Coaching and Prompting for Remote Physical Activity Promotion: Study Protocol of a Three-Arm Randomized Controlled Trial (Movingcall)
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Recruitment and Sample Size
2.3. Inclusion Criteria
2.4. Group Allocation
2.5. Program Development
2.5.1. Theoretical Foundation
2.5.2. Intervention Content
2.6. Intervention Delivery
2.6.1. Tailoring
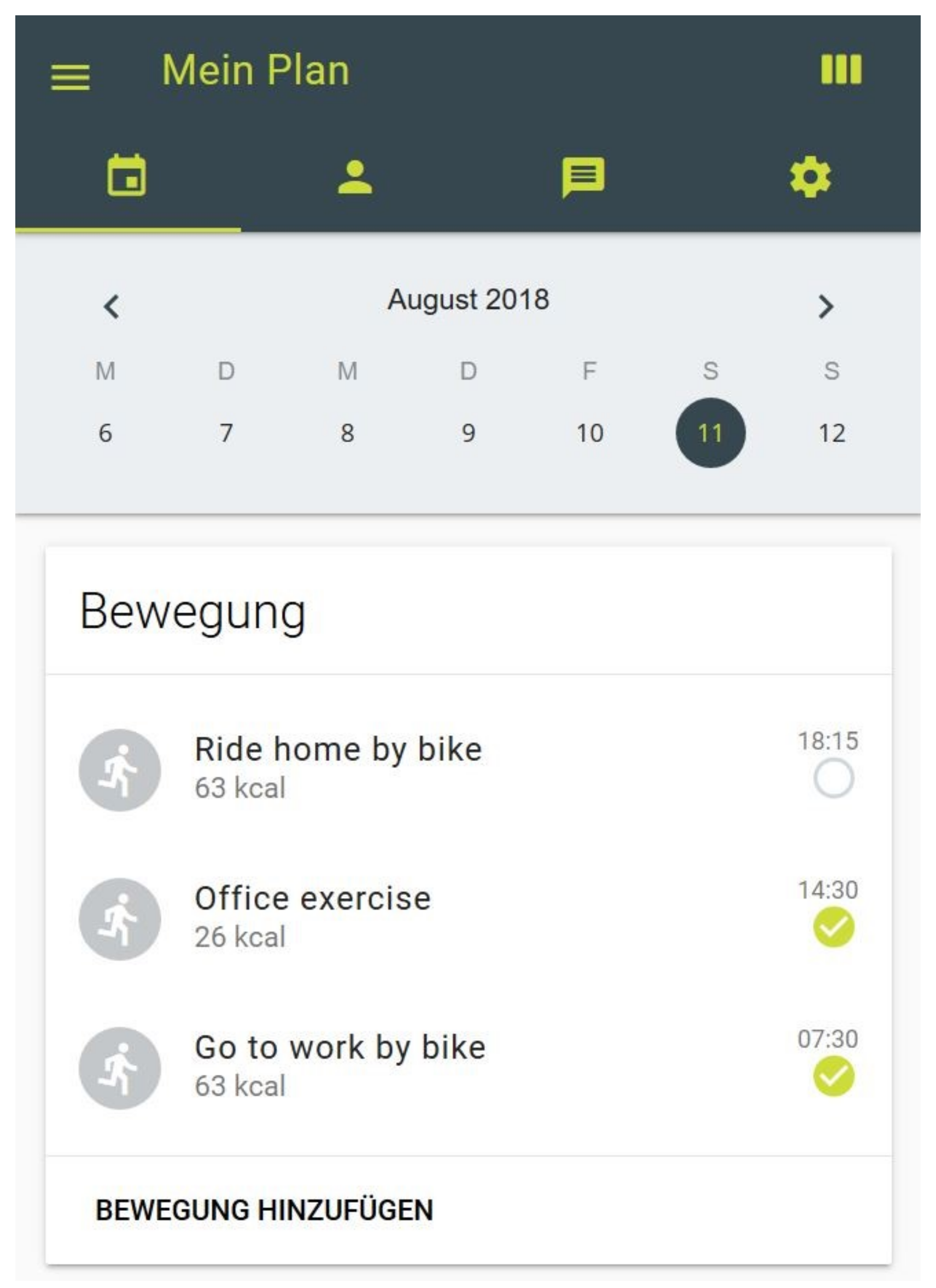
2.6.2. Activity Profile
2.6.3. Telephone Coaching (Coaching Group)
2.6.4. Telephone Coaching and SMS Prompting (Coaching and SMS Group)
2.6.5. Intervention Provider
2.6.6. Intervention Documentation and Assessment of Adherence
2.6.7. Minimal Intervention (Control Group)
2.7. Assessment of Primary and Secondary Outcomes
2.7.1. Self-Reported Physical Activity
2.7.2. ActiGraph Data
2.7.3. Psychosocial Determinants of PA and other Measures
- Intention: Motivational readiness for PA-related behavior change is assessed according to the stages of change of the Transtheoretical Model [56,76]. Participants select one out of five answers to the question “Are you regularly physically active, this means at least 20 minutes on 3 days of the week?”, e.g., “No, but I intend to become more physically active in the next 6 months”. A single item to measure the strength of intention is added. Participants quantify their intention to be regularly physically active on a scale from zero (no intention) to five (very strong intention) [57,63].
