Shared Decision Making and Choice for Bariatric Surgery
Abstract
1. Introduction
2. Methods
2.1. Case Hospital Selection
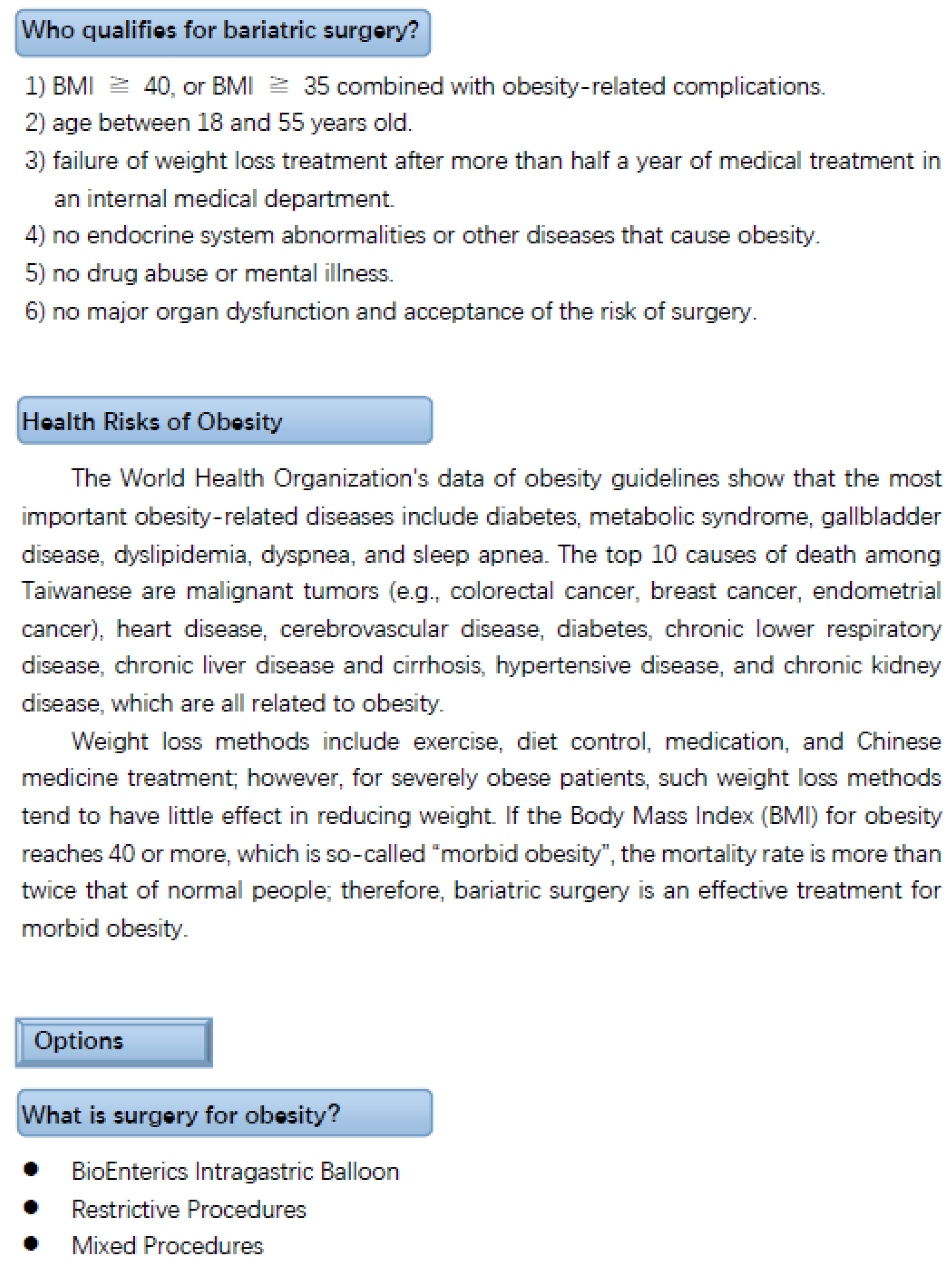
2.2. PDA Development and Design
2.3. Patients and Procedures
2.4. Questionnaires
2.5. Data Analysis
3. Results
Patient Characteristics
4. Discussion
5. Implications for Practice
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Hsieh, M.; Hsu, C.W. The Strategies of Doctor-Patient Communication in the Emergency Department. Taipei City Med. J. 2014, 11, 121–128. [Google Scholar]
- Chung, B.F. Did You do Your Homework Before the Operation? Available online: https://www.ttv.com.tw/lohas/view/19666 (accessed on 12 October 2019).
