Health Risk Assessment Indicators for the Left-Behind Elderly in Rural China: A Delphi Study
Abstract
1. Introduction
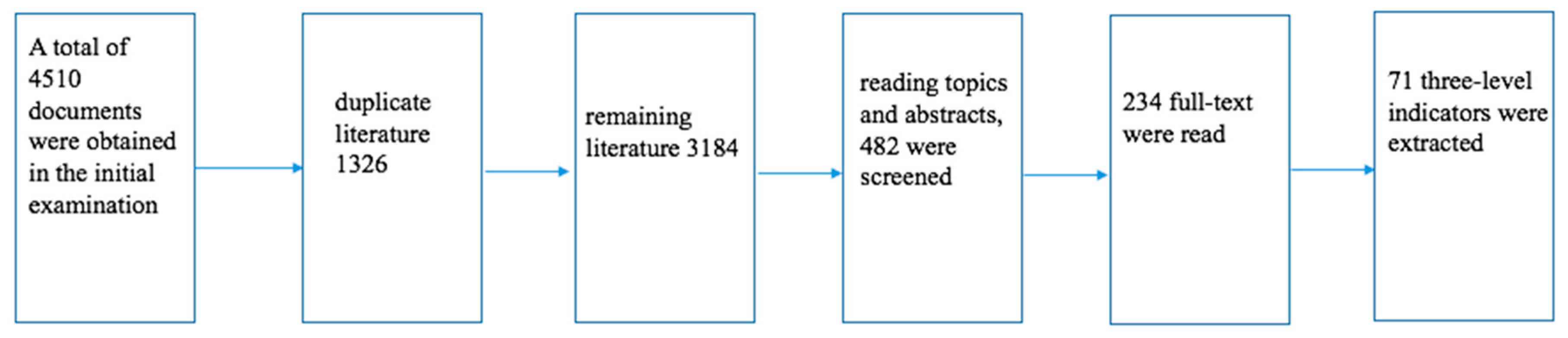
2. Materials and Methods
2.1. Experts Selection and Delphi Implemention
2.2. Questionnaire Preparation
2.3. Statistical Analysis
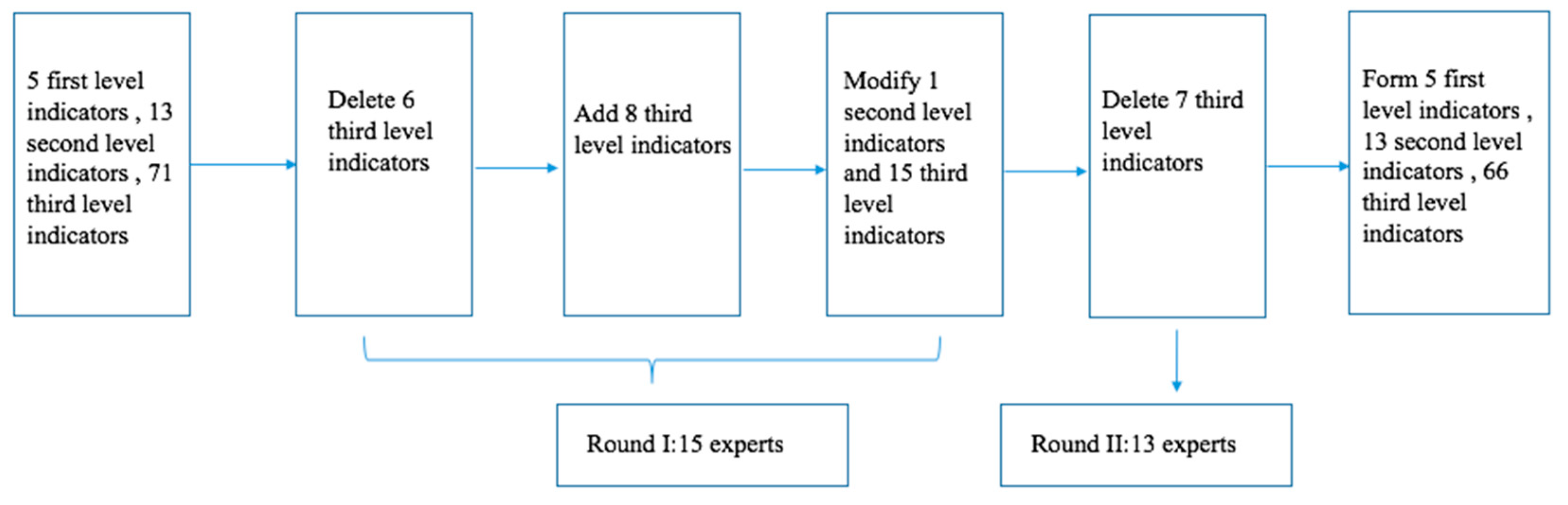
3. Results
3.1. The Authority of Experts
3.2. The Authority of Experts
3.3. Delphi Round I
3.4. Delphi Round II
3.5. Final Indicators
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Cao, G.Z.; Bian, X.; Zhao, J.H. The structural character and spatial disparity of left-behind families in rural China: Evidence from a nationwide survey in 30 counties in 6 provinces. Popul. Dev. 2013, 19, 2–10. [Google Scholar]
- Zhou, L.; Wang, G.; Jia, C. Being left-behind, mental disorder, and elderly suicide in rural China: A case–control psychological autopsy study. Psychol. Med. 2018, 49, 1–7. [Google Scholar] [CrossRef]
- Ye, J.Z.; He, Z.C. The Silent Sunset: The Left-Behind Elderly in Rural China Areas; Beijing Social Science Press: Beijing, China, 2008. [Google Scholar]
- Carballo, M.; Divino, J.J.; Zeric, D. Migration and health in the European Union. Trop. Med. Int. Health 1998, 3, 936–944. [Google Scholar] [CrossRef] [PubMed]
- Federal Interagency Forum on Aging-Related Statistics. Older Americans 2012: Key Indicators of Well-Being. Federal Interagency Forum on Aging-Related Statistics; Government Printing Office: Washington, DC, USA, 2012.
- Theeke, L.A. Predictors of loneliness in U.S. adults over age sixty-five. Arch. Psychiatr. Nurs. 2009, 23, 387–396. [Google Scholar] [CrossRef] [PubMed]
- Li, L.W.; Liu, J.; Xu, H.; Zhang, Z. Understanding rural-urban differences in depressive symptoms among older adults in china. J. Aging Health 2016, 28, 341–362. [Google Scholar] [CrossRef] [PubMed]
- Song, Q. Facing double jeopardy? Depressive symptoms in left-behind elderly in rural china. J. Aging Health 2017, 29, 1182–1213. [Google Scholar] [PubMed]
- Yang, X.L.; Xu, H.; Tang, G.Z.; He, Z.C.; Tu, D.; Yang, Y. Two-week prevalence rate and risk factors of rural left-behind elderly in Chongqing. Chongqing Med. 2015, 44, 2947–2948. [Google Scholar]
- Abas, M.; Tangchonlatip, K.; Punpuing, S.; Jirapramukpitak, T.; Darawuttimaprakorn, N.; Prince, M.; Flach, C. Migration of Children and Impact on Depression in Older Parents in Rural Thailand, Southeast Asia. JAMA Psychiatry 2013, 70, 226–234. [Google Scholar] [CrossRef]
- Antman, F.M. Adult Child Migration and the Health of Elderly Parents Left Behind in Mexico. Am. Econ. Rev. 2010, 100, 205–208. [Google Scholar] [CrossRef]
- He, G.; Xie, J.F.; Zhou, J.D.; Zhong, Z.Q.; Qin, C.X.; Ding, S.Q. Depression in left-behind elderly in rural china: Prevalence and associated factors. Geriatr. Gerontol. Int. 2016, 16, 638–643. [Google Scholar] [CrossRef]
