Risk of Cardiovascular Disease Due to General Anesthesia and Neuraxial Anesthesia in Lower-Limb Fracture Patients: A Retrospective Population-Based Cohort Study
Abstract
1. Introduction
2. Experimental Section
2.1. Data Sources
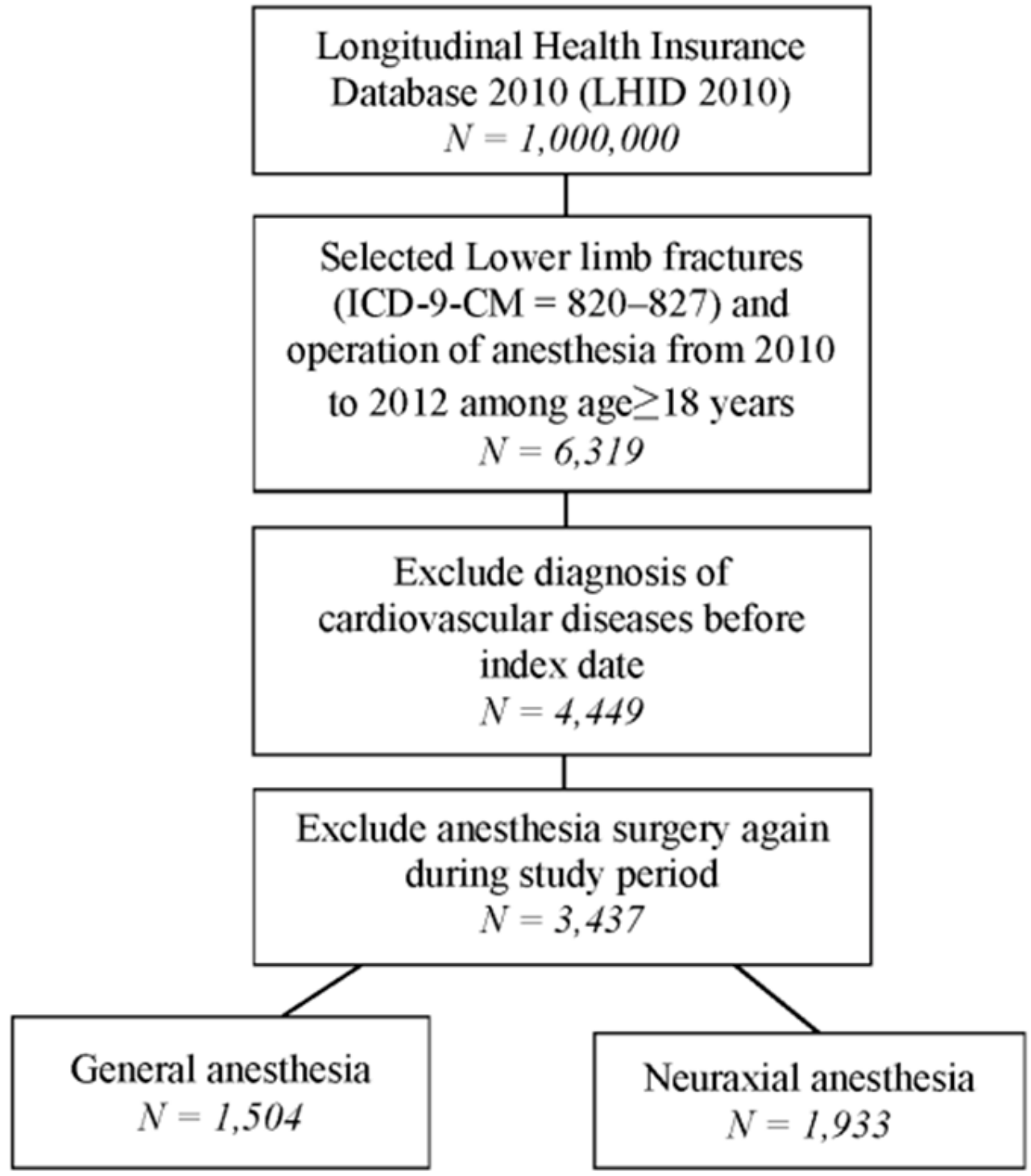
2.2. Study Groups
2.3. Outcome and Covariate Measurement
2.4. Statistical Analysis
3. Results
3.1. Characteristics of Study Subjects
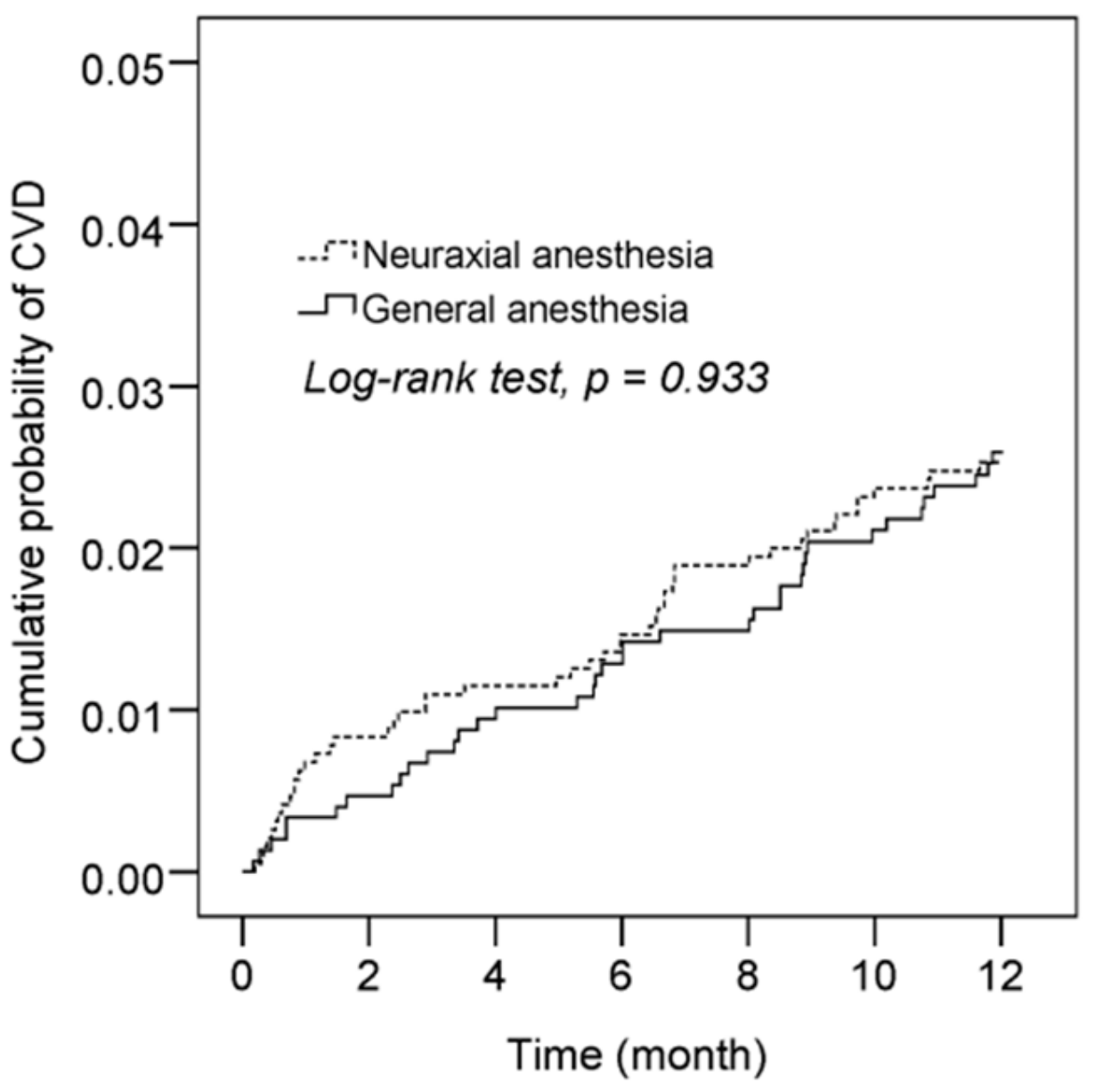
3.2. Risk of CVD with General Anesthesia, Neuraxial Anesthesia, Age, Gender, Different Comorbidities, and Other Conditions
3.3. Risk of CVD Between General Anesthesia and Neuraxial Anesthesia Patients and Specific Subgroup Characteristics
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Neuraxial Anesthesia | General Anesthesia | |
|---|---|---|
| Follow-up duration (month, mean ± SD) | 11.6 ± 2 | 11.5 ± 2.0 |
| Time to CVD (month, mean ± SD), N = 86 | 4.8 ± 3.6 | 6.0 ± 3.8 |
References
- Run, X.; Liang, Z.; Zhang, L.; Iqbal, K.; Grundke-Iqbal, I.; Gong, C.X. Anesthesia induces phosphorylation of tau. J. Alzheimer′s Dis. JAD 2009, 16, 619–626. [Google Scholar] [CrossRef] [PubMed]
- Perucho, J.; Rubio, I.; Casarejos, M.J.; Gomez, A.; Rodriguez-Navarro, J.A.; Solano, R.M.; De Yebenes, J.G.; Mena, M.A. Anesthesia with isoflurane increases amyloid pathology in mice models of alzheimer′s disease. J. Alzheimer′s Dis. JAD 2010, 19, 1245–1257. [Google Scholar] [CrossRef] [PubMed]
- Chia, Y.Y.; Lo, Y.; Chen, Y.B.; Liu, C.P.; Huang, W.C.; Wen, C.H. Risk of chronic low back pain among parturients who undergo cesarean delivery with neuraxial anesthesia: A nationwide population-based retrospective cohort study. Medicine 2016, 95, e3468. [Google Scholar] [CrossRef] [PubMed]
- Francula-Zaninovic, S.; Nola, I.A. Management of measurable variable cardiovascular disease′ risk factors. Curr. Cardiol. Rev. 2018, 14, 153–163. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention (CDC). Recommendations for use of an isoniazid-rifapentine regimen with direct observation to treat latent mycobacterium tuberculosis infection. MMWR Morb. Mortal. Wkly. Rep. 2011, 60, 1650–1653. [Google Scholar]
