What Factors Affect Patient Satisfaction in Public Sector Hospitals: Evidence from an Emerging Economy
Abstract
:1. Introduction
2. Literature Review
2.1. Patient Satisfaction
2.2. Physical Facilities
2.3. Doctor–Patient Relationship
2.4. Laboratory Services
2.5. Pharmacy Services
3. Methodology
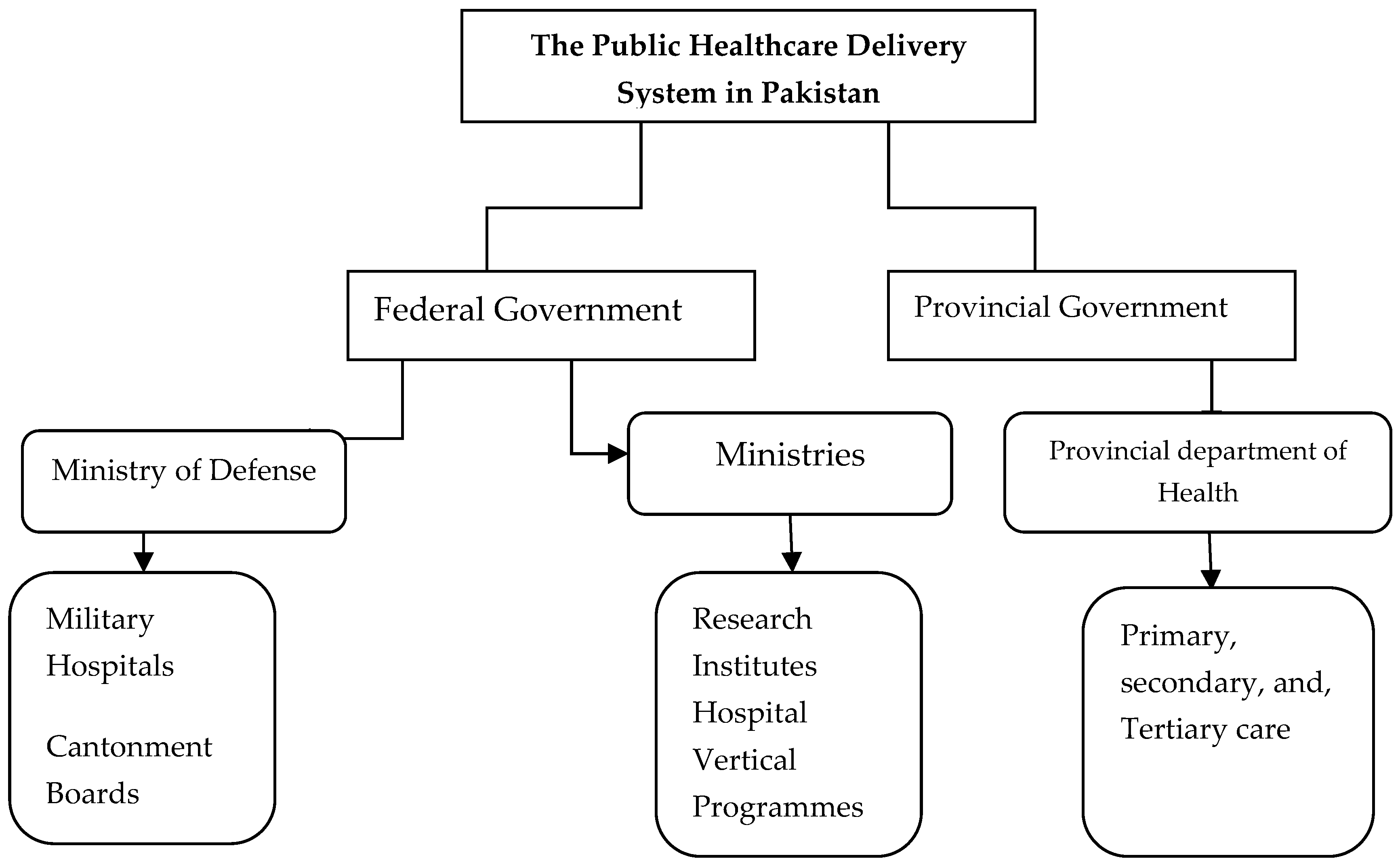
3.1. Study Setting
3.2. The Sample
3.3. Data Collection and Instruments
4. Results
4.1. Sociodemographic Characteristics
4.2. Statistical Analysis and Data Interpretation
4.3. Confirmatory Factor Analysis (CFA)
4.4. Hypothesis Testing Using a Multiple Regression Analysis
5. Discussion and Implications
6. Limitations and Future Research
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Mossialos, E.; Wenzl, M.; Osborn, R.; Sarnak, D. 2015 International Profiles of Health Care Systems; The Commonwealth Fund: New York, NY, USA, 2016. [Google Scholar]
- Duan, G.; Qiu, L.; Yu, W.; Hu, H. Outpatient service quality and doctor-patient relationship: A study in Chinese public hospital. Int. J. Serv. Econ. Manag. 2014, 6, 97–111. [Google Scholar] [CrossRef]
- Bahadori, M.; Teymourzadeh, E.; Faizy Bagejan, F.; Ravangard, R.; Raadabadi, M.; Hosseini, S.M. Factors affecting the effectiveness of quality control circles in a hospital using a combination of fuzzy VIKOR and Grey Relational Analysis. Proc. Singap. Healthc. 2018, 27, 180–186. [Google Scholar] [CrossRef]
- WHO. The Sustainable Development Goals; WHO: Geneva, Switzerland, 2015. [Google Scholar]
- Javed, S.A.; Ilyas, F. Service Quality and Satisfaction in Healthcare Sector of Pakistan–The Patients’ Expectations. Int. J. Health Care Qual. Assur. 2018, 31, 489–501. [Google Scholar] [CrossRef] [PubMed]
- Bank, W. Out-of-Pocket Expenditure (% of Current Health Expenditure). Available online: https://data.worldbank.org/indicator/SH.XPD.OOPC.CH.ZS (accessed on 26 December 2018).
- Irfan, S.; Ijaz, A. Comparison of service quality between private and public hospitals: Empirical evidences from Pakistan. J. Qual. Technol. Manag. 2011, 7, 1–22. [Google Scholar]
- Shabbir, A.; Malik, S.A.; Malik, S.A. Measuring patients’ healthcare service quality perceptions, satisfaction, and loyalty in public and private sector hospitals in Pakistan. Int. J. Qual. Reliab. Manag. 2016, 33, 538–557. [Google Scholar] [CrossRef]
- Gadit, A.A.M. Opinion and Debate-Corruption in medical practice: How far have we gone? JPMA-J. Pak. Med Assoc. 2011, 61, 93. [Google Scholar]
- Kumar, S.; Bano, S. Comparison and Analysis of Health Care Delivery Systems: Pakistan versus Bangladesh. J. Hosp. Med. Manag. 2017, 3, 1–7. [Google Scholar] [CrossRef]