- Miltiades, H.B. The social and psychological effect of an adult child’s emigration on non-immigrant Asian Indian elderly parents. J. Cross Cult. Gerontol. 2002, 17, 33. [Google Scholar] [CrossRef] [PubMed]
- Glaesmer, H.; Riedel-Heller, S.; Braehler, E.; Spangenberg, L.; Luppa, M. Age-and gender-specific prevalence and risk factors for depressive symptoms in the elderly: A population-based study. Int. Psychogeriatr. 2011, 23, 1294–1300. [Google Scholar] [CrossRef] [PubMed]
- Ding, Z.J.; Wang, G.P.; Zhang, Y.L.; Xie, R.; Pei, G.X.; Du, H.Y. Epidemiological survey of mental disorders in the rural left behind elderly aged 60 years and older in Gansu. Zhonghua Yi Xue Za Zhi 2019, 99, 2429–2434. [Google Scholar] [PubMed]
- Forlani, C.; Morri, M.; Ferrari, B.; Dalmonte, E.; Menchetti, M.; De Ronchi, D.; Atti, A.R. Prevalence and gender differences in late-life depression: A population-based study. Am. J. Geriatr. Psychiatry 2014, 22, 370–380. [Google Scholar] [CrossRef] [PubMed]
- Houtjes, W.; Deeg, D.; Van de Van, P.; Van Meijel, B.; Van Tilburg, T.; Beekman, A. Is the naturalistic course of depression in older people related to received support over time? results from a longitudinal population-based study. Int. J. Geriatr. Psychiatry 2017, 32, 657–663. [Google Scholar] [CrossRef]
- Williams, L.; Zhang, R.; Packard, K.C. Factors affecting the physical and mental health of older adults in china: The importance of marital status, child proximity, and gender. SSM Popul. Health 2017, 3, 20–36. [Google Scholar] [CrossRef]
- Zhong, Y.; Pär, S.; Bo, B.; Kristina, B. Association between social capital and health-related quality of life among left behind and not left behind older people in rural china. BMC Geriatr. 2017, 17, 287. [Google Scholar] [CrossRef]
- Xie, J.F.; Ding, S.Q.; Zhong, Z.Q.; Yi, Q.F.; Zeng, S.N.; Hu, J.H.; Zhou, J.D. Mental health is the most important factor influencing quality of life in elderly left behind when families migrate out of rural China. Rev. Lat. Am. Enferm. 2014, 22, 364–370. [Google Scholar] [CrossRef]
- Adhikari, R.; Jampaklay, A.; Chamratrithirong, A. Impact of children’s migration on health and health care-seeking behavior of elderly left behind. BMC Public Health 2011, 11, 143. [Google Scholar] [CrossRef]
- Fu, H. Preventive Medicine; People’s Health Press: Beijing, China, 2008. [Google Scholar]
- Fisher, E.B.; Brownson, C.A.; O’toole, M.L. Ecological approaches to self-management: The case of diabetes. Am. J. Public Health 2005, 95, 1523–1535. [Google Scholar] [CrossRef]
- Huberty, J.L.; Balluff, M.; O’dell, M. From good ideas to actions: A model-driven community collaborative to prevent childhood obesity. Prev. Med. 2010, 50, S36. [Google Scholar] [CrossRef] [PubMed]