- Wu, B.C.; Chang, C.Y.; Chuang, S.M.; Lee, Y.C.; Yu, Y.L.; Liao, S.H. Introduction and Implementation of Shared Decision Making. J. Healthc. Qual. 2017, 11, 4–10. [Google Scholar]
- Ministry of Health and Welfare. Introduction to Patient Decision Aids. 2016. Available online: https://sdm.patientsafety.mohw.gov.tw/Public/Detail?sn=9&id=1064 (accessed on 12 October 2019).
- Blanc, X.; Collet, T.H.; Auer, R.; Fischer, R.; Locatelli, I.; Iriarte, P.; Krause, J.; Legare, F.; Cornuz, J. Publication trends of shared decision making in 15 high impact medical journals: A full-text review with bibliometric analysis. BMC Med. Inf. Decis. Mak. 2014, 14, 71. [Google Scholar]
- Wang, E.W. Shared Decision Making-Decision Making Aids and Clinical Application. J. Healthc. Qual. 2016, 10, 15–24. [Google Scholar]
- Charles, C.; Whelan, T.; Gafni, A. What do we mean by partnership in making decisions about treatment? BMJ 1999, 319, 780–782. [Google Scholar] [CrossRef]
- Jordan, J.L.; Ellis, S.J.; Chambers, R. Defining shared decision making and concordance: Are they one and the same? Postgrad. Med. J. 2002, 78, 383–384. [Google Scholar] [CrossRef][Green Version]
- Montgomery, A.A.; Fahey, T. How do patients’ treatment preferences compare with those of clinicians? BMJ Qual. Saf. 2001, 10, i39–i43. [Google Scholar] [CrossRef]
- Frosch, D.L.; Kaplan, R.M. Shared decision making in clinical medicine: Past research and future directions. Am. J. Prev. Med. 1999, 17, 285–294. [Google Scholar] [CrossRef]
- Hamann, J.; Leucht, S.; Kissling, W. Shared decision making in psychiatry. Acta Psychiatr. Scand. 2003, 107, 403–409. [Google Scholar] [CrossRef]
- Joosten, E.A.G.; DeFuentes-Merillas, L.; de Weert, G.H.; Sensky, T.; van der Staak, C.P.F.; de Jong, C.A.J. Systematic Review of the Effects of Shared Decision-Making on Patient Satisfaction, Treatment Adherence and Health Status. Psychother. Psychosom. 2008, 77, 219–226. [Google Scholar] [CrossRef]
- Grol, R. Improving the quality of medical care. Building bridges among professional pride, payer profit, and patient satisfaction. JAMA 2001, 286, 2578–2585. [Google Scholar] [CrossRef]
- Sensky, T. Withdrawal of life-sustaining treatment. BMJ 2002, 325, 175–176. [Google Scholar] [CrossRef]
- Crawford, M.J.; Aldridge, T.; Bhui, K.; Rutter, D.; Manley, C.; Weaver, T.; Tyrer, T.; Fulop, N. User involvement in the planning and delivery of mental health services: A cross-sectional survey of service users and providers. Acta Psychiatr. Scand. 2003, 107, 410–414. [Google Scholar] [CrossRef]
- Coulter, A.; Collins, A. Making Shared Decision-Making a Reality. 2011. Available online: https://www.kingsfund.org.uk/sites/default/files/Making-shared-decision-making-a-reality-paper-Angela-Coulter-Alf-Collins-July-2011_0.pdf (accessed on 11 October 2019).