- Shafiq, M.; Naeem, M.A.; Munawar, Z.; Fatima, I. Service Quality Assessment of Hospitals in Asian Context: An Empirical Evidence From Pakistan. INQUIRY J. Health Care Organ. Provis. Financ. 2017, 54, 0046958017714664. [Google Scholar] [CrossRef] [PubMed]
- Javed, S.A.; Liu, S. Evaluation of outpatient satisfaction and service quality of Pakistani healthcare projects: Application of a novel synthetic grey incidence analysis model. Grey Syst. Theory Appl. 2018, 8, 462–480. [Google Scholar] [CrossRef]
- Algudairi, G.; Al-Eisa, E.S.; Alghadir, A.H.; Iqbal, Z.A. Patient satisfaction with outpatient physical therapy in Saudi Arabia. BMC Health Serv. Res. 2018, 18, 888. [Google Scholar] [CrossRef]
- Devreux, I.C.; Jacquerye, A.; Kittel, F.; Elsayed, E.; Al-Awa, B. Benchmarking of patient satisfaction with physical rehabilitation services in various hospitals of Jeddah. Life Sci. J. 2012, 9, 73–78. [Google Scholar]
- Kamimura, A.; Ashby, J.; Myers, K.; Nourian, M.M.; Christensen, N. Satisfaction with healthcare services among free clinic patients. J. Community Health 2015, 40, 62–72. [Google Scholar] [CrossRef]
- Aljuaid, M.; Mannan, F.; Chaudhry, Z.; Rawaf, S.; Majeed, A. Quality of care in university hospitals in Saudi Arabia: a systematic review. BMJ Open 2016, 6, e008988. [Google Scholar] [CrossRef] [Green Version]
- Cheng, Y.; Raisch, D.W.; Borrego, M.E.; Gupchup, G.V. Economic, clinical, and humanistic outcomes (ECHOs) of pharmaceutical care services for minority patients: A literature review. Res. Soc. Adm. Pharm. 2013, 9, 311–329. [Google Scholar] [CrossRef]
- Jalil, A.; Zakar, R.; Zakar, M.Z.; Fischer, F. Patient satisfaction with doctor-patient interactions: a mixed methods study among diabetes mellitus patients in Pakistan. BMC Health Serv. Res. 2017, 17, 155. [Google Scholar] [CrossRef]
- Wankar, A.D. Study of determination of laboratory turnaround time in tertiary care hospital in India. Int. J. Res. Med Sci. 2017, 2, 1396–1401. [Google Scholar] [CrossRef]
- Anna, S. How the Physical Environment of a Hospital Affects Patient Health. Available online: https://today.mims.com/how-the-physical-environment-of-a-hospital-affects-patient-health (accessed on 21 December 2018).
- Ko, H.H.; Zhang, H.; Telford, J.J.; Enns, R. Factors influencing patient satisfaction when undergoing endoscopic procedures. Gastrointest. Endosc. 2009, 69, 883–891, quiz 891 e881. [Google Scholar] [CrossRef] [PubMed]
- Pilpel, D. Hospitalized patients’ satisfaction with caregivers’ conduct and physical surroundings. J. Gen. Intern. Med. 1996, 11, 312–314. [Google Scholar] [CrossRef] [PubMed]
- Aiken, L.H.; Clarke, S.P.; Sloane, D.M.; Lake, E.T.; Cheney, T. Effects of hospital care environment on patient mortality and nurse outcomes. J. Nurs. Adm. 2008, 38, 223. [Google Scholar] [CrossRef]