- Maibach, E.; Abroms, L.; Marosits, M. Communication and Marketing as Tools to Cultivate the Public’s Health. BMC Public Health 2007, 7, 88. [Google Scholar] [CrossRef] [PubMed]
- Anand, M. A Common Monitoring & Evaluation Framework Guided by the Collective Impact Model: Recommendations to Enhance the Tobacco Control Effort in Sub-Saharan Africa. Master’s Thesis, Georgia State University, Atlanta, GA, USA, 2013. [Google Scholar]
- Dalkey, N.; Helmer, O. An experimental application of the Delphi method to the use of experts. Manag. Sci. 1963, 9, 458–467. [Google Scholar] [CrossRef]
- Ryan, M.; Scott, D.A.; Reeves, C.; Bate, A.; van Teijlingen, E.R.; Russell, E.M.; Napper, M.; Robb, C.M. Eliciting public preferences for healthcare: A systematic review of techniques. Health Technol. Assess. 2001, 5, 1–186. [Google Scholar] [CrossRef]
- Hsu, C.-C.; Sandford, B.A. The Delphi technique: Making sense of consensus. Pract. Assess. Res. Eval. 2007, 12, 1–8. [Google Scholar]
- Boulkedid, R.; Abdoul, H.; Loustau, M.; Sibony, O.; Alberti, C. Using and reporting the Delphi method for selecting healthcare quality indicators: A systematic review. PLoS ONE 2011, 6, e20476. [Google Scholar] [CrossRef]
- Prinsen, C.A.; Vohra, S.; Rose, M.R. Core Outcome Measures in Effectiveness Trials (COMET) initiative: Protocol for an international Delphi study to achieve consensus on how to select outcome measurement instruments for outcomes included in a ‘core outcome set’. Trials 2014, 15, 247. [Google Scholar] [CrossRef]
- Murphy, M.K.; Black, N.A.; Lamping, D.L. Consensus development methods, and their use in clinical guideline development. Health Technol. Assess. 1998, 2, 1–88. [Google Scholar] [CrossRef]
- Young, J.M.; Masya, L.M.; Solomon, M.J.; Shepherd, H.L. Identifying indicators of colorectal cancer care coordination: A Delphi study. Colorectal Dis. 2014, 16, 17–25. [Google Scholar] [CrossRef]
- Mcgeoch, M.; Brunetto, Y.; Brown, K. The policy delphi method: Contribution to policy and strategy within energy organisations: A 2013 malaysian case study with global implications. Qual. Quant. 2014, 48, 3195–3208. [Google Scholar] [CrossRef]
- Rees, T. St john health, integrating new corporate identity, brand. brand/logo to be rolled out over two-year period. Profiles Healthc. Mark. 2003, 19, 14–18. [Google Scholar]
- Pi, H.Y.; Peng, P.P.; Su, Q.Q.; Wang, Y.L.; Tang, J.P.; Zhang, J. A study on long-term care of quality evaluation index system for disabled elderly. Chin. J. Nurs. 2018, 53, 1110–1114. [Google Scholar]
- Zhao, Y.X.; Zhang, H. Survey on the quality of life of the left-behind elderly in a rural area of Henan Province and analysis of its influencing factors. China Rural Health 2016, 13, 46–48. [Google Scholar]
