Workplace-Based Organizational Interventions Promoting Mental Health and Happiness among Healthcare Workers: A Realist Review
Abstract
1. Introduction
2. Methods
2.1. Search Strategy
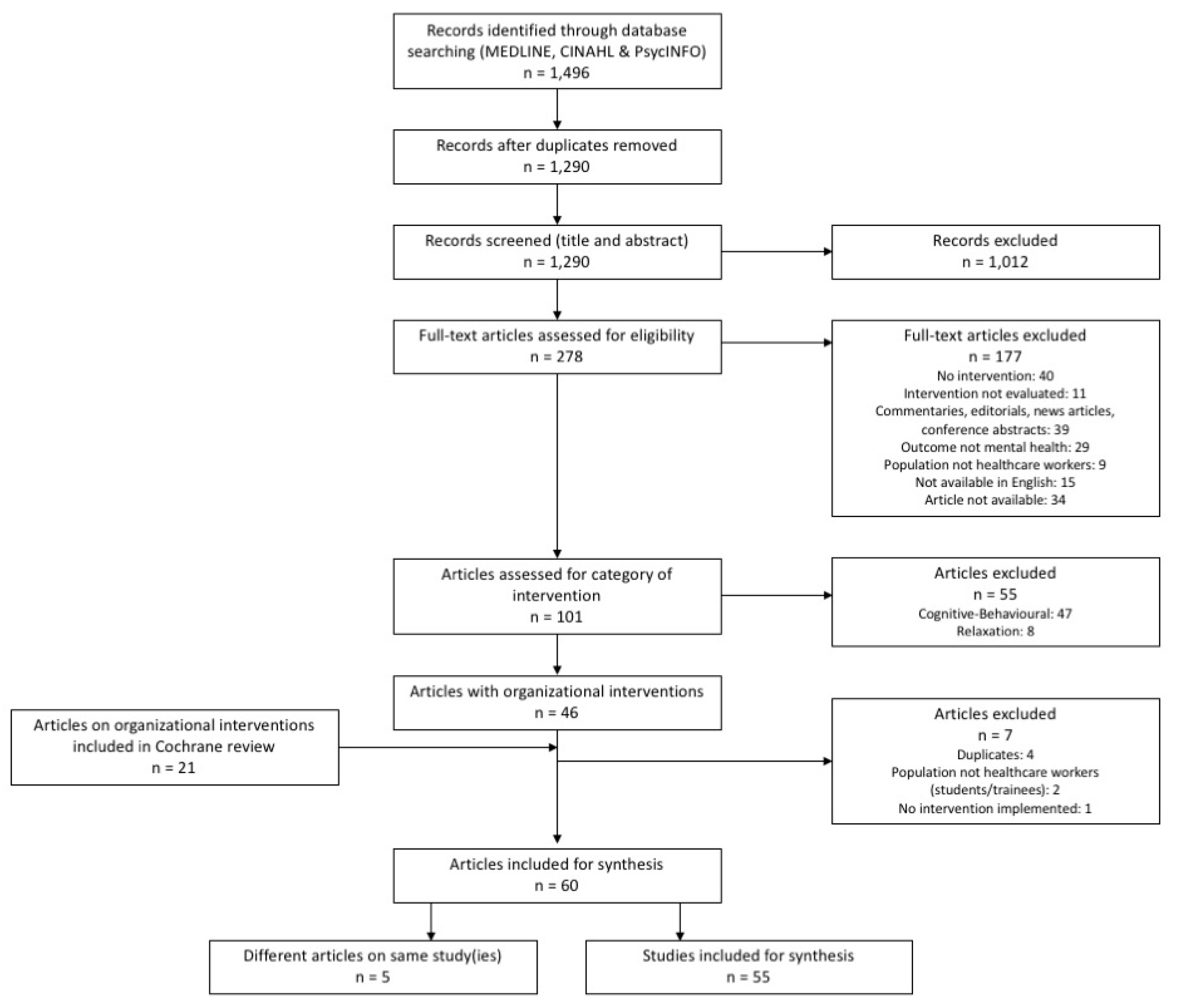
2.2. Selection and Appraisal of Documents
2.3. Data Extraction
2.4. Analysis and Synthesis Processes
3. Results
3.1. Document Characteristics
3.2. Main Findings
3.3.1. Stakeholder Engagement and Support
3.3.2. Approaches to Developing Interventions
3.3.3. Managing Expectations
3.3.4. Complexity of Evaluating Organizational-Level Interventions
3.3.5. Process vs. Mechanism
3.3.6. Sustainability and Longevity of Interventions
3.3.7. Broad Definition of Mental Health
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
- exp health personnel/
- (health* adj (provider* or professional* or worker* or staff*)).tw.
- (physician* or nurs*).tw.
- 1 or 2 or 3
- occupational stress/ or burnout, professional/
- mental health/ or resilience, psychological/ or exp mental disorders/
- “Quality of Life”/ or Personal Satisfaction/
- (mental health or life satisfaction or burnout or happiness).tw.
- 5 or 6 or 7 or 8
- Workplace/
- (workplace* or employer*).tw.
- 10 or 11
- (interven* or program* or implement* or activit* or participat* or effective* or evaluat*).m_titl.
- pc.fs.
- 13 or 14
- 4 and 9 and 12 and 15
- (MH “Health Personnel+”)
- AB health* n1 (provider* or professional* or worker* or staff*)
- AB (physician* or nurs*)
- S1 OR S2 OR S3
- (MH “Stress, Occupational+”) OR (MH “Burnout, Professional+”)
- (MH “Mental Disorders+”) OR (MH “Mental Disorders, Chronic”)
- “resilience”
- (MH “Adaptation, Psychological+”)
- (MH “Quality of Life+”) OR (MH “Quality of Working Life”)
- (MH “Personal Satisfaction+”)
- AB (mental health or life satisfaction or burnout or happiness)
- S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11
- (MH “Work Environment+”)
- AB (workplace* or employer*)
- S13 OR S14
- TI (interven* or program* or implement* or activit* or participat* or effective* or evaluat*)
- S4 AND S12 AND S15 AND S16
- MA health personnel
- AB health* n1 (provider* or professional* or worker* or staff*)
- AB physician* or nurs*
- S1 OR S2 OR S3
- AB stress, occupational OR AB burnout, professional
- AB mental disorders or mental health or mental illness
- AB resilience
- AB adaptation, psychological
- AB (quality of life or wellbeing or wellbeing or health-related quality of life) OR AB quality of working life
- AB personal satisfaction
- AB life satisfaction or happiness or wellbeing
- AB workplace
- AB employer
- S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11
- (S12 OR S13)
- TI (interven* or program* or implement* or activit* or participat* or effective* or evaluat*)
- (S4 AND S14 AND S15 AND S16)
References
- Vigo, D.; Thornicroft, G.; Atun, R. Estimating the true global burden of mental illness. Lancet Psychiatry 2016, 3, 171–178. [Google Scholar] [CrossRef]
- WHO. Mental Health in the Workplace. 2017. Available online: http://www.who.int/mental_health/in_the_workplace/en/ (accessed on 13 December 2017).
