Adapting Translational Research Methods to Water, Sanitation, and Hygiene
Abstract
:1. Introduction
2. Methods
- Translational research conceptualization,
- Actor characterization,
- Translational research categorization,
- Research type comparison,
- Practical WaSH applications, and
- Overarching good practices.
3. Results and Discussion
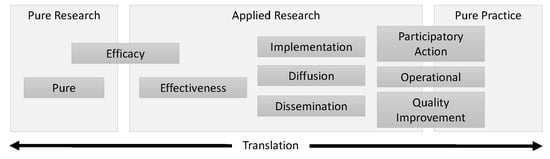
3.1. Conceptualization of Translational Research
3.2. Characterization of Actors
3.3. Comparison of Research Types
3.3.1. Purpose
3.3.2. History
3.3.3. Actors
3.3.4. Good Practices
3.4. Model Research Questions
3.5. Practical Recommendations
3.5.1. Recognize Challenges and Potential Pitfalls
3.5.2. Select a Guiding Theory and Define Terms
3.5.3. Consider Context
3.5.4. Involve Diverse Stakeholder Groups
3.5.5. Document Fidelity and Adaptations
3.5.6. Conduct Long-Term Monitoring and Evaluation
3.5.7. Revisit Results
3.5.8. Seek Continuing Education in Research Rigor and Reliability
3.6. Carrying Out Recommendations in Action: Example of Community-Led Total Sanitation
3.7. Examples and Resources for Carrying Out Translational Research Recommendations
- Koehler et al. (2018) carefully articulated how cultural theory, in the context of rural water management, provided a basis for understanding the cooperation and conflict between management cultures to handle operational, financial, institutional and environmental risk. The authors thoroughly defined terminology relevant to cultural theory and a pluralist framework at the outset of the study [169].
- Bresee et al. (2016) explained how theory informed their study design in multiple ways. Researchers aligned focus group data collection methods with diffusion of innovation theory, and based data analysis methods on grounded theory. They cited the original works that provided a basis for these approaches when reporting [107].
- Pfadenhauer et al. (2017) developed the Context and Implementation of Complex Interventions (CICI) framework for use as a determinant or evaluation framework broadly applicable to public health interventions. They describe contextual domains but do not define constructs within domains [87].
- The Consolidated Framework for Implementation Research (CFIR) outlines contextual determinants likely to influence implementation [70] and provides qualitative and quantitative tools for researchers to assess context (https://cfirguide.org/).
- Craig et al. (2018) proposed guidelines for addressing the influence of context when adapting and scaling population health interventions [132].
- West et al. (2016) investigated the effects of context on residential recycled water schemes in Australia to assess common reasons for failure. They found contextual factors such as regulatory environment, operational costs, and consumer preferences to influence success [170].
- Novotný et al. (2018) conducted a systematic review to identify which studies reported the contextual factors associated with sanitation adoption and implementation. They proposed a typology that categorizes contextual factors into societal, community, interpersonal, and individual levels [171].
- Amjad et al. (2016) used service provider interviews to assess perceived willingness and ability as measures of actor readiness for implementing the WHO’s Water Safety Plan intervention [172]. Setty et al. (2019a) used this preliminary research on context and the CFIR to inform a multi-criteria decision process for selecting appropriate intervention guidance for US source water risk management [173]. The authors recommended adapting the intervention guidance, e.g., by hybridizing with existing programs, to fit the context.
- White et al. (2008) qualitatively analyzed data from in-depth interviews with water managers to assess perceptions. They published a model for boundary organizations to mediate negotiations between scientific and political actors to inform decision making for water resources [16].
- Liu et al. (2008) applied an integrated modeling framework that engages stakeholders in every step from problem formation to monitoring and evaluation. They suggest adoption of research results and informed decision making requires open lines of communication among all parties associated with the project [174].
- Nelson et al. (2014) suggest the perspectives and values of stakeholders must be considered in the process of policy formation and decision-making. They examine the strategy of assigning roles and responsibilities to different stakeholders, concluding that engagement between actors and ‘clear messages’ from top level political entities are important factors in the provision of sanitation facilities [175].
- Sigler et al. (2014) helped to identify core components of community-led total sanitation by documenting (a) which behavior change frameworks and techniques were commonly used, (b) how implementation differs by region and context, and (c) which implementation activities were considered most valuable in achieving and sustaining desired intervention outcomes [176].
- Crocker et al. (2016) evaluated how an implementation variation to train natural leaders (motivated community members) to influence peer behaviors affected implementation and intervention outcomes for community-led total sanitation [177].
- Benjamin-Chung et al. (2017) assessed program delivery of a UNICEF intervention called Sanitation Hygiene Education and Water Supply in Bangladesh (SHEWA-B) to 20 million rural people to assess whether implementation quality affected program success, as measured by a survey of household recall. They developed an implementation quality index and compared fidelity measures, such as hygiene promotor visitation and knowledge of key messages, to outcome measures, such as health behaviors and sanitation infrastructure access [109].
- Using annual school-level data approximately 14 years after implementation of a sanitation intervention in India, Adukia (2017) demonstrated health benefits associated with school-latrine construction (especially for younger children) but not educational benefits [178].
- Cronk and Bartram (2017) aggregated existing country-level monitoring program data across Nigeria and Tanzania to develop Bayesian network models comparing diverse water system and management types. By following systems ranging from zero to more than 30 years of use, they garnered insights on water system functionality and service availability [113].
- Following a national program adopted in 2011, Senbeta and Shu (2019) studied three different management modalities (community, local government, and other external sources including non-governmental organizations) used for rural water supply sustainability in Ethiopia. Data were collected via household surveys, interviews with committee members, direct observation, and records review. They found community-management modalities performed better on most sustainability indicators [179].
- The WaSH Benefits randomized controlled trials in Kenya and Bangladesh assessed the effects on stunting and diarrhea of WaSH interventions separately and in combination with nutrition interventions. Interventions were adapted to fit the local cultural context but adhere to the same theory of change [103,180].
- The Open Science Framework (https://osf.io/) is a free scholarly commons that seeks to align practice with scientific values by improving research openness, integrity and reproducibility. They also offer a training curriculum (https://osf.io/48up3/).
- Dataverse (https://dataverse.org/) offers an open-source research data repository.
- The US National Institutes of Health provide training modules on rigor (https://www.nih.gov/research-training/rigor-reproducibility/training) as well as periodic email updates on rigor and reproducibility topics (https://www.nih.gov/research-training/rigor-reproducibility).
- The Center for Effective Global Action at the University of California, Berkeley offers in-person fee-based Research Transparency and Reproducibility Training (RT2) events in Los Angeles and London, and openly shares the training materials.
3.8. Limitations and Remaining Research Needs
4. Conclusions
- Recognizing challenges and potential pitfalls,
- Selecting an appropriate theoretical basis for study design and defining terms,
- Considering the role of context,
- Involving a diverse set of stakeholders throughout research phases,
- Documenting intervention adaptations,
- Supporting follow-up monitoring and evaluation,
- Understanding the difference between efficacy and effectiveness research and actively replicating studies in more than one setting or context, and
- Seeking ongoing training in research methods and rigor.
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- United Nations General Assembly. Transforming our world: The 2030 Agenda for Sustainable Development. In Proceedings of the General Assembley 70 sessio, New York, NY, USA, 15 September 2015; pp. 1–35. [Google Scholar]
- UN Water. Sustainable Development Goal 6 Synthesis Report on Water and Sanitation; UN Water: Geneva, Switzerland, 2018; ISBN 9789211013702. [Google Scholar]
- Prüss-Ustün, A.; Bartram, J.; Clasen, T.; Colford, J.M.; Cumming, O.; Curtis, V.; Bonjour, S.; Dangour, A.D.; De France, J.; Fewtrell, L.; et al. Burden of disease from inadequate water, sanitation and hygiene in low- and middle-income settings: A retrospective analysis of data from 145 countries. Trop. Med. Int. Heal. 2014, 19, 894–905. [Google Scholar] [CrossRef] [PubMed]
- Prüss-Ustün, A.; Wolf, J.; Bartram, J.; Clasen, T.; Cumming, O.; Freeman, M.C.; Gordon, B.; Hunter, P.R.; Medlicott, K.; Johnston, R. Burden of disease from inadequate water, sanitation and hygiene for selected adverse health outcomes: An updated analysis with a focus on low- and middle-income countries. Int. J. Hyg. Environ. Health 2019, 222, 765–777. [Google Scholar] [CrossRef] [PubMed]
- Alston, P. Report of the Special Rapporteur on Extreme Poverty and Human Rights on his Mission to the United States of America. Available online: https://digitallibrary.un.org/record/3802219?ln=en (accessed on 22 October 2019).