- Dijkstra, K.; Pieterse, M.; Pruyn, A. Physical environmental stimuli that turn healthcare facilities into healing environments through psychologically mediated effects: systematic review. J. Adv. Nurs. 2006, 56, 166–181. [Google Scholar] [CrossRef] [PubMed]
- Szasz, T.S.; Hollender, M.H. A contribution to the philosophy of medicine: the basic models of the doctor-patient relationship. AMA Arch. Intern. Med. 1956, 97, 585–592. [Google Scholar] [CrossRef] [PubMed]
- He, Z.; Zhou, J. Can zero-markup policy for drug sales in public hospitals resolve the problem of ‘seeing a doctor is too expensive’in China? A case study of four municipal general tertiary hospitals at H City in Z Province. J. Chin. Gov. 2017, 2, 329–342. [Google Scholar] [CrossRef]
- Takahashi, N.; Kobayashi, H.; Nakamura, T.; Maruo, Y.; Iwanaga, S.; Yamamoto, T.; Fujisaki, S.; Saitou, H.; Okita, T.; Fukunaga, H. Importance of clerical staff in the hospital administration: The serial change of clerical staff number in a national hospital after incorporating administrative agency shift. IRYO-Jpn. J. Natl. Med Serv. 2017, 71, 119–125. [Google Scholar]
- Mohr, J.; Spekman, R. Characteristics of partnership success: partnership attributes, communication behavior, and conflict resolution techniques. Strateg. Manag. J. 1994, 15, 135–152. [Google Scholar] [CrossRef]
- Waters, S.; Edmondston, S.J.; Yates, P.J.; Gucciardi, D.F. Identification of factors influencing patient satisfaction with orthopaedic outpatient clinic consultation: A qualitative study. Man. Ther. 2016, 25, 48–55. [Google Scholar] [CrossRef] [PubMed]
- Stewart, M.A. Effective physician-patient communication and health outcomes: A review. CMAJ Can. Med Assoc. J. 1995, 152, 1423. [Google Scholar]
- Ting, X.; Yong, B.; Yin, L.; Mi, T. Patient perception and the barriers to practicing patient-centered communication: A survey and in-depth interview of Chinese patients and physicians. Patient Educ. Couns. 2016, 99, 364–369. [Google Scholar] [CrossRef]
- Otani, K.; Waterman, B.; Faulkner, K.M.; Boslaugh, S.; Dunagan, W.C. How patient reactions to hospital care attributes affect the evaluation of overall quality of care, willingness to recommend, and willingness to return. J. Healthc. Manag. 2010, 55, 25–38. [Google Scholar] [CrossRef]
- Gu, E.; Page-Jarrett, I. The top-level design of social health insurance reforms in China: Towards universal coverage, improved benefit design, and smart payment methods. J. Chin. Gov. 2018, 3, 331–350. [Google Scholar] [CrossRef]
- Mekoth, N.; George, B.P.; Dalvi, V.; Rajanala, N.; Nizomadinov, K. Service quality in the public sector hospitals: a study in India. Hosp. Top. 2012, 90, 16–22. [Google Scholar] [CrossRef]