- Qiu, H.X.; Luo, W.; Xiao, Y.; Huang, J.Y. Comparison of health status and outpatient treatment behaviour of elderly people with different income levels. Chin. J. Gerontol. 2017, 37, 6225–6227. [Google Scholar]
- He, C.; Ye, J. Lonely sunsets: Impacts of rural-urban migration on the left-behind elderly in rural China. Popul. Space Place 2014, 20, 352–369. [Google Scholar] [CrossRef]
- Yang, S. Structural analysis of health evaluation and influencing factors of the old left behind in rural areas. J. Hebei Univ. Philos. Soc. Sci. 2017, 42, 154–160. [Google Scholar]
- Wakai, A.; O’Sullivan, R.; Staunton, P.; Walsh, C.; Hickey, F.; Plunkett, P.K. Development of key performance indicators for emergency departments in Ireland using an electronic modified-Delphi consensus approach. Eur. J. Emerg. Med. 2013, 20, 109–114. [Google Scholar] [CrossRef]
- Buxton, M.J. Economic evaluation and decision making in the UK. Pharm. Econ. 2006, 24, 1133–1142. [Google Scholar] [CrossRef]
| Judgment Basis | Degree of Influence on Expert Judgment | ||
|---|---|---|---|
| Big | Medium | Small | |
| theoretical analysis | 0.1 | 0.1 | 0.1 |
| practical experience | 0.5 | 0.4 | 0.3 |
| peer understanding | 0.3 | 0.2 | 0.1 |
| intuitive perception | 0.1 | 0.1 | 0.1 |
| Characteristics | Experts in Round I (n = 13) | Experts in Round II (n = 12) |
|---|---|---|
| Age | M = 46.92, SD = 5.63 | M = 47.67, SD = 5.18 |
| Gender | ||
| Male | 2 (15.38%) | 2 (16.67%) |
| Female | 11 (84.61) | 10 (83.33%) |
| Province | ||
| Beijing | 1 (7.69%) | 1 (8.33%) |
| Tianjin | 5 (38.46%) | 4 (33.33%) |
| Shanxi | 1 (7.69%) | 1 (8.33%) |
| Fujian | 3 (23.08%) | 3 (25%) |
| Zhejiang | 2 (15.38%) | 2 (16.67%) |
| Jilin | 1 (7.69%) | 1 (8.33%) |
| Speciality | ||
| Geriatrics | 7 (53.85%) | 6 (50%) |
| Health management | 4 (30.77%) | 4 (33.33%) |
| Social psychology | 2 (15.38%) | 2 (16.67%) |
| Professional title | ||
| Senior professional title | 5 (38.46%) | 5 (41.27%) |
| Sub-senior professional title | 8 (61.54%) | 7 (58.33%) |
| Judgment Basis | Big | Medium | Small | |||
|---|---|---|---|---|---|---|
| Number | Frequency | Number | Frequency | Number | Frequency | |
| Theoretical analysis | 11 | 84.62% | 2 | 15.38% | 0 | 0.00% |
| Practical experience | 8 | 61.54% | 5 | 38.46% | 0 | 0.00% |
| Peer understanding | 3 | 23.08% | 8 | 61.54% | 2 | 15.38% |
| Intuitive perception | 0 | 0.00% | 6 | 46.15% | 7 | 53.85% |
| Expert Familiarity | Very Familiar | Relatively Familiar | Generally Familiar | A Little Familiar | Unfamiliar |
|---|---|---|---|---|---|
| Round I (Number of experts) | 6 | 5 | 2 | 0 | 0 |
| Round II (Number of experts) | 6 | 5 | 1 | 0 | 0 |
| First-Grade Index (Weight) | Second-Grade Index (Weight) | Third-Grade Index | M ± SD | CV | Weight |
