Self-Reported Prevalence of Allergies in the USA and Impact on Skin—An Epidemiological Study on a Representative Sample of American Adults
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Survey
2.3. Statistical Analysis
3. Results
3.1. General Population
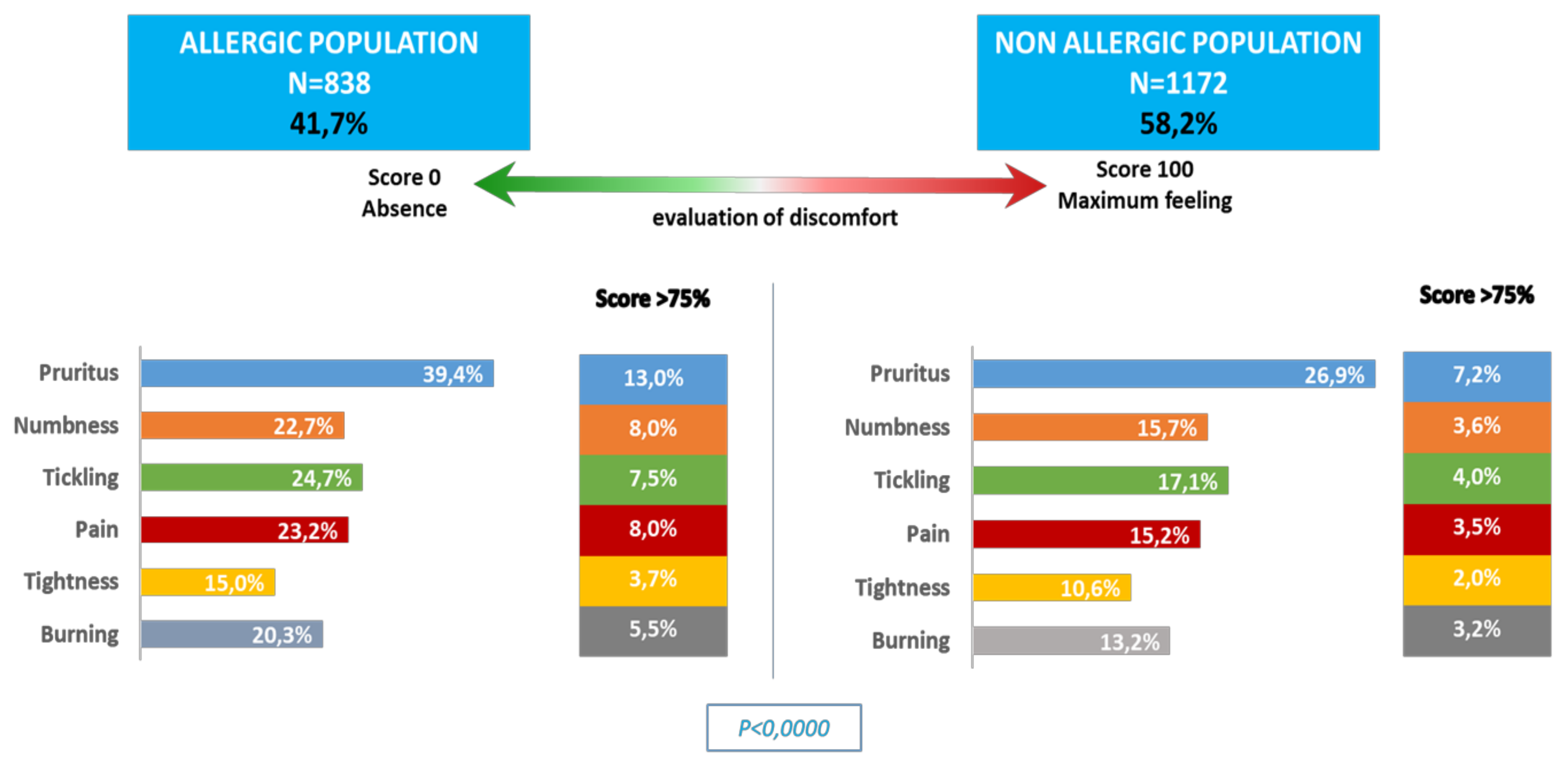
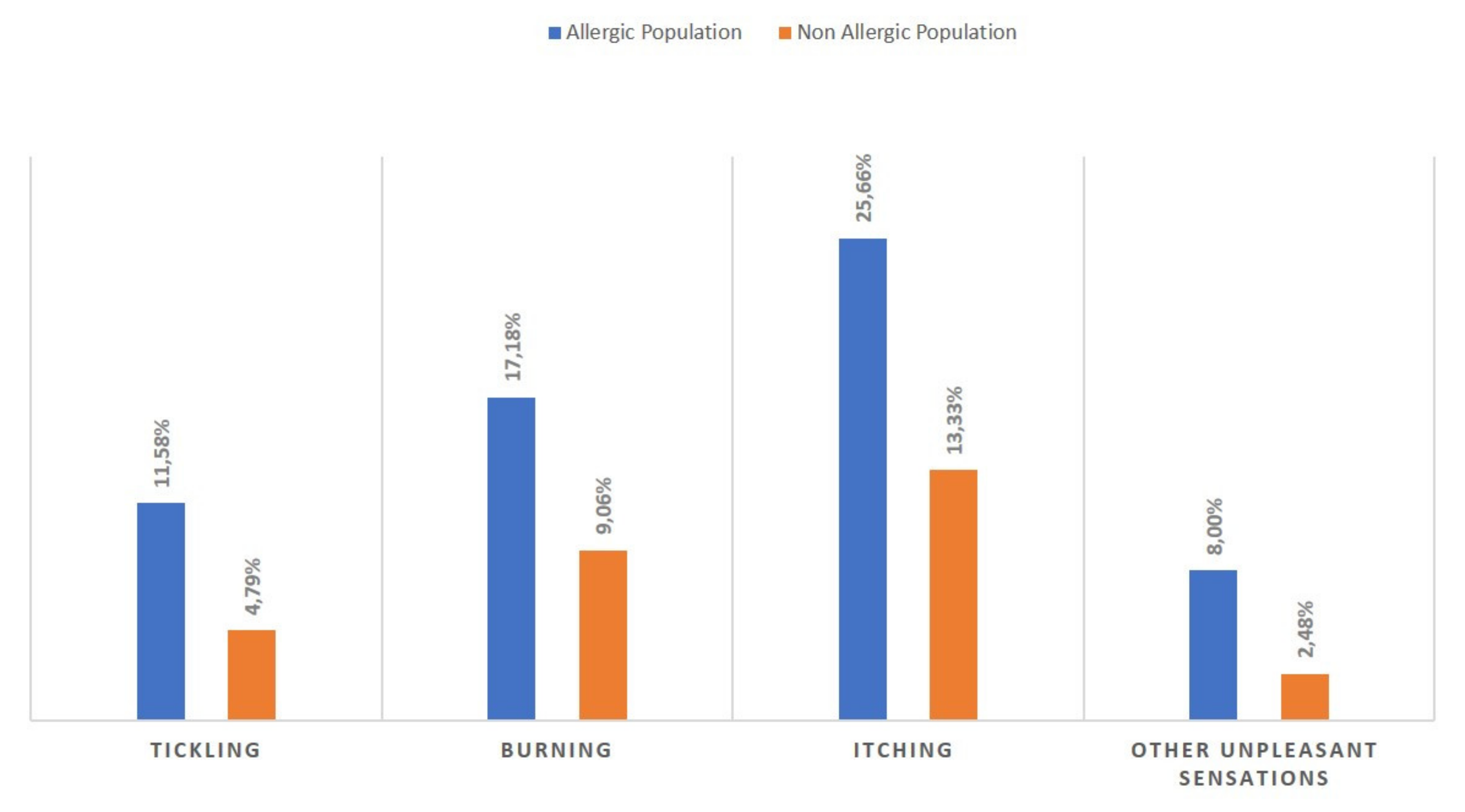
3.2. Allergic Population Versus Non-Allergic Population
3.3. Environmental Impact
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Okada, H.; Kuhn, C.; Feillet, H.; Bach, J.-F. The ‘hygiene hypothesis’ for autoimmune and allergic diseases: An update. Clin. Exp. Immunol. 2010, 160, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Tang, M.L.; Mullins, R.J. Food allergy: Is prevalence increasing? Intern. Med. J. 2017, 47, 256–261. [Google Scholar] [CrossRef] [PubMed]
- Jackson, K.D.; Howie, L.D.; Akinbami, L.J. Trends in allergic conditions among children: United States, 1997–2011. NCHS Data Brief 2013, 121, 1–8. [Google Scholar]
- Grief, S.N. Food Allergies. Prim. Care Clin. Off. Pract. 2016, 43, 375–391. [Google Scholar] [CrossRef]
- Molinari, G.; Colombo, G.; Celenza, C. Respiratory Allergies: A General Overview of Remedies, Delivery Systems, and the Need to Progress. ISRN Allergy 2014, 2014, 326980. [Google Scholar] [CrossRef] [Green Version]
- Schiavoni, G.; D’Amato, G.; Afferni, C. The dangerous liaison between pollens and pollution in respiratory allergy. Ann. Allergy Asthma Immunol. 2017, 118, 269–275. [Google Scholar] [CrossRef] [Green Version]
- Kostner, L.; Anzengruber, F.; Guillod, C.; Recher, M.; Schmid-Grendelmeier, P.; Navarini, A. Allergic Contact Dermatitis. Immunol. Allergy Clin. North Am. 2017, 37, 141–152. [Google Scholar] [CrossRef] [Green Version]
- Bantz, S.K.; Zhu, Z.; Zheng, T. The Atopic March: Progression from Atopic Dermatitis to Allergic Rhinitis and Asthma. J. Clin. Cell. Immunol. 2014, 5, 1–8. [Google Scholar]
