Prevalence of Muscular Skeletal Disorders among Qualified Dental Assistants
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Questionnaire
2.3. Recruitment
2.4. Data Editing and Analysis
3. Results
3.1. Study Population—Demographic Data
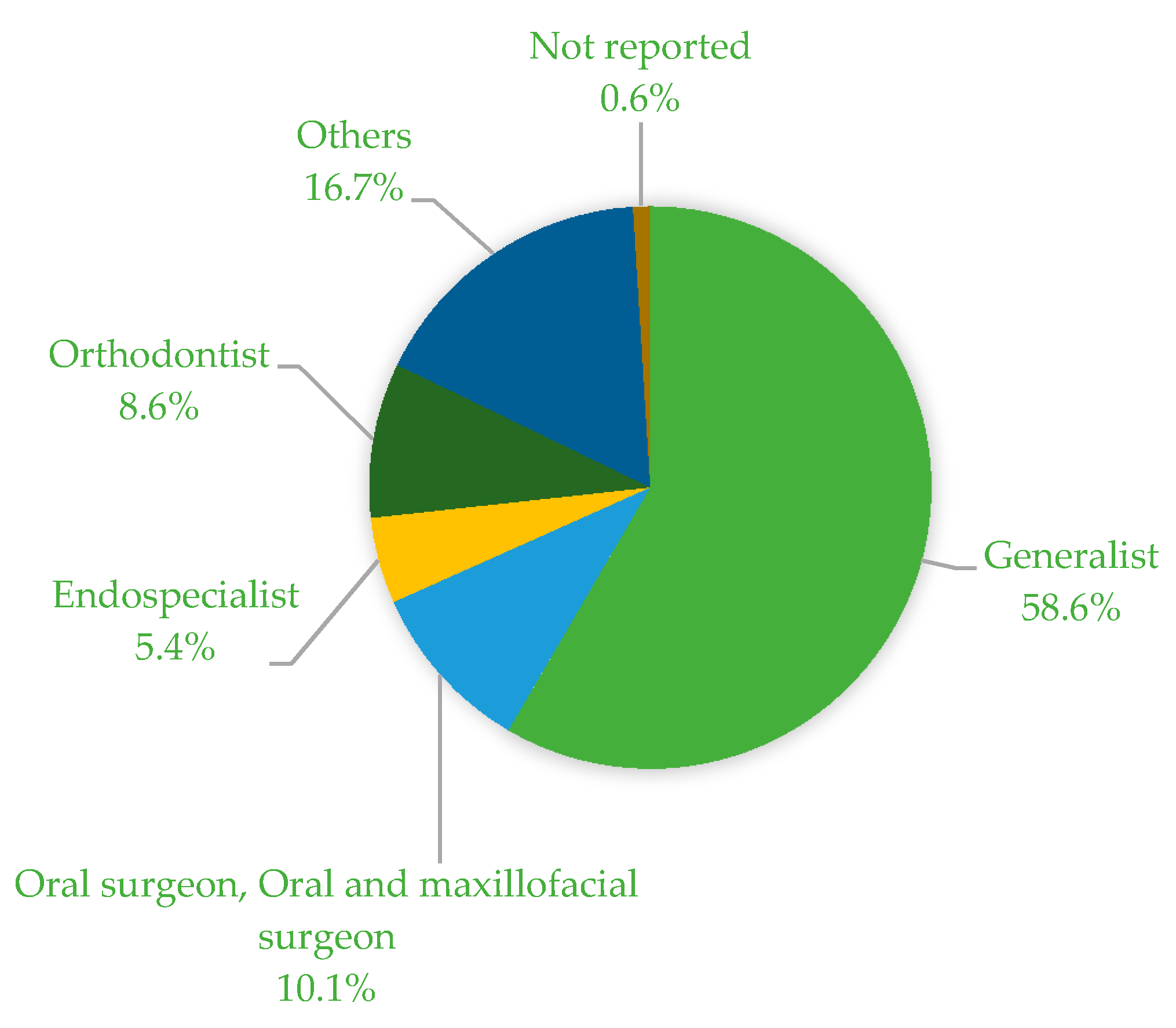
3.2. Study Population—Work-Related Questions
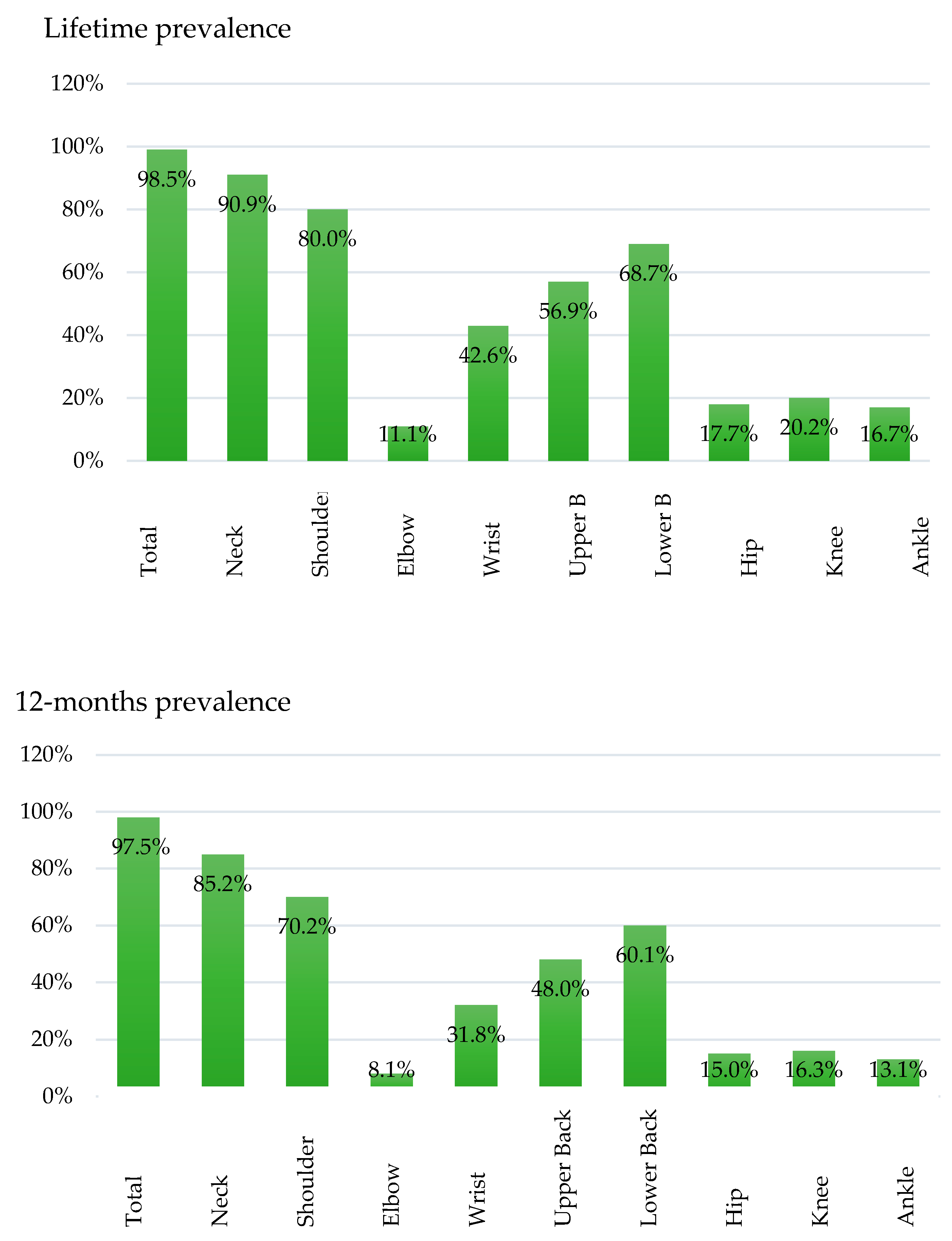
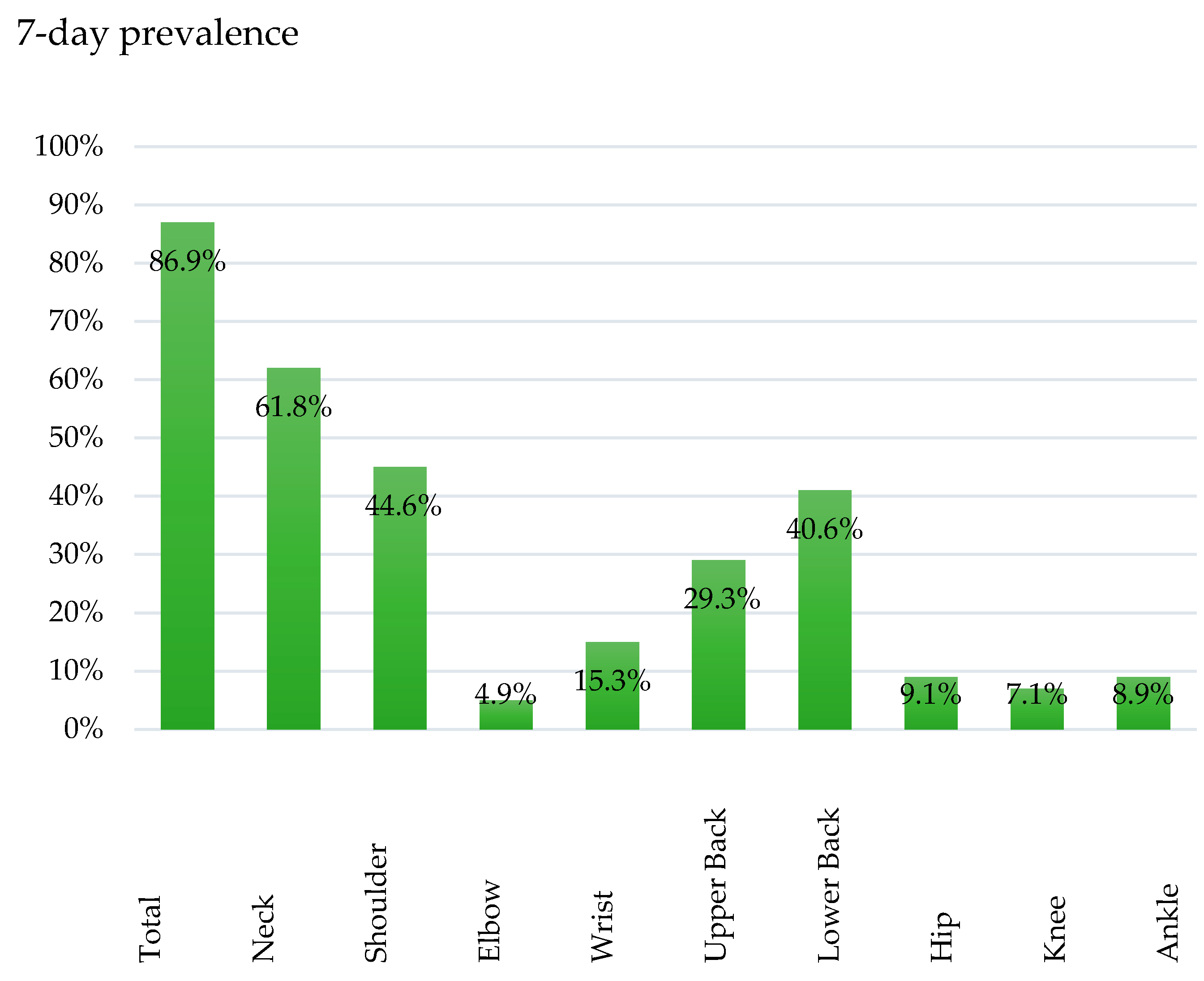
3.3. Prevalence of MSDs
3.4. Prevalence of Specific Medical Conditions
3.5. Correlations between Age/BMI/Height and MSDs
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ohlendorf, D.; Erbe, C.; Hauck, I.; Nowak, J.; Hermanns, I.; Ditchen, D.; Ellegast, R.; Groneberg, D. Kinematic analysis of work-related musculoskeletal loading of trunk among dentists in Germany. BMC Musculoskelet. Disord. 2016, 17, 427. [Google Scholar] [CrossRef]
- Valachi, B.; Valachi, K. Mechanisms leading to musculoskeletal disorders in dentistry. J. Am. Dent. Assoc. 2003, 134, 1344–1350. [Google Scholar] [CrossRef]
- Lietz, J.; Kozak, A.; Nienhaus, A. Prevalence and occupational risk factors of musculoskeletal diseases and pain among dental professionals in western countries: A systematic literature review and meta-analysis. PLoS ONE 2018, 13, e0208628. [Google Scholar] [CrossRef] [PubMed]
- Kiersz, A. The 27 Jobs That Are Most Damaging to Your Health. Business Insider 2015. Available online: https://www.businessinsider.com/the-most-unhealthy-jobs-in-america-2015-11?r=US&IR=T#1-dentists-dental-surgeons-and-dental-assistants-27 (accessed on 29 April 2020).
- Danquah, I.H.; Kloster, S.; Holtermann, A.; Aadahl, M.; Tolstrup, J.S. Effects on musculoskeletal pain from “Take a Stand!”—A cluster-randomized controlled trial reducing sitting time among office workers. Scand. J. Work Environ. Health 2017, 3639, 350–357. [Google Scholar] [CrossRef] [PubMed]
- Naqvi, W.M.; Kulkarni, P.S.; Sumbh, S.J. Mechanisms leading to work related musculoskeletal disorders in dental. Professionals. Pravara Med. Rev. 2008, 3, 35–37. [Google Scholar]
- Nowotny-Czupryna, O.; Czupryna, K.; Skucha-Nowak, M.; Szymanska, J. Spine arrangement during work in sitting position and occurrence of pain among dentists and medical assistants. Med. Pr. 2018, 69, 509–522. [Google Scholar] [CrossRef]
- Ratzon, N.Z.; Yaros, T.; Mizlik, A.; Kanner, T. Musculoskeletal symptoms among dentists in relation to work posture. Work 2000, 15, 153–158. [Google Scholar]
- Feng, B.; Liang, Q.; Wang, Y.; Andersen, L.L.; Szeto, G. Prevalence of work-related musculoskeletal symptoms of the neck and upper extremity among dentists in China. BMJ Open 2014, 4, e006451. [Google Scholar] [CrossRef]
- Brown, J.; Burke, F.J.; Macdonald, E.B.; Gilmour, H.; Hill, K.B.; Morris, A.J.; White, D.A.; Muirhead, E.K.; Murray, K. Dental practitioners and ill health retirement: Causes, outcomes and re-employment. Br. Dent. J. 2010, 209, E7. [Google Scholar] [CrossRef]
- Hoevenaars, J.G. Dentist and disability: A matter of occupational disease? Ned. Tijdschr. Tandheelkd. 2002, 109, 207–211. [Google Scholar]
- Bauer, S.; Bauer, W.; Bethge, M.; Brinkmann, A.; Bullwinkel, S.; Crößmann, A.; Döbler, A.-S.; Eekhoff, A.; Ehses-Flohr, M.; Emmermacher, A.; et al. Arbeit Und gesundheit Generation 50+. Zahlen, Daten, Fakten; BKK Dachverband: Berlin, Germany, 2018. [Google Scholar]
- Marschall, J.H.; Nolting, H.-D.; Burgart, E.; Heil, K.L.; Tisch, T.; Woköck, T. DAK Gesundheitsreport 2019; DAK-Gesundheit: Berlin, Germany, 2019. [Google Scholar]
- Meyer, V.P.; Brehler, R.; Castro, W.H.M.; Nentwig, C.G. Arbeitsbelastungen bei Zahnärzten in Niedergelassener Praxis: Eine Arbeitsmedizinische Bestandsaufnahme Zu Wirbelsäulenbelastungen, Berufsdermatosen Und Stressfaktoren; DÄV-Hanser: Köln, Germany, 2001; p. 167. (In German) [Google Scholar]
- Nokhostin, M.R.; Zafarmand, A.H. Musculoskeletal problem: Its prevalence among Iranian dentists. J. Int. Soc. Prev. Community Dent. 2016, 6, S41–S46. [Google Scholar] [CrossRef] [PubMed]
- Proteau, R.-A. Prevention of Work-Related Musculoskeletal Disorders (MSDs) in Dental Clinics; Asstsas: Montréal, QC, Canada, 2009; pp. 1–104. [Google Scholar]
- Harutunian, K.; Gargallo-Albiol, J.; Figueiredo, R.; Gay-Escoda, C. Ergonomics and musculoskeletal pain among postgraduate students and faculty members of the School of Dentistry of the University of Barcelona (Spain). A cross-sectional study. Med. Oral Patol. Oral Cir. Bucal 2011, 16, 425–429. [Google Scholar] [CrossRef] [PubMed]
- Hodacova, L.; Sustova, Z.; Cermakova, E.; Kapitan, M.; Smejkalova, J. Self-reported risk factors related to the most frequent musculoskeletal complaints among Czech dentists. Ind. Health 2015, 53, 48–55. [Google Scholar] [CrossRef] [PubMed]
- Lindfors, P.; von Thiele, U.; Lundberg, U. Work characteristics and upper extremity disorders in female dental health workers. J. Occup. Health 2006, 48, 192–197. [Google Scholar] [CrossRef]