|---|---|---|---|---|---|
| Personal traits (0.248) | Native traits (0.124) | Gender | 4.33 ± 0.65 | 0.15 | 0.062 |
| Age | 5 | 0 | 0.062 | ||
| Disease susceptibility (0.124) | Inheritance factor | 4.75 ± 0.45 | 0.10 | 0.015 | |
| Nutritional status | 4.75 ± 0.45 | 0.10 | 0.015 | ||
| Suffering from chronic diseases | 4.83 ± 0.39 | 0.08 | 0.026 | ||
| Types of chronic diseases | 4.83 ± 0.39 | 0.08 | 0.026 | ||
| Severity of chronic diseases | 5 | 0 | 0.041 | ||
| Behavioral characteristics (0.248) | Psychosocial characteristics (0.062) | Character | 4.50 ± 0.67 | 0.15 | 0.009 |
| Coping style | 4.75 ± 0.45 | 0.10 | 0.017 | ||
| Hobbies and interests | 4.08 ± 0.90 | 0.22 | 0.004 | ||
| Negative life events | 4.92 ± 0.29 | 0.06 | 0.027 | ||
| Ageing attitudes | 4.33 ± 0.89 | 0.21 | 0.006 | ||
| Habits (0.062) | Eating habits | 4.83 ± 0.39 | 0.08 | 0.028 | |
| Smoking | 4.92 ± 0.29 | 0.06 | 0.028 | ||
| Drinking | 5 | 0 | 0.053 | ||
| Sleep condition | 4.67 ± 0.49 | 0.11 | 0.015 | ||
| Health behavior (0.124) | Medication compliance | 5 | 0 | 0.031 | |
| Health knowledge | 4.75 ± 0.45 | 0.10 | 0.009 | ||
| Physical exercise | 4.92 ± 0.29 | 0.06 | 0.022 | ||
| Active medical seeking behavior | 4.83 ± 0.39 | 0.08 | 0.012 | ||
| Activities of daily life | 4.75 ± 0.45 | 0.10 | 0.016 | ||
| Interpersonal network (0.150) | Family Interpersonal Network (0.090) | Marital status | 4.58 ± 0.52 | 0.11 | 0.003 |
| Spouse health | 4.75 ± 0.45 | 0.10 | 0.004 | ||
| Family relationship | 4.83 ± 0.39 | 0.08 | 0.006 | ||
| Family size | 3.92 ± 0.90 | 0.23 | 0.001 | ||
| Living style | 4.50 ± 0.67 | 0.15 | 0.002 | ||
| Look after by spouse | 4.75 ± 0.45 | 0.10 | 0.004 | ||
| Frequency of children returning home | 3.92 ± 0.67 | 0.17 | 0.001 | ||
| Physical condition of children | 4.08 ± 0.90 | 0.22 | 0.001 | ||
| Economic status of children | 4.50 ± 0.52 | 0.12 | 0.003 | ||
| Number of outgoing children | 3.75 ± 0.75 | 0.20 | 0.001 | ||
| Take care of grandchildren | 4.17 ± 0.84 | 0.20 | 0.001 | ||
| Number of grandchildren to take care | 3.92 ± 0.67 | 0.17 | 0.001 | ||
| Years of left behind | 4.33 ± 0.78 | 0.18 | 0.002 | ||
| Community interpersonal network (0.030) | Frequency of communication with neighborhood | 4.17 ± 0.58 | 0.14 | 0.004 | |
| Neighborhood friendship | 4.50 ± 0.67 | 0.15 | 0.008 | ||
| Assistant for neighborhood | 4.33 ± 0.78 | 0.18 | 0.008 | ||
| Frequency of communication with relatives | 4.08 ± 0.67 | 0.16 | 0.002 | ||
| relationship | 4.42 ± 0.79 | 0.18 | 0.005 | ||
| Relatives’ help | 4.17 ± 0.84 | 0.20 | 0.004 | ||
| Social Interpersonal Network (0.030) | Assistance provided by medical institutions | 4.83 ± 0.58 | 0.12 | 0.111 | |
| Access to external information | 4.42 ± 0.67 | 0.15 | 0.037 | ||