- WHO. Burn-Out an “Occupational Phenomenon”: International Classification of Diseases. 2019. Available online: http://www.who.int/mental_health/evidence/burn-out/en/ (accessed on 29 May 2019).
- Schultz, A.B.; Edington, D.W. Employee Health and Presenteeism: A Systematic Review. J. Occup. Rehabil. 2007, 17, 547–579. [Google Scholar] [CrossRef]
- Ammendolia, C.; Côté, P.; Cancelliere, C.; Cassidy, J.D.; Hartvigsen, J.; Boyle, E.; Soklaridis, S.; Stern, P.; Amick, B. Healthy and productive workers: Using intervention mapping to design a workplace health promotion and wellness program to improve presenteeism. BMC Public Health 2016, 16, 1190. [Google Scholar] [CrossRef]
- WHO. Mental Health: Massive Scale-up of Resources Needed if Global Targets Are to Be Met. 2018. Available online: http://www.who.int/mental_health/evidence/atlas/atlas_2017_web_note/en/ (accessed on 12 June 2018).
- Marchand, A.; Durand, P.; Haines, V.; Harvey, S. The multilevel determinants of workers’ mental health: Results from the SALVEO study. Soc. Psychiatry Psychiatr. Epidemiol. 2015, 50, 445–459. [Google Scholar] [CrossRef]
- Harvey, S.B.; Modini, M.; Joyce, S.; Milligan-Saville, J.S.; Tan, L.; Mykletun, A.; Bryant, R.A.; Christensen, H.; Mitchell, P.B. Can work make you mentally ill? A systematic meta-review of work-related risk factors for common mental health problems. Occup. Environ. Med. 2017, 74, 301–310. [Google Scholar] [CrossRef]
- Beauregard, N.; Marchand, A.; Blanc, M.-E. What do we know about the non-work determinants of workers’ mental health? A systematic review of longitudinal studies. BMC Public Health 2011, 11, 439. [Google Scholar] [CrossRef]
- Hannan, E.; Breslin, N.; Doherty, E.; McGreal, M.; Moneley, D.; Offiah, G. Burnout and stress amongst interns in Irish hospitals: Contributing factors and potential solutions. Ir. J. Med. Sci. 2018, 187, 301–307. [Google Scholar] [CrossRef]
- Qiao, Z.; Chen, L.; Chen, M.; Guan, M.; Wang, L.; Jiao, Y.; Yang, J.; Tang, Q.; Han, D.; Ma, J.; et al. Prevalence and factors associated with occupational burnout among HIV/AIDS healthcare workers in China: A cross-sectional study. BMC Public Health 2016, 16, 335. [Google Scholar] [CrossRef]
- Shanafelt, T.D.; Boone, S.; Tan, L.; Dyrbye, L.N.; Sotile, W.; Satele, D.; West, C.P.; Sloan, J.; Oreskovich, M.R. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch. Intern. Med. 2012, 172, 1377–1385. [Google Scholar] [CrossRef]
- Shanafelt, T.D.; Hasan, O.; Dyrbye, L.N.; Sinsky, C.; Satele, D.; Sloan, J.; West, C.P. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin. Proc. 2015, 90, 1600–1613. [Google Scholar] [CrossRef]
- Zhou, C.; Shi, L.; Gao, L.; Liu, W.; Chen, Z.; Tong, X.; Xu, W.; Peng, B.; Zhao, Y.; Fan, L. Determinate factors of mental health status in Chinese medical staff. Medicine (Baltimore) 2018, 97. [Google Scholar] [CrossRef]
- Shanafelt, T.D.; West, C.P.; Sloan, J.A.; Novotny, P.J.; Poland, G.A.; Menaker, R.; Rummans, T.A.; Dyrbye, T.A. Career fit and burnout among academic faculty. Arch. Intern. Med. 2009, 169, 990–995. [Google Scholar] [CrossRef]
- Shanafelt, T.D.; Mungo, M.; Schmitgen, J.; Storz, K.A.; Reeves, D.; Hayes, S.N.; Sloan, J.A.; Swensen, S.J.; Buskirk, S.J. Longitudinal study evaluating the association between physician burnout and changes in professional work effort. Mayo Clin. Proc. 2016, 91, 422–431. [Google Scholar] [CrossRef]
- Anderson, J.C.; Pfeil, S.; Surawicz, C. Strategies to combat physician burnout in gastroenterology. Am. J. Gastroenterol. 2017, 112, 1356–1359. [Google Scholar] [CrossRef]
- Van Ham, I.; Verhoeven, A.A.H.; Groenier, K.H.; Groothoff, J.W.; De Haan, J. Job satisfaction among general practitioners: A systematic literature review. Eur. J. Gen. Pract. 2006, 12, 174–180. [Google Scholar] [CrossRef]
- Groenewegen, P.P.; Hutten, J.B. Workload and job satisfaction among general practitioners: A review of the literature. Soc. Sci. Med. 1991, 32, 1111–1119. [Google Scholar] [CrossRef]
- Laubach, W.; Fischbeck, S. Job satisfaction and the work situation of physicians: A survey at a German university hospital. Int. J. Public Health 2007, 52, 54–59. [Google Scholar] [CrossRef]
- Adriaenssens, J.; De Gucht, V.; Maes, S. Causes and consequences of occupational stress in emergency nurses, a longitudinal study. J. Nurs. Manag. 2015, 23, 346–358. [Google Scholar] [CrossRef]
- Dyrbye, L.N.; Eacker, A.; Durning, S.J.; Brazeau, C.; Moutier, C.; Massie, F.S.; Satele, D.; Sloan, J.A.; Shanafelt, T.D. The impact of stigma and personal experiences on the help-seeking behaviors of medical students with burnout. Acad. Med. 2015, 90, 961. [Google Scholar] [CrossRef]
- Hall, B.J.; Xiong, P.; Chang, K.; Yin, M.; Sui, X. Prevalence of medical workplace violence and the shortage of secondary and tertiary interventions among healthcare workers in China. J. Epidemiol. Community Health 2018, 72, 516–518. [Google Scholar] [CrossRef]
- Yang, B.X.; Stone, T.E.; Petrini, M.A.; Morris, D.L. Incidence, Type, Related Factors, and Effect of Workplace Violence on Mental Health Nurses: A Cross-sectional Survey. Arch. Psychiatr. Nurs. 2018, 32, 31–38. [Google Scholar] [CrossRef]
- Panagioti, M.; Geraghty, K.; Johnson, J.; Zhou, A.; Panagopoulou, E.; Chew-Graham, C.; Peters, D.; Hodkinson, A.; Riley, R.; Esmail, A. Association Between Physician Burnout and Patient Safety, Professionalism, and Patient Satisfaction: A Systematic Review and Meta-analysis. JAMA Intern. Med. 2018, 178, 1317–1331. [Google Scholar] [CrossRef]