- Action planning is measured by five items [61]. Participants are asked if they defined when, where, how, how often, and with whom they plan to exercise. For example “I have made a detailed plan regarding when to exercise”. Answers are given on a Likert-scale from one (not true) to four (completely true).
- Outcome expectations regarding regular PA are assessed with 16 items validated by Fuchs [59]. Participants are asked to rate their expectations towards specific outcomes on a Likert-scale ranging from one (not true) to four (completely true). For example “If I were physically active on a regular basis, I would lose weight”.
- Self-efficacy is assessed consistently with Fuchs [60] by three items. The confidence to begin, to maintain and to restart regular PA is measured on a six-point Likert-scale from one (No confidence) to four (100% confidence). For example, “I am confident that I could start with new physical activity”.
- Perceived barriers: Participants are presented 19 potential barriers (e.g., “being tired”) and asked to indicate how strong each one prevented PA on a Likert-scale from one (not at all) to four (very much) [46].
- Coping strategies on barriers are measured by five items applied and validated by Sniehotta et al. [58]. For example “I have made a detailed plan regarding what to do if something interferes with my plans”. Responses are given on a four-point Likert-scale from one (not true) to four (completely true).
- Social support is assessed by seven items that rate the confidence for support of the social environment on a four-point Likert-scale from one (never) to four (always) [62]. For example, “I am confident that people of my social environment will be physically active with me”.
- Self-concordance is measured by four items on the self-concordance scale. The scale was composed and validated by Seelig and Fuchs [63]. Participants are asked to rate their internal/external motivation on a Likert-scale ranging from one (completely false) to four (completely true). For example, “If I am physically active within the next weeks and months, this is because other people say I should”.
- Knowledge about health enhancing PA and fitness rating: Participants are asked to rate their fitness level (on a scale from one to ten, one item) [64] and their level of health-enhancing PA (“Do you think you are sufficiently active for your health? Yes/No”, one item) [65]. Knowledge of general PA recommendations are assessed by two items previously used by Gerber et al. [66].
- Perceived stress-related exhaustion symptoms are measured by the validated Shirom–Melamed Burnout Measure (SMBM) [67]. Three subscales (physical fatigue, emotional exhaustion and cognitive weariness) are assessed within 14 items.
- Health-related quality of life: The Short–Form 12 Questionnaire (SF-12) is used to assess health-related quality of life [68,69]. The questionnaire includes 12 items on general physical health status and mental health distress. The questionnaire’s validity and reliability has been demonstrated by Craig et al. [36].
2.8. Data Processing and Statistical Analysis
3. Discussion
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Lee, I.M.; Shiroma, E.J.; Lobelo, F.; Puska, P.; Blair, S.N.; Katzmarzyk, P.T. Effect of physical inactivity on major non-communicable diseases worldwide: An analysis of burden of disease and life expectancy. Lancet 2012, 380, 219–229. [Google Scholar] [CrossRef]
- WHO. Global Recommendations on Physical Activity for Health; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Stamm, H.P.; Fischer, A.; Wiegand, D.; Lamprecht, M. Indikatorensammlung zum Monitoring-System Ernährung und Bewegung (Moseb); Bundesamt für Gesundheit (BAG): Bern, Switzerland, 2017. [Google Scholar]
- Hallal, P.C.; Andersen, L.B.; Bull, F.C.; Guthold, R.; Haskell, W.; Ekelund, U. Lancet Physical Activity Series Working Group. Global physical activity levels: Surveillance progress, pitfalls, and prospects. Lancet 2012, 380, 247–257. [Google Scholar] [CrossRef]
- Borodulin, K.; Sipila, N.; Rahkonen, O.; Leino-Arjas, P.; Kestila, L.; Jousilahti, P.; Prattala, R. Socio-demographic and behavioral variation in barriers to leisure-time physical activity. Scand. J. Public Health 2016, 44, 62–69. [Google Scholar] [CrossRef] [PubMed]