- O’Connor, A.M.; Bennett, C.L.; Stacey, D.; Barry, M.; Col, N.F.; Eden, K.B.; Margaret, H.-R.; Hilary, L.-T.; Lyddiatt, A.; Thomson, R.; et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst. Rev. 2009, 3, CD001431. [Google Scholar]
- Chen, K.H.; Kao, C.C. Patient Preferences and Values in Shared Decision Making. J. Healthc. Qual. 2017, 11, 31–37. [Google Scholar]
- Ministry of Health and Welfare. 2018 Cause of Death Statistics. 2019. Available online: https://www.mohw.gov.tw/cp-16-48057-1.html (accessed on 1 October 2019).
- World Health Organization. Obesity and Overweight. 2018. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 2 October 2019).
- Lee, W.J. Surgical Treatment of Obesity. Formos. J. Med. 2002, 6, 64–69. [Google Scholar]
- American Society for Metabolic and Bariatric Surgery. Estimate of Bariatric Surgery Numbers, 2011–2017. 2018. Available online: https://asmbs.org/resources/estimate-of-bariatric-surgery-numbers (accessed on 1 October 2019).
- Taiwan Society for Metabolic and Bariatric Surgery. 2016 the Statistics of Taiwan Weight Loss Surgery. 2017. Available online: http://www.tsmbs.org.tw/download/2016%E5%B9%B4%E5%8F%B0%E7%81%A3%E6%B8%9B%E9%87%8D%E6%89%8B%E8%A1%93%E7%B5%B1%E8%A8%88.pdf (accessed on 5 October 2019).
- Lin, W.L.; Su, S.F.; Lee, W.J.; Lee, C.H. The Influence of Bariatric Surgery on Body Image in Obesity Patients. J. Nurs. 2015, 62, 50–57. [Google Scholar]
- Lee, Y.C.; Hsieh, H.F.; Lee, C.K.; Lee, W.J.; Yu, P.J.; Lin, Y.C. Gastrointestinal Quality of Life Following Laparoscopic Bariatric Surgery. Cheng Ching Med. J. 2008, 4, 8–13. [Google Scholar]
- Lee, W.J. Surgical Treatment of Obesity an Asia Perspective. Tzu Chi Med. J. 2007, 19, 200–206. [Google Scholar] [CrossRef]
- Adams, T.D.; Gress, R.E.; Smith, S.C.; Halverson, R.C.; Simper, S.C.; Rosamond, W.D.; LaMonte, M.J.; Stroup, A.M.; Hunt, S.C. Long-term mortality after gastric bypass surgery. N. Engl. J. Med. 2007, 357, 753–761. [Google Scholar] [CrossRef]
- Sjöström, L.; Narbro, K.; Sjöström, C.D.; Karason, K.; Larsson, B.; Wedel, H.; Lystig, T.; Sullivan, M.; Bouchard, C.; Carlsson, B.; et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N. Engl. J. Med. 2007, 357, 741–752. [Google Scholar] [CrossRef]
- Lee, W.C.; Wang, W.; Hsu, K.H.; Chen, R.C.; Yao, W.C.; Chuang, C.; Chang, Y.Y.; Chang, C.C.; Wei, S.C.; Chen, S.C.; et al. Surgical Treatment and Care for Morbid Obesity and Diabetes; Easy Book: New Taipei City, Taiwan, 2014. [Google Scholar]
- Asia-Pacific Endoscopic Bariatric Surgical Center. Bariatric Surgery. 2018. Available online: http://www.8320.com.tw/index.asp (accessed on 5 October 2019).
- Physician’s Weekly. Patient Factors in Bariatric Surgery Choices. 2014. Available online: https://www.physiciansweekly.com/patient-factors-bariatric-surgery/ (accessed on 7 October 2019).