- Yi-ren, D.; Peng-de, T. A Statistic Analysis on the Factors of Influencing Patient Satisfaction. Appl. Stat. Manag. 2005, 1, 021. [Google Scholar]
- Spreng, R.A.; MacKenzie, S.B.; Olshavsky, R.W. A reexamination of the determinants of consumer satisfaction. J. Mark. 1996, 60, 15–32. [Google Scholar] [CrossRef]
- Jenkinson, C.; Coulter, A.; Bruster, S.; Richards, N.; Chandola, T. Patients’ experiences and satisfaction with health care: results of a questionnaire study of specific aspects of care. Qual Saf Health Care 2002, 11, 335–339. [Google Scholar] [CrossRef] [PubMed]
- McKinley, R.; Roberts, C. Patient satisfaction with out of hours primary medical care. BMJ Qual. Saf. 2001, 10, 23–28. [Google Scholar] [CrossRef] [Green Version]
- WHO. The World Health Report 2000: Health Systems: Improving Performance; World Health Organization: Geneva, Switzerland, 2000. [Google Scholar]
- Young, M.D.; Stilling, W.J.; Munger, M.A. Pharmacy practice acts: a decade of progress. Ann. Pharmacother. 1999, 33, 920–926. [Google Scholar] [CrossRef] [PubMed]
- Toklu, H.Z.; Hussain, A. The changing face of pharmacy practice and the need for a new model of pharmacy education. J. Young Pharm. 2013, 5, 38–40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dosea, A.S.; Brito, G.C.; Santos, L.M.; Marques, T.C.; Balisa-Rocha, B.; Pimentel, D.; Bueno, D.; Lyra, D.P., Jr. Establishment, implementation, and consolidation of clinical pharmacy services in community pharmacies: perceptions of a group of pharmacists. Qual. Health Res. 2017, 27, 363–373. [Google Scholar] [CrossRef] [PubMed]
- WHO. Joint FIP/WHO Guidelines on Good Pharmacy Practice: Standards for Quality of Pharmacy Services. Geneva 2011; Report: 2011; WHO: Geneva, Switzerland, 2011. [Google Scholar]
- Hepler, C.D.; Strand, L.M. Opportunities and responsibilities in pharmaceutical care. Am. J. Health-Syst. Pharm. 1990, 47, 533–543. [Google Scholar] [CrossRef]
- Ramalho de Oliveira, D.; Brummel, A.R.; Miller, D.B. Medication therapy management: 10 years of experience in a large integrated health care system. J. Manag. Care Pharm. 2010, 16, 185–195. [Google Scholar] [CrossRef]
- Hashmi, F.K.; Hassali, M.A.; Saleem, F.; Babar, Z.U.D.; Ahmad, A.; Khan, M.U. A qualitative study exploring perceptions of policymakers about community pharmacy practice and extended pharmacy services in Lahore, Pakistan. J. Pharm. Health Serv. Res. 2018, 9, 71–73. [Google Scholar] [CrossRef]
- Ibrahim, M.I.M. Assessment of Medication Dispensing and Extended Community Pharmacy Services. In Social and Administrative Aspects of Pharmacy in Low-and Middle-Income Countries; Elsevier: Amsterdam, The Netherlands, 2018; pp. 295–309. [Google Scholar]