- Devereaux, P.J.; Sessler, D.I. Cardiac complications in patients undergoing major noncardiac surgery. N. Engl. J. Med. 2015, 373, 2258–2269. [Google Scholar] [CrossRef]
- Fitz-Henry, J. The asa classification and peri-operative risk. Ann. R. Coll. Surg. Engl. 2011, 93, 185–187. [Google Scholar] [CrossRef]
- Gelb, A.W.; Morriss, W.W.; Johnson, W.; Merry, A.F.; Abayadeera, A.; Belii, N.; Brull, S.J.; Chibana, A.; Evans, F.; Goddia, C.; et al. World health organization-world federation of societies of anaesthesiologists (who-wfsa) international standards for a safe practice of anesthesia. Anesth. Analg. 2018, 126, 2047–2055. [Google Scholar] [CrossRef]
- Fassoulaki, A.; Petropoulos, G.; Staikou, C.; Siafaka, I.; Sarantopoulos, C. General versus neuraxial anaesthesia for caesarean section: Impact on the duration of hospital stay. J. Obstet. Gynaecol. J. Inst. Obstet. Gynaecol. 2009, 29, 25–30. [Google Scholar] [CrossRef]
- Catro-Alves, L.J.; De Azevedo, V.L.; De Freitas Braga, T.F.; Goncalves, A.C.; De Oliveira, G.S., Jr. The effect of neuraxial versus general anesthesia techniques on postoperative quality of recovery and analgesia after abdominal hysterectomy: A prospective, randomized, controlled trial. Anesth. Analg. 2011, 113, 1480–1486. [Google Scholar] [CrossRef]
- Mauermann, W.J.; Shilling, A.M.; Zuo, Z. A comparison of neuraxial block versus general anesthesia for elective total hip replacement: A meta-analysis. Anesth. Analg. 2006, 103, 1018–1025. [Google Scholar] [CrossRef] [PubMed]
- An, R.; Pang, Q.Y.; Chen, B.; Liu, H.L. Effect of anesthesia methods on postoperative major adverse cardiac events and mortality after non-cardiac surgeries: A systematic review and meta-analysis. Minerva Anestesiol. 2017, 83, 749–761. [Google Scholar] [PubMed]