- Bain, R.; Johnston, R.; Mitis, F.; Chatterley, C.; Slaymaker, T. Establishing Sustainable Development Goal Baselines for Household Drinking Water, Sanitation and Hygiene Services. Water 2018, 10, 1711. [Google Scholar] [CrossRef]
- Deitz, S.; Meehan, K. Plumbing Poverty: Mapping Hot Spots of Racial and Geographic Inequality in U.S. Household Water Insecurity. Ann. Am. Assoc. Geogr. 2019, 109, 1092–1109. [Google Scholar] [CrossRef]
- Stillo, F.; Macdonald Gibson, J. Exposure to contaminated drinking water and health disparities in North Carolina. Am. J. Public Health 2017, 107, 180–185. [Google Scholar] [CrossRef]
- UNICEF; WHO. Progress on Drinking Water, Sanitation and Hygiene; UNICEF: New York, NY, USA; WHO: Geneva, Switzerland, 2017; ISBN 9789241512893. [Google Scholar]
- Setty, K.; Jimenez, A.; Willetts, J.; Leifels, M.; Bartram, J. Global water, sanitation, and hygiene research priorities and learning challenges under Sustainable Development Goal 6. Dev. Policy Rev. 2019. [Google Scholar] [CrossRef]
- Loevinsohn, M.; Mehta, L.; Cuming, K.; Nicol, A.; Cumming, O.; Ensink, J.H.J. The cost of a knowledge silo: A systematic re-review of water, sanitation and hygiene interventions. Health Policy Plan. 2015, 30, 660–674. [Google Scholar] [CrossRef]
- Cash, D.W.; Clark, W.C.; Alcock, F.; Dickson, N.M.; Eckley, N.; Guston, D.H.; Jäger, J.; Mitchell, R.B.; Jager, J.; Mitchelll, R.B. Knowledge systems for sustainable development. Proc. Natl. Acad. Sci. USA 2003, 100, 8086–8091. [Google Scholar] [CrossRef] [Green Version]
- Gustafsson, K.M.; Lidskog, R. Boundary organizations and environmental governance: Performance, institutional design, and conceptual development. Clim. Risk Manag. 2018, 19, 1–11. [Google Scholar] [CrossRef]
- Kirchhoff, C.J.; Lemos, M.C.; Engle, N.L. What influences climate information use in water management? The role of boundary organizations and governance regimes in Brazil and the U.S. Environ. Sci. Policy 2013, 26, 6–18. [Google Scholar] [CrossRef]
- Posner, S.M.; Cvitanovic, C. Evaluating the impacts of boundary-spanning activities at the interface of environmental science and policy: A review of progress and future research needs. Environ. Sci. Policy 2019, 92, 141–151. [Google Scholar] [CrossRef]
- White, D.; Corley, E.; White, M. Water managers’ perceptions of the science-policy interface in Phoenix, Arizona: Implications for an emerging boundary organization. Soc. Nat. Resour. 2008, 21, 230–243. [Google Scholar] [CrossRef]
- DFID. Maximizing the Benefits of Water Research to International Development—What Researchers Can Do. SPLASH Briefing Note 2, 1 January 2010. [Google Scholar]
- Ménard, C.; Jimenez, A.; Tropp, H. Addressing the policy-implementation gaps in water services: The key role of meso-institutions. Water Int. 2018, 43, 13–33. [Google Scholar] [CrossRef]
- Rose, D.C.; Mukherjee, N.; Simmons, B.I.; Tew, E.R.; Robertson, R.J.; Vadrot, A.B.M.; Doubleday, R.; Sutherland, W.J. Policy windows for the environment: Tips for improving the uptake of scientific knowledge. Environ. Sci. Policy 2017. [Google Scholar] [CrossRef]
- Hering, J.G. Implementation Science for the Environment. Environ. Sci. Technol. 2018, 52, 5555–5560. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nutley, S.M.; Walter, I.; Davies, H.T.O. Using evidence: How research can inform public services; Policy Press: Bristol, UK, 2007; ISBN 978 1 86134 664 3. [Google Scholar]
- Morris, Z.S.; Wooding, S.; Grant, J.; Med, J.R.S. The answer is 17 years, what is the question: Understanding time lags in translational research. J. R. Soc. Med. 2011, 104, 510–520. [Google Scholar] [CrossRef]
- Alberts, B.; Kirschner, M.W.; Tilghman, S.; Varmus, H. Rescuing US biomedical research from its systemic flaws. Proc. Natl. Acad. Sci. USA 2014, 111, 5773–5777. [Google Scholar] [CrossRef] [Green Version]
- Bauer, M.S.; Damschroder, L.; Hagedorn, H.; Smith, J.; Kilbourne, A.M. An introduction to implementation science for the non-specialist. BMC Psychol. 2015, 3, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Roberts, S.F.; Fischhoff, M.A.; Sakowski, S.A.; Feldman, E.L. Perspective: Transforming science into medicine: How clinician-scientists can build bridges across research’s “valley of Death.”. Acad. Med. 2012, 87, 266–270. [Google Scholar] [CrossRef]
- Poch, M.; Comas, J.; Cortés, U.; Sànchez-Marrè, M.; Rodríguez-Roda, I. Crossing the death valley to transfer environmental decision support systems to the water market. Glob. Chall. 2017, 1, 1700009. [Google Scholar] [CrossRef]
- Fang, F.C.; Casadevall, A. Editorial: Lost in translation - Basic science in the era of translational research. Infect. Immun. 2010, 78, 563–566. [Google Scholar] [CrossRef] [PubMed]
- Fort, D.G.; Herr, T.M.; Shaw, P.L.; Gutzman, K.E.; Starren, J.B. Mapping the evolving definitions of translational research. J. Clin. Transl. Sci. 2017, 1, 60–66. [Google Scholar] [CrossRef] [PubMed]
- Remme, J.H.F.; Adam, T.; Becerra-Posada, F.; D’Arcangues, C.; Devlin, M.; Gardner, C.; Ghaffar, A.; Hombach, J.; Kengeya, J.F.K.; Mbewu, A.; et al. Defining research to improve health systems. PLoS Med. 2010, 7. [Google Scholar] [CrossRef] [PubMed]
- Graham, I.D.; Logan, J.; Harrison, M.B.; Straus, S.E.; Tetroe, J.; Caswell, W.; Robinson, N. Lost in knowledge translation: Time for a map? J. Contin. Educ. Health Prof. 2006, 26, 13–24. [Google Scholar] [CrossRef]
- Rabin, B.A.; Brownson, R.C. Terminology for Dissemination and Implementation Research. In Dissemination and Implementation Research in Health: Translating Science to Practice; Brownson, R.C., Colditz, G.A., Proctor, E.K., Eds.; Oxford University Press: Oxford, UK, 2017; ISBN 9780190683214. [Google Scholar]
- Brown, C.H.; Curran, G.; Palinkas, L.A.; Aarons, G.A.; Wells, K.B.; Jones, L.; Collins, L.M.; Duan, N.; Mittman, B.S.; Wallace, A.; et al. An Overview of Research and Evaluation Designs for Dissemination and Implementation. Annu. Rev. Public Health 2017, 38, 1–22. [Google Scholar] [CrossRef] [Green Version]
- Dijkers, M.P.J.M. The value of “traditional” reviews in the era of systematic reviewing. Am. J. Phys. Med. Rehabil. 2009, 88, 423–430. [Google Scholar] [CrossRef]
- Aarons, G.A.; Hurlburt, M.; Horwitz, S.M.C. Advancing a conceptual model of evidence-based practice implementation in public service sectors. Adm. Policy Ment. Heal. Ment. Heal. Serv. Res. 2011, 38, 4–23. [Google Scholar] [CrossRef]
- Van der Laan, A.L.; Boenink, M. Beyond Bench and Bedside: Disentangling the Concept of Translational Research. Heal. Care Anal. 2015, 23, 32–49. [Google Scholar] [CrossRef]
- Jasanoff, S. States of Knowledge: The Co-Production of Science and Social Order; Routledge: London, UK, 2004. [Google Scholar]
- Curran, G.M.; Bauer, M.; Mittman, B.; Pyne, J.M.; Stetler, C. Effectiveness-implementation Hybrid Designs. Med. Care 2012, 50, 217–226. [Google Scholar] [CrossRef] [Green Version]
- Institute for Healthcare Improvement. IHI’s Collaborative Model for Achieving Breakthrough Improvement; Institute for Healthcare Improvement: Cambridge, MA, USA, 2003. [Google Scholar]
- Fisher, M.B. Proposed Core WaSH MEL Indicators: Monitoring for Continuous Program. Quality Improvement; The Water Institute at UNC: Chapel Hill, NC, USA, 2014. [Google Scholar]
- Gauch, H.G., Jr. Scientific Method in Brief; Cambridge University Press: Cambridge, UK, 2012; ISBN 978-1-107-66672-6. [Google Scholar]
- Tracy, S.J. Qualitative Research Methods: Collecting Evidence, Crafting Analysis, Communicating Impact; John Wiley & Sons, Ltd: Chichester, UK, 2013; ISBN 978-1-4051-9202-6. [Google Scholar]
- Fisher, R.A. The Arrangement of Field Experiments; Springer: New York, NY, USA, 1926. [Google Scholar]
- Peirce, C.S. Illustrations of the Logic of Science; Open Court: Chicago, IL, USA, 1878. [Google Scholar]
