Health Literacy: Current Status and Challenges in the Work of Family Doctors in Bosnia and Herzegovina
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Selection and Description of Participants
2.3. Data Collection
2.4. Instrument
2.5. Description of Instrument
2.6. Statistical Analysis
3. Results
3.1. Sociodemographic Characteristics of Respondents
3.2. Health Characteristics of Respondents
3.3. Health Literacy of Respondents
3.4. Determinants of Inadequate and Marginal Health Literacy
4. Discussion
4.1. Summary of Results
4.2. Comparision with International Population-Based Studies
4.3. Comparison with the Current Literature
4.4. The Significance for Clinical Practice
4.5. The Significance for Future Analysis
4.6. Study Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Ethics Approval and Consent to Participate
References
- WHO. Health Promotion. Available online: http://www.who.int/healthpromotion/conferences/9gchp/resources/en/ (accessed on 19 January 2019).
- Sorensen, K.; van den Broucke, S.; Fullam, J.; Doyle, G.; Pelikan, J.; Slonska, Z.; Brand, H. Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health 2012, 12, 80. Available online: https://bmcpublichealth.biomedcentral.com/articles/10.1186/1471-2458-12-80 (accessed on 18 November 2018). [CrossRef] [PubMed]
- Quaglio, G.; Sorensen, S.; Rübig, P.; Bertinato, L.; Brand, H.; Karapiperis, T.; Dinca, I.; Peetso, T.; Kadenbach, K.; Dario, C. Accelerating the health literacy agenda in Europe. Health Promot. Int. 2016, 32, 1074–1080. Available online: https://www.researchgate.net/publication/301563082_Accelerating_the_health_literacy_agenda_in_Europe/download (accessed on 11 November 2018). [CrossRef] [PubMed]
- U.S. Department of Health and Human Services. Office of Disease Prevention and Health Promotion. National Action Plan to Improve Health Literacy. Washington. 2010. Available online: https://health.gov/communication/HLActionPlan/pdf/Health_Lit_Action_Plan_Summary.pdf (accessed on 19 February 2019).
- Eagle, L.; Hawkins, J.; Styles, E.; Reid, J. Breaking through the invisible barrier of low functional literacy: Implications for health communication. Stud. Commun. Sci. Spec. Issue Health Lit. 2006, 5, 29–55. Available online: http://eprints.uwe.ac.uk/13981 (accessed on 20 February 2019).
- Osborne, H. Health Literacy from A to Z: Practical Ways to Communicate your Health Message, 2nd ed.; Jones and Bartlett Learning: Burlington, MA, USA, 2013; Available online: http://samples.jbpub.com/9781449600532/00532_FMxx_PASS03.pdf (accessed on 25 January 2019).
- Peterson, P.N.; Shetterly, S.M.; Clarke, C.L.; Bekelman, D.B.; Chan, P.S.; Allen, L.A. Health Literacy and Outcomes Among Patients with Heart Failure. JAMA 2011, 305, 1695–1701. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4540335/ (accessed on 25 January 2019). [CrossRef] [PubMed]
- Petricek, G.; Vrcic-Keglevic, M.; Vuletic, G.; Cerovecki, V.; Ozvacic, Z.; Murgic, L. Illness perception and cardiovascular risk factors in patients with type 2 diabetes: Cross-sectional questionnaire study. Croat. Med. J. 2009, 50, 583–593. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2802092/ (accessed on 10 February 2019). [CrossRef] [PubMed]
- Parikh, N.S.; Parker, R.M.; Nurss, J.R.; Baker, D.W.; Williams, M.V. Shame and health literacy: The unspoken connection. Patient Educ. Couns. 1996, 27, 33–39. Available online: https://doi.org/10.1016/0738-3991(95)00787-3 (accessed on 1 December 2018). [CrossRef]
- Parker, R.M.; Baker, D.W.; Wiliams, M.V.; Nurss, J.R. The test of functional health literacy in adults: A new instrument for measuring patient’s literacy skills. J. Gen. Intern. Med. 1995, 10, 537–541. Available online: https://doi.org/10.1007/BF02640361 (accessed on 10 October 2018). [CrossRef]
- Health Literacy Tool Shed. A Database of Health Literacy Measures. Available online: http://healthliteracy.bu.edu/all (accessed on 10 December 2018).