- Belmont, P.J., Jr.; Goodman, G.P.; Kusnezov, N.A.; Magee, C.; Bader, J.O.; Waterman, B.R.; Schoenfeld, A.J. Postoperative myocardial infarction and cardiac arrest following primary total knee and hip arthroplasty: Rates, risk factors, and time of occurrence. J. Bone Jt. Surg. Am. 2014, 96, 2025–2031. [Google Scholar] [CrossRef] [PubMed]
- You, A.H.; Han, D.W.; Ham, S.Y.; Lim, W.; Song, Y. Serum alkaline phosphatase as a predictor of cardiac and cerebrovascular complications after lumbar spinal fusion surgery in elderly: A retrospective study. J. Clin. Med. 2019, 8, 1111. [Google Scholar] [CrossRef] [PubMed]
- Costantino, S.; Paneni, F.; Cosentino, F. Ageing, metabolism and cardiovascular disease. J. Physiol. 2016, 594, 2061–2073. [Google Scholar] [CrossRef] [PubMed]
- Ageno, W.; Becattini, C.; Brighton, T.; Selby, R.; Kamphuisen, P.W. Cardiovascular risk factors and venous thromboembolism: A meta-analysis. Circulation 2008, 117, 93–102. [Google Scholar] [CrossRef] [PubMed]
- Ljungqvist, M.; Holmstrom, M.; Kieler, H.; Odeberg, J.; Larfars, G. Cardiovascular disease and mortality after a first episode of venous thromboembolism in young and middle-aged women. Thromb. Res. 2016, 138, 80–85. [Google Scholar] [CrossRef] [PubMed]
- Roshani, S.; Lijfering, W.M.; Coppens, M.; Hamulyak, K.; Prins, M.H.; Buller, H.R.; Middeldorp, S. Risk factors of arterial cardiovascular complications in patients with prior venous thromboembolism. Neth. J. Med. 2011, 69, 27–30. [Google Scholar]
- Gammelager, H.; Christiansen, C.F.; Johansen, M.B.; Tonnesen, E.; Jespersen, B.; Sorensen, H.T. Three-year risk of cardiovascular disease among intensive care patients with acute kidney injury: A population-based cohort study. Crit. Care (Lond. Engl.) 2014, 18, 492. [Google Scholar] [CrossRef]
- Gu, W.J.; Hou, B.L.; Kwong, J.S.W.; Tian, X.; Qian, Y.; Cui, Y.; Hao, J.; Li, J.C.; Ma, Z.L.; Gu, X.P. Association between intraoperative hypotension and 30-day mortality, major adverse cardiac events, and acute kidney injury after non-cardiac surgery: A meta-analysis of cohort studies. Int. J. Cardiol. 2018, 258, 68–73. [Google Scholar] [CrossRef]