- Peirce, C.S. A Theory of Probable Inference; Little, Brown, and Company: Boston, MA, USA, 1883. [Google Scholar]
- Zwarenstein, M.; Treweek, S.; Gagnier, J.J.; Altman, D.G.; Tunis, S.; Haynes, B.; Oxman, A.D.; Moher, D. Improving the reporting of pragmatic trials: An extension of the CONSORT statement. BMJ 2008, 337, 1–8. [Google Scholar] [CrossRef]
- Mercer, S.L.; DeVinney, B.J.; Fine, L.J.; Green, L.W.; Dougherty, D. Study Designs for Effectiveness and Translation Research. Identifying Trade-offs. Am. J. Prev. Med. 2007, 33, 139–154. [Google Scholar] [CrossRef] [PubMed]
- Morra Imas, L.G.; Rist, R.C. The Road To Results: Designing and Conducting Effective Development Evaluations; The World Bank: Washington, DC, USA, 2009; ISBN 9780821378915. [Google Scholar]
- Narayanamurti, V.; Odumosu, T. Cycles of Invention and Discovery: Rethinking the Endless Frontier; Harvard University Press: Cambridge, MA, USA, 2016; ISBN 9780674967960. [Google Scholar]
- Bartram, J. Routledge Handbook of Water and Health; Bartram, J., Ed.; Routledge: Abingdon, UK; New York, NY, USA, 2015; ISBN 9781138910072. [Google Scholar]
- Rogers, E.M. Diffusion of Innovations, 5th ed.; Free Press: New York, NY, USA, 2003; ISBN 0743258231. [Google Scholar]
- Perkins, J.M.; Subramanian, S.V.; Christakis, N.A. Social networks and health: A systematic review of sociocentric network studies in low- and middle-income countries. Soc. Sci. Med. 2015, 125, 60–78. [Google Scholar] [CrossRef] [PubMed]
- Lewis, M.A. Charles Babbage: Reclaiming an operations management pioneer. J. Oper. Manag. 2007, 25, 248–259. [Google Scholar] [CrossRef]
- Encyclopedia of Operations Research and Management Science, 3rd ed.; Gass, S.I.; Fu, M.C. (Eds.) Springer: New York, NY, USA, 2013; ISBN 978-1-4419-1137-7. [Google Scholar]
- Torres, C.A. Participatory action research and popular education in latin america. Int. J. Qual. Stud. Educ. 1992, 5, 51–62. [Google Scholar] [CrossRef]
- Lewin, K. Action Research and Minority Problems. J. Soc. Issues 1946, 2, 34–46. [Google Scholar] [CrossRef]
- The New Production of Knowledge: The Dynamics of Science and Research in Contemporary Society; Gibbons, M. (Ed.) Sage Publications: Stockholm, Sweden, 1994. [Google Scholar]
- Stringer, E.T. Action Research, 4th ed.; Sage Publications: Los Angeles, CA, USA, 2013; ISBN 1452205086. [Google Scholar]
- Methods for Community-Based Participatory Research for Health, 2nd ed.; Israel, B.A.; Eng, E.; Schulz, A.J.; Parker, E.A. (Eds.) Jossey-Bass: San Francisco, CA, USA, 2013; ISBN 9781118021866. [Google Scholar]
- O’Fallon, L.R.; Dearry, A. Community-Based Participatory Research as a Tool to Advance Environmental Health Sciences. Environ. Heal. 2002, 110, 155–159. [Google Scholar] [CrossRef]
- Tsutsui, W.M.W. Edwards Deming and the Origins of Quality Control in Japan. J. Jpn. Stud. 1996, 22, 295–325. [Google Scholar] [CrossRef]
- Langley, G.J.; Moen, R.D.; Nolan, K.M.; Nolan, T.W.; Norman, C.L.; Provost, L.P. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance, 2nd ed.; Jossey-Bass: San Francisco, CA, USA, 2009; ISBN 0470430885. [Google Scholar]
- Grimshaw, J.M.; Eccles, M.P.; Lavis, J.N.; Hill, S.J.; Squires, J.E. Knowledge translation of research findings. Implement. Sci. 2012, 7, 1. [Google Scholar] [CrossRef]
- WHO; IWA. Global Status Report on Water Safety Plans: A Review of Proactive Risk Assessment and Risk Management Practices to Ensure the Safety of Drinking-Water; WHO: Geneva, Switzerland, 2017. [Google Scholar]
- WHO. Guidelines for Drinking-Water Quality, 3rd ed.; WHO: Geneva, Switzerland, 2004; Volume 1. [Google Scholar]
- Cohen, D.; Crabtree, B. Qualitative Research Guidelines Project: Action Research. Available online: http://www.qualres.org/HomeActi-3592.html (accessed on 2 August 2018).
- Baum, F.; MacDougall, C.; Smith, D. Participatory action research. J. Epidemiol. Community Health 2006, 60, 854–857. [Google Scholar] [CrossRef] [Green Version]
- Martinez, R.G.; Lewis, C.C.; Weiner, B.J. Instrumentation issues in implementation science. Implement. Sci. 2014, 9, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Nilsen, P. Making sense of implementation theories, models and frameworks. Implement. Sci. 2015, 10, 1–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rehfuess, E.A.; Bartram, J. Beyond direct impact: Evidence synthesis towards a better understanding of effectiveness of environmental health interventions. Int. J. Hyg. Environ. Health 2014, 217, 155–159. [Google Scholar] [CrossRef] [PubMed]
- Damschroder, L.J.; Aron, D.C.; Keith, R.E.; Kirsh, S.R.; Alexander, J.A.; Lowery, J.C. Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implement. Sci. 2009, 4, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Cahan, D. From Natural Philosophy to the Sciences: Writing the History of Nineteenth-Century Science; University of Chicago Press: Chicago, IL, USA; London, UK, 2003. [Google Scholar]
- Fetters, M.D.; Curry, L.A.; Creswell, J.W. Achieving integration in mixed methods designs - Principles and practices. Health Serv. Res. 2013, 48, 2134–2156. [Google Scholar] [CrossRef] [PubMed]
- Venkataramanan, V. Qualitative Methods for Water, Sanitation, Hygiene (WaSH) and Health. Available online: http://www.washmel.org/wp-content/uploads/2015/05/final-notes.pdf (accessed on 1 September 2019).
- Kaminsky, J.; Jordan, E. Qualitative comparative analysis for WASH research and practice. J. Water Sanit. Hyg. Dev. 2017, 7, 196–208. [Google Scholar] [CrossRef]
- Theobald, S.; Brandes, N.; Gyapong, M.; El-Saharty, S.; Proctor, E.; Diaz, T.; Wanji, S.; Elloker, S.; Raven, J.; Elsey, H.; et al. Implementation research: New imperatives and opportunities in global health. Lancet 2018, 392, 2214–2228. [Google Scholar] [CrossRef]
- Polk, M. Transdisciplinary co-production: Designing and testing a transdisciplinary research framework for societal problem solving. Futures 2015, 65, 110–122. [Google Scholar] [CrossRef]
- Wallerstein, N.; Duran, B. Commentary: Community-Based Participatory Research Contributions to Intervention Research: The Intersection of Science and Practice to Improve Health Equity. Am. J. Public Health 2010, 100, S40–S46. [Google Scholar] [CrossRef]
- Jiménez, A.; LeDeunff, H.; Giné, R.; Sjödin, J.; Cronk, R.; Murad, S.; Takane, M.; Bartram, J. The enabling environment for participation in water and sanitation: A conceptual framework. Water 2019, 11, 308. [Google Scholar]
- Klenk, N.L.; Meehan, K. Transdisciplinary sustainability research beyond engagement models: Toward adventures in relevance. Environ. Sci. Policy 2017, 78, 27–35. [Google Scholar] [CrossRef]
- Acosta, J.; Chinman, M.; Ebener, P.; Malone, P.S.; Paddock, S.; Phillips, A.; Scales, P.; Slaughter, M.E. An intervention to improve program implementation: Findings from a two-year cluster randomized trial of Assets-Getting To Outcomes. Implement. Sci. 2013, 8, 87. [Google Scholar] [CrossRef] [PubMed]
- Unicomb, L.; Begum, F.; Leontsini, E.; Rahman, M.; Ashraf, S.; Naser, A.M.; Nizame, F.A.; Jannat, K.; Hussain, F.; Parvez, S.M.; et al. WASH Benefits Bangladesh trial: Management structure for achieving high coverage in an efficacy trial. Trials 2018, 19, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Gilliland, C.T.; Sittampalam, G.S.; Wang, P.Y.; Ryan, P.E. The translational science training program at NIH: Introducing early career researchers to the science and operation of translation of basic research to medical interventions. Biochem. Mol. Biol. Educ. 2017, 45, 13–24. [Google Scholar] [CrossRef] [PubMed]
- Dunn, M.; Glasgow, R.; Handley, K.; Kayondo, J.K.; Kupfer, L.; Krishna, A.; Sanchez, M.; Smith, J.; Tang, S.; Tran, N.; et al. Fundamentals of Implementation Research 2012. Available online: https://www.measureevaluation.org/resources/publications/ms-12-55 (accessed on 22 October 2019).