- Jovic-Vranes, A.; Bjegovic-Mikanovic, V.; Marinkovic, J.; Kocev, N. Health literacy in a population primary health-care patients in Belgrade, Serbia. Int. J. Public Health 2011, 56, 201–207. Available online: https://link.springer.com/article/10.1007%2Fs00038-010-0181-0 (accessed on 10 October 2018). [CrossRef]
- Todorovic, N.; Jovic-Vranes, A.; Djikanovic, B.; Pilipovic-Broceta, N.; Vasiljevic, N.; Lucic-Samardzija, V.; Peric, A. Assessment of health literacy in the adult population registered to family medicine physicians in the Republic of Srpska, Bosnia and Herzegovina. Eur. J. Gen. Pract. 2019, 25, 32–38. Available online: https://www.tandfonline.com/doi/full/10.1080/13814788.2019.1571579 (accessed on 22 February 2019). [CrossRef]
- Sorensen, K.; Pelikan, J.M.; Röthlin, F.; Ganahl, K.; Slonska, Z.; Doyle, G.; Fullam, J.; Kondilis, B.; Agrafiotis, D.; Uiters, E.; et al. Health literacy in Europe: Comparative results of the European health literacy survey (HLS-EU). Eur. J. Public Health 2015, 25, 1053–1058. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4668324/ (accessed on 1 December 2018). [CrossRef]
- Eronen, J.; Paakkari, L.; Portegijs, E.; Saajanaho, M.; Rantane, T. Assessment of health literacy among older Finns. Aging Clin. Exp. Res. 2018, 31, 549–556. Available online: https://link.springer.com/article/10.1007/s40520-018-1104-9 (accessed on 20 March 2019). [CrossRef]
- Papp-Zipernovszky, O.; Náfrádi, L.; Schulz, P.J.; Csabai, M. “So that each patient may comprehend”: Measuring health literacy in Hungary. Orv. Hetil. 2016, 157, 905–915. Available online: https://www.ncbi.nlm.nih.gov/pubmed/27233834 (accessed on 20 March 2019). [CrossRef] [PubMed]
- Jovic-Vranes, A.; Bjegovic-Mikanovic, V.; Marinkovic, J. Functional health literacy among primary health-care patients: Data from the Belgrade pilot study. J. Public Health 2009, 31, 490–495. Available online: https://www.ncbi.nlm.nih.gov/pubmed/19454605 (accessed on 20 March 2019). [CrossRef]
- Marmot, M.; Wilkinson, R. Social Determinants of Health, 2nd ed.; WHO Library: Copenhagen, Denmark, 2003; Available online: http://www.euro.who.int/__data/assets/pdf_file/0005/98438/e81384.pdf (accessed on 1 December 2018).
- The European Health Literacy Project 2009-2012 (HLS-EU), Final Report. Available online: www.health-literacy.eu (accessed on 5 October 2018).