- Salo, P.M.; Arbes, S.J.; Jaramillo, R.; Calatroni, A.; Weir, C.H.; Sever, M.L.; Hoppin, J.A.; Rose, K.M.; Liu, A.H.; Gergen, P.J.; et al. Prevalence of allergic sensitization in the United States: Results from the National Health and Nutrition Examination Survey (NHANES) 2005-2006. J. Allergy Clin. Immunol. 2014, 134, 350–359. [Google Scholar] [CrossRef] [Green Version]
- Boerma, T.; Hosseinpoor, A.R.; Verdes, E.; Chatterji, S. A global assessment of the gender gap in self-reported health with survey data from 59 countries. BMC Public Health 2016, 16, 675. [Google Scholar] [CrossRef] [Green Version]
- Kandrack, M.A.; Grant, K.R.; Segall, A. Gender differences in health related behaviour: Some unanswered questions. Soc. Sci. Med. 1991, 32, 579–590. [Google Scholar] [CrossRef]
- Sicherer, S.H. Epidemiology of food allergy. J. Allergy Clin. Immunol. 2011, 127, 594–602. [Google Scholar] [CrossRef] [PubMed]
- Dunlop, J.H.; Keet, C.A. Epidemiology of Food Allergy. Immunol. Allergy Clin. N. Am. 2018, 38, 13–25. [Google Scholar] [CrossRef] [PubMed]
- Ring, J.; Krämer, U.; Schäfer, T.; Behrendt, H. Why are allergies increasing? Curr. Opin. Immunol. 2001, 13, 701–708. [Google Scholar] [CrossRef]
- Platts-Mills, T.A. The allergy epidemics: 1870–2010. J. Allergy Clin. Immunol. 2015, 136, 3–13. [Google Scholar] [CrossRef] [Green Version]
- Lambrecht, B.N.; Hammad, H. The immunology of the allergy epidemic and the hygiene hypothesis. Nat. Immunol. 2017, 18, 1076–1083. [Google Scholar] [CrossRef]
- Strugar, T.L.; Kuo, A.; Seité, S.; Lin, M.; Lio, P. Connecting the Dots: From Skin Barrier Dysfunction to Allergic Sensitization, and the Role of Moisturizers in Repairing the Skin Barrier. J. Drugs Dermatol. 2019, 18, 581. [Google Scholar]