- Fahrenkopf, A.M.; Sectish, T.C.; Barger, L.K.; Sharek, P.J.; Lewin, D.; Chiang, V.W.; Edwards, S.; Wiedermann, B.L.; Landrigan, C.P. Rates of medication errors among depressed and burnt out residents: Prospective cohort study. BMJ 2008, 336, 488–491. [Google Scholar] [CrossRef]
- Tawfik, D.S.; Profit, J.; Morgenthaler, T.I.; Satele, D.V.; Sinsky, C.A.; Dyrbye, L.N.; Tutty, M.A.; West, C.P.; Shanafelt, T.D. Physician Burnout, Well-being, and Work Unit Safety Grades in Relationship to Reported Medical Errors. Mayo Clin. Proc. 2018, 93, 1571–1580. [Google Scholar] [CrossRef]
- Nantsupawat, A.; Nantsupawat, R.; Kunaviktikul, W.; Turale, S.; Poghosyan, L. Nurse burnout, nurse-reported quality of care, and patient outcomes in Thai hospitals. J. Nurs. Scholarsh. 2016, 48, 83–90. [Google Scholar] [CrossRef]
- Vahey, D.C.; Aiken, L.H.; Sloane, D.M.; Clarke, S.P.; Vargas, D. Nurse Burnout and Patient Satisfaction. Med. Care 2004, 42, II57–II66. [Google Scholar] [CrossRef]
- Spence Laschinger, H.K.; Leiter, M.P. The Impact of Nursing Work Environments on Patient Safety Outcomes: The Mediating Role of Burnout Engagement. JONA J. Nurs. Adm. 2006, 36, 259. [Google Scholar] [CrossRef]
- Sinsky, C.A.; Dyrbye, L.N.; West, C.P.; Satele, D.; Tutty, M.; Shanafelt, T.D. Professional Satisfaction and the Career Plans of US Physicians. Mayo Clin. Proc. 2017, 92, 1625–1635. [Google Scholar] [CrossRef]
- Han, S.; Shanafelt, T.D.; Sinsky, C.A.; Awad, K.M.; Dyrbye, L.N.; Fiscus, L.C.; Trockel, M.; Goh, J. Estimating the Attributable Cost of Physician Burnout in the United StatesCost of Physician Burnout. Ann. Intern. Med. 2019. [Google Scholar] [CrossRef]
- WHO. Mental Health: A State of Well-Being. 2014. Available online: http://www.who.int/features/factfiles/mental_health/en/ (accessed on 10 Janurary 2018).
- WHO. Mental Health Atlas 2017; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- de Neve, J.-E. Chapter 5: Work and Well-being: A Global Perspective. In Global Happiness Policy Report; Sustainable Development Solutions Network: New York, NY, USA, 2018. [Google Scholar]
- Ruotsalainen, J.H.; Verbeek, J.H.; Mariné, A.; Serra, C. Preventing occupational stress in healthcare workers. In Cochrane Database of Systematic Reviews; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2015. [Google Scholar]
- Pawson, R.; Greenhalgh, T.; Harvey, G.; Walshe, K. Realist review—A new method of systematic review designed for complex policy interventions. J. Health Serv. Res. Policy 2005, 10, 21–34. [Google Scholar] [CrossRef]
- Nielsen, K.; Taris, T.W.; Cox, T. The future of organizational interventions: Addressing the challenges of today’s organizations. Work Stress 2010, 24, 219–233. [Google Scholar] [CrossRef]
- Carrieri, D.; Briscoe, S.; Jackson, M.; Mattick, K.; Papoutsi, C.; Pearson, M.; Wong, G. ‘Care Under Pressure’: A realist review of interventions to tackle doctors’ mental ill-health and its impacts on the clinical workforce and patient care. BMJ Open 2018, 8, e021273. [Google Scholar] [CrossRef]
- Ali, N.A.; Wolf, K.M.; Hammersley, J.; Hoffmann, S.P.; O’Brien, J.M.; Phillips, G.S.; Rashkin, M.; Warren, E.; Garland, A. Continuity of care in intensive care units. Am. J. Respir. Crit. Care Med. 2011, 184, 803–808. [Google Scholar] [CrossRef]
- Arnetz, J.E.; Hasson, H. Evaluation of an educational “toolbox” for improving nursing staff competence and psychosocial work environment in elderly care: results of a prospective, non-randomized controlled intervention. Int. J. Nurs. Stud. 2007, 44, 723–735. [Google Scholar] [CrossRef]
- Aust, B.; Rugulies, R.; Finken, A.; Jensen, C. When workplace interventions lead to negative effects: Learning from failures. Scand. J. Public Health 2010, 38, 106–119. [Google Scholar] [CrossRef]
- Bourbonnais, R.; Brisson, C.; Vinet, A.; Vezina, M.; Abdous, B.; Gaudet, M. Effectiveness of a participative intervention on psychosocial work factors to prevent mental health problems in a hospital setting. Occup. Environ. Med. 2006, 63, 335–342. [Google Scholar] [CrossRef]
- Bourbonnais, R.; Brisson, C.; Vezina, M. Long-term effects of an intervention on psychosocial work factors among healthcare professionals in a hospital setting. Occup. Environ. Med. 2011, 68, 479–486. [Google Scholar] [CrossRef]
- Bryan, Y.E.; Hitchings, K.S.; Fox, M.A.; Kinneman, M.T.; Young, M.J. The evaluation of hospital restructuring efforts: Satisfaction, quality, and costs. Qual. Manag. Health Care 1998, 6, 22–34. [Google Scholar] [CrossRef]
- Bunce, D.; MA, W. Stress management and innovation interventions at work. Hum. Relat. 1996, 49, 209–232. [Google Scholar] [CrossRef]
- Carson, J.; Cavagin, J.; Bunclark, J.; Maal, S.; Gournay, K.; Kuipers, E.; Holloway, F.; West, M. Effective communication in mental health nurses: Did social support save the psychiatric nurse? NT Res. 1999, 4, 31–42. [Google Scholar] [CrossRef]
- Doran, D.; Jeffs, L.; Rizk, P.; Laporte, D.R.; Chilcote, A.M.; Bai, Y.Q. Evaluating the late career nurse initiative: a cross-sectional survey of senior nurses in Ontario. J. Nurs. Manag. 2015, 23, 859–867. [Google Scholar] [CrossRef]
- Ewers, P.; Bradshaw, T.; McGovern, J.; Ewers, B. Does training in psychosocial interventions reduce burnout rates in forensic nurses? J. Adv. Nurs. 2002, 37, 470–476. [Google Scholar] [CrossRef]