- Aziz, M.M.; Fang, Y.; Usman, M. Hospital pharmacy services in Pakistan. Eur. J. Hosp. Pharm. 2017, 24, 253. [Google Scholar] [CrossRef]
- Khan, T. Challenges to pharmacy and pharmacy practice in Pakistan. Australas. Med J. 2011, 4, 230. [Google Scholar] [CrossRef]
- Aslam, N.; Bushra, R.; Khan, M.U. Community pharmacy practice in Pakistan. Arch. Pharm. Pract. 2012, 3, 297–303. [Google Scholar]
- Punjab, B.o.S. Bureau of Statistics: Planning & Development Department Government of the Punjab; Bureau of Statistics Punjab: Lahore, Pakistan, 2018; pp. 1–16.
- Saunders, M.N. Research Methods for Business Students, 5/e; Pearson Education: Noida, India, 2011. [Google Scholar]
- Tucker, J.L.; Adams, S.R. Incorporating patients’ assessments of satisfaction and quality: an integrative model of patients’ evaluations of their care. Manag. Serv. Qual. Int. J. 2001, 11, 272–287. [Google Scholar] [CrossRef]
- Xie, Z.; Or, C. Associations Between Waiting Times, Service Times, and Patient Satisfaction in an Endocrinology Outpatient Department: A Time Study and Questionnaire Survey. INQUIRY J. Health Care Organ. Provis. Financ. 2017, 54, 0046958017739527. [Google Scholar] [CrossRef] [PubMed]
- Andaleeb, S.S. Service quality perceptions and patient satisfaction: a study of hospitals in a developing country. Soc. Sci. Med. 2001, 52, 1359–1370. [Google Scholar] [CrossRef]
- Brislin, R.W. Research instruments. Field Methods Cross-Cult. Res. 1986, 8, 137–164. [Google Scholar]
- Gatewood, R.; Feild, H.S.; Barrick, M. Human Resource Selection; Nelson Education: Scarborough, ON, Canada, 2015. [Google Scholar]
- Nunnally, J.; Bernstein, I. Psychometric Theory 3E; Tata McGraw-Hill Education: New York, NY, USA, 2010. [Google Scholar]
- Hair, J.; Anderson, R.; Tahtam, R.; Black, W. Multivariate Data Analysis; Prentice Hall International: London, UK, 1998; p. 374. [Google Scholar]
- Joseph, F.; Hair, J.; Black, W.; Babin, B.; Anderson, R. Multivariate Data Analysis: A Global Perspective (7th (Global Edition) ed.); Prentice Hall: Upper Saddle River, NJ, USA, 2010. [Google Scholar]
- Hu, L.t.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. Multidiscip. J. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Fornell, C.; Larcker, D.F. Structural equation models with unobservable variables and measurement error: Algebra and statistics. J. Mark. Res. 1981, 18, 382–388. [Google Scholar] [CrossRef]
- Shaffer, J.A.; DeGeest, D.; Li, A. Tackling the problem of construct proliferation: A guide to assessing the discriminant validity of conceptually related constructs. Organ. Res. Methods 2016, 19, 80–110. [Google Scholar] [CrossRef]