- Heath, G.W.; Parra, D.C.; Sarmiento, O.L.; Andersen, L.B.; Owen, N.; Goenka, S.; Montes, F.; Brownson, R.C. Evidence-based intervention in physical activity: Lessons from around the world. Lancet 2012, 380, 272–281. [Google Scholar] [CrossRef]
- Noar, S.M.; Benac, C.N.; Harris, M.S. Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychol. Bull. 2007, 133, 673–693. [Google Scholar] [CrossRef] [PubMed]
- Foster, C.; Richards, J.; Thorogood, M.; Hillsdon, M. Remote and web 2.0 interventions for promoting physical activity. Cochrane Database Syst. Rev. 2013, 9, Cd010395. [Google Scholar] [PubMed]
- Thomas, J.G.; Bond, D.S. Review of innovations in digital health technology to promote weight control. Curr. Diabetes Rep. 2014, 14, 485. [Google Scholar] [CrossRef] [PubMed]
- Lewis, B.A.; Napolitano, M.A.; Buman, M.P.; Williams, D.M.; Nigg, C.R. Future directions in physical activity intervention research: Expanding our focus to sedentary behaviors, technology, and dissemination. J. Behav. Med. 2017, 40, 112–126. [Google Scholar] [CrossRef]
- Olsen, J.M. Health coaching: A concept analysis. Nurs. Forum 2014, 49, 18–29. [Google Scholar] [CrossRef]
- Goode, A.D.; Reeves, M.M.; Eakin, E.G. Telephone-delivered interventions for physical activity and dietary behavior change: An updated systematic review. Am. J. Prev. Med. 2012, 42, 81–88. [Google Scholar] [CrossRef]
- Eakin, E.G.; Lawler, S.P.; Vandelanotte, C.; Owen, N. Telephone interventions for physical activity and dietary behavior change: A systematic review. Am. J. Prev. Med. 2007, 32, 419–434. [Google Scholar] [CrossRef]
- O’Hara, B.J.; Phongsavan, P.; Venugopal, K.; Eakin, E.G.; Eggins, D.; Caterson, H.; King, L.; Allman-Farinelli, M.; Haas, M.; Bauman, A.E. Effectiveness of australia’s get healthy information and coaching service(r): Translational research with population wide impact. Prev. Med. 2012, 55, 292–298. [Google Scholar] [CrossRef] [PubMed]
- Joseph, R.P.; Durant, N.H.; Benitez, T.J.; Pekmezi, D.W. Internet-based physical activity interventions. Am. J. Lifestyle Med. 2014, 8, 42–68. [Google Scholar] [CrossRef] [PubMed]
- Davies, C.A.; Spence, J.C.; Vandelanotte, C.; Caperchione, C.M.; Mummery, W.K. Meta-analysis of internet-delivered interventions to increase physical activity levels. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 52. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Leon, E.; Fuentes, L.W.; Cohen, J.E. Characterizing periodic messaging interventions across health behaviors and media: Systematic review. J. Med. Internet Res. 2014, 16, e93. [Google Scholar] [CrossRef] [PubMed]
- Hall, A.K.; Cole-Lewis, H.; Bernhardt, J.M. Mobile text messaging for health: A systematic review of reviews. Annu. Rev. Public Health 2015, 36, 393–415. [Google Scholar] [CrossRef] [PubMed]
- Armanasco, A.A.; Miller, Y.D.; Fjeldsoe, B.S.; Marshall, A.L. Preventive health behavior change text message interventions: A meta-analysis. Am. J. Prev. Med. 2017, 52, 391–402. [Google Scholar] [CrossRef] [PubMed]
- Head, K.J.; Noar, S.M.; Iannarino, N.T.; Grant Harrington, N. Efficacy of text messaging-based interventions for health promotion: A meta-analysis. Soc. Sci. Med. 2013, 97, 41–48. [Google Scholar] [CrossRef] [PubMed]
- Michie, S.; Richardson, M.; Johnston, M.; Abraham, C.; Francis, J.; Hardeman, W.; Eccles, M.P.; Cane, J.; Wood, C.E. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: Building an international consensus for the reporting of behavior change interventions. Ann. Behav. Med. 2013, 46, 81–95. [Google Scholar] [CrossRef]
- Bird, E.L.; Baker, G.; Mutrie, N.; Ogilvie, D.; Sahlqvist, S.; Powell, J. Behavior change techniques used to promote walking and cycling: A systematic review. Health Psychol. 2013, 32, 829–838. [Google Scholar] [CrossRef]
- Olander, E.K.; Fletcher, H.; Williams, S.; Atkinson, L.; Turner, A.; French, D.P. What are the most effective techniques in changing obese individuals’ physical activity self-efficacy and behavior: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2013, 10, 29. [Google Scholar] [CrossRef] [PubMed]
- Michie, S.; Abraham, C.; Whittington, C.; McAteer, J.; Gupta, S. Effective techniques in healthy eating and physical activity interventions: A meta-regression. Health Psychol. 2009, 28, 690–701. [Google Scholar] [CrossRef] [PubMed]