- Morse, P.M.; Kimball, G.E. Methods of Operations Research; The MIT Press: Cambridge, MA, USA, 1970; ISBN 0 262 13005 X. [Google Scholar]
- Phillipson, J.; Lowe, P.; Proctor, A.; Ruto, E. Stakeholder engagement and knowledge exchange in environmental research. J. Environ. Manag. 2012, 95, 56–65. [Google Scholar] [CrossRef]
- Reed, M.S.; Stringer, L.C.; Fazey, I.; Evely, A.C.; Kruijsen, J.H.J. Five principles for the practice of knowledge exchange in environmental management. J. Environ. Manag. 2014, 146, 337–345. [Google Scholar] [CrossRef] [Green Version]
- Pfadenhauer, L.M.; Gerhardus, A.; Mozygemba, K.; Lysdahl, K.B.; Booth, A.; Hofmann, B.; Wahlster, P.; Polus, S.; Burns, J.; Brereton, L.; et al. Making sense of complexity in context and implementation: The Context and Implementation of Complex Interventions (CICI) fra1mework. Implement. Sci. 2017, 12, 1–17. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and Elaboration. Ann. Intern. Med. 2007, 147, 573–577. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. The PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Ogrinc, G.; Davies, L.; Goodman, D.; Batalden, P.; Davidoff, F.; Stevens, D. SQUIRE 2.0 (Standards for QUality Improvement Reporting Excellence) 2.0: Revised publication guidelines from a detailed consensus process. BMJ Qual. Saf. 2016, 25, 986–992. [Google Scholar] [CrossRef]
- Goodman, D.; Ogrinc, G.; Davies, L.; Baker, G.R.; Barnsteiner, J.; Foster, T.C.; Gali, K.; Hilden, J.; Horwitz, L.; Kaplan, H.C.; et al. Explanation and elaboration of the SQUIRE (Standards for Quality Improvement Reporting Excellence) Guidelines, V.2.0: Examples of SQUIRE elements in the healthcare improvement literature. BMJ Qual. Saf. 2016, 25, e7. [Google Scholar] [CrossRef] [PubMed]
- Pinnock, H.; Barwick, M.; Carpenter, C.R.; Eldridge, S.; Grandes, G.; Griffiths, C.J.; Rycroft-Malone, J.; Meissner, P.; Murray, E.; Patel, A.; et al. Standards for Reporting Implementation Studies (StaRI) Statement. BMJ 2017, 356, i6795. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hales, S.; Lesher-Trevino, A.; Ford, N.; Maher, D.; Ramsay, A.; Tran, N. Reporting guidelines for implementation and operational research. Bull. World Health Organ. 2016, 94, 58–64. [Google Scholar] [CrossRef] [PubMed]
- Taylor, M.J.; McNicholas, C.; Nicolay, C.; Darzi, A.; Bell, D.; Reed, J.E. Systematic review of the application of the plan-do-study-act method to improve quality in healthcare. BMJ Qual. Saf. 2014, 23, 290–298. [Google Scholar] [CrossRef] [PubMed]
- Powell, B.J.; Waltz, T.J.; Chinman, M.J.; Damschroder, L.J.; Smith, J.L.; Matthieu, M.M.; Proctor, E.K.; Kirchner, J.A.E. A refined compilation of implementation strategies: Results from the Expert Recommendations for Implementing Change (ERIC) project. Implement. Sci. 2015, 10, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Cole, B.; DeGabriele, J.; Ho, G.; Anda, M. Exploring the utility of diffusion theory to evaluate social marketing approaches to improve urban sanitation in Malawi. J. Watersanit. Hyg. Dev. 2015, 5, 289. [Google Scholar] [CrossRef]
- Kim, D.A.; Hwong, A.R.; Stafford, D.; Hughes, D.A.; O’Malley, A.J.; Fowler, J.H.; Christakis, N.A. Social network targeting to maximise population behaviour change: A cluster randomised controlled trial. Lancet 2015, 386, 145–153. [Google Scholar] [CrossRef]
- Wigginton, K.R.; Pecson, B.M.; Sigstam, T.; Bosshard, F.; Kohn, T. Virus inactivation mechanisms: Impact of disinfectants on virus function and structural integrity. Environ. Sci. Technol. 2012, 46, 12069–12078. [Google Scholar] [CrossRef]
- Domman, D.; Chowdhury, F.; Khan, A.I.; Dorman, M.J.; Mutreja, A.; Uddin, M.I.; Paul, A.; Begum, Y.A.; Charles, R.C.; Calderwood, S.B.; et al. Defining endemic cholera at three levels of spatiotemporal resolution within Bangladesh. Nat. Genet. 2018, 50, 951–955. [Google Scholar] [CrossRef]
- Rayner, J.; Luo, X.; Schubert, J.; Lennon, P.; Jellison, K.; Lantagne, D. The effects of input materials on ceramic water filter efficacy for household drinking water treatment. Water Sci. Technol. Water Supply 2016, 17, 859–869. [Google Scholar] [CrossRef]
- Reid, B.; Seu, R.; Orgle, J.; Roy, K.; Pongolani, C.; Chileshe, M.; Fundira, D.; Stoltzfus, R. A community-designed play-yard intervention to prevent microbial ingestion: A baby water, sanitation, and hygiene pilot study in rural Zambia. Am. J. Trop. Med. Hyg. 2018, 99, 513–525. [Google Scholar] [CrossRef] [PubMed]
- Luby, S.P.; Rahman, M.; Arnold, B.F.; Unicomb, L.; Ashraf, S.; Winch, P.J.; Stewart, C.P.; Begum, F.; Hussain, F.; Benjamin-Chung, J.; et al. Effects of water quality, sanitation, handwashing, and nutritional interventions on diarrhoea and child growth in rural Bangladesh: A cluster randomised controlled trial. Lancet Glob. Heal. 2018, 6, e302–e315. [Google Scholar] [CrossRef]
- Chiposa, R.; Holm, R.H.; Munthali, C.; Chidya, R.C.G.; de los Reyes, F.L. Characterization of pit latrines to support the design and selection of emptying tools in peri-urban Mzuzu, Malawi. J. Water Sanit. Hyg. Dev. 2017, 7, 151–155. [Google Scholar] [CrossRef] [Green Version]
- Omar, Y.Y.; Parker, A.; Smith, J.A.; Pollard, S.J.T. Risk management for drinking water safety in low and middle income countries - cultural influences on water safety plan (WSP) implementation in urban water utilities. Sci. Total Environ. 2017, 576, 895–906. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meierhofer, R.; Landolt, G. Factors supporting the sustained use of solar water disinfection - Experiences from a global promotion and dissemination programme. Desalination 2009, 248, 144–151. [Google Scholar] [CrossRef]
- Bresee, S.; Caruso, B.A.; Sales, J.; Lupele, J.; Freeman, M.C. “A child is also a teacher”: Exploring the potential for children as change agents in the context of a school-based WASH intervention in rural Eastern Zambia. Health Educ. Res. 2016, 31, 521–534. [Google Scholar] [CrossRef]
- Crocker, J.; Geremew, A.; Atalie, F.; Yetie, M.; Bartram, J. Teachers and Sanitation Promotion: An Assessment of Community-Led Total Sanitation in Ethiopia. Environ. Sci. Technol. 2016, 50, 6517–6525. [Google Scholar] [CrossRef] [Green Version]
- Benjamin-Chung, J.; Sultana, S.; Halder, A.K.; Ahsan, M.A.; Arnold, B.F.; Hubbard, A.E.; Unicomb, L.; Luby, S.P.; Jr, J.M.C. Scaling Up a Water, Sanitation, and Hygiene Program in Rural Bangladesh: The Role of Program Implementation. Am. J. Public Health 2017, 107, 694–702. [Google Scholar] [CrossRef]