| Living conditions (0.223) | Conditions for medical treatment (0.149) | Sources of medical expenses | 4.67 ± 0.49 | 0.11 | 0.007 |
| Children bear medical expenses | 4.08 ± 0.67 | 0.16 | 0.002 | ||
| Utilization of health resources | 5 | 0 | 0.016 | ||
| Traffic time of go to doctor | 5 | 0 | 0.016 | ||
| Regular physical examination | 5 | 0 | 0.016 | ||
| Technical level of medical staff | 4.33 ± 0.49 | 0.11 | 0.004 | ||
| Service attitudes of medical staff | 4.17 ± 0.84 | 0.20 | 0.003 | ||
| Infrastructure health facilities | 4.83 ± 0.58 | 0.12 | 0.010 | ||
| Socio-economic status (0.074) | Degree of education | 4.67 ± 0.49 | 0.11 | 0.007 | |
| Labor intensity | 4.25 ± 0.75 | 0.18 | 0.011 | ||
| Residential environment | 4.92 ± 0.29 | 0.06 | 0.001 | ||
| Engage in sideline work | 3.42 ± 0.52 | 0.15 | 0.017 | ||
| Economic source | 5 | 0 | 0.011 | ||
| Family economic situation | 4.83 ± 0.39 | 0.08 | 0.005 | ||
| Social assistance | 4.42 ± 0.79 | 0.18 | 0.005 | ||
| New rural social pension insurance | 4.50 ± 0.52 | 0.12 | 0.028 | ||
| Social, economic, cultural, and related policies (0.131) | Political environment (0.056) | Social security policy | 5 | 0 | 0.028 |
| Public health policy | 5 | 0 | 0.019 | ||
| Economic environment (0.056) | Local economic development level | 4.58 ± 0.52 | 0.11 | 0.037 | |
| Local economic burden of medical care | 4.75 ± 0.45 | 0.10 | 0.002 | ||
| Cultural and recreational activities | 3.67 ± 0.78 | 0.21 | 0.003 | ||
| Cultural environment (0.019) | Nationality | 3.92 ± 0.79 | 0.20 | 0.007 | |
| Ideology | 4.33 ± 0.99 | 0.23 | 0.001 | ||
| Hygiene concept | 3.42 ± 0.67 | 0.20 | 0.007 | ||
| Religious belief | 4.33 ± 0.49 | 0.11 | 0.062 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Luo, R.; Zhang, C.; Liu, Y. Health Risk Assessment Indicators for the Left-Behind Elderly in Rural China: A Delphi Study. Int. J. Environ. Res. Public Health 2020, 17, 340. https://doi.org/10.3390/ijerph17010340
Luo R, Zhang C, Liu Y. Health Risk Assessment Indicators for the Left-Behind Elderly in Rural China: A Delphi Study. International Journal of Environmental Research and Public Health. 2020; 17(1):340. https://doi.org/10.3390/ijerph17010340
Chicago/Turabian StyleLuo, Ruzhen, Chunmei Zhang, and Yanhui Liu. 2020. "Health Risk Assessment Indicators for the Left-Behind Elderly in Rural China: A Delphi Study" International Journal of Environmental Research and Public Health 17, no. 1: 340. https://doi.org/10.3390/ijerph17010340
APA StyleLuo, R., Zhang, C., & Liu, Y. (2020). Health Risk Assessment Indicators for the Left-Behind Elderly in Rural China: A Delphi Study. International Journal of Environmental Research and Public Health, 17(1), 340. https://doi.org/10.3390/ijerph17010340




