, K.; Kanha, S.; Yoshiike, N.; FIDR Research Team. Urban-Rural Differences in Nutritional Status and Dietary Intakes of School-Aged Children in Cambodia. Nutrients 2018, 11, 14. [Google Scholar] [CrossRef] [PubMed]
- Shafique, S.; Akhter, N.; Stallkamp, G.; de Pee, S.; Panagides, D.; Bloem, M.W. Trends of Under- and Overweight among Rural and Urban Poor Women Indicate the Double Burden of Malnutrition in Bangladesh. Int. J. Epidemiol. 2007, 36, 449–457. [Google Scholar] [CrossRef] [PubMed]
- Galiano, L.P.; Abril, F.M.; Ernert, A.; Bau, A.-M. The Double Burden of Malnutrition and Its Risk Factors in School Children in Tunja. Arch. Latinoam. Nutr. 2012, 62, 119–126. [Google Scholar]
- Garrett, J.L.; Ruel, M.T. Stunted Child—Overweight Mother Pairs: Prevalence and Association with Economic Development and Urbanization. Food Nutr. Bull. 2005, 26, 209–221. [Google Scholar] [CrossRef] [PubMed]
- Morris, M.J.; Beilharz, J.E.; Maniam, J.; Reichelt, A.C.; Westbrook, R.F. Why Is Obesity Such a Problem in the 21st Century? The Intersection of Palatable Food, Cues and Reward Pathways, Stress, and Cognition. Neurosci. Biobehav. Rev. 2015, 58, 36–45. [Google Scholar] [CrossRef] [PubMed]
- Ng, S.W.; Zhai, F.; Popkin, B.M. Impacts of China’s Edible Oil Pricing Policy on Nutrition. Soc. Sci. Med. 2008, 66, 414–426. [Google Scholar] [CrossRef] [PubMed]
- Popkin, B.M. An Overview on the Nutrition Transition and Its Health Implications: The Bellagio Meeting. Public Health Nutr. 2002, 5, 93–103. [Google Scholar] [PubMed]
- James, W.P.T. The Fundamental Drivers of the Obesity Epidemic. Obes. Rev. 2008, 9, 6–13. [Google Scholar] [CrossRef]
- Zeba, A.N.; Delisle, H.F.; Renier, G. Dietary Patterns and Physical Inactivity, Two Contributing Factors to the Double Burden of Malnutrition among Adults in Burkina Faso, West Africa. J. Nutr. Sci. 2014, 3, e50. [Google Scholar] [CrossRef]
- Kimani-Murage, E.W.; Schofield, L.; Wekesah, F.; Mohamed, S.; Mberu, B.; Ettarh, R.; Egondi, T.; Kyobutungi, C.; Ezeh, A. Vulnerability to Food Insecurity in Urban Slums: Experiences from Nairobi, Kenya. J. Urban. Health 2014, 91, 1098–1113. [Google Scholar] [CrossRef] [Green Version]
- Caperon, L.; Arjyal, A.; Puja, K.C.; Kuikel, J.; Newell, J.; Peters, R.; Prestwich, A.; King, R. Developing a Socio-Ecological Model of Dietary Behaviour for People Living with Diabetes or High Blood Glucose Levels in Urban Nepal: A Qualitative Investigation. PLoS ONE 2019, 14, e0214142. [Google Scholar] [CrossRef] [PubMed]
- Leroy, J.L.; Habicht, J.-P.; González de Cossío, T.; Ruel, M.T. Maternal Education Mitigates the Negative Effects of Higher Income on the Double Burden of Child Stunting and Maternal Overweight in Rural Mexico. J. Nutr. 2014, 144, 765–770. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haddad, L.; Cameron, L.; Barnett, I. The Double Burden of Malnutrition in SE Asia and the Pacific: Priorities, Policies and Politics. Health Policy Plan. 2015, 30, 1193–1206. [Google Scholar] [CrossRef] [PubMed]
- Mahmudiono, T.; Nindya, T.S.; Andrias, D.R.; Megatsari, H.; Rosenkranz, R.R. The Effectiveness of Nutrition Education for Overweight/Obese Mothers with Stunted Children (NEO-MOM) in Reducing the Double Burden of Malnutrition in Indonesia: Study Protocol for a Randomized Controlled Trial. BMC Public Health 2016, 16, 486. [Google Scholar] [CrossRef]
- Prawirohartono, E.P.; Nyström, L.; Ivarsson, A.; Stenlund, H.; Lind, T. The Impact of Prenatal Vitamin A and Zinc Supplementation on Growth of Children up to 2 Years of Age in Rural Java, Indonesia. Public Health Nutr. 2011, 14, 2197–2206. [Google Scholar] [CrossRef]