- An, R.; Pang, Q.Y.; Liu, H.L. Association of intra-operative hypotension with acute kidney injury, myocardial injury and mortality in non-cardiac surgery: A meta-analysis. Int. J. Clin. Pract. 2019, 73, e13394. [Google Scholar] [CrossRef] [PubMed]
- Janssen, H.; Dehne, S.; Giannitsis, E.; Weigand, M.A.; Larmann, J. [Perioperative cardiovasular morbidity and mortality in noncardiac surgical interventions: Measures for optimal anesthesiological care]. Der Anaesthesist 2019, 68, 653–664. [Google Scholar] [PubMed]
| Variables | General Anesthesia (N = 1504) | Neuraxial Anesthesia (N = 1933) | p-Value | ||
|---|---|---|---|---|---|
| N | % | N | % | ||
| Age | <0.001 | ||||
| <65 | 1080 | 71.8 | 1176 | 60.8 | |
| ≥65 | 424 | 28.2 | 757 | 39.2 | |
| Mean ± SD | 50.7 ± 20.8 | 57.6 ± 20.8 | <0.001 | ||
| Gender | 0.406 | ||||
| Female | 720 | 47.9 | 953 | 49.3 | |
| Male | 784 | 52.1 | 980 | 50.7 | |
| Hypertension | 384 | 25.5 | 565 | 29.2 | 0.016 |
| Hyperlipidemia | 107 | 7.1 | 200 | 10.3 | 0.001 |
| Diabetes | 204 | 13.6 | 321 | 16.6 | 0.014 |
| Renal disease | 39 | 2.6 | 56 | 2.9 | 0.590 |
| Liver disease | 80 | 5.3 | 71 | 3.7 | 0.019 |
| Chronic pulmonary disease | 88 | 5.9 | 153 | 7.9 | 0.019 |
| Intensive care unit (ICU) admission | 127 | 8.4 | 44 | 2.3 | <0.001 |
| Anticoagulants | 69 | 4.6 | 107 | 5.5 | 0.211 |
| Anesthesia time | <0.001 | ||||
| <2 h | 742 | 49.3 | 1377 | 71.2 | |
| ≥2 h | 762 | 50.7 | 556 | 28.8 | |
| Hospital level | <0.001 | ||||
| Medical centers | 553 | 36.8 | 480 | 24.8 | |
| Regional hospitals | 725 | 48.2 | 826 | 42.7 | |
| District hospitals | 180 | 12.0 | 599 | 31.0 | |
| Clinics | 46 | 3.1 | 28 | 1.4 | |
| Variables | No. of CVD Events | Observed Person-Years | Incidence Density (Per 1000 Person-Years) | Crude HR | 95% CI | p-Value | Adjusted HR † | 95% CI | p-Value |
|---|---|---|---|---|---|---|---|---|---|
| Group | |||||||||
| Neuraxial anesthesia | 48 | 1861 | 25.8 | 1 | 1 | ||||
| General anesthesia | 38 | 1447 | 26.3 | 1.02 | 0.67–1.56 | 0.933 | 1.24 | 0.80–1.92 | 0.334 |
| Age | |||||||||