- Marsh, H.W.; Hau, K.-T.; Wen, Z. In search of golden rules: Comment on hypothesis-testing approaches to setting cutoff values for fit indexes and dangers in overgeneralizing Hu and Bentler’s (1999) findings. Struct. Equ. Model. 2004, 11, 320–341. [Google Scholar] [CrossRef]
- Hooper, D.; Coughlan, J.; Mullen, M. Structural equation modelling: Guidelines for determining model fit. Articles 2008, 2. [Google Scholar] [CrossRef]
- McNeish, D.; An, J.; Hancock, G.R. The thorny relation between measurement quality and fit index cutoffs in latent variable models. J. Personal. Assess. 2018, 100, 43–52. [Google Scholar] [CrossRef] [PubMed]
- Sharma, R.; Sharma, M.; Sharma, R. The patient satisfaction study in a multispecialty tertiary level hospital, PGIMER, Chandigarh, India. Leadersh. Health Serv. 2011, 24, 64–73. [Google Scholar] [CrossRef]
- Hussain, A.; Malik, M.; Toklu, H.Z. A literature review: pharmaceutical care an evolving role at community pharmacies in Pakistan. Pharmacol. Pharm. 2013, 4, 425–430. [Google Scholar] [CrossRef]
- George, M. The role of basic laboratory services in strengthening primary health centres. Indian J. Med. Ethics 2011, 8, 161–163. [Google Scholar] [CrossRef]
- Mindaye, T.; Taye, B. Patients satisfaction with laboratory services at antiretroviral therapy clinics in public hospitals, Addis Ababa, Ethiopia. BMC Res. Notes 2012, 5, 184. [Google Scholar] [CrossRef] [PubMed]
- Abera, R.G.; Abota, B.A.; Legese, M.H.; Negesso, A.E. Patient satisfaction with clinical laboratory services at Tikur Anbessa specialized hospital, Addis Ababa, ethiopia. Patient Prefer. Adherence 2017, 11, 1181–1188. [Google Scholar] [CrossRef]
- Rao, K.D.; Peters, D.H.; Bandeen-Roche, K. Towards patient-centered health services in India—A scale to measure patient perceptions of quality. Int. J. Qual. Health Care 2006, 18, 414–421. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.-K.; Cho, C.-H.; Ahn, S.-K.; Goh, I.-H.; Kim, H.-J. A study on medical services quality and its influence upon value of care and patient satisfaction–Focusing upon outpatients in a large-sized hospital. Total Qual. Manag. 2008, 19, 1155–1171. [Google Scholar] [CrossRef]
- Zarei, E.; Daneshkohan, A.; Pouragha, B.; Marzban, S.; Arab, M. An Empirical study of the Impact of Service Quality on patient Satisfaction in private Hospitals, Iran. Glob. J. Health Sci. 2015, 7, 1–9. [Google Scholar] [CrossRef] [PubMed]
| Population | Area km2 | |
|---|---|---|
| Punjab Province | 110,012,442 | 205,344 |
| Bahawalpur District | 3,668,106 | 24,830 |
| Bahawalnagar District | 2,981,919 | 8878 |
| Rahim Yar Khan District | 4,814,006 | 11,880 |