- Ojomo, E.; Elliott, M.; Goodyear, L.; Forson, M.; Bartram, J. Sustainability and scale-up of household water treatment and safe storage practices: Enablers and barriers to effective implementation. Int. J. Hyg. Environ. Health 2015, 218, 704–713. [Google Scholar] [CrossRef] [Green Version]
- Guerra, P.; Kim, M.; Teslic, S.; Alaee, M.; Smyth, S.A. Bisphenol-A removal in various wastewater treatment processes: Operational conditions, mass balance, and optimization. J. Environ. Manag. 2015, 152, 192–200. [Google Scholar] [CrossRef]
- Torlesse, H.; Cronin, A.A.; Sebayang, S.K.; Nandy, R. Determinants of stunting in Indonesian children: Evidence from a cross-sectional survey indicate a prominent role for the water, sanitation and hygiene sector in stunting reduction. BMC Public Health 2016, 16, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Cronk, R.; Bartram, J. Factors influencing water system functionality in Nigeria and Tanzania: A regression and Bayesian network analysis. Environ. Sci. Technol. 2017, 51, acs.est.7b03287. [Google Scholar] [CrossRef] [PubMed]
- Barrington, D.J.; Sridharan, S.; Saunders, S.G.; Souter, R.T.; Bartram, J.; Shields, K.F.; Meo, S.; Kearton, A.; Hughes, R.K. Improving community health through marketing exchanges: A participatory action research study on water, sanitation, and hygiene in three Melanesian countries. Soc. Sci. Med. 2016, 171, 84–93. [Google Scholar] [CrossRef] [PubMed]
- Webb, T.; Burgin, S.; Maheshwari, B. Action research for sustainable water futures in western Sydney: Reaching beyond traditional stakeholder engagement to understand community stakeholder language and its implications for action. Syst. Pract. Action Res. 2009, 22, 1–14. [Google Scholar] [CrossRef]
- Bisung, E.; Elliott, S.J.; Abudho, B.; Karanja, D.M.; Schuster-wallace, C.J. Using photovoice as a community based participatory research tool for changing water, sanitation, and hygiene behaviours in Usoma, Kenya. Biomed. Res. Int. 2015, 1–10. [Google Scholar] [CrossRef]
- Weber, N.; Martinsen, A.L.; Sani, A.; Kokou, E.; Assigbley, E.; Azzouz, C.; Gelting, R.; Hayter, A.; Ayite, K.; Afefa, A.; et al. Strengthening healthcare facilities through water, sanitation, and hygiene (WASH) improvements: A pilot evaluation of ‘“WASH FIT”’ in Togo. Heal. Secur. 2018, 16, S54–S65. [Google Scholar] [CrossRef]
- Kallam, B.; Pettitt-Schieber, C.; Owen, M.; Asante, R.A.; Darko, E.; Ramaswamy, R. Implementation science in low-resource settings: Using the interactive systems framework to improve hand hygiene in a tertiary hospital in Ghana. Int. J. Qual. Heal. Care 2018, 30, 724–730. [Google Scholar] [CrossRef]
- Jiménez, A.; Livsey, J.; Åhlén, I.; Scharp, C.; Takane, M. Global assessment of accountability in water and sanitation services using GLAAS data. Water Altern. 2018, 11, 238–259. [Google Scholar]
- SWA Sanitation and Water for All (SWA) Framework. Available online: http://sanitationandwaterforall.org/priority-areas/swa-framework/ (accessed on 26 February 2019).
- Proctor, E.K.; Powell, B.J.; McMillen, J.C. Implementation strategies: Recommendations for specifying and reporting. Implement. Sci. 2013, 8, 1–11. [Google Scholar] [CrossRef]
- Birken, S.A.; Rohweder, C.L.; Powell, B.J.; Shea, C.M.; Scott, J.; Leeman, J.; Grewe, M.E.; Alexis Kirk, M.; Damschroder, L.; Aldridge, W.A.; et al. T-CaST: An implementation theory comparison and selection tool. Implement. Sci. 2018, 13, 143. [Google Scholar] [CrossRef]
- Roll-Hansen, N. Why the Distinction between Basic (Theoretical) and Applied (Practical) Research is Important in the Politics of Science. Available online: https://pdfs.semanticscholar.org/62f0/dced123c24c7bc89b7d0d72bfcf885634a43.pdf (accessed on 22 October 2019).
- Pfadenhauer, L.M.; Mozygemba, K.; Gerhardus, A.; Hofmann, B.; Booth, A.; Lysdahl, K.B.; Tummers, M.; Burns, J.; Rehfuess, E.A. Context and implementation: A concept analysis towards conceptual maturity. Z. Evid. Fortbild. Qual. Gesundhwes. 2015, 109, 103–114. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Øvretveit, J. Understanding the conditions for improvement: Research to discover which context influences affect improvement success. BMJ Qual. Saf. 2011, 20, 1–6. [Google Scholar]
- McDonald, K.M. Considering context in quality improvement interventions and implementation: Concepts, frameworks, and application. Acad. Pediatr. 2013, 13, S45–S53. [Google Scholar] [CrossRef] [PubMed]
- Peters, D.H.; Adam, T.; Alonge, O.; Agyepong, I.A.; Tran, N. Implementation research: What it is and how to do it. BMJ 2013, 347, f6753. [Google Scholar] [PubMed]
- Kaplan, H.C.; Brady, P.W.; Dritz, M.C.; Hooper, D.K.; Linam, W.M.; Froehle, C.M.; Margolis, P.; Linam, M.; Froehle, C.M.; Margolis, P. The influence of context on quality improvement success in health care. Milbank Q. 2008, 86, 529–532. [Google Scholar]
- Hamilton, A.B.; Mittman, B.S. Implementation Science in Health Care. In Dissemination and Implementation Research in Health: Translating Science to Practice; Brownson, R.C., Colditz, G.A., Proctor, E.K., Eds.; Oxford Scholarship: Oxford, UK, 2017; ISBN 9780190683214. [Google Scholar]
- Jacobs, S.; Weiner, B.; Bunger, A.C. Context matters: Measuring implementation climate among individuals and groups. Implement. Sci. 2014, 4, 46. [Google Scholar] [CrossRef]
- May, C.R.; Johnson, M.; Finch, T. Implementation, context and complexity. Implement. Sci. 2016, 11, 1–12. [Google Scholar] [CrossRef]
- Craig, P.; Di Ruggiero, E.; Frohlich, K.L.; Mykhalovskiy, E.; White, M.; Campbell, R.; Cummins, S.; Edwards, N.; Hunt, K.; Kee, F.; et al. Taking Account of Context in Population Health Intervention Research: Guidance for Producers, Users and Funders of Research; NIHR Evaluation, Trials and Studies Coordinating Centre: Glasgow, UK, 2018. [Google Scholar]
- Saywell, D.; Crocker, J. Process learning on partnerships: Building functioning research and practice organizational relationships. Waterlines 2019, 38, 3–19. [Google Scholar] [CrossRef]
- Rehfuess, E.A.; Durao, S.; Kyamanywa, P.; Meerpohl, J.J.; Young, T.; Rohwer, A. An approach for setting evidence-based and stakeholder-informed research priorities in low- and middle-income countries. Bull. World Health Organ. 2016, 94, 297–305. [Google Scholar] [CrossRef]
- DFID. Maximizing the Benefits of Water Research to International Development—What Researchers Can Do. Available online: https://splash-era.net/downloads/SPLASH_Briefing_note_02.pdf (accessed on 22 October 2019).