- Bergmann, M.M.; Caubet, J.-C.; Boguniewicz, M.; Eigenmann, P. Evaluation of Food Allergy in Patients with Atopic Dermatitis. J. Allergy Clin. Immunol. Pract. 2013, 1, 22–28. [Google Scholar] [CrossRef]
- Östling, J.; Van Geest, M.; Schofield, J.P.; Jevnikar, Z.; Wilson, S.; Ward, J.; Lutter, R.; Shaw, D.E.; Bakke, P.S.; Caruso, M.; et al. IL-17–high asthma with features of a psoriasis immunophenotype. J. Allergy Clin. Immunol. 2019, 144, 1198–1213. [Google Scholar] [CrossRef] [Green Version]
- Schmier, J.K.; Chan, K.S.; Leidy, N.K. The impact of asthma on health-related quality of life. J. Asthma 1998, 35, 585–597. [Google Scholar] [CrossRef]
- Bacal, L.R. The impact of food allergies on quality of life. Pediatr. Ann. 2013, 42, 141–145. [Google Scholar] [CrossRef] [PubMed]
- Kalboussi, H.; Kacem, I.; Aroui Kalboussi, H.; Kacem, I.; Aroui, H.; El Maalel, O.; Maoua, M.; Brahem, A.; El Guedri, S.; Chatti, S.; et al. Impact of Allergic Contact Dermatitis on the Quality of Life and Work Productivity. Dermatol. Res. Pract. 2019, 2019, 3797536. [Google Scholar] [CrossRef] [PubMed]
- Burks, A.W.; Sampson, H.A.; Plaut, M.; Lack, G.; Akdis, C.A. Treatment for food allergy. J. Allergy Clin. Immunol. 2018, 141, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Del Giacco, S.R.; Bakirtas, A.; Bel, E.; Custovic, A.; Diamant, Z.; Hamelmann, E.; Heffler, E.; Kalayci, Ö.; Saglani, S.; Sergejeva, S.; et al. Allergy in severe asthma. Allergy 2016, 72, 207–220. [Google Scholar] [CrossRef] [Green Version]

| US Sex and Age Breakdown | Males | Females |
|---|---|---|
| 18–24 | 7% | 7% |
| 25–34 | 10% | 10% |
| 35–44 | 9% | 9% |
| 45–54 | 10% | 10% |
| 55–64 | 8% | 9% |
| 65–74 | 5% | 6% |
| USA Regions | ||
| West | 23% | |
| Midwest | 23% | |
| South | 36% | |
| Northwest/Northeast | 18% | |
| USA Annual Income in US$ | ||