| Sr. No. | Teaching Hospital | District Hospital (DHQ) | Tehsil Headquarter (THQs) | Rural Health Center (RHCs) | Basic Health Unit (BHUs) |
|---|---|---|---|---|---|
| 1 | 1 | 0 | 4 | 10 | 72 |
| 2 | 0 | 1 | 4 | 10 | 101 |
| 3 | 1 | 0 | 3 | 19 | 104 |
| 2 | 1 | 11 | 29 | 277 |
| Characteristics | Frequency | % |
|---|---|---|
| Gender | ||
| Male | 199 | 44.7 |
| Female | 246 | 55.3 |
| Age | ||
| Less than 20 | 36 | 8.1 |
| 20 to 29 | 53 | 11.9 |
| 30 to 39 | 93 | 20.9 |
| 40 to 49 | 137 | 30.8 |
| 50 and above | 126 | 28.3 |
| Marital status | ||
| Married | 243 | 54.6 |
| Single | 188 | 42.3 |
| Divorced | 12 | 2.7 |
| Widow | 2 | 0.4 |
| Occupation | ||
| Student | 7 | 1.6 |
| Government employee | 45 | 10.2 |
| House wife | 117 | 26.2 |
| Laborer | 108 | 24.2 |
| Agriculture | 43 | 9.7 |
| Un-employed | 71 | 16.0 |
| Retired | 33 | 7.5 |
| Other | 21 | 4.6 |
| Education | ||
| No formal education | 135 | 30.3 |
| Primary/elementary school | 145 | 32.6 |
| Secondary/high school | 106 | 23.8 |
| College/university | 24 | 5.3 |
| Postgraduate | 35 | 8.0 |
| Monthly income | ||
| Less than PKR 10,000 | 123 | 27.6 |
| PKR 10,000 to 14,999 | 103 | 23.2 |
| PKR 15,000 to 19,999 | 74 | 16.6 |
| PKR 20,000 to 24,999 | 61 | 13.8 |
| PKR 25,000 to 29,999 | 47 | 10.5 |
| PKR 30,000 or more | 37 | 8.3 |
| Variable | Mean | SD | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|---|---|
| Patient satisfaction | 3.99 | 0.61 | (0.96) | ||||
| Laboratory services | 3.52 | 0.77 | 440 ** | (0.92) | |||
| Pharmacy services | 4.15 | 0.66 | 0.445 ** | 0.339 ** | (0.93) | ||
| Doctor–patient communication | 2.25 | 0.80 | 0.205 ** | 0.189 ** | 0.230 ** | (0.94) | |
| Physical services | 3.02 | 0.89 | 0.269 ** | 0.402 ** | 0.192 ** | 0.253 ** | (0.96) |
| CR | AVE | MSV | MAX (H) | PS | PHS | LS | PF | DPC | |
|---|---|---|---|---|---|---|---|---|---|
| PS | 0.965 | 0.753 | 0.230 | 0.976 | 0.868 | ||||
| PHS | 0.934 | 0.639 | 0.230 | 0.939 | 0.479 *** | 0.799 | |||
| LS | 0.928 | 0.685 | 0.202 | 0.935 | 0.450 *** | 0.369 *** | 0.827 | ||
| PF | 0.964 | 0.844 | 0.148 | 0.984 | 0.267 *** | 0.199 *** | 0.385 *** | 0.919 | |
| DPC | 0.942 | 0.804 | 0.063 | 0.974 | 0.220 *** | 0.222 *** | 0.192 *** | 0.251 *** | 0.897 |
| Absolute Model Fit Indices | |
|---|---|
| Chi Square | 780.547 |
| DF | 415 |
| Chi Square/DF | 1.881 |
| Standardized Root Mean Residual (SRMR) | 0.042 |
| Comparative Fit Index (CFI) | 0.980 |
| Normed Fit Index (NFI) | 0.959 |
| Tucker Lewis Index (TLI) | 0.976 |
| Relative Fit Index (RFI) | 0.951 |
| Incremental Fit Index (IFI) | 0.980 |
| Root Mean Square Error of Approximation (RMSEA) | 0.045 |
| Construct/Factors | Items | Factor Loadings | Cronbach Alpha |
|---|---|---|---|
| Patient satisfaction | 0.966 | ||