- Eichler, K.; Wieser, S.; Brügger, U. The costs of limited health literacy: A systematic review. Int. J. Public Health 2009, 54, 313–324. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3785182/ (accessed on 5 December 2018). [CrossRef]
- Zotti, P.; Cocchi, S.; Polesel, J.; Cipolat, M.C.; Bragatto, D.; Cavuto, S.; Conficconi, A.; Costanzo, C.; De Giorgi, M.; Christina, A.; et al. Cross-cultural validation of health literacy measurement tools in Italian oncology patients. BMC Health Serv. Res. 2017, 17, 410. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5477151/ (accessed on 5 October 2018). [CrossRef]
- Kobayashi, L.C.; Wardle, J.; Wolf, M.S.; von Wagner, C. Cognitive Function and Health Literacy Decline in a Cohort of Aging English Adults. J. Gen. Intern Med. 2015, 30, 958–964. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4471026/ (accessed on 25 October 2018). [CrossRef] [Green Version]
- Rowlands, G.P.; Mehay, A.; Hampshire, S.; Phillips, R.; Williams, P.; Mann, A.; Steptoe, A.; Walters, P.; Tylee, A.T. Characteristics of people with low health literacy on coronary heart disease GP registers in South London: A cross-sectional study. BMJ Open 2013, 3, e001503. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3549254/ (accessed on 25 November 2018). [CrossRef]
- Kobayashi, L.C.; Smith, S.G.; O’Conor, R.; Curtis, L.M.; Park, D.; von Wagner, C.; Deary, I.J.; Wolf, M.S. The role of cognitive function in the relationship between age and health literacy: A cross-sectional analysis of older adults in Chicago, USA. BMJ Open 2015, 5, e007222. Available online: https://www.researchgate.net/publication/275356363 (accessed on 23 December 2018). [CrossRef] [PubMed]
- Connor, M.; Mantwill, S.; Schultz, P.J. Functional health literacy in Switzerland–validation of a German, Italian, and French health literacy test. Patient Educ. Couns. 2013, 90, 12–17. Available online: https://www.ncbi.nlm.nih.gov/pubmed/23089240 (accessed on 25 October 2018). [CrossRef] [PubMed]
- Geboers, B.; Brainard, J.S.; Loke, Y.K.; Jansen, C.J.M.; Salter, C.; Reijneveld, S.A.; de Winter, A.F. Erratum to: The association of health literacy with adherence in older adults, and its role in interventions: A systematic meta-review. BMC Public Health 2015, 15, 1091. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4573285/ (accessed on 25 October 2018). [CrossRef]
- Furuya, Y.; Kondo, N.; Yamagata, Z.; Hashimoto, H. Health literacy, socioeconomic status and self-rated health in Japan. Health Promot. Int. 2015, 30, 505–513. Available online: https://academic.oup.com/heapro/article/30/3/505/621284 (accessed on 25 November 2018). [CrossRef]
- Kobayashi, L.C.; Wardle, J.; Wolf, M.S.; von Wagner, C. Aging and Functional Health Literacy: A Systematic Review and Meta-Analysis. J. Gerontol. B Psychol. Sci. Soc. Sci. 2016, 71, 445–457. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4834761/ (accessed on 25 October 2018). [CrossRef]
- Jessup, R.L.; Osborne, R.H.; Beauchamp, A.; Bourne, A.; Buchbinder, R. Health literacy of recently hospitalised patients: A cross-sectional survey using the Health Literacy Questionnaire (HLQ). BMC Health Serv. Res. 2017, 17, 52. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5244731/ (accessed on 25 November 2018). [CrossRef]
- Jessup, R.L.; Osborne, R.H.; Beauchamp, A.; Bourne, A.; Buchbinder, R. Differences in health literacy profiles of patients admitted to a public and a private hospital in Melbourne, Australia. BMC Health Serv. Res. 2018, 18, 134. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5824469/ (accessed on 25 October 2018). [CrossRef]
- Nakayama, K.; Osaka, W.; Togari, T.; Ishikawa, H.; Yonekura, Y.; Sekido, A.; Matsumoto, M. Comprehensive health literacy in Japan is lower than in Europe: A validated Japanese-language assessment of health literacy. BMC Public Health 2015, 15, 505. Available online: https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-015-1835-x (accessed on 25 November 2018). [CrossRef]
- N’Goran, A.A.; Pasquier, J.; Deruaz-Luyet, A.; Burnand, B.; Haller, D.; Neuner-Jehle, S.; Streit, S.; Herzig, L.; Bodenmann, P. Factors associated with health literacy in multimorbid patients in primary care: A cross-sectional study in Switzerland. BMJ Open 2018, 8, e018281. Available online: https://bmjopen.bmj.com/content/8/2/e018281 (accessed on 25 November 2018). [CrossRef]
- Martin, L.T.; Ruder, T.; Escarce, J.J.; Ghosh-Dastidar, B.; Sherman, D.; Elliott, M.; Bird, C.E.; Fremont, A.; Gasper, C.; Culbert, A.; et al. Developing Predictive Models of Health Literacy. J. Gen. Intern. Med. 2009, 24, 1211–1216. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2771237/ (accessed on 10 February 2019). [CrossRef] [Green Version]
- Parker, R.M.; Davis, T.C.; Williams, M.V.; Bateman, W.B.; Kramer, E.J.; Glassman, K.S. Patients with limited health literacy. In Patient and Family Education in Managed in Managed Care and Beyond: Seizing the Teachable Moment; Springer: New York, NY, USA, 1999; pp. 63–71. Available online: https://archive.org/stream/understandinghe00nati/understandinghe00nati_djvu.txt (accessed on 25 October 2018).