- Burke, L.E.; Wang, J.; Sevick, M.A. Self-monitoring in weight loss: A systematic review of the literature. J. Am. Diet. Assoc. 2011, 111, 92–102. [Google Scholar] [CrossRef] [PubMed]
- Greaves, C.J.; Sheppard, K.E.; Abraham, C.; Hardeman, W.; Roden, M.; Evans, P.H.; Schwarz, P. Systematic review of reviews of intervention components associated with increased effectiveness in dietary and physical activity interventions. BMC Public Health 2011, 11, 119. [Google Scholar] [CrossRef] [PubMed]
- Webb, T.L.; Joseph, J.; Yardley, L.; Michie, S. Using the internet to promote health behavior change: A systematic review and meta-analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. J. Med. Internet Res. 2010, 12, e4. [Google Scholar] [CrossRef]
- Dombrowski, S.U.; Sniehotta, F.F.; Avenell, A.; Johnston, M.; MacLennan, G.; Araújo-Soares, V. Identifying active ingredients in complex behavioral interventions for obese adults with obesity-related co-morbidities or additional risk factors for co-morbidities: A systematic review. Health Psychol. Rev. 2012, 6, 7–32. [Google Scholar] [CrossRef]
- Ashford, S.; Edmunds, J.; French, D.P. What is the best way to change self-efficacy to promote lifestyle and recreational physical activity? A systematic review with meta-analysis. Br. J. Health Psychol. 2010, 15, 265–288. [Google Scholar] [CrossRef] [PubMed]
- Dusseldorp, E.; van Genugten, L.; van Buuren, S.; Verheijden, M.W.; van Empelen, P. Combinations of techniques that effectively change health behavior: Evidence from meta-cart analysis. Health Psychol. 2014, 33, 1530–1540. [Google Scholar] [CrossRef]
- Williams, S.L.; French, D.P. What are the most effective intervention techniques for changing physical activity self-efficacy and physical activity behavior—And are they the same? Health Educ. Res. 2011, 26, 308–322. [Google Scholar] [CrossRef]
- Samdal, G.B.; Eide, G.E.; Barth, T.; Williams, G.; Meland, E. Effective behavior change techniques for physical activity and healthy eating in overweight and obese adults; systematic review and meta-regression analyses. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 42. [Google Scholar] [CrossRef]
- Prochaska, J.O.; Evers, K.E.; Castle, P.H.; Johnson, J.L.; Prochaska, J.M.; Rula, E.Y.; Coberley, C.; Pope, J.E. Enhancing multiple domains of well-being by decreasing multiple health risk behaviors: A randomized clinical trial. Popul. Health Manag. 2012, 15, 276–286. [Google Scholar] [CrossRef] [PubMed]
- Richards, J.; Thorogood, M.; Hillsdon, M.; Foster, C. Face-to-face versus remote and web 2.0 interventions for promoting physical activity. Cochrane Database Syst. Rev. 2013, 9, Cd010393. [Google Scholar]
- Blair, S.N.; Haskell, W.L.; Ho, P.; Paffenbarger, R.S., Jr.; Vranizan, K.M.; Farquhar, J.W.; Wood, P.D. Assessment of habitual physical activity by a seven-day recall in a community survey and controlled experiments. Am. J. Epidemiol. 1985, 122, 794–804. [Google Scholar] [CrossRef] [PubMed]
- Craig, C.L.; Marshall, A.L.; Sjostrom, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef] [PubMed]
- King, A.C.; Friedman, R.; Marcus, B.; Castro, C.; Napolitano, M.; Ahn, D.; Baker, L. Ongoing physical activity advice by humans versus computers: The community health advice by telephone (chat) trial. Health Psychol. 2007, 26, 718–727. [Google Scholar] [CrossRef] [PubMed]
- Vandelanotte, C.; Muller, A.M.; Short, C.E.; Hingle, M.; Nathan, N.; Williams, S.L.; Lopez, M.L.; Parekh, S.; Maher, C.A. Past, present, and future of ehealth and mhealth research to improve physical activity and dietary behaviors. JMIR Res. Protoc. 2016, 48, 219–228.e211. [Google Scholar] [CrossRef] [PubMed]
- Vickers, A.J.; Altman, D.G. Statistics notes: Analysing controlled trials with baseline and follow up measurements. BMJ 2001, 323, 1123–1124. [Google Scholar] [CrossRef]
- Rosenbaum, S.; Ward, P.B. The simple physical activity questionnaire. Lancet Psychiatry 2016, 3, e1. [Google Scholar] [CrossRef]
- Thomas, S.; Reading, J.; Shephard, R.J. Revision of the physical activity readiness questionnaire (par-q). Can. J. Sport Sci. 1992, 17, 338–345. [Google Scholar]