| Ps1 | 0.798 | ||
| Ps2 | 0.817 | ||
| Ps3 | 0.877 | ||
| Ps4 | 0.893 | ||
| Ps5 | 0.863 | ||
| Ps6 | 0.723 | ||
| Ps7 | 0.879 | ||
| Ps8 | 0.876 | ||
| Ps9 | 0.859 | ||
| Pharmacy services | 0.931 | ||
| Ph1 | 0.780 | ||
| Ph2 | 0.826 | ||
| Ph3 | 0.796 | ||
| Ph4 | 0.764 | ||
| Ph5 | 0.797 | ||
| Ph6 | 0.827 | ||
| Ph7 | 0.795 | ||
| Ph8 | 0.752 | ||
| Doctor–patient communication | 0.942 | ||
| Dpc1 | 0.937 | ||
| Dpc2 | 0.877 | ||
| Dpc3 | 0.883 | ||
| Dpc4 | 0.926 | ||
| Laboratory services | 0.927 | ||
| Ls1 | 0.748 | ||
| Ls2 | 0.851 | ||
| Ls3 | 0.827 | ||
| Ls4 | 0.845 | ||
| Ls5 | 0.800 | ||
| Ls6 | 0.770 | ||
| Physical services | 0.968 | ||
| PF1 | 0.930 | ||
| PF2 | 0.933 | ||
| PF3 | 0.883 | ||
| PF4 | 0.875 | ||
| PF5 | 0.923 |
| β Coefficients | 95.0% Confidence Interval for β | Collinearity Statistics | |||||
|---|---|---|---|---|---|---|---|
| Β | T | Sig. | Lower Bound | Upper Bound | Tolerance | VIF | |
| Constant | 9.591 | 0.000 | 1.316 | 1.994 | |||
| 1. Pharmacy services | 0.287 | 6.328 | 0.000 | 0.158 | 0.300 | 0.766 | 1.306 |
| 2. Laboratory services | 0.331 | 7.713 | 0.000 | 0.230 | 0.387 | 0.855 | 1.169 |
| 3. Doctor–patient communication | 0.055 | 1.316 | 0.189 | −0.021 | 0.105 | 0.900 | 1.111 |
| 4. Physical services | 0.076 | 1.727 | 0.085 | 0-.007 | 0.113 | 0.806 | 1.241 |
| Model summary R = 0.555, R2 = 0.308, F = 49.06, p = 0.000, Durbin-Watson (DW) = 2.01 | |||||||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hussain, A.; Sial, M.S.; Usman, S.M.; Hwang, J.; Jiang, Y.; Shafiq, A. What Factors Affect Patient Satisfaction in Public Sector Hospitals: Evidence from an Emerging Economy. Int. J. Environ. Res. Public Health 2019, 16, 994. https://doi.org/10.3390/ijerph16060994
Hussain A, Sial MS, Usman SM, Hwang J, Jiang Y, Shafiq A. What Factors Affect Patient Satisfaction in Public Sector Hospitals: Evidence from an Emerging Economy. International Journal of Environmental Research and Public Health. 2019; 16(6):994. https://doi.org/10.3390/ijerph16060994
Chicago/Turabian StyleHussain, Abid, Muhammad Safdar Sial, Sardar Muhammad Usman, Jinsoo Hwang, Yushi Jiang, and Awaisra Shafiq. 2019. "What Factors Affect Patient Satisfaction in Public Sector Hospitals: Evidence from an Emerging Economy" International Journal of Environmental Research and Public Health 16, no. 6: 994. https://doi.org/10.3390/ijerph16060994
APA StyleHussain, A., Sial, M. S., Usman, S. M., Hwang, J., Jiang, Y., & Shafiq, A. (2019). What Factors Affect Patient Satisfaction in Public Sector Hospitals: Evidence from an Emerging Economy. International Journal of Environmental Research and Public Health, 16(6), 994. https://doi.org/10.3390/ijerph16060994