- Klug, T.; Shields, K.F.; Cronk, R.; Kelly, E.; Behnke, N.; Lee, K.; Bartram, J. Water system hardware and management rehabilitation: Qualitative evidence from Ghana, Kenya, and Zambia. Int. J. Hyg. Environ. Health 2017, 220, 531–538. [Google Scholar] [CrossRef] [Green Version]
- Kelly, E.; Lee, K.; Shields, K.F.; Cronk, R.; Behnke, N.; Klug, T.; Bartram, J. The role of social capital and sense of ownership in rural community-managed water systems: Qualitative evidence from Ghana, Kenya, and Zambia. J. Rural Stud. 2017, 56, 156–166. [Google Scholar] [CrossRef]
- Behnke, N.L.; Klug, T.; Cronk, R.; Shields, K.F.; Lee, K.; Kelly, E.R.; Allgood, G.; Bartram, J. Resource mobilization for community-managed rural water systems: Evidence from Ghana, Kenya, and Zambia. J. Clean. Prod. 2017, 156, 437–444. [Google Scholar] [CrossRef]
- Kelly, E.; Shields, K.F.; Cronk, R.; Lee, K.; Behnke, N.; Klug, T.; Bartram, J. Seasonality, water use and community management of water systems in rural settings: Qualitative evidence from Ghana, Kenya, and Zambia. Sci. Total Environ. 2018, 628–629, 715–721. [Google Scholar] [CrossRef] [PubMed]
- Proctor, E.; Silmere, H.; Raghavan, R.; Hovmand, P.; Aarons, G.; Bunger, A.; Griffey, R.; Hensley, M. Outcomes for Implementation Research: Conceptual Distinctions, Measurement Challenges, and Research Agenda. Adm. Policy Ment. Health 2011, 38, 65–76. [Google Scholar] [CrossRef] [PubMed]
- Saunders, S.G.; Barrington, D.J.; Sridharan, S.; Meo, S.; Hadwen, W.; Shields, K.F.; Souter, R.; Bartram, J.K. Addressing WaSH challenges in Pacific Island Countries: A participatory marketing systems mapping approach to empower informal settlement community action. Habitat Int. 2016, 55, 159–166. [Google Scholar] [CrossRef]
- Carroll, C.; Patterson, M.; Wood, S.; Booth, A.; Rick, J.; Balain, S. A conceptual framework for implementation fidelity. Implement. Sci. 2007, 2, 1–9. [Google Scholar] [CrossRef]
- Blase, K.; Fixsen, D. Core Intervention Components:Identifying and Operationalizing What Makes Programs Work. Available online: https://eric.ed.gov/?id=ED541353 (accessed on 22 October 2019).
- Allen, J.D.; Shelton, R.C.; Emmons, K.M.; Linnan, L.A. Fidelity and Its Relationship to Implementation Effectiveness, Adaptation, and Dissemination. In Dissemination and Implementation Research in Health; Brownson, R.C., Colditz, G.A., Proctor, E.K., Shelton, R.C., Emmons, K.M., Linnan, L.A., Eds.; Oxford University Press: Oxford, UK, 2017; pp. 1–41. ISBN 9780190683214. [Google Scholar]
- Baumann, A.A.; Cabassa, L.J.; Stirman, S.W. Adaptation in Dissemination and Implementation Science. In Dissemination and Implementation Research in Health: Translating Science to Practice; Brownson, R.C., Colditz, G.A., Proctor, E.K., Baumann, A.A., Eds.; Oxford Scholarship: Oxford, USA, 2017; ISBN 9780190683214. [Google Scholar]
- Wolf, J.; Hunter, P.R.; Freeman, M.C.; Cumming, O.; Clasen, T.; Bartram, J.; Higgins, J.P.T.; Johnston, R.; Medlicott, K.; Boisson, S.; et al. Impact of drinking water, sanitation and handwashing with soap on childhood diarrhoeal disease: Updated meta-analysis and meta-regression. Trop. Med. Int. Heal. 2018, 23, 508–525. [Google Scholar] [CrossRef]
- Venkataramanan, V. Testing CLTS Approaches for Scalability CLTS Learning Series: Lessons from CLTS Implementation in Seven Countries; The Water Institute at UNC: Washington, DC, USA; Chapel Hill, NC, USA, 2016. [Google Scholar]
- Newhart, K.B.; Holloway, R.W.; Hering, A.S.; Cath, T.Y. Data-driven performance analyses of wastewater treatment plants: A review. Water Res. 2019, 157, 498–513. [Google Scholar] [CrossRef]
- Clasen, T.; Roberts, I.; Rabie, T.; Schmidt, W.; Cairncross, S. Cochrane review: Interventions to improve water quality for preventing diarrhoea. Evid. -Based Child. Heal. A Cochrane Rev. J. 2007, 2, 226–329. [Google Scholar] [CrossRef]
- Ejemot-Nwadiaro, R.I.; Ehiri, J.E.; Arikpo, D.; Meremikwu, M.M.; Critchley, J.A. Hand Washing Promotion for Preventing Diarrhoea (Review). Available online: https://www.cochrane.org/CD004265/INFECTN_hand-washing-promotion-preventing-diarrhoea (accessed on 22 October 2019).
- Freeman, M.C.; Garn, J.V.; Sclar, G.D.; Boisson, S.; Medlicott, K.; Alexander, K.T.; Penakalapati, G.; Anderson, D.; Mahtani, A.G.; Grimes, J.E.T.; et al. The impact of sanitation on infectious disease and nutritional status: A systematic review and meta-analysis. Int. J. Hyg. Environ. Health 2017, 220, 928–949. [Google Scholar] [CrossRef]
- Glasgow, R.E.; Lichtenstein, E.; Marcus, A.C. Why Don’t We See More Translation of Health Promotion Research to Practice? Rethinking the Efficacy-to-Effectiveness Transition. 2003, 93, 1261–1267. Am. J. Public Health 2003, 93, 1261–1267. [Google Scholar] [CrossRef] [PubMed]
- Glasgow, R.E.; Chambers, D. Developing Robust, Sustainable, Implementation Systems Using Rigorous, Rapid and Relevant Science. Clin. Transl. Sci. 2012, 5, 48–55. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- International Committee of Medical Journal Editors. Recommendations for the Conduct, Reporting, Editing, and Publication of Scholarly Work in Medical Journals. Available online: http://www.icmje.org/icmje-recommendations.pdf (accessed on 22 October 2019).
- Bartram, J.; Charles, K.; Evans, B.; O’hanlon, L.; Pedley, S. Commentary on community-led total sanitation and human rights: Should the right to community-wide health be won at the cost of individual rights? J. Water Health 2012, 10, 499–503. [Google Scholar] [CrossRef] [PubMed]
- Bateman, M.; Engel, S. To shame or not to shame—that is the sanitation question. Dev. Policy Rev. 2018, 36, 155–173. [Google Scholar] [CrossRef]
- Mosler, H.J. A systematic approach to behavior change interventions for the water and sanitation sector in developing countries: A conceptual model, a review, and a guideline. Int. J. Environ. Health Res. 2012, 22, 431–449. [Google Scholar] [CrossRef]
- Dreibelbis, R.; Winch, P.J.; Leontsini, E.; Hulland, K.R.; Ram, P.K.; Unicomb, L.; Luby, S.P. The Integrated Behavioural Model for Water, Sanitation, and Hygiene: A systematic review of behavioural models and a framework for designing and evaluating behaviour change interventions in infrastructure-restricted settings. BMC Public Health 2013, 13, 1015. [Google Scholar] [CrossRef]
- Harter, M.; Mosch, S.; Mosler, H.J. How does Community-Led Total Sanitation (CLTS) affect latrine ownership? A quantitative case study from Mozambique. BMC Public Health 2018, 18, 1–10. [Google Scholar] [CrossRef]
- Alemu, F.; Kumie, A.; Medhin, G.; Gebre, T.; Godfrey, P. A socio-ecological analysis of barriers to the adoption, sustainablity and consistent use of sanitation facilities in rural Ethiopia. BMC Public Health 2017, 17, 1–9. [Google Scholar] [CrossRef]
- McMichael, C.; Robinson, P. Drivers of sustained hygiene behaviour change: A case study from mid-western Nepal. Soc. Sci. Med. 2016, 163, 28–36. [Google Scholar] [CrossRef]
- Crocker, J.; Saywell, D.; Bartram, J. Sustainability of community-led total sanitation outcomes: Evidence from Ethiopia and Ghana. Int. J. Hyg. Environ. Health 2017, 220, 551–557. [Google Scholar] [CrossRef]
- Kar, K.; Chambers, R. Community-Led Total Sanitation Handbook; Plan UK and Institute of Development Studies at the University of Sussex: London, UK, 2008; ISBN 9780955047954. [Google Scholar]
- Chambers, R. Sharing and co-generating knowledges: Reflections on experiences with PRA and CLTS. Ids Bull. 2012, 43, 71–87. [Google Scholar] [CrossRef]
- Lüthi, C.; McConville, J.; Kvarnström, E. Community-based approaches for addressing the urban sanitation challenges. Int. J. Urban. Sustain. Dev. 2010, 1, 49–63. [Google Scholar] [CrossRef]
- Myers, J.; Cavill, S.; Musyoki, S.; Pasteur, K.; Stevens, L. Innovations for Urban. Sanitation; Practical Action Publishing: Rugby, UK, 2018; ISBN 978-1-78044-738-4. [Google Scholar]
- Tyndale-Biscoe, P.; Bond, M.; Kidd, R. ODF Sustainability Study. Available online: https://www.communityledtotalsanitation.org/sites/communityledtotalsanitation.org/files/Plan_International_ODF_Sustainability_Study.pdf (accessed on 22 October 2019).