- Saghaei, M. An overview of randomization and minimization programs for randomized clinical trials. J. Med. Signals Sens. 2011, 1, 55–61. [Google Scholar]
- Michie, S.; Atkins, L.; West, R. The Behavior Change Wheel: A Guide to Designing Interventions; Silverback Publishing: London, UK, 2014. [Google Scholar]
- Michie, S.; van Stralen, M.M.; West, R. The behavior change wheel: A new method for characterising and designing behavior change interventions. Implement. Sci. 2011, 6, 42. [Google Scholar] [CrossRef] [PubMed]
- Cane, J.; O’Connor, D.; Michie, S. Validation of the theoretical domains framework for use in behavior change and implementation research. Implement. Sci. 2012, 7, 37. [Google Scholar] [CrossRef] [PubMed]
- Fuchs, R.; Seelig, H.; Gohner, W.; Burton, N.W.; Brown, W.J. Cognitive mediation of intervention effects on physical exercise: Causal models for the adoption and maintenance stage. Psychol. Health 2012, 27, 1480–1499. [Google Scholar] [CrossRef] [PubMed]
- Schwarzer, R. Modeling health behavior change: How to predict and modify the adoption and maintenance of health behaviors. Appl. Psychol. 2008, 57, 1–29. [Google Scholar] [CrossRef]
- Michie, S.; Ashford, S.; Sniehotta, F.F.; Dombrowski, S.U.; Bishop, A.; French, D.P. A refined taxonomy of behavior change techniques to help people change their physical activity and healthy eating behaviors: The calo-re taxonomy. Psychol. Health 2011, 26, 1479–1498. [Google Scholar] [CrossRef] [PubMed]
- Abraham, C.; Michie, S. A taxonomy of behavior change techniques used in interventions. Health Psychol. 2008, 27, 379–387. [Google Scholar] [CrossRef]
- Michie, S.; Johnston, M.; Francis, J.; Hardeman, W.; Eccles, M. From theory to intervention: Mapping theoretically derived behavioral determinants to behavior change techniques. Appl. Psychol. 2008, 57, 660–680. [Google Scholar] [CrossRef]
- Cane, J.; Richardson, M.; Johnston, M.; Ladha, R.; Michie, S. From lists of behavior change techniques (bcts) to structured hierarchies: Comparison of two methods of developing a hierarchy of bcts. Br. J. Health Psychol. 2015, 20, 130–150. [Google Scholar] [CrossRef]
- Vogel, D.; Usov, A.; Fischer, X.; Donath, L.; Zahner, L. Movingcall activity-profile. Available online: https://www.movingcall.com (accessed on 17 January 2018).
- Ainsworth, B.E.; Haskell, W.L.; Herrmann, S.D.; Meckes, N.; Bassett, D.R., Jr.; Tudor-Locke, C.; Greer, J.L.; Vezina, J.; Whitt-Glover, M.C.; Leon, A.S. 2011 compendium of physical activities: A second update of codes and met values. Med. Sci. Sports Exerc. 2011, 43, 1575–1581. [Google Scholar] [CrossRef]
- Eysenbach, G. The law of attrition. J. Med. Internet Res. 2005, 7, e11. [Google Scholar] [CrossRef]
- Gabrys, L.; Thiel, C.; Tallner, A.; Wilms, B.; Müller, C.; Kahlert, D.; Jekauc, D.; Frick, F.; Schulz, H.; Sprengeler, O.; et al. Akzelerometrie zur erfassung körperlicher aktivität. Sportwissenschaft 2015, 45, 1–9. [Google Scholar] [CrossRef]
- Fuchs, R. Aufbau Eines Körperlich-Aktiven Lebensstils: Theorie, Empirie und Praxis; Hogrefe: Göttingen, Germany, 2007. [Google Scholar]
- Gerber, M.; Fuchs, R.; Pühse, U. Follow-up of a short motivational and volitional exercise-intervention trial with overweight and obese individuals. Schweiz. Z. Sportmed. Sporttraumatologie 2010, 58, 108–114. [Google Scholar]
- Sniehotta, F.F.; Schwarzer, R.; Scholz, U.; Schüz, B. Action planning and coping planning for long-term lifestyle change: Theory and assessment. Eur. J. Soc. Psychol. 2005, 35, 565–576. [Google Scholar] [CrossRef]
- Fuchs, R. Konsequenzerwartungena ls determinante des sport- und bewegungsverhaltens. Z. Gesundheitspsychologie 1994, 2, 269–291. [Google Scholar]
- Fuchs, R. Aufbau Eines Körperlich-Aktiven Lebensstils im Kontext der Medizinischen Rehabilitation: Ein Motivational-Volitionales Interventionskonzept (Movo-Lisa Projekt); Universität Freiburg: Freiburg im Breisgau, Germany, 2008. [Google Scholar]
- Sniehotta, F.F.; Scholz, U.; Schwarzer, R. Bridging the intention–behavior gap: Planning, self-efficacy, and action control in the adoption and maintenance of physical exercise. Psychol. Health 2005, 20, 143–160. [Google Scholar] [CrossRef]
- Fuchs, R. Psychologie und Körperliche Bewegung: Grundlagen für Theoriegeleitete Interventionen; Hogrefe Verlag für Psychologie: Göttingen, Germany, 1997. [Google Scholar]