| Less than 40,000 | 40% | |
| More than 40,000 | 60% |
| n | % | |
|---|---|---|
| Participants Reporting an Allergy | 838 | 41.73% |
| Subjects able to name the allergy | 333 | 39.74% |
| Percentage of Participants Diagnosed by A Doctor | 573 | 68.38% |
| Health professional who diagnosed the allergy | ||
| General practitioner | 259 | 45.20% |
| Allergy specialist | 145 | 25.31% |
| Dermatologist | 94 | 16.40% |
| Pediatrician | 33 | 5.76% |
| Otolaryngologist | 14 | 2.44% |
| Pulmonary specialist | 10 | 1.75% |
| Acupuncturist | 2 | 0.35% |
| Homeopathic doctor | 1 | 0.17% |
| Another specialized physician | 15 | 2.62% |
| n | % | |
|---|---|---|
| Symptoms Associated with Allergy Reported by Participants | ||
| Allergic rhinitis (hay fever) | 367 | 43.79% |
| Asthma | 220 | 26.25% |
| Eczema/Atopic dermatitis | 188 | 22.43% |
| Bronchitis with wheezing | 151 | 18.02% |
| Conjunctivitis | 61 | 7.28% |
| Edema | 35 | 4.18% |
| Other | 195 | 23.27% |
| Allergens Reported by Participants | n | % |
| Pollens | 529 | 63.13% |
| Dust mites | 353 | 42.12% |
| Mold | 294 | 35.08% |
| Dogs, cats, ferrets, other animals | 214 | 25.54% |
| Food allergens | 177 | 21.12% |
| Latex | 60 | 7.16% |
| Cockroaches | 59 | 7.04% |
| Hymenoptera (bees, wasps, hornets, etc.) | 50 | 5.97% |
| Other | 125 | 14.92% |
| n | % | |
|---|---|---|
| Percentage of Participants Reporting Skin Reaction | 400 | 47.73% |
| Percentage managed by a doctor | 189 | 47.25% |
| Who is the Health Professional Who Managed the Skin Reaction? | ||
| General practitioner | 88 | 46.56% |
| Allergy specialist | 59 | 31,22% |
| Dermatologist | 26 | 13.76% |
| Participants Reporting Prescribed Treatment for Skin Reaction | 148 | 78.30% |
| What kind of treatment was prescribed for your skin reaction? | ||
| Topical | 106 | 71.62% |
| Oral | 66 | 44.59% |