- Duong, V.T.; Lin, I.F.; Sorensen, K.; Pelikan, J.M.; van den Broucke, S.; Lin, Y.C.; Chang, P.W. Health literacy in Taiwan: A population-based study. Asia Pac. J. Public Health 2015, 27, 871–880. Available online: https://www.ncbi.nlm.nih.gov/pubmed/26419635 (accessed on 10 February 2019). [CrossRef]
- Duong, T.V.; Aringazina, A.; Baisunova, G.; Nurjanah; Pham, T.V.; Pham, K.M.; Truong, T.Q.; Nguyen, K.T.; Oo, W.M.; Mohamad, E.; et al. Measuring health literacy in Asia: Validation of the HLS-EU-Q47 survey tool in six Asian countries. J. Epidemiol. 2017, 27, 80–86. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5328731/ (accessed on 25 October 2018). [CrossRef]
- Vandenbosch, J.; van den Broucke, S.; Vancorenland, S.; Avalosse, H.; Verniest, R.; Callens, M. Health literacy and the use of healthcare services in Belgium. J. Epidemiol. Community Health 2016, 70, 1032–1038. Available online: https://www.ncbi.nlm.nih.gov/pubmed/27116951 (accessed on 10 November 2018). [CrossRef] [Green Version]
- Shih, S.F.; Liu, C.H.; Liao, L.L.; Osborne, R. Health literacy and the determinants of obesity: A population-based survey of sixth grade school children in Taiwan. BMC Public Health 2016, 16, 280. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4802836/ (accessed on 1 October 2018). [CrossRef]
- Al Sayah, F.; Johnson, S.T.; Vallance, J. Health Literacy, Pedometer, and Self-Reported Walking Among Older Adults. Am. J. Public Health 2016, 106, 327–333. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4815562/ (accessed on 31 October 2018). [CrossRef]
- MacLeod, S.; Musich, S.; Gulyas, S.; Cheng, Y.; Tkatch, R.; Cempellin, D.; Bhattarai, G.R.; Hawkins, K.; Yeh, C.S. The impact of inadequate health literacy on patient satisfaction, healthcare utilization, and expenditures among older adults. Geriatr. Nurs. 2017, 38, 334–341. Available online: https://www.ncbi.nlm.nih.gov/pubmed/28089217 (accessed on 10 November 2018). [CrossRef]
| N | % | |
|---|---|---|
| Gender | ||
| Male | 326 | (42.5) |
| Female | 442 | (57.5) |
| Age, years | ||
| Below 44 | 298 | (38.8) |
| 45–54 | 132 | (17.2) |