- Seelig, H.; Fuchs, R. Messung der sport- und bewegungsbezogenen selbstkonkordanz. Z. Sportpsychol. 2006, 13, 121–139. [Google Scholar] [CrossRef]
- Plante, T.; Lantis, A.; Checa, G. The influence of perceived versus aerobic fitness on psychological health and physiological stress responsivity. Int. J. Stress Manag. 1998, 5, 141–156. [Google Scholar] [CrossRef]
- Martin, B.W. Physical activity related attitudes, knowledge and behavior in the swiss population: Comparison of the hepa surveys 2001 and 1999. Schweiz. Z. Sportmed. Sporttraumatologie 2002, 50, 164–168. [Google Scholar]
- Gerber, M.; Oberer, N.; Pühse, U. Beweg Dich Gesund! Ein Praktischer Ratgeber für ein Körperlich Aktives Leben; Meyer & Meyer Verlag: Aachen, Germany, 2014. [Google Scholar]
- Shirom, A.; Melamed, S. A comparison of the construct validity of two burnout measures in two groups of professionals. Int. J. Stress Manag. 2006, 13, 176–200. [Google Scholar] [CrossRef]
- Bullinger, M. German translation and psychometric testing of the sf-36 health survey: Rteliminary results from the iqola project. Soc. Sci. Med. 1995, 41, 1359–1366. [Google Scholar] [CrossRef]
- Ware, J., Jr.; Kosinski, M.; Keller, S.D. A 12-item short-form health survey: Construction of scales and preliminary tests of reliability and validity. Med. Care 1996, 34, 220–233. [Google Scholar] [CrossRef] [PubMed]
- Schilling, R.; Scharli, E.; Fischer, X.; Donath, L.; Faude, O.; Brand, S.; Puhse, U.; Zahner, L.; Rosenbaum, S.; Ward, P.B.; et al. The utility of two interview-based physical activity questionnaires in healthy young adults: Comparison with accelerometer data. PLoS ONE 2018, 13, e0203525. [Google Scholar] [CrossRef] [PubMed]
- Hayden-Wade, H.A.; Coleman, K.J.; Sallis, J.F.; Armstrong, C. Validation of the telephone and in-person interview versions of the 7-day par. Med. Sci. Sports Exerc. 2003, 35, 801–809. [Google Scholar] [CrossRef] [PubMed]
- Lee, P.H.; Macfarlane, D.J.; Lam, T.H.; Stewart, S.M. Validity of the international physical activity questionnaire short form (ipaq-sf): A systematic review. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 115. [Google Scholar] [CrossRef] [PubMed]
- Ellis, K.; Kerr, J.; Godbole, S.; Lanckriet, G.; Wing, D.; Marshall, S. A random forest classifier for the prediction of energy expenditure and type of physical activity from wrist and hip accelerometers. Physiol. Meas. 2014, 35, 2191–2203. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dieu, O.; Mikulovic, J.; Fardy, P.S.; Bui-Xuan, G.; Beghin, L.; Vanhelst, J. Physical activity using wrist-worn accelerometers: Comparison of dominant and non-dominant wrist. Clin. Physiol. Funct. Imaging 2017. [Google Scholar] [CrossRef]
- Freedson, P.S.; John, D. Comment on “estimating activity and sedentary behavior from an accelerometer on the hip and wrist”. Med. Sci. Sports Exerc. 2013, 45, 962–963. [Google Scholar] [CrossRef]
- Marcus, B.H.; Rakowski, W.; Rossi, J.S. Assessing motivational readiness and decision making for exercise. Health Psychol. 1992, 11, 257–261. [Google Scholar] [CrossRef]
- Kamada, M.; Shiroma, E.J.; Harris, T.B.; Lee, I.M. Comparison of physical activity assessed using hip- and wrist-worn accelerometers. Gait Posture 2016, 44, 23–28. [Google Scholar] [CrossRef] [Green Version]
- Kim, Y.; Lee, J.M.; Peters, B.P.; Gaesser, G.A.; Welk, G.J. Examination of different accelerometer cut-points for assessing sedentary behaviors in children. PLoS ONE 2014, 9, e90630. [Google Scholar] [CrossRef]
- McMinn, D.; Acharya, R.; Rowe, D.A.; Gray, S.R.; Allan, J.L. Measuring activity energy expenditure: Accuracy of the gt3x+ and actiheart monitors. Int. J. Exerc. Sci. 2013, 6, 217–229. [Google Scholar]
- Cole, R.J.; Kripke, D.F.; Gruen, W.; Mullaney, D.J.; Gillin, J.C. Automatic sleep/wake identification from wrist activity. Sleep 1992, 15, 461–469. [Google Scholar] [CrossRef] [PubMed]
- Troiano, R.P. Large-scale applications of accelerometers: New frontiers and new questions. Med. Sci. Sports Exerc. 2007, 39, 1501. [Google Scholar] [CrossRef] [PubMed]
- Clemente, F.M.; Nikolaidis, P.T.; Martins, F.M.; Mendes, R.S. Physical activity patterns in university students: Do they follow the public health guidelines? PLoS ONE 2016, 11, e0152516. [Google Scholar] [CrossRef] [PubMed]