- Kulsum, A.; Lakshmi, J.A.; Prakash, J. Food Intake and Energy Protein Adequacy of Children from an Urban Slum in Mysore, India—A Qualitative Analysis. Malays. J. Nutr. 2008, 14, 163–172. [Google Scholar] [PubMed]
- Pem, D.; Jeewon, R. Fruit and Vegetable Intake: Benefits and Progress of Nutrition Education Interventions—Narrative Review Article. Iran. J. Public Health 2015, 44, 1309–1321. [Google Scholar]
- Falbe, J.; Rosner, B.; Willett, W.C.; Sonneville, K.R.; Hu, F.B.; Field, A.E. Adiposity and Different Types of Screen Time. Pediatrics 2013, 132, e1497–e1505. [Google Scholar] [CrossRef] [Green Version]
- Ying, C.; Kuay, L.K.; Huey, T.C.; Hock, L.K.; Hamid, H.A.A.; Omar, M.A.; Ahmad, N.A.; Cheong, K.C. Prevalence and Factors Associated with Physical Inactivity among Malaysian Adults. Southeast Asian J. Trop. Med. Public Health 2014, 45, 467–480. [Google Scholar]
- Siddiqui, N.I.; Nessa, A.; Hossain, M.A. Regular Physical Exercise: Way to Healthy Life. Mymensingh Med. J. 2010, 19, 154–158. [Google Scholar]
- Kimani-Murage, E.W.; Muthuri, S.K.; Oti, S.O.; Mutua, M.K.; van de Vijver, S.; Kyobutungi, C. Evidence of a Double Burden of Malnutrition in Urban Poor Settings in Nairobi, Kenya. PLoS ONE 2015, 10, e0129943. [Google Scholar] [CrossRef] [PubMed]
- Klohe-Lehman, D.M.; Freeland-Graves, J.; Clarke, K.K.; Cai, G.; Voruganti, V.S.; Milani, T.J.; Nuss, H.J.; Proffitt, J.M.; Bohman, T.M. Low-Income, Overweight and Obese Mothers as Agents of Change to Improve Food Choices, Fat Habits, and Physical Activity in Their 1-to-3-Year-Old Children. J. Am. Coll. Nutr. 2007, 26, 196–208. [Google Scholar] [CrossRef] [PubMed]
- Bauman, A.E.; Sallis, J.F.; Dzewaltowski, D.A.; Owen, N. Toward a Better Understanding of the Influences on Physical Activity: The Role of Determinants, Correlates, Causal Variables, Mediators, Moderators, and Confounders. Am. J. Prev. Med. 2002, 23, 5–14. [Google Scholar] [CrossRef]
- Abegunde, D.O.; Mathers, C.D.; Adam, T.; Ortegon, M.; Strong, K. The Burden and Costs of Chronic Diseases in Low-Income and Middle-Income Countries. Lancet 2007, 370, 1929–1938. [Google Scholar] [CrossRef]
- Delisle, H.; Agueh, V.; Fayomi, B. Partnership Research on Nutrition Transition and Chronic Diseases in West Africa–Trends, Outcomes and Impacts. BMC Int. Health Hum. Rights 2011, 11, S10. [Google Scholar] [CrossRef] [PubMed]



© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mahmudiono, T.; Segalita, C.; Rosenkranz, R.R. Socio-Ecological Model of Correlates of Double Burden of Malnutrition in Developing Countries: A Narrative Review. Int. J. Environ. Res. Public Health 2019, 16, 3730. https://doi.org/10.3390/ijerph16193730
Mahmudiono T, Segalita C, Rosenkranz RR. Socio-Ecological Model of Correlates of Double Burden of Malnutrition in Developing Countries: A Narrative Review. International Journal of Environmental Research and Public Health. 2019; 16(19):3730. https://doi.org/10.3390/ijerph16193730
Chicago/Turabian StyleMahmudiono, Trias, Calista Segalita, and Richard R. Rosenkranz. 2019. "Socio-Ecological Model of Correlates of Double Burden of Malnutrition in Developing Countries: A Narrative Review" International Journal of Environmental Research and Public Health 16, no. 19: 3730. https://doi.org/10.3390/ijerph16193730
APA StyleMahmudiono, T., Segalita, C., & Rosenkranz, R. R. (2019). Socio-Ecological Model of Correlates of Double Burden of Malnutrition in Developing Countries: A Narrative Review. International Journal of Environmental Research and Public Health, 16(19), 3730. https://doi.org/10.3390/ijerph16193730