| 55–64 | 151 | (19.7) |
| 65 and above | 186 | (24.3) |
| Marital status | ||
| Married | 437 | (57.3) |
| Other | 325 | (42.7) |
| Low: Primary school or less (≤8) | 151 | (19.8) |
| Moderate: Secondary school (8–12) | 462 | (60.5) |
| High: High and higher school (>12) | 150 | (19.7) |
| Area | ||
| Urban | 264 | (34.4) |
| Rural | 503 | (65.6) |
| Employment | ||
| Employed | 294 | (38.3) |
| Other | 474 | (61.7) |
| Income (per person) | ||
| Poor (<700 BAM *) | 134 | (17.5) |
| Average (700–900 BAM) | 410 | (53.5) |
| Good (>900 BAM) | 223 | (29.1) |
| Insufficient physical activity risk | ||
| No | 323 | (42.1) |
| Yes | 444 | (57.9) |
| Chronic diseases | ||
| Without | 410 | (53.5) |
| One | 156 | (20.4) |
| Two | 74 | (9.7) |
| Three | 49 | (6.4) |
| More than three | 77 | (10.1) |
| Self-perception of health | ||
| Poor | 86 | (11.3) |
| Average | 294 | (38.6) |
| Good | 382 | (50.1) |
| Life satisfaction | ||
| Low | 165 | (21.5) |
| Average | 390 | (50.9) |
| High | 211 | (27.5) |
| Municipality | ||
| Bijeljina | 384 | (50.0) |
| Prijedor | 384 | (50.0) |
| Total | 768 |
| S-TOFHLA Score Categories | |||||||
|---|---|---|---|---|---|---|---|
| Characteristics | Inadequate | Marginal | Adequate | p Value a | |||
| (n = 189) | % | (n = 77) | % | (n = 502) | % | ||
| Area | <0.001 | ||||||
| Urban | 36 | (19.0) | 25 | (32.5) | 203 | (40.5) | |
| Rural | 153 | (81.0) | 52 | (67.5) | 298 | (59.5) | |
| Gender | 0.244 | ||||||
| Male | 88 | (46.6) | 36 | (46.8) | 202 | (40.3) | |
| Female | 101 | (53.4) | 41 | (53.2) | 299 | (59.7) | |
| Age, years | <0.001 | ||||||
| Below 44 | 39 | (20.7) | 25 | (32.5) | 234 | (46.6) | |
| 45–54 | 18 | (9.6) | 11 | (14.3) | 103 | (20.5) | |
| 55–64 | 44 | (23.4) | 20 | (26.0) | 87 | (17.3) | |
| 65 and above | 87 | (46.3) | 21 | (27.3) | 78 | (15.5) | |
| Marital status | 0.001 | ||||||
| Married | 86 | (46.0) | 49 | (64.5) | 302 | (60.5) | |
| Other | 101 | (54.0) | 27 | (35.5) | 197 | (39.5) | |
| Employment | 0.002 | ||||||
| Employed | 53 | (28.0) | 27 | (35.1) | 214 | (42.6) | |
| Other | 136 | (72.0) | 50 | (64.9) | 288 | (57.4) | |