- Finnema, E.; Dröes, R.-M.; Ettema, T.; Ooms, M.; Adèr, H.; Ribbe, M.; van Tilburg, W. The effect of integrated emotion-oriented care versus usual care on elderly persons with dementia in the nursing home and on nursing assistants: a randomized clinical trial. Int. J. Geriat. Psychiatry 2005, 20, 330–343. [Google Scholar] [CrossRef]
- Ghazavi, Z.; Lohrasbi, F.; Mehrabi, T. Effect of communication skill training using group psychoeducation method on the stress level of psychiatry ward nurses. Iran J. Nurs. Midwifery Res. 2010, 15, 395–400. [Google Scholar]
- Gregory, S.T.; Menser, T.; Gregory, B.T. An Organizational Intervention to Reduce Physician Burnout. J. Healthc. Manag. 2018, 63, 338–352. [Google Scholar] [CrossRef]
- Günüşen, N.P.; Üstün, B. An RCT of coping and support groups to reduce burnout among nurses. Int. Nurs. Rev. 2010, 57, 485–492. [Google Scholar] [CrossRef]
- Häggström, E.; Skovdahl, K.; Fläckman, B.; AL, K.; Kihlgren, M. Work satisfaction and dissatisfaction—Caregivers’ experiences after a two-year intervention in a newly opened nursing home. J. Clin. Nurs. 2005, 14, 9–19. [Google Scholar] [CrossRef]
- Hall, L.M.; Doran, D.; Pink, L.; LM, H.; Doran, D.; Pink, L. Outcomes of interventions to improve hospital nursing work environments. J. Nurs. Adm. 2008, 38, 40–46. [Google Scholar] [CrossRef]
- Heaney, C.A.; Price, R.H.; Rafferty, J. Increasing coping resources at work: A field experiment to increase social support, improve work team functioning, and enhance employee mental health. J. Organ. Behav. 1995, 16, 335–352. [Google Scholar] [CrossRef]
- Hyman, R.B. Evaluation of an intervention for staff in a long-term care facility using a retrospective pretest design. Eval. Health Prof. 1993, 16, 212–224. [Google Scholar] [CrossRef]
- Jeon, Y.-H.; Simpson, J.M.; Li, Z.; Cunich, M.M.; Thomas, T.H.; Chenoweth, L.; Kendig, H.L. Cluster Randomized Controlled Trial of an Aged Care Specific Leadership and Management Program to Improve Work Environment, Staff Turnover, and Care Quality. J. Am. Med Dir. Assoc. 2015, 16, 629.e19–629.e28. [Google Scholar] [CrossRef]
- Joyce, T.; Higgins, I.; Magin, P.; Goode, S.; Pond, D.; Stone, T.; Elsom, S.; O’Neill, K. Nurses’ perceptions of a mental health education programme for Australian nurses. Int. J. Ment. Health Nurs. 2011, 20, 247–252. [Google Scholar] [CrossRef]
- Kapoor, S.; Morgan, C.K.; Siddique, M.A.; Guntupalli, K.K. “Sacred Pause” in the ICU: Evaluation of a Ritual and Intervention to Lower Distress and Burnout. Am. J. Hosp. Palliat. Med. 2018, 35, 1337–1341. [Google Scholar] [CrossRef]
- Koivu, A.; Saarinen, P.I.; Hyrkas, K. Does clinical supervision promote medical-surgical nurses’ well-being at work? A quasi-experimental 4-year follow-up study. J. Nurs. Manag. 2012, 20, 401–413. [Google Scholar] [CrossRef]
- Lavoie-Tremblay, M.; Bourbonnais, R.; Viens, C.; Vezina, M.; Durand, P.J.; Rochette, L. Improving the psychosocial work environment. J. Adv. Nurs. 2005, 49, 655–664. [Google Scholar] [CrossRef]
- Le Blanc, P.M.; Hox, J.J.; Schaufeli, W.B.; Taris, T.W.; Peeters, M.C.W. Take care! The evaluation of a team-based burnout intervention program for oncology care providers. J. Appl. Psychol. 2007, 92, 213–227. [Google Scholar] [CrossRef]
- Ledikwe, J.H.; Kleinman, N.J.; Mpho, M.; Mothibedi, H.; Mawandia, S.; Semo, B.-W.; O’Malley, G. Associations between healthcare worker participation in workplace wellness activities and job satisfaction, occupational stress and burnout: A cross-sectional study in Botswana. BMJ Open 2018, 8, e018492. [Google Scholar] [CrossRef]
- Leiter, M.P.; Laschinger, H.K.; Day, A.; Oore, D.G. The impact of civility interventions on employee social behavior, distress, and attitudes. J. Appl. Psychol. 2011, 96, 1258–1274. [Google Scholar] [CrossRef]
- Leiter, M.P.; Day, A.; Oore, D.G.; Spence Laschinger, H.K. Getting better and staying better: Assessing civility, incivility, distress, and job attitudes one year after a civility intervention. J. Occup. Health Psychol. 2012, 17, 425–434. [Google Scholar] [CrossRef]
- Gilin Oore, D.; Leblanc, D.; Day, A.; Leiter, M.P.; Spence Laschinger, H.; Price, S.L.; Latimer, M. When respect deteriorates: Incivility as a moderator of the stressor-strain relationship among hospital workers. J. Nurs. Manag. 2010, 18, 878–888. [Google Scholar] [CrossRef]
- Linzer, M.; Poplau, S.; Grossman, E.; Varkey, A.; Yale, S.; Williams, E.; Hicks, L.; Brown, R.L.; Wallock, J.; Kohnhorst, D.; et al. A Cluster randomized trial of interventions to improve work conditions and clinician burnout in primary care: Results from the healthy work place (HWP) study. J. Gen. Intern. Med. 2015, 30, 1105–1111. [Google Scholar] [CrossRef]
- Linzer, M.; Sinsky, C.A.; Poplau, S.; Brown, R.; Williams, E. In medical practice: Clinician satisfaction in the healthy work place trial. Health Aff. 2017, 36, 1808–1814. [Google Scholar] [CrossRef]
- Loiselle, C.G.; Gélinas, C.; Cassoff, J.; Boileau, J.; McVey, L. A pre–post evaluation of the Adler/Sheiner Programme (ASP): A nursing informational programme to support families and nurses in an intensive care unit (ICU). Intensive Crit. Care Nurs. 2012, 28, 32–40. [Google Scholar] [CrossRef]