| <65 | 18 | 2221 | 8.1 | 1 | 1 | ||||
| ≥65 | 68 | 1087 | 62.6 | 7.67 | 4.56–12.90 | <0.001 | 5.77 | 3.21–10.38 | <0.001 |
| Gender | |||||||||
| Female | 43 | 1616 | 26.6 | 1 | 1 | ||||
| Male | 43 | 1692 | 25.4 | 0.95 | 0.63–1.46 | 0.829 | 1.89 | 1.21–2.95 | 0.005 |
| Hypertension | 52 | 886 | 58.7 | 4.16 | 2.70–6.42 | <0.001 | 1.63 | 0.98–2.70 | 0.059 |
| Hyperlipidemia | 14 | 293 | 47.8 | 2.00 | 1.13–3.54 | 0.018 | 0.91 | 0.49–1.66 | 0.749 |
| Diabetes | 35 | 485 | 72.2 | 3.97 | 2.58–6.11 | <0.001 | 2.09 | 1.29–3.37 | 0.003 |
| Renal disease | 8 | 78 | 102.7 | 4.18 | 2.02–8.66 | <0.001 | 1.48 | 0.70–3.12 | 0.305 |
| Liver disease | 3 | 142 | 21.1 | 0.80 | 0.25–2.54 | 0.707 | 0.58 | 0.18–1.84 | 0.354 |
| Chronic pulmonary disease | 11 | 221 | 49.8 | 2.04 | 1.08–3.84 | 0.027 | 1.21 | 0.64–2.30 | 0.561 |
| ICU admission | 11 | 142 | 77.3 | 3.22 | 1.71–6.06 | <0.001 | 2.59 | 1.35–4.96 | 0.004 |
| Anticoagulants | 14 | 159 | 87.8 | 3.81 | 2.15–6.75 | <0.001 | 1.80 | 0.97–3.31 | 0.061 |
| Variables | No. of CVD Events | Observed Person-Years | Incidence Density (Per 1000 Person-Years) | Crude HR | 95% CI | p-Value | Adjusted HR † | 95% CI | p-Value |
|---|---|---|---|---|---|---|---|---|---|
| Group | |||||||||
| NA < 2 h | 32 | 1326 | 24.1 | 1 | 1 | ||||
| NA ≥ 2 h | 16 | 535 | 29.9 | 1.24 | 0.68–2.26 | 0.482 | 1.00 | 0.55–1.83 | 0.999 |
| GA < 2 h | 15 | 720 | 20.8 | 0.86 | 0.47–1.60 | 0.641 | 1.05 | 0.57–1.95 | 0.866 |
| GA ≥ 2 h | 23 | 727 | 31.7 | 1.31 | 0.77–2.24 | 0.322 | 1.43 | 0.81–2.50 | 0.217 |
| General Anesthesia | Neuraxial Anesthesia | HR | 95% CI | p-Value | |||
|---|---|---|---|---|---|---|---|
| N | No. of CVD Events | N | No. of CVD Event | ||||
| Age † | |||||||
| <65 | 1080 | 7 | 1176 | 11 | 0.60 | 0.21–1.66 | 0.323 |
| ≥65 | 424 | 31 | 757 | 37 | 1.49 | 0.92–2.43 | 0.107 |
| sex ‡ | |||||||
| Female | 720 | 22 | 953 | 21 | 1.68 | 0.92–3.07 | 0.093 |
| Male | 784 | 16 | 980 | 27 | 0.84 | 0.43–1.66 | 0.619 |
| N | No. of CVD Event | Adjusted HR † | 95% CI | p-Value | |