| Education (years of school completed) | <0.001 | ||||||
| Low: Primary school or less (≤8) | 62 | (32.8) | 20 | (26.0) | 69 | (13.9) | |
| Moderate: Secondary school (8–12) | 111 | (58.7) | 46 | (59.7) | 305 | (61.4) | |
| High: High and higher school (>12) | 16 | (8.5) | 11 | (14.3) | 123 | (24.7) | |
| Income (per person) | <0.001 | ||||||
| Poor (<700 BAM) | 56 | (29.6) | 20 | (26.0) | 58 | (11.6) | |
| Average (700–900 BAM) | 96 | (50.8) | 38 | (49.4) | 276 | (55.1) | |
| Good (>900 BAM) | 37 | (19.6) | 19 | (24.7) | 167 | (33.3) | |
| Self-perception of health | <0.001 | ||||||
| Poor | 66 | (35.3) | 26 | (34.7) | 32 | (6.4) | |
| Average | 75 | (40.1) | 41 | (54.7) | 178 | (35.6) | |
| Good | 46 | (24.6) | 8 | (10.7) | 290 | (58.0) | |
| Chronic diseases | <0.001 | ||||||
| Without | 86 | (45.5) | 37 | (48.1) | 287 | (57.4) | |
| One | 40 | (21.2) | 17 | (22.1) | 99 | (19.8) | |
| Two | 16 | (8.5) | 6 | (7.8) | 52 | (10.4) | |
| Three | 10 | (5.3) | 6 | (7.8) | 33 | (6.6) | |
| More than three | 37 | (19.6) | 11 | (14.3) | 29 | (5.8) | |
| Insufficient physical activity risk | <0.001 | ||||||
| No | 39 | (20.6) | 27 | (35.1) | 257 | (51.3) | |
| Yes | 150 | (79.4) | 50 | (64.9) | 244 | (48.7) | |
| Family doctor visits | 0.017 | ||||||
| No visits | 37 | (20.4) | 19 | (10.5) | 125 | (69.1) | |
| 1–2 visits | 63 | (27.5) | 27 | (11.8) | 139 | (60.7) | |
| 3–4 visits | 41 | (30.8) | 8 | (6.0) | 84 | (63.2) | |
| 5–10 visits | 23 | (22.3) | 4 | (3.9) | 76 | (73.8) | |
| More than 10 | 24 | (20.0) | 19 | (15.8) | 77 | (64,2) | |
| Number of hospitalisations | 0.007 | ||||||
| No hospitalisations | 145 | (77.1) | 67 | (87.0) | 438 | (87.8) | |
| 1–2 times | 37 | (19.7) | 7 | (9.1) | 50 | (10.0) | |
| More than 2 | 6 | (3.2) | 3 | (3.9) | 11 | (2.2) | |
| Change of health | <0.001 | ||||||
| Better | 30 | (16.3) | 18 | (24.0) | 147 | (29.6) | |
| Same | 96 | (52.2) | 45 | (60.0) | 279 | (56.1) | |
| Worse | 58 | (31.5) | 12 | (16.0) | 71 | (14.3) | |
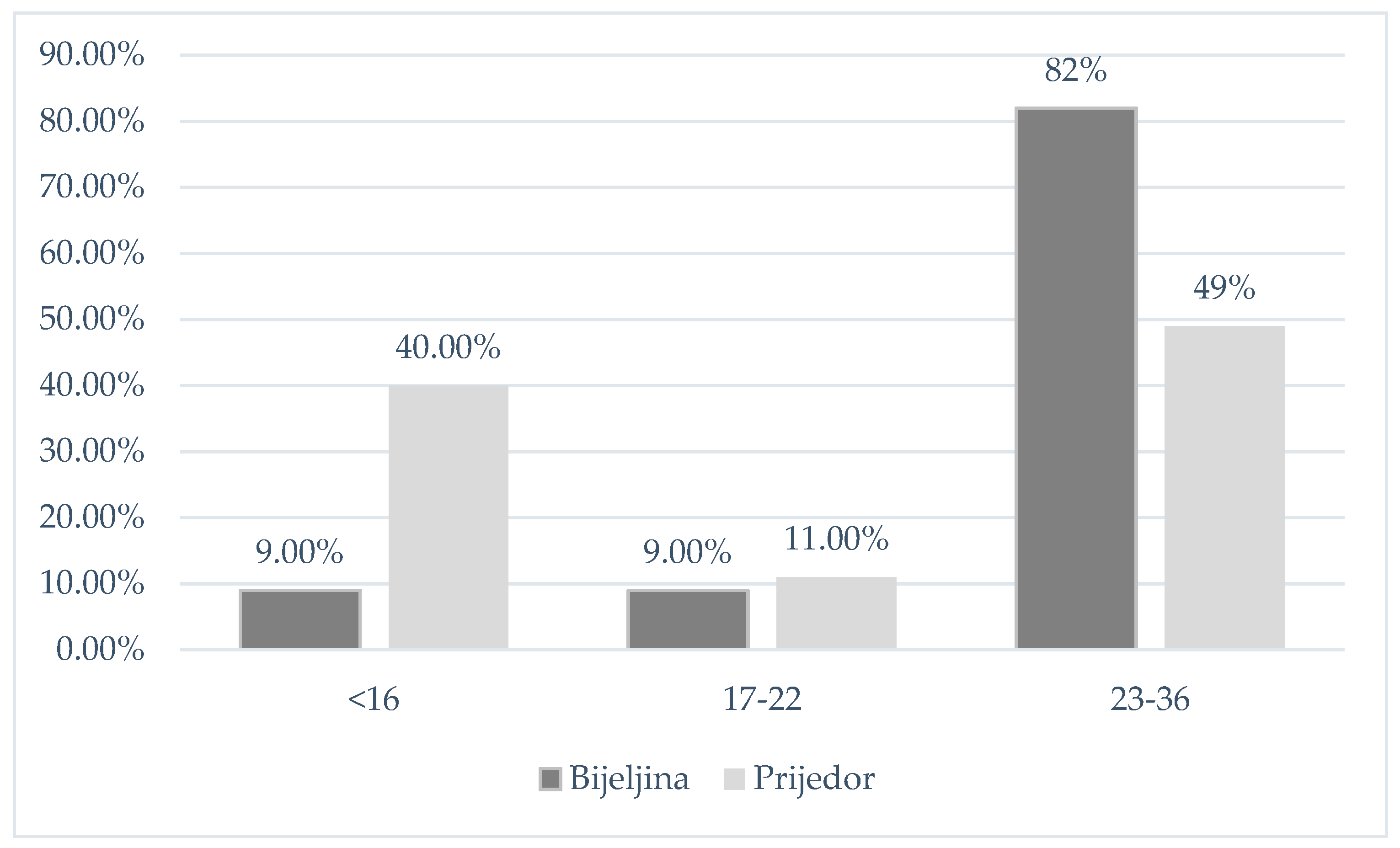
| Municipality | <0.001 | ||||||
| Bijeljina | 34 | (8.8) | 36 | (9.4) | 314 | (81.8) | |