- Lucas, B.P.; Trick, W.E.; Evans, A.T.; Mba, B.; Smith, J.; Das, K.; Clarke, P.; Varkey, A.; Mathew, S.; Weinstein, R.A. Effects of 2- vs 4-week attending physician inpatient rotations on unplanned patient revisits, evaluations by trainees, and attending physician burnout: a randomized trial. JAMA 2012, 308, 2199–2207. [Google Scholar] [CrossRef]
- McDonald, G.; Jackson, D.; Wilkes, L.; Vickers, M.H. A work-based educational intervention to support the development of personal resilience in nurses and midwives. Nurse Educ. Today 2012, 32, 378–384. [Google Scholar] [CrossRef]
- McDonald, G.; Jackson, D.; Wilkes, L.; Vickers, M.H. Personal resilience in nurses and midwives: Effects of a work-based educational intervention. Contemp. Nurse 2013, 45, 134–143. [Google Scholar] [CrossRef]
- Melchior, M.E.W.; Phihpsen, H.; Abu-Saad, H.H.; Halfens, R.J.G.; van de Berg, A.A.; Gassman, P. The effectiveness of primary nursing on burnout among psychiatric nurses in long-stay settings. J. Adv. Nurs. 1996, 24, 694–702. [Google Scholar] [CrossRef]
- Mikkelsen, A.; PO, S.; Landsbergis, P. The impact of a participatory organizational intervention on job stress in community health care institutions. Work Stress 2000, 14, 156–170. [Google Scholar] [CrossRef]
- Newman, C.; Patterson, K.; Clark, G. Evaluation of a support and challenge framework for nursing managers in correctional and forensic health. J. Nurs. Manag. 2015, 23, 118–127. [Google Scholar] [CrossRef]
- Odle-Dusseau, H.N.; Hammer, L.B.; Crain, T.L.; Bodner, T.E. The influence of family-supportive supervisor training on employee job performance and attitudes: An organizational work-family intervention. J. Occup. Health Psychol. 2016, 21, 296–308. [Google Scholar] [CrossRef]
- Parsons, M. Capacity building for magnetism at multiple levels: A healthy workplace intervention, part I. Top. Emerg. Med. 2004, 26, 287–295. [Google Scholar]
- Peterson, U.; Bergstrom, G.; Samuelsson, M.; Asberg, M.; Nygren, A. Reflecting peer-support groups in the prevention of stress and burnout: randomized controlled trial. J. Adv. Nurs. 2008, 63, 506–516. [Google Scholar] [CrossRef]
- Petterson, I.L.; Arnetz, B.B. Psychosocial stressors and well-being in health care workers. The impact of an intervention program. Soc. Sci. Med. 1998, 47, 1763–1772. [Google Scholar] [CrossRef]
- Petterson, I.L.; Donnersvärd, H.Å.; Lagerström, M.; Toomingas, A. Evaluation of an intervention programme based on empowerment for eldercare nursing staff. Work Stress 2006, 20, 353–369. [Google Scholar] [CrossRef]
- Proctor, R.; Stratton-Powell, H.; Tarrier, N.; Burns, A. The impact of training and support on stressamong care staff in nursing and residential homesfor the elderly. J. Ment. Health 1998, 7, 59–70. [Google Scholar]
- Quenot, J.P.; Rigaud, J.P.; Prin, S.; Barbar, S.; Pavon, A.; Hamet, M.; Jacquiot, N.; Blettery, B.; Herve, C.; Charles, P.E.; et al. Suffering among carers working in critical care can be reduced by an intensive communication strategy on end-of-life practices. Intensive Care Med. 2012, 38, 55–61. [Google Scholar] [CrossRef]
- Razavi, D.; Delvaux, N.; Marchal, S.; Bredart, A.; Farvacques, C.; Paesmans, M. The effects of a 24-h psychological training program on attitudes, communication skills and occupational stress in oncology: A randomised study. Eur. J. Cancer 1993, 29, 1858–1863. [Google Scholar] [CrossRef]
- Redhead, K.; Bradshaw, T.; Braynion, P.; Doyle, M. An evaluation of the outcomes of psychosocial intervention training for qualified and unqualified nursing staff working in a low-secure mental health unit. J. Psychiatr. Ment. Health Nurs. 2011, 18, 59–66. [Google Scholar] [CrossRef]
- Richter, A.; Kostova, P.; Baur, X.; Wegner, R. Less work: More burnout? A comparison of working conditions and the risk of burnout by German physicians before and after the implementation of the EU Working Time Directive. Int. Arch. Occup. Environ. Health 2014, 87, 205–215. [Google Scholar] [CrossRef]
- Rickard, G.; Lenthall, S.; Dollard, M.; Opie, T.; Knight, S.; Dunn, S.; Wakerman, J.; MacLeod, M.; Seller, J.; Brewster-Webb, D. Organisational intervention to reduce occupational stress and turnover in hospital nurses in the Northern Territory, Australia. Collegian 2012, 19, 211–221. [Google Scholar] [CrossRef]
- Romig, M.C.; Latif, A.; Gill, R.S.; Pronovost, P.J.; Sapirstein, A. Perceived benefit of a telemedicine consultative service in a highly staffed intensive care unit. J. Crit. Care 2012, 27, 426.e9–426.e16. [Google Scholar] [CrossRef]
- Saint-Louis, N.M.; Bourjolly, J.N. Narrative intervention: Stories from the front lines of oncology health care. Soc. Work Health Care 2018, 57, 637–655. [Google Scholar] [CrossRef]
- Schrijnemaekers, V.J.J.; van Rossum, E.; Candel, M.J.J.M.; Frederiks, C.M.A.; Derix, M.M.A.; Sielhorst, H.; van den Brandt, P.A. Effects of emotion-oriented care on work-related outcomes of professional caregivers in homes for elderly persons. J. Gerontol. B Psychol. Sci. Soc. Sci. 2003, 58, S50–S57. [Google Scholar] [CrossRef]
- Sexton, J.B.; Sharek, P.J.; Thomas, E.J.; Gould, J.B.; Nisbet, C.C.; Amspoker, A.B.; Kowalkowski, M.A.; Schwendimann, R.; Profit, J. Exposure to Leadership WalkRounds in neonatal intensive care units is associated with a better patient safety culture and less caregiver burnout. BMJ Qual. Saf. 2014, 23, 814–822. [Google Scholar] [CrossRef]