- Harcourt, D.; Paraskeva, N.; White, P.; Powell, J.; Clarke, A. A study protocol of the effectiveness of PEGASUS: A multi-centred study comparing an intervention to promote shared decision making about breast reconstruction with treatment as usual. BMC Med. Inf. Decis. Mak. 2017, 17, 143. [Google Scholar] [CrossRef]
- Nota, I.; Drossaert, C.H.C.; Melissant, H.C.; Taal, E.; Vonkeman, H.E.; Haagsma, C.J.; van de Laar, M.A.F.J. Development of a web-based patient decision aid for initiating disease modifying anti-rheumatic drugs using user-centred design methods. BMC Med. Inf. Decis. Mak. 2017, 17, 51. [Google Scholar] [CrossRef]
- Li, L.C.; Adam, P.M.; Backman, C.L.; Lineker, S.; Jones, C.A.; Lacaille, D.; Townsend, A.F.; Yacyshyn, E.; Yousefi, C.; Tugwell, P.; et al. Proof-of-concept study of a web-based methotrexate decision aid for patients with rheumatoid arthritis. Arthritis Care Res. 2014, 66, 1472–1481. [Google Scholar] [CrossRef]
- British Obesity & Metabolic Surgery Society. BOMSS Standards for Clinical Services. 2012. Available online: https://www.bomss.org.uk/bomss-standards-for-clinical-services/ (accessed on 5 October 2019).
- Ministry of Health and Welfare. Platform for Shared Decision Making. 2017. Available online: https://sdm.patientsafety.mohw.gov.tw/AssistTool/Category?sn=24 (accessed on 10 October 2019).
- American Society for Metabolic and Bariatric Surgery. Bariatric Surgery Procedures. 2019. Available online: https://asmbs.org/patients/bariatric-surgery-procedures (accessed on 10 October 2019).
- Healthwise Staff. American College of Cardiology. 2018. Available online: https://www.cardiosmart.org/healthwise/ug23/64/ug2364 (accessed on 1 September 2018).
- Healthwise. Obesity: Should I Have Weight-Loss Surgery? 2017. Available online: https://www.healthlinkbc.ca/health-topics/ug2364 (accessed on 11 October 2018).
- The Joint Commission of Taiwan. Shared Decision Making. 2017. Available online: https://sdm.patientsafety.mohw.gov.tw/Files/PublicContent/19/%E5%BC%B5%E9%9D%9C%E6%80%A1-2016%E5%B9%B4%E8%A8%88%E7%95%AB%E6%8E%A8%E8%A1%8C%E6%88%90%E6%9E%9C%E5%9B%9E%E9%A1%A7.pdf (accessed on 11 October 2019).
- Holmes-Rovner, M.; Kroll, J.; Schmitt, N.; Rovner, D.R.; Breer, M.L.; Rothert, M.L.; Padonu, G.; Talarczyk, G. Patient satisfaction with health care decisions: The satisfaction with decision scale. Med. Decis. Mak. 1996, 16, 58–64. [Google Scholar] [CrossRef]
- Brehaut, J.C.; O’Connor, A.M.; Wood, T.J.; Hack, T.F.; Siminoff, L.; Gordon, E.; Deb, F.-S. Validation of a decision regret scale. Med. Decis. Mak. 2003, 23, 281–292. [Google Scholar] [CrossRef]
- IBM Corp. IBM SPSS Statistics for Windows, 210th ed.; IBM Corp: Armonk, NY, USA, 2012. [Google Scholar]
- Varban, O.A.; Dimick, J.B. Bariatric Surgery: Safe, Effective, and Underutilized. Fam. Med. 2019, 51, 552–554. [Google Scholar] [CrossRef]
- Health Promotion Administration, MOHW. Obesity Is a Chronic Disease! Adjusting Diet and Sports Life Is the Best Prescription. 2018. Available online: https://www.hpa.gov.tw/Pages/Detail.aspx?nodeid=1405&pid=8840 (accessed on 5 October 2019).