- Cameron, L.; Olivia, S.; Shah, M. Scaling up sanitation: Evidence from an RCT in Indonesia. J. Dev. Econ. 2019, 138, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Koehler, J.; Rayner, S.; Katuva, J.; Thomson, P.; Hope, R. A cultural theory of drinking water risks, values and institutional change. Glob. Environ. Chang. 2018, 50, 268–277. [Google Scholar] [CrossRef]
- West, C.; Kenway, S.; Hassall, M.; Yuan, Z. Why do residential recycled water schemes fail? A comprehensive review of risk factors and impact on objectives. Water Res. 2016, 102, 271–281. [Google Scholar] [CrossRef]
- Novotný, J.; Hasman, J.; Lepič, M. Contextual factors and motivations affecting rural community sanitation in low- and middle-income countries: A systematic review. Int. J. Hyg. Environ. Health 2018, 221, 121–133. [Google Scholar] [CrossRef]
- Amjad, U.Q.; Luh, J.; Baum, R.; Bartram, J. Water safety plans: Bridges and barriers to implementation in North Carolina. J. Water Health 2016, 14, 816–826. [Google Scholar] [CrossRef]
- Setty, K.; McConnell, R.; Raucher, R.; Bartram, J. Comparative evaluation of risk management frameworks for U.S. source waters. Awwa Water Sci. 2019, 1, e1125. [Google Scholar] [CrossRef]
- Liu, Y.; Gupta, H.; Springer, E.; Wagener, T. Linking science with environmental decision making: Experiences from an integrated modeling approach to supporting sustainable water resources management. Environ. Model. Softw. 2008, 23, 846–858. [Google Scholar] [CrossRef]
- Nelson, E.; Bjorn, N.; Kjellen, M.; Noel, S.; Weitz, N. Multi-level sanitation governance: Understanding and overcoming challenges in the sanitation sector in sub-Saharan Africa. Waterlines 2014, 33, 243–256. [Google Scholar]
- Sigler, R.; Mahmoudi, L.; Graham, J.P. Analysis of behavioral change techniques in community-led total sanitation programs. Health Promot. Int. 2015, 30, 16–28. [Google Scholar] [CrossRef] [PubMed]
- Crocker, J.; Abodoo, E.; Asamani, D.; Domapielle, W.; Gyapong, B.; Bartram, J. Impact Evaluation of Training Natural Leaders during a Community-Led Total Sanitation Intervention: A Cluster-Randomized Field Trial in Ghana. Environ. Sci. Technol. 2016, 50, 8867–8875. [Google Scholar] [CrossRef] [PubMed]
- Adukia, A. Sanitation and Education. Am. Econ. J. Appl. Econ. 2017, 9, 23–59. [Google Scholar] [CrossRef] [Green Version]
- Senbeta, F.M.; Shu, Y. Project implementation management modalities and their implications on sustainability ofwater services in rural areas in Ethiopia: Are community-managed projects more effective? Sustainability 2019, 11, 1675. [Google Scholar] [CrossRef]
- Null, C.; Stewart, C.P.; Pickering, A.J.; Dentz, H.N.; Arnold, B.F.; Arnold, C.D.; Benjamin-Chung, J.; Clasen, T.; Dewey, K.G.; Fernald, L.C.H.; et al. Effects of water quality, sanitation, handwashing, and nutritional interventions on diarrhoea and child growth in rural Kenya: A cluster-randomised controlled trial. Lancet Glob. Heal. 2018, 6, e316–e329. [Google Scholar] [CrossRef]
- Gunnarsdottir, M.J.; Gardarsson, S.M.; Elliott, M.; Sigmundsdottir, G.; Bartram, J. Benefits of Water Safety Plans: Microbiology, Compliance, and Public Health. Environ. Sci. Technol. 2012, 46, 7782–7789. [Google Scholar] [CrossRef]
- Setty, K.; Kayser, G.; Bowling, M.; Enault, J.; Loret, J.F.; Serra, C.P.; Alonso, J.M.; Mateu, A.P.; Bartram, J. Water quality, compliance, and health outcomes among utilities implementing Water Safety Plans in France and Spain. Int. J. Hyg. Environ. Health 2017, 220, 513–530. [Google Scholar] [CrossRef]
- UN Sustainable Development Goals. 17 Goals to Transform Our World. Available online: http://www.un.org/sustainabledevelopment/water-and-sanitation/ (accessed on 29 June 2018).
- Dunn, G.; Laing, M. Policy-makers perspectives on credibility, relevance and legitimacy (CRELE). Environ. Sci. Policy 2017, 76, 146–152. [Google Scholar] [CrossRef]

| Roles in Translational Research | ||||||
|---|---|---|---|---|---|---|
| Individual or Collective Actors 2 | Fund Research | Lead Research Investiga-tions | Interpret and/or Communicate Research | Provide Policies, Guidance, Technical Assistance, and/or Facilitation (“Decision Makers”) | Implement Practices (“Service Providers”) | Receive Services/Engage in Behaviors |
| Professional Actors | ||||||
| Researchers | X | X | ||||
| Educators | X | |||||
| Governments | X | X | X | X | X | |
| Multilateral organizations | X | X | X | X | X | |
| Service providers | X | X | X | |||
| Civil society organizations | X | X | X | |||
| Policymakers | X | X | X | |||
| Businesses | X | X | X | X | ||
| Foundations | X | X | ||||
| Networks | X | X | ||||
| Media | X | |||||
| Non-Professional Actors | ||||||
| Volunteers | X | X | X | |||
| General Public | X | X | ||||
| Research Type (Related or Commonly Used Associated Terms) | Purpose | History/ Origins | Primary Actors | Good Practices | Resources for More Information |
|---|---|---|---|---|---|
| Pure (fundamental, basic) | Observe, describe, question, hypothesize, experiment, and develop theory | Scientific method (17th century) | Researchers | Expand knowledge; avoid bias; share findings among scientific community to develop evidence base | Scientific Method in Brief [40]; Qualitative Research Methods: Collecting Evidence, Crafting Analysis, Communicating Impact [41] |
| Efficacy (comparative efficacy) | Determine if an intervention produces desired results in controlled or limited settings | 18th–20th centuries; randomized design (e.g., Peirce, Fisher) [42,43,44] | Researchers | Systematic experimentation or observation; avoid confounding (e.g., via blinding, matched controls, randomization); offer measure of statistical certainty | Improving the reporting of pragmatic trials: An extension of the CONSORT statement [45]; |
| Effectiveness (comparative effectiveness) | Determine if an intervention produces desired results in diverse real-world settings | 18th–20th centuries; randomized design (e.g., Peirce, Fisher) [42,43,44] | Researchers | Systematic experimentation or observation; understand confounding; offer measure of statistical certainty | Study designs for effectiveness and translation research: identifying trade-offs [46]; The road to results: designing and conducting effective development evaluations [47] |
| Applied 1 | Apply science with intention to address a practical problem | 18th–20th centuries; especially post-WWII | Researchers; service providers; decision-makers | Problem- or client-driven; may or may not lead to invention | Cycles of invention and discovery: Rethinking the endless frontier [48]; Routledge Handbook of Water and Health [49] |
| Diffusion | Examine how novel ideas and practices (often passively) spread among groups of people | Rogers (1962) Theory of Diffusion of Innovation | Researchers; service providers; decision-makers | Classify adopters by stages; study channels, rates, variables (e.g., member characteristics), and consequences | Diffusion of innovations, 5th edition [50]; Social networks and health: A systematic review of sociocentric network studies in low- and middle-income countries [51] |
| Dissemination | Target (often active) distribution of information or an intervention to (a) specific audience(s) | Rogers (1962) Theory of Diffusion of Innovation; government initiatives beginning in late-1990s and early-2000s (e.g., US National Institutes of Health) | Researchers; service providers; decision-makers | Identify potential adopters; facilitate uptake and effective use of specific (implicitly evidence-based) interventions | An overview of research and evaluation designs for dissemination and implementation [32] |
| Implementation (knowledge translation) | Develop methods to promote uptake of research and evidence-based practices into routine practice | Dedicated Implementation Science journal begun in 2006, following evidence-based movement of 1990s and recognition of science-to-service gap | Service providers; researchers (as external facilitators) | Grounded in theory; trans-disciplinary research teams; evidence-based practice, barrier and strategy selection; documenting context and adaptations | An introduction to implementation science for the non-specialist [24] |
| Operations/ operational (analytics, systems analysis, management science) | Apply scientific principles to business management, providing quantitative basis for complex decisions | Babbage (1840s); military planning during World Wars I and II (early-mid 1900s) [52] | Service providers; researchers | Often uses simulation, modeling, mathematical, or statistical techniques; practical objective to optimize complex systems | Encyclopedia of operations research and management science [53]; Structured Operational Research and Training IniTiative (SORT IT) from Médecins Sans Frontières (https://msf.lu/de/node/283) |
| Participatory action (action, community-based participatory, transdisciplinary) | Undertake self-reflective enquiry to solve social problems, create change to improve quality of life | Popular education (1930s) [54]; Lewin’s (1946) work on action research and minority problems [55]; theories of transdisciplinary knowledge co-production [36,56] | Civil society, service providers, community organizations, and/or public (acting as researchers); researchers | Equitable involvement; shared decision-making and ownership; critical self-examination; empower participants to develop and implement improvements | Action research, 4th ed. [57]; Methods in community-based participatory research for health [58]; Community-based participatory research as a tool to advance environmental health sciences [59]; Michigan Public Health Training Center online course “CBPR: A Partnership Approach for Public Health” (https://www.mitrainingcenter.org/courses/cbprs0218) |