- Spetz, J. Nurse satisfaction and the implementation of minimum nurse staffing regulations. Policy Polit. Nurs. Pract. 2008, 9, 15–21. [Google Scholar] [CrossRef]
- Takizawa, T.; Takahashi, M.; Takai, M.; Ikeda, T.; Miyaoka, H. Changes in job stress and coping skills among caregivers after dementia care practitioner training. Psychogeriatrics 2017, 17, 52–60. [Google Scholar] [CrossRef]
- Traeger, L.; Park, E.R.; Sporn, N.; Repper-DeLisi, J.; Convery, M.S.; Jacobo, M.; Pirl, W.F. Development and evaluation of targeted psychological skills training for oncology nurses in managing stressful patient and family encounters. Oncol. Nurs. Forum 2013, 40, E327–E336. [Google Scholar] [CrossRef]
- Uchiyama, A.; Odagiri, Y.; Ohya, Y.; Takamiya, T.; Inoue, S.; Shimomitsu, T. Effect on mental health of a participatory intervention to improve psychosocial work environment: A cluster randomized controlled trial among nurses. J. Occup. Health 2013, 55, 173–183. [Google Scholar] [CrossRef]
- Van Bogaert, P.; Van heusden, D.; Somers, A.; Tegenbos, M.; Wouters, K.; Van der Straeten, J.; Van Aken, P.; Havens, D.S. The productive ward programTM. J. Nurs. Adm. 2014, 44, 452–461. [Google Scholar] [CrossRef]
- Wallbank, S. Effectiveness of individual clinical supervision for midwives and doctors in stress reduction: findings from a pilot study. Evid. Based Midwifery 2010, 8, 65–70. [Google Scholar]
- Wei, R.; Ji, H.; Li, J.; Zhang, L. Active intervention can decrease burnout in Ed nurses. J. Emerg. Nurs. 2017, 43, 145–149. [Google Scholar] [CrossRef]
- Yamagishi, M.; Kobayashi, T.; Kobayashi, T.; Nagami, M.; Shimazu, A.; Kageyama, T. Effect of web-based assertion training for stress management of Japanese nurses. J. Nurs. Manag. 2007, 15, 603–607. [Google Scholar] [CrossRef][Green Version]
- World Bank Country and Lending Groups—World Bank Data Help Desk. Available online: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519 (accessed on 17 April 2019).
- Lee, R.T.; Ashforth, B.E. On the meaning of Maslach’s three dimensions of burnout. J. Appl. Psychol. 1990, 75, 743–747. [Google Scholar] [CrossRef]
- Wong, G.; Greenhalgh, T.; Westhorp, G.; Buckingham, J.; Pawson, R. RAMESES publication standards: Realist syntheses. BMC Med. 2013, 11, 21. [Google Scholar] [CrossRef]
- LaMontagne, A.D.; Martin, A.; Page, K.M.; Reavley, N.J.; Noblet, A.J.; Milner, A.J.; Keegel, T.; Smith, P.M. Workplace mental health: Developing an integrated intervention approach. BMC Psychiatry 2014, 14, 131. [Google Scholar] [CrossRef]
- Harden, A.; Peersman, G.; Oliver, S.; Mauthner, M.; Oakley, A. A systematic review of the effectiveness of health promotion interventions in the workplace. Occup. Med. 1999, 49, 540–548. [Google Scholar] [CrossRef]
- LaMontagne, A.D.; Noblet, A.J.; Landsbergis, P.A. Intervention development and implementation: Understanding and addressing barriers to organizational-level interventions. In Improving Organizational Interventions for Stress and Well-Being: Addressing Process and Context; Routledge/Taylor & Francis Group: New York, NY, USA, 2012; pp. 21–38. [Google Scholar]
- Dollard, M.F.; Bakker, A.B. Psychosocial safety climate as a precursor to conducive work environments, psychological health problems, and employee engagement. J. Occup. Organ. Psychol. 2010, 83, 579–599. [Google Scholar] [CrossRef]
- Hall, G.B.; Dollard, M.F.; Coward, J. Psychosocial safety climate: Development of the PSC-12. Int. J. Stress Manag. 2010, 17, 353–383. [Google Scholar] [CrossRef]
- Kent, K.; Goetzel, R.Z.; Roemer, E.C.; Prasad, A.; Freundlich, N. Promoting Healthy Workplaces by Building Cultures of Health and Applying Strategic Communications. J. Occup. Environ. Med. 2016, 58, 114–122. [Google Scholar] [CrossRef]
- Rongen, A.; Robroek, S.J.W.; van Lenthe, F.J.; Burdorf, A. Workplace Health Promotion: A Meta-Analysis of Effectiveness. Am. J. Prev. Med. 2013, 44, 406–415. [Google Scholar] [CrossRef]
- Campbell, N.C.; Murray, E.; Darbyshire, J.; Emery, J.; Farmer, A.; Griffiths, F.; Guthrie, B.; Lester, H.; Wilson, P. Kinmonth, A.L. Designing and evaluating complex interventions to improve health care. BMJ 2007, 334, 455–459. [Google Scholar] [CrossRef]
- Schelvis, R.M.C.; Oude Hengel, K.M.; Burdorf, A.; Blatter, A.; Strijk, J.E.; van der Beek, A.J. Evaluation of occupational health interventions using a randomized controlled trial: Challenges and alternative research designs. Scand. J. Work Environ. Health 2015, 41, 491–503. [Google Scholar] [CrossRef]
- Wickström, G.; Bendix, T. The “Hawthorne effect”—What did the original Hawthorne studies actually show? Scand. J. Work Environ. Health 2000, 26, 363–367. [Google Scholar] [CrossRef]
- Bitz, J.; Howland, D.; Cornelissen, E.; Scheirer, M.A.; Saul, J.; Willis, C.D.; Bevan, H.; Best, A.; Mannion, R.; Jenkins, E.; et al. Sustaining organizational culture change in health systems. J. Health Organ. Manag. 2016, 30, 2–30. [Google Scholar] [CrossRef]
- Selamu, M.; Thornicroft, G.; Fekadu, A.; Hanlon, C. Conceptualisation of job-related wellbeing, stress and burnout among healthcare workers in rural Ethiopia: A qualitative study. BMC Health Serv. Res. 2017, 17. [Google Scholar] [CrossRef]
- Diener, E. Well-Being for Public Policy; Oxford University Press: Oxford, UK, 2009. [Google Scholar]
- Helliwell, J.F.; Barrington-Leigh, C.P. Viewpoint: Measuring and understanding subjective well-being. Can. J. Econ. /Rev. Can. Écon. 2010, 43, 729–753. [Google Scholar] [CrossRef]