|---|---|---|---|---|---|
| Follow-up period ≤6 months | |||||
| Group | |||||
| Neuraxial anesthesia | 1933 | 28 | 1 | ||
| General anesthesia | 1504 | 19 | 1.05 | 0.58–1.91 | 0.875 |
| Follow-up period 7–12 months | |||||
| Group | |||||
| Neuraxial anesthesia | 1859 | 20 | 1 | ||
| General anesthesia | 1444 | 19 | 1.52 | 0.79–2.91 | 0.206 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yeh, H.-W.; Yeh, L.-T.; Chou, Y.-H.; Yang, S.-F.; Ho, S.-W.; Yeh, Y.-T.; Yeh, Y.-T.; Wang, Y.-H.; Chan, C.-H.; Yeh, C.-B. Risk of Cardiovascular Disease Due to General Anesthesia and Neuraxial Anesthesia in Lower-Limb Fracture Patients: A Retrospective Population-Based Cohort Study. Int. J. Environ. Res. Public Health 2020, 17, 33. https://doi.org/10.3390/ijerph17010033
Yeh H-W, Yeh L-T, Chou Y-H, Yang S-F, Ho S-W, Yeh Y-T, Yeh Y-T, Wang Y-H, Chan C-H, Yeh C-B. Risk of Cardiovascular Disease Due to General Anesthesia and Neuraxial Anesthesia in Lower-Limb Fracture Patients: A Retrospective Population-Based Cohort Study. International Journal of Environmental Research and Public Health. 2020; 17(1):33. https://doi.org/10.3390/ijerph17010033
Chicago/Turabian StyleYeh, Han-Wei, Liang-Tsai Yeh, Ying-Hsiang Chou, Shun-Fa Yang, Sai-Wai Ho, Ying-Tung Yeh, Ying-Ting Yeh, Yu-Hsun Wang, Chi-Ho Chan, and Chao-Bin Yeh. 2020. "Risk of Cardiovascular Disease Due to General Anesthesia and Neuraxial Anesthesia in Lower-Limb Fracture Patients: A Retrospective Population-Based Cohort Study" International Journal of Environmental Research and Public Health 17, no. 1: 33. https://doi.org/10.3390/ijerph17010033
APA StyleYeh, H.-W., Yeh, L.-T., Chou, Y.-H., Yang, S.-F., Ho, S.-W., Yeh, Y.-T., Yeh, Y.-T., Wang, Y.-H., Chan, C.-H., & Yeh, C.-B. (2020). Risk of Cardiovascular Disease Due to General Anesthesia and Neuraxial Anesthesia in Lower-Limb Fracture Patients: A Retrospective Population-Based Cohort Study. International Journal of Environmental Research and Public Health, 17(1), 33. https://doi.org/10.3390/ijerph17010033