- Stang, A.; Poole, C.; Kuss, O. The ongoing tyranny of statistical significance testing in biomedical research. Eur. J. Epidemiol. 2010, 25, 225–230. [Google Scholar] [CrossRef] [Green Version]
- Stovitz, S.D.; Verhagen, E.; Shrier, I. Misinterpretations of the ‘p value’: A brief primer for academic sports medicine. Br. J. Sports Med. 2017, 51, 1176–1177. [Google Scholar] [CrossRef] [PubMed]
- van Wier, M.F.; Ariens, G.A.; Dekkers, J.C.; Hendriksen, I.J.; Smid, T.; van Mechelen, W. Phone and e-mail counselling are effective for weight management in an overweight working population: A randomized controlled trial. BMC Public Health 2009, 9, 6. [Google Scholar] [CrossRef] [PubMed]
- Marcus, B.H.; Napolitano, M.A.; King, A.C.; Lewis, B.A.; Whiteley, J.A.; Albrecht, A.; Parisi, A.; Bock, B.; Pinto, B.; Sciamanna, C.; et al. Telephone versus print delivery of an individualized motivationally tailored physical activity intervention: Project stride. Health Psychol. 2007, 26, 401–409. [Google Scholar] [CrossRef]
- van Keulen, H.M.; Mesters, I.; Ausems, M.; van Breukelen, G.; Campbell, M.; Resnicow, K.; Brug, J.; de Vries, H. Tailored print communication and telephone motivational interviewing are equally successful in improving multiple lifestyle behaviors in a randomized controlled trial. Ann. Behav. Med. 2011, 41, 104–118. [Google Scholar] [CrossRef]
- Patrick, K.; Raab, F.; Adams, M.A.; Dillon, L.; Zabinski, M.; Rock, C.L.; Griswold, W.G.; Norman, G.J. A text message-based intervention for weight loss: Randomized controlled trial. J. Med. Internet Res. 2009, 11, e1. [Google Scholar] [CrossRef]
- Lamprecht, M.; Fischer, A.; Stamm, H.P. Sport Schweiz 2014. Sportaktivität und Sportinteresse der Schweizer Bevölkerung; Bundesamt für Sport: Magglingen, Switzerland, 2014. [Google Scholar]
- Freedland, K.E.; Mohr, D.C.; Davidson, K.W.; Schwartz, J.E. Usual and unusual care: Existing practice control groups in randomized controlled trials of behavioral interventions. Psychosom. Med. 2011, 73, 323–335. [Google Scholar] [CrossRef] [PubMed]
- Whitehead, W.E. Control groups appropriate for behavioral interventions. Gastroenterology 2004, 126, S159–S163. [Google Scholar] [CrossRef] [PubMed]

| BCT (V1 Number) | Definition |
|---|---|
| Goal setting (behavior) (1.1) | Set or agree on (a) behavioral goal(s) that leads to increased PA. |
| Problem solving (1.2) | Analyze, or prompt the person to analyze factors influencing PA and generate or select strategies to overcome barriers and/or increase facilitators. |
| Action planning (1.4) | Prompt detailed planning of PA (must include at least one of context, frequency, duration and intensity). Context may be environmental (physical or social) or internal (physical, emotional or cognitive). |
| Review of behavioral goal(s) (1.5) | Review PA goal(s) jointly with the person and consider modifying goal(s). This may lead to re-setting the same goal, a small change in that goal, or setting a new goal instead of (or in addition to) the first, or no change. |
| Feedback on behavior (2.2) | Give informative or evaluative feedback on monitored (including self-monitored) PA. |
| Self-monitoring of behavior (2.3) | Prompt self-monitoring and recording of PA (i.e., diary). |
| Social support (3.1) | Advise on, arrange or provide social support (e.g., from friends, relatives, colleagues, buddies or staff). This may include practical help (3.2) and emotional support (3.3) |
| Instruction on how to perform the behavior (4.1) | Teach skills and knowledge required for specific physical activities, i.e., give clear instructions. |
| Information about health consequences (5.1) | Provide information about health consequences of physical inactivity (PA). |
| Behavior practice/rehearsal (8.1) | Prompt practice or rehearsal of the PA one or more times in a context or at a time when the performance may not be necessary, in order to increase habit and skill. |