| Prijedor | 155 | (40.4) | 41 | (10.7) | 188 | (48.9) | |
| Variable | Univariate | Multivariate | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | |||||
| Age, years | 1.04 | 1.03 | ‒ | 1.05 | 0.000 | 1.02 | 1.00 | ‒ | 1.05 | 0.03 |
| Marital status, divorced | 4.2 | 2.43 | ‒ | 7.28 | 0.000 | 3.32 | 1.26 | ‒ | 8.72 | 0.02 |
| Place of residence, rural | 2.29 | 1.63 | ‒ | 3.21 | 0.000 | 2.25 | 1.31 | ‒ | 3.87 | 0.00 |
| Income, low | 3.06 | 2.09 | ‒ | 4.47 | 0.000 | 1.96 | 1.09 | ‒ | 3.53 | 0.03 |
| Number of chronic diseases, more than three | 3.58 | 2.19 | ‒ | 5.83 | 0.000 | 1.94 | 1.02 | ‒ | 3.67 | 0.04 |
| Taking medicines | 0.53 | 0.32 | ‒ | 0.88 | 0.015 | |||||
| Self-perception of health | 1.96 | 1.64 | ‒ | 2.35 | 0.000 | 1.59 | 1.12 | ‒ | 2.26 | 0.01 |
| Physical activity, insufficient | 1.41 | 1.3 | ‒ | 1.52 | 0.000 | 1.29 | 1.16 | ‒ | 1.45 | 0.00 |
| Tertiary education | 0.34 | 0.22 | ‒ | 0.54 | 0.000 | |||||
| Employment status, retired | 3.16 | 2.19 | ‒ | 4.55 | 0.000 | |||||
| Frequency of hospitalization | 1.54 | 1.12 | ‒ | 2.13 | 0.009 | |||||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Todorovic, N.; Jovic-Vranes, A.; Djikanovic, B.; Pilipovic-Broceta, N.; Vasiljevic, N.; Racic, M. Health Literacy: Current Status and Challenges in the Work of Family Doctors in Bosnia and Herzegovina. Int. J. Environ. Res. Public Health 2019, 16, 1324. https://doi.org/10.3390/ijerph16081324
Todorovic N, Jovic-Vranes A, Djikanovic B, Pilipovic-Broceta N, Vasiljevic N, Racic M. Health Literacy: Current Status and Challenges in the Work of Family Doctors in Bosnia and Herzegovina. International Journal of Environmental Research and Public Health. 2019; 16(8):1324. https://doi.org/10.3390/ijerph16081324
Chicago/Turabian StyleTodorovic, Nevena, Aleksandra Jovic-Vranes, Bosiljka Djikanovic, Natasa Pilipovic-Broceta, Nadja Vasiljevic, and Maja Racic. 2019. "Health Literacy: Current Status and Challenges in the Work of Family Doctors in Bosnia and Herzegovina" International Journal of Environmental Research and Public Health 16, no. 8: 1324. https://doi.org/10.3390/ijerph16081324