- Lyubomirsky, S.; King, L.; Diener, E. The Benefits of Frequent Positive Affect: Does Happiness Lead to Success? Psychol. Bull. 2005, 131, 803–855. [Google Scholar] [CrossRef]
- OECD. Guidelines on Measuring Subjective Well-Being; OECD Publishing: Paris, France, 2013. [Google Scholar]
- Helliwell, J.F.; Wang, S. Weekends and subjective well-being. Soc. Indic. Res. 2014, 116, 389–407. [Google Scholar] [CrossRef]
- Sustainable Development Solutions Network. World Happiness Report 2018; Sustainable Development Solutions Network: New York, NY, USA, 2018. [Google Scholar]
- Kakuma, R.; Kleintjes, S.; Lund, C.; Drew, N.; Green, A.; Filsher, A.J. Mental health stigma: What is being done to raise awareness and reduce stigma in South Africa? Afr. J. Psychiatry (Johannesbg) 2010, 13, 116–124. [Google Scholar] [CrossRef]
- Clement, S.; Schauman, O.; Graham, T.; Maggioni, F.; Evans-Lacko, S.; Bezborodovs, N.; Morgan, C.; Rusch, N.; Brown, J.S.L.; Thornicroft, G. What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychol. Med. 2015, 45, 11–27. [Google Scholar] [CrossRef]
- Evans-Lacko, S.; Clement, S.; Corker, E.; Brohan, E.; Dockery, L.; Farrelly, S.; Hamilton, S.; Pinfold, V.; Rose, D.; Henderson, C.; et al. How much does mental health discrimination cost: Valuing experienced discrimination in relation to healthcare care costs and community participation. Epidemiol. Psychiatr. Sci. 2015, 24, 423–434. [Google Scholar] [CrossRef]
- van Brakel, W.H.; Cataldo, J.; Grover, S.; Kohrt, B.A.; Nyblade, L.; Stockton, M.; Wouters, E.; Yang, L.H. Out of the silos: Identifying cross-cutting features of health-related stigma to advance measurement and intervention. BMC Med. 2019, 17, 13. [Google Scholar] [CrossRef]
- Kane, J.C.; Elafros, M.A.; Murray, S.M.; Mitchell, E.M.H.; Augustinavicius, J.L.; Causevic, S.; Baral, S.D. A scoping review of health-related stigma outcomes for high-burden diseases in low- and middle-income countries. BMC Med. 2019, 17, 17. [Google Scholar] [CrossRef]
- Yassi, A.; Lockhart, K.; Sykes, M.; Buck, B.; Stime, B.; Spiegel, J.M. Effectiveness of joint health and safety committees: A realist review. Am. J. Ind. Med. 2013, 56, 424–438. [Google Scholar] [CrossRef]
| Study Characteristic | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| Population |
|
|
| Intervention |
|
|
| Context |
|
|
| Outcome |
|
|
| Study Design |
|
|
| Publication |
|
|
| Citation | Reference number# | Country | Type of Health Worker | Workplace | Measure(s) of Mental Health |
|---|---|---|---|---|---|
| Ali et al. (2011) | [40] | United States | Physicians | Hospital | burnout, stress, work–home life imbalance |
| Arnetz and Hasson (2007) | [41] | Sweden | Nurses | Elder care organizations | psychosocial work environment |
| Aust et al. (2010) | [42] | Denmark | Mixed | Hospital | psychosocial work environment |
| Bourbonnais et al. (2006 and 2011) | [43,44] | Canada | Mixed | Hospital | psychosocial work factors, psychological distress, burnout, sleeping problems |
| Bryan et al. (1998) | [45] | United States | Nurses | Hospital | job satisfaction |
| Bunce and West (1996) | [46] | United Kingdom | Mixed | Mixed | job motivation, job satisfaction, psychological strain, job-induced tension |
| Carson et al. (1999) | [47] | United Kingdom | Nurses | Hospital | occupational stressors, psychological distress, burnout |
| Doran et al. (2015) | [48] | Canada | Nurses | Mixed | work environment, organizational commitment and job satisfaction, burnout |
| Ewers et al. (2002) | [49] | United Kingdom | Nurses | Mental Health Unit | burnout |
| Finnema et al. (2005) | [50] | The Netherlands | Nurses | Nursing home | stress, stress reactions, work satisfaction, absenteeism |
| Ghazavi et al. (2010) | [51] | Iran | Nurses | Hospital | occupational stress |
| Gregory et al. (2018) | [52] | United States | Physicians | Primary care clinics | burnout |
| Gunusen and Ustun (2010) | [53] | Turkey | Nurses | Hospital | burnout |
| Haggstrom et al. (2005) | [54] | Sweden | Nurses | Nursing home | work satisfaction and dissatisfaction |
| Hall et al. (2008) | [55] | Canada | Nurses | Hospital | satisfaction, stress, work environment, role tension |
| Heaney et al. (1995) | [56] | United States | Care staff and managers | Residential care facility | social support, organizational climate for participation and influence in decision-making, employees’ confidence in ability to cope with common work problems, psychological wellbeing |
| Hyman (1993) | [57] | United States | Mixed | Residential care facility | burnout, work atmosphere |
| Jeon et al. (2015) | [58] | Australia | Mixed | Residential and community aged care sites | work environment, staff turnover, stress, absenteeism |
| Joyce et al. (2011) | [59] | Australia | Nurses | Hospital and community health settings | mental health literacy for peer support |
| Kapoor et al. (2018) | [60] | United States | Mixed | Hospital | burnout, grief, distress |
| Koivu et al. (2012) | [61] | Finland | Nurses | Hospital | psychological and social factors at work, burnout, psychological distress |
| Lavoie-Tremblay et al. (2005) | [62] | Canada | Mixed | Hospital | decision latitude, psychological demands, social support, effort/reward imbalance, reward, psychological distress, absenteeism |