- Memarian, E.; Sundquist, K.; Calling, S.; Sundquist, J.; Li, X.J. Socioeconomic factors, body mass index and bariatric surgery: A Swedish nationwide cohort study. BMC Public Health 2019, 19, 258. [Google Scholar] [CrossRef]
- Lamb, C.C.; Wang, Y.; Lyytinen, K. Shared decision making: Does a physician’s decision-making style affect patient participation in treatment choices for primary immunodeficiency? J. Eval. Clin. Pract. 2019. [Google Scholar] [CrossRef]
- Moore, J.; Haemer, M.; Mirza, N.; Weatherall, Y.Z.; Han, J.; Mangarelli, C.; Hawkins, M.J.; Xanthakos, S.; Siegel, R. Pilot Testing of a Patient Decision Aid for Adolescents with Severe Obesity in US Pediatric Weight Management Programs within the COMPASS Network. Int. J. Environ. Res. Public Health 2019, 16, 1776. [Google Scholar] [CrossRef]
- Weinstein, A.L.; Marascalchi, B.J.; Spiegel, M.A.; Saunders, J.K.; Fagerlin, A.; Parikh, M. Patient preferences and bariatric surgery procedure selection; the need for shared decision-making. Obes. Surg. 2014, 24, 1933–1939. [Google Scholar] [CrossRef] [PubMed]
- National Taiwan University Hospital. Center for Obesity, Life Style and Metabolic Surgery. 2019. Available online: https://www.ntuh.gov.tw/obesity/service/Pages/%E6%B8%9B%E7%A8%AE%E6%89%8B%E8%A1%93%E7%B5%A6%E4%BB%98.aspx (accessed on 1 October 2019).
- Wang, M.; Ma, L.; Yuen, H. Application of Family Shared Decision Making Model in Informed Consent of Surgery. Int. J. Chin. Comp. Philos. Med. 2013, 11, 140–145. [Google Scholar]
- Lin, M.L.; Wu, J.Y.W.; Huang, M.C. The Meaning of Autonomy in Chinese Culture: Obtaining Informed Consent for Operation. J. Nurs. 2008, 55, 69–72. [Google Scholar]
| Decision-Making Models | Traditional Medical Model | SDM | Informed Medical Model |
|---|---|---|---|
| Doctor’s role | Initiative: Only explain the selected information to the patient and choose the treatment they think is best. | Initiative: Explain all information and treatment possibilities to the patient. Can recommend an option. Work with the patient to determine the treatment method. | Passive: Explain all the information and treatment possibilities to the patient. Withhold advice. Do not make any decisions. |
| Patient’s role | Passive: Accept the advice of the clinician. It is necessary to cooperate with the doctor during patient recovery. | Initiative: Receive all information. Have their own judgments about the hazards and benefits of treatment options. Discuss their preferences with the clinician. Determine the treatment with the clinician. | Initiative: Receive all information. Form their own judgment. The patient is free to choose from the options provided by the clinician and can determine the treatment on their own. |
| Information | One way (largely) Doctor → Patient | Two way Patient ↔ Doctor | One way (largely) Doctor → Patient |
| Discussion | Doctor alone or with other doctors | Doctors and patients (plus potential others) | Patient (plus potential others) |
| Who makes a decision? | Doctor | Doctor and Patient | Patient |
| Situation | Description | |
|---|---|---|
| Applicable situation | 1. There is no clear empirical medical conclusion, or the timing of SDM is appropriate, as suggested by clinical diagnosis and treatment guidelines. | 1. Existing evidence does not present strongly recommended options. 2. If the advantages and disadvantages of the options are close (benefit, risk, difficulty, or cost), then patient preference is an important determinant. |
| 2. Patient values and preferences vary greatly (different choices). | 1. The option has an effect or side effect that the patient cares about, such as possible significant physical or mental function, image change, or pain. | |
| 3. The balance of benefits and risks depends on the patient’s actions. | 1. For example: patient medication, continuous monitoring, and dietary compliance. | |