| Goal setting (outcome) (1.3) Discrepancy between current behavior and goal (1.6) Review outcome goal(s) (1.7) Behavioral contract (1.8) Time management (according to the ‘Coventry, Aberdeen & London – Refined’ (CALO-RE) Taxonomy [48]) Self-monitoring of outcome(s) of behavior (2.4) Feedback on outcome(s) of behavior (2.7) Provide information on consequences of behavior to the individual (5.2 and 5.6 summarized) Provide info on where and when (According the CALO-RE Taxonomy [48]) Demonstration of the behavior (6.1) Prompts/cues (7.1) Habit formation (8.3) | Habit reversal (8.4) Generalization of target behavior (8.6) Graded tasks (8.7) Pros and cons (9.2) Reward and threat (summarizing 10.4, 10.5, 10.7, 10.9) Restructuring the physical environment (12.1) Restructuring the social environment (12.2) Avoidance/reducing exposure to cues for the behavior (12.3) Adding objects to the environment (12.5) Framing/reframing (13.2) Mental rehearsal of successful performance (15.2) Focus on past success (15.3) Self-talk (15.4) |
| Topic | Example |
|---|---|
| Knowledge transfer | Dear Ruth, did you know that regular endurance exercise helps boost your immune system? |
| Feedback on performance | Hello Mr. Meier, based on your online entries, I have seen that you had an active weekend. Gardening and a long walk on Sunday, congratulations! |
| BCT | Dear Katy, take your time to think about what prevents you from using the bike to go to work. Let’s discuss these obstacles next time☺. Have a good day. |
| Reminder | Good morning Ms. Bianchi, today is your first after-work swimming session. Don’t forget to pack your swimwear and have fun! Regards |
| Outcome Measure | Data Collection Instrument | Measure Point (Months) |
|---|---|---|
| Inclusion criteria | Adapted version of the Simple Physical Activity Questionnaire (SIMPAQ) [40] | 0 |
| Readiness for PA | Physical Activity Readiness Questionnaire (PAR-Q) [41] | 0 |
| Socio-demographic data | Commonly used items | 0 |
| Physical activity level | SIMPAQ [40] | 0, 6, 12 |
| ActiGraph data of 7 days [55] | 0, 6, 12 | |
| Variables used for tailoring | Self-compiled questionnaire on personal situation | 0 |
| Self-compiled questionnaire on health restrictions, experience in PA and goals | 0 | |
| Psychosocial determinants | Intention [56,57] | 0, 6, 12 |
| Action planning [58] | 0, 6, 12 | |
| Outcome expectations [59] | 0, 6, 12 | |
| Self-efficacy [60]. | 0, 6, 12 | |
| Perceived barriers [46] | 0, 6, 12 | |
| Coping strategies [61] | 0, 6, 12 | |
| Social support [62] | 0, 6, 12 | |
| Self-concordance [63]. | 0, 6, 12 | |
| Knowledge about health enhancing PA and fitness rating [64,65,66] | 0, 6, 12 | |
| Perceived stress-related exhaustion symptoms | Shirom–Melamed Burnout Measure (SMBM) [67] | 0, 6, 12 |
| Health-related quality of life | Short-Form 12 Questionnaire (SF-12) [68,69] | 0, 6, 12 |
| Feedback on aspects of the | Self-compiled questionnaire on satisfaction and homepage usability | 3 |
| Intervention | Self-compiled questionnaire on intervention depending on study arm | 3, 6 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fischer, X.; Donath, L.; Zwygart, K.; Gerber, M.; Faude, O.; Zahner, L. Coaching and Prompting for Remote Physical Activity Promotion: Study Protocol of a Three-Arm Randomized Controlled Trial (Movingcall). Int. J. Environ. Res. Public Health 2019, 16, 331. https://doi.org/10.3390/ijerph16030331
Fischer X, Donath L, Zwygart K, Gerber M, Faude O, Zahner L. Coaching and Prompting for Remote Physical Activity Promotion: Study Protocol of a Three-Arm Randomized Controlled Trial (Movingcall). International Journal of Environmental Research and Public Health. 2019; 16(3):331. https://doi.org/10.3390/ijerph16030331
Chicago/Turabian StyleFischer, Xenia, Lars Donath, Kimberly Zwygart, Markus Gerber, Oliver Faude, and Lukas Zahner. 2019. "Coaching and Prompting for Remote Physical Activity Promotion: Study Protocol of a Three-Arm Randomized Controlled Trial (Movingcall)" International Journal of Environmental Research and Public Health 16, no. 3: 331. https://doi.org/10.3390/ijerph16030331
APA StyleFischer, X., Donath, L., Zwygart, K., Gerber, M., Faude, O., & Zahner, L. (2019). Coaching and Prompting for Remote Physical Activity Promotion: Study Protocol of a Three-Arm Randomized Controlled Trial (Movingcall). International Journal of Environmental Research and Public Health, 16(3), 331. https://doi.org/10.3390/ijerph16030331