| Le Blanc et al. (2007) | [63] | The Netherlands | Mixed | Hospital | burnout, social support, participation in decision making, job control, job demands |
| Ledikwe et al. (2018) | [64] | Botswana | Mixed | Public health facilities | job satisfaction, psychological wellbeing, burnout, stress |
| Leiter et al. (2011 and 2012); Oore et al. (2010) | [65,66,67] | Canada | Mixed | Hospital | workload, job control, incivility, respect, negative affect and anxiety |
| Linzer et al. (2015 and 2017) | [68,69] | United States | Physicians | Primary care clinics | work control, stress, burnout, chaos, likelihood to leave |
| Loiselle et al. (2012) | [70] | Canada | Nurses | Hospital | performance obstacles, perceived work support, emotional distress |
| Lucas et al. (2012) | [71] | United States | Physicians | Hospital | burnout, stress, workplace control |
| McDonald et al. (2012 and 2013) | [72,73] | Australia | Mixed | Hospital | personal resilience |
| Melchior et al. (1996) | [74] | The Netherlands | Nurses | Hospital | burnout |
| Mikkelsen et al. (2000) | [75] | Norway | Mixed | Community health care | work-related stress, subjective health, demands-control, social support, role harmony, |
| Newman et al. (2015) | [76] | Australia | Nurses | Correctional centers and forensic health | burnout, workplace satisfaction |
| Odle-Dusseau et al. (2016) | [77] | United States | Supervisors | Nursing home | job satisfaction, organizational commitment, turnover intentions, employee engagement, work-family conflict |
| Parsons et al. (2004) | [78] | United States | Nurses | Hospital | control, work satisfaction, interactions, organizational commitment |
| Peterson et al. (2008) | [79] | Sweden | Mixed | Hospital | burnout, quantitative demands, anxiety, depression, general health |
| Petterson and Arnetz (1998) | [80] | Sweden | Mixed | Hospital | job demands, work pressure, psychosomatic symptoms, exhaustion, job control, coping |
| Petterson et al. (2006) | [81] | Sweden | Nurses | Elder care organizations | work demands, job control, support, psychosomatic symptoms, stress, coping |
| Proctor et al. (1998) | [82] | United Kingdom | Elder care staff | Nursing and residential homes (elder care) | general health, occupational stress |
| Quenot et al. (2012) | [83] | France | Mixed | Hospital | burnout, depression |
| Razavi et al. (1993) | [84] | Belgium, France | Nurses | Hospital | occupational stress, attitudes |
| Redhead et al. (2011) | [85] | United Kingdom | Nurses | Inpatient care for mental health patients | burnout |
| Richter et al. (2014) | [86] | Germany | Physicians | Hospital | burnout, physical and mental health |
| Rickard et al. (2012) | [87] | Australia | Nurses | Hospital | occupational stress, turnover |
| Romig et al. (2012) | [88] | United States | Nurses | Hospital | psychological working conditions, burnout, relations and communications |
| Saint-Louis and Bourjolly (2018) | [89] | United States | Mixed | Oncology Unit | N/A |
| Schrijnemaekers et al. (2003) | [90] | The Netherlands | Elder care staff | Residential care facility | job satisfaction, burnout, sick leave |
| Sexton et al. (2014) | [91] | United States | Mixed | NICUs | burnout |
| Spetz (2008) | [92] | United States | Nurses | Hospital | job satisfaction |
| Takizawa et al. (2017) | [93] | Japan | Mixed | Elder care organizations | job stress, coping |
| Traeger et al. (2013) | [94] | United States | Mixed | Oncology Unit | burnout, stress |
| Uchiyama et al. (2013) | [95] | Japan | Nurses | Hospital | depression, psychosocial work environment |
| Van Bogaert et al. (2014) | [96] | Belgium | Mixed | Hospital | job satisfaction, burnout, intent to leave |
| Wallbank (2010) | [97] | United Kingdom | Mixed | Hospital | burnout, compassion satisfaction, compassion fatigue, stress |
| Wei et al. (2017) | [98] | China | Nurses | Hospital | burnout |
| Yamagishi et al. (2007) | [99] | Japan | Nurses | Hospital | job stress, depression |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gray, P.; Senabe, S.; Naicker, N.; Kgalamono, S.; Yassi, A.; Spiegel, J.M. Workplace-Based Organizational Interventions Promoting Mental Health and Happiness among Healthcare Workers: A Realist Review. Int. J. Environ. Res. Public Health 2019, 16, 4396. https://doi.org/10.3390/ijerph16224396
Gray P, Senabe S, Naicker N, Kgalamono S, Yassi A, Spiegel JM. Workplace-Based Organizational Interventions Promoting Mental Health and Happiness among Healthcare Workers: A Realist Review. International Journal of Environmental Research and Public Health. 2019; 16(22):4396. https://doi.org/10.3390/ijerph16224396
Chicago/Turabian StyleGray, Patricia, Sipho Senabe, Nisha Naicker, Spo Kgalamono, Annalee Yassi, and Jerry M. Spiegel. 2019. "Workplace-Based Organizational Interventions Promoting Mental Health and Happiness among Healthcare Workers: A Realist Review" International Journal of Environmental Research and Public Health 16, no. 22: 4396. https://doi.org/10.3390/ijerph16224396
APA StyleGray, P., Senabe, S., Naicker, N., Kgalamono, S., Yassi, A., & Spiegel, J. M. (2019). Workplace-Based Organizational Interventions Promoting Mental Health and Happiness among Healthcare Workers: A Realist Review. International Journal of Environmental Research and Public Health, 16(22), 4396. https://doi.org/10.3390/ijerph16224396