| Quality improvement (improvement science) | Design and trial strategies to improve specific problem within specific system | Deming (1950s) [60]; Institute for Healthcare Improvement (IHI) Model for Improvement (2003) | Service providers; researchers (as external facilitators) | Create effective change by repeating plan-do-check-act (PDCA) or plan-do-study-act (PDSA) cycles | The improvement guide [61]; Public Health Foundation (phf.org) |
| Research Type | Model Research Question (Linked to End Goal/Outcome) | Example Studies | Specific Research Questions |
|---|---|---|---|
| Pure | How can we understand a phenomenon? Can we measure ___? Does evidence support theory? How are phenomena related? | Virus inactivation mechanisms: Impact of disinfectants on virus function and structural integrity [99] Defining endemic cholera at three levels of spatiotemporal resolution within Bangladesh [100] | How are viral functions affected by exposure to inactivating treatments? What does whole-genome sequencing tell us about cholera diversity and transmission dynamics at individual, household, regional and intercontinental scales? |
| Efficacy | Does intervention work in a controlled setting or specific population? | The effects of input materials on ceramic water filter efficacy for household drinking water treatment [101] A community-designed play-yard intervention to prevent microbial ingestion: A baby water, sanitation, and hygiene pilot study in rural Zambia [102] | How do production methods and quality control protocols alter efficacy of ceramic drinking water filters? Did a novel play-yard intervention help rural farming families reduce infant and young children’s exposure to human and free-range livestock feces? |
| Effectiveness | Does intervention work in real-world settings? | Effects of water quality, sanitation, handwashing, and nutritional interventions on diarrhea and child growth in rural Bangladesh: a cluster randomized controlled trial [103] | Do individual water, sanitation, handwashing, or nutrition interventions reduce linear growth faltering? Are combined water, sanitation, and handwashing interventions more effective at reducing diarrhea than individual interventions? Does the combination of water, sanitation, handwashing, and nutrition interventions reduce growth faltering more than each individual intervention? |
| Applied | What type of intervention might solve a problem? Does intervention fulfill an identified need? Should intervention be modified? | Characterization of pit latrines to support the design and selection of emptying tools in peri-urban Mzuzu, Malawi [104] | What characteristics of household pit latrines are important when designing and selecting pit latrine-emptying tools? |
| Diffusion | How or why does intervention spread (often passively)? Who carries information? | Exploring the utility of diffusion theory to evaluate social marketing approaches to improve urban sanitation in Malawi [97] Risk management for drinking water safety in low and middle income countries–cultural influences on water safety plan (WSP) implementation in urban water utilities [105] | Do ‘first movers’ display characteristics of innovators including relatively high incomes and risk-taking behaviors? What is the role of interpersonal information sources (opinion leaders and change agents) on the decision-making process of ‘first movers’ of the ecological toilet? Do ‘first movers’ report all five attributes described by Rogers (2003) [50] (relative advantage, compatibility, simplicity, observability and trialability) as positive reasons for purchasing the ecological toilet? How do cultural constructs in different countries influence implementation of the water safety plan intervention? |
| Dissemination | How can we (often actively) facilitate spread of an intervention? Who or what influences spread of the intervention? | Factors supporting the sustained use of solar water disinfection—experiences from a global promotion and dissemination program [106] Social network targeting to maximize population behaviour change: A cluster randomized controlled trial [98] “A child is also a teacher”: exploring the potential for children as change agents in the context of a school-based WASH intervention in rural Eastern Zambia [107] | Which factors influenced acceptance and sustained use of a solar water disinfection intervention? Which methods of targeting influential individuals produce the greatest cascades or spillover effects? Can children can influence their families to adopt healthy WASH behaviors in Eastern Zambia? If so, how? |
| Implementation | How can we scale an evidence-based intervention effectively? | Teachers and sanitation promotion: an assessment of community-led total sanitation in Ethiopia [108] Scaling up a water, sanitation, and hygiene program in rural Bangladesh: the role of program implementation [109] Sustainability and scale-up of household water treatment and safe storage practices: enablers and barriers to effective implementation [110] | How did context and process (implementation arrangements) influence effectiveness of the community-led total sanitation intervention? How did the implementation process influence achievement of desired intervention outcomes? What are the barriers and enablers for sustaining and scaling up household water treatment and safe storage practices such as boiling, chlorination, and filtration? |
| Operations/ Operational | How can we better understand and intervene on the factors affecting ongoing operational or systems processes? | Bisphenol-A removal in various wastewater treatment processes: Operational conditions, mass balance, and optimization [111] Determinants of stunting in Indonesian children: evidence from a cross-sectional survey indicate a prominent role for the water, sanitation and hygiene sector in stunting reduction [112] Factors influencing water system functionality in Nigeria and Tanzania: a regression and Bayesian network analysis [113] | Which operational conditions promoted BPA removal during wastewater treatment? What variables were statistically associated with stunting in Indonesian children? What were the data relationships between water system functionality and poverty, population density, groundwater availability, and distance to urban centers? |
| Participatory action | How can we work collectively to create knowledge to address a problem? | Improving community health through marketing exchanges: A participatory action research study on water, sanitation, and hygiene in three Melanesian countries [114] Action research for sustainable water futures in western Sydney [115] Using photovoice as a community based participatory research tool for changing water, sanitation, and hygiene behaviours in Usoma, Kenya [116] | How did impoverished communities in urban and peri-urban areas attempt to meet their water, sanitation, and hygiene needs through marketing exchange? How do people who are ‘hard to reach’ or seen as ‘apathetic’ engage using an ‘action-conversations’ tool that explores the social climate for action? How can scientific or technical messages be framed in the language of the community? What are local perceptions and practices around water-health linkages? Did photovoice tool help participants actively engage and/or change their behaviors? |
| Quality improvement | How can we adjust systems to achieve a desired improvement? | Strengthening healthcare facilities through water, sanitation, and hygiene improvements: A pilot evaluation of ‘‘WASH FIT’’ in Togo [117] Implementation science in low-resource settings: Using the interactive systems framework to improve hand hygiene in a tertiary hospital in Ghana [118] | How does the continuous improvement tool work? What are the implementation outcomes? Is the tool acceptable and feasible? Can a quality improvement intervention improve hand hygiene compliance in low-resource settings? |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Setty, K.; Cronk, R.; George, S.; Anderson, D.; O’Flaherty, G.; Bartram, J. Adapting Translational Research Methods to Water, Sanitation, and Hygiene. Int. J. Environ. Res. Public Health 2019, 16, 4049. https://doi.org/10.3390/ijerph16204049
Setty K, Cronk R, George S, Anderson D, O’Flaherty G, Bartram J. Adapting Translational Research Methods to Water, Sanitation, and Hygiene. International Journal of Environmental Research and Public Health. 2019; 16(20):4049. https://doi.org/10.3390/ijerph16204049
Chicago/Turabian StyleSetty, Karen, Ryan Cronk, Shannan George, Darcy Anderson, Għanja O’Flaherty, and Jamie Bartram. 2019. "Adapting Translational Research Methods to Water, Sanitation, and Hygiene" International Journal of Environmental Research and Public Health 16, no. 20: 4049. https://doi.org/10.3390/ijerph16204049
APA StyleSetty, K., Cronk, R., George, S., Anderson, D., O’Flaherty, G., & Bartram, J. (2019). Adapting Translational Research Methods to Water, Sanitation, and Hygiene. International Journal of Environmental Research and Public Health, 16(20), 4049. https://doi.org/10.3390/ijerph16204049