- Alghadir, A.; Zafar, H.; Iqbal, Z.A. Work-related musculoskeletal disorders among dental professionals in Saudi Arabia. J. Phys. Ther. Sci. 2015, 27, 1107–1112. [Google Scholar] [CrossRef]
- Dajpratham, P.; Ploypetch, T.; Kiattavorncharoen, S.; Boonsiriseth, K. Prevalence and associated. Factors of musculoskeletal pain among the dental personnel in a dental school. J. Med. Assoc. Thai. 2010, 93, 714–721. [Google Scholar]
- Finsen, L.; Christensen, H.; Bakke, M. Musculoskeletal disorders among dentists and variation in dental work. Appl. Ergon. 1998, 29, 119–125. [Google Scholar] [CrossRef]
- Golchha, V.; Sharma, P.; Wadhwa, J.; Yadav, D.; Paul, R. Ergonomic risk factors and their association with musculoskeletal disorders among Indian dentist: A preliminary study using rapid upper limb assessment. Indian J. Dent. Res. 2014, 25, 767–771. [Google Scholar] [CrossRef]
- Hayes, M.; Smith, D.; Cockrell, D. Prevalence and correlates of musculoskeletal disorders among Australian dental hygiene students. Int. J. Dent. Hyg. 2009, 7, 176–181. [Google Scholar] [CrossRef]
- Morse, T.; Bruneau, H.; Dussetschleger, J. Musculoskeletal disorders of the neck and shoulder in the dental professions. Work 2010, 35, 419–429. [Google Scholar] [CrossRef]
- Shrestha, B.P.; Singh, G.K.; Niraula, S.R. Work related complaints among dentists. JNMA J. Nepal Med. Assoc. 2008, 47, 77–81. [Google Scholar] [CrossRef] [PubMed]
- Leiner, D.J. SoSCi Survey (Version 3.1.06). Available online: https://www.soscisurvey.de/ (accessed on 13 May 2020).
- Caffier, G.; Steinberg, U.; Liebers, F. Praxisorientiertes Methodeninventar zur Belastungs—Und Beanspruchungsbeurteilung im Zusammenhang mit arbeitsbedingten Muskel- Skelett-Erkrankungen; Bundesanstalt für Arbeitsschutz und Arbeitsmedizin: Dortmund, 1999; Available online: https://www.baua.de/DE/Angebote/Publikationen/Schriftenreihe/Forschungsberichte/1999/Fb850.pdf?__blob=publicationFile&v=3 (accessed on 29 April 2020).
- Kuorinka, I.; Jonsson, B.; Kilbom, A.; Vinterberg, H.; Biering-Sorensen, F.; Andersson, G.; Jorgensen, K. Standardised nordic questionnaires for the analysis of musculoskeletal symptoms. Appl. Ergon. 1987, 18, 233–237. [Google Scholar] [CrossRef]
- Ayanniyi, O.; Ukpai, B.O.O.; Adeniyi, A.F. Differences in prevalence of self-reported musculoskeletal symptoms among computer and non-computer users in a Nigerian population: A cross-sectional study. BMC Musculoskelet. Disord. 2010, 11, 177. [Google Scholar] [CrossRef] [PubMed]
- Johansson, J.A. Work-related and non-work-related musculoskeletal symptoms. Appl. Ergon. 1994, 25, 248–251. [Google Scholar] [CrossRef]
- Malińska, M.; Bugajska, J. The influence of occupational and non-occupational factors on the prevalence of musculoskeletal complaints in users of portable computers. Int. J. Occup. Saf. Ergon. 2010, 16, 337–343. [Google Scholar] [CrossRef]
- Piranveyseh, P.; Motamedzade, M.; Osatuke, K.; Mohammadfam, I.; Moghimbeigi, A.; Soltanzadeh, A.; Mohammadi, H. Association between psychosocial, organizational and personal factors and prevalence of musculoskeletal disorders in office workers. Int. J. Occup. Saf. Ergon. 2016, 22, 267–273. [Google Scholar] [CrossRef]
- Blåder, S.; Barck-Holst, U.; Danielsson, S.; Ferhm, E.; Kalpamaa, M.; Leijon, M.; Lindh, M.; Markhede, G. Neck and shoulder complaints among sewing-machine operators: A study concerning frequency, symptomatology and dysfunction. Appl. Ergon. 1991, 