| 4. Serious illness. | 1. For example: serious life-threatening diseases, advanced stages of major chronic diseases, multiple and debilitating chronic diseases. | |
| Not an applicable situation | 1. The quality and conclusion of the evidence can provide strong suggestions, the advantages outweigh the disadvantages, and the patient value and preference are high. | 1. This topic is suitable for direct execution, without the need for SDM with the patient. 2. Unless the patient has other considerations, this option does not need to be included in the discussion. |
| Variables | Categories | Female Group (n = 64) | Male Group (n = 39) | p-Value |
|---|---|---|---|---|
| Age, years | 35.6 ± 11.4 | 37.3 ± 9.9 | 0.489 | |
| Education, n (%) | Junior high school (inclusive) or below | 9 (14%) | 3 (7.8%) | 0.291 |
| High school or vocational high school | 27 (42.2%) | 13 (33.3%) | ||
| University (inclusive) or above | 28 (43.8%) | 23 (58.9%) | ||
| Operation methods, n (%) | Mini-gastric bypass surgery | 33 (51.6%) | 25 (64.1%) | 0.187 |
| Roux-en-Y gastric bypass surgery | 4 (6.2%) | 0 (%) | ||
| Sleeve gastrectomy surgery | 27 (42.2%) | 14 (35.9%) | ||
| Body mass index (BMI) | 39.0 ± 6.5 | 42.8 ± 7.7 | 0.015 * | |
| Patients with diabetes mellitus, n (%) | 1 (1.6%) | 9 (23.1%) | <0.001 * |
| Variables | Mean (Standard Deviation) | PDA Use Experience | Decision Satisfaction | Decision Regret |
|---|---|---|---|---|
| PDA use experience | 4.3 (0.6) | 1 | ||
| Decision satisfaction | 4.4 (0.5) | 0.522 ** | 1 | |
| Decision regret | 1.6 (0.6) | −0.451 ** | −0.711 ** | 1 |
| Variables | Categories/Range | Female Group (n = 64) | Male Group (n = 39) | p-Value |
|---|---|---|---|---|
| Correct answer rate | I will be able to eat normal amounts of food. | 76.6% (49) | 82.1% (32) | 0.623 |
| Having weight-loss surgery can cause problems, but my being very overweight can also cause health problems. | 92.2% (59) | 100% (39) | 0.154 | |
| Surgery may be an option for me because my BMI is higher than 40. | 87.5% (56) | 89.7% (35) | 0.731 | |
| Making decisions with confidence | 4.4 ± 0.9 | 4.7 ± 0.7 | 0.067 | |
| PDA use experience | 4.3 ± 0.6 | 4.2 ± 0.6 | 0.696 | |
| Decision satisfaction | 4.4 ± 0.5 | 4.3 ± 0.5 | 0.316 | |
| Decision regret | 1.6 ± 0.5 | 1.7 ± 0.6 | 0.640 | |
| Main surgical decision maker | Patient | 18.8% (12) | 25.6% (10) | 0.015 * |
| Spouse | 14.1% (9) | 25.6% (10) | ||
| Children or children-in-law | 12.4% (8) | 0% (0) | ||
| Parents | 32.8% (21) | 43.6% (17) | ||
| Other | 21.9% (14) | 5.2% (2) |
| Maker | Patient | Spouse | Children or Spouse | Parents | Other | p-Value | |
|---|---|---|---|---|---|---|---|
| Education | |||||||
| Junior high school (inclusive) or below | 16.7% (2) | 8.3% (1) | 33.3% (4) | 16.7% (2) | 25% (3) | 0.004 * | |
| High school or vocational high school | 20% (8) | 15% (6) | 7.5% (3) | 32.5% (13) | 25% (10) | ||
| University (inclusive) or above | 23.5% (12) | 23.5% (12) | 2% (1) | 45.1% (23) | 5.9% (3) | ||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, Y.-C.; Wu, W.-L. Shared Decision Making and Choice for Bariatric Surgery. Int. J. Environ. Res. Public Health 2019, 16, 4966. https://doi.org/10.3390/ijerph16244966
Lee Y-C, Wu W-L. Shared Decision Making and Choice for Bariatric Surgery. International Journal of Environmental Research and Public Health. 2019; 16(24):4966. https://doi.org/10.3390/ijerph16244966
Chicago/Turabian StyleLee, Yi-Chih, and Wei-Li Wu. 2019. "Shared Decision Making and Choice for Bariatric Surgery" International Journal of Environmental Research and Public Health 16, no. 24: 4966. https://doi.org/10.3390/ijerph16244966
APA StyleLee, Y.-C., & Wu, W.-L. (2019). Shared Decision Making and Choice for Bariatric Surgery. International Journal of Environmental Research and Public Health, 16(24), 4966. https://doi.org/10.3390/ijerph16244966