| Skincare products | 21 | 14.19% |
| Impacted | Worried | |||
|---|---|---|---|---|
| Allergic | Non-Allergic | Allergic | Non-Allergic | |
| n = 838 | n = 1172 | n = 838 | n = 1172 | |
| Air | 74.22% | 61.28% | 51.19% | 34.96% |
| Water | 29.47% | 22.65% | 6.56% | 7.18% |
| Soil | 12.05% | 6.75% | 2.86% | 1.62% |
| Noise | 35.92% | 27.01% | 11.22% | 13.59% |
| Light | 31.86% | 22.31% | 9.31% | 5.98% |
| Radiation | 18.26% | 15.13% | 4.06% | 4.79% |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seité, S.; Kuo, A.M.-S.; Taieb, C.; Strugar, T.L.; Lio, P. Self-Reported Prevalence of Allergies in the USA and Impact on Skin—An Epidemiological Study on a Representative Sample of American Adults. Int. J. Environ. Res. Public Health 2020, 17, 3360. https://doi.org/10.3390/ijerph17103360
Seité S, Kuo AM-S, Taieb C, Strugar TL, Lio P. Self-Reported Prevalence of Allergies in the USA and Impact on Skin—An Epidemiological Study on a Representative Sample of American Adults. International Journal of Environmental Research and Public Health. 2020; 17(10):3360. https://doi.org/10.3390/ijerph17103360
Chicago/Turabian StyleSeité, Sophie, Alyce Mei-Shiuan Kuo, Charles Taieb, Tamara Lazić Strugar, and Peter Lio. 2020. "Self-Reported Prevalence of Allergies in the USA and Impact on Skin—An Epidemiological Study on a Representative Sample of American Adults" International Journal of Environmental Research and Public Health 17, no. 10: 3360. https://doi.org/10.3390/ijerph17103360
APA StyleSeité, S., Kuo, A. M.-S., Taieb, C., Strugar, T. L., & Lio, P. (2020). Self-Reported Prevalence of Allergies in the USA and Impact on Skin—An Epidemiological Study on a Representative Sample of American Adults. International Journal of Environmental Research and Public Health, 17(10), 3360. https://doi.org/10.3390/ijerph17103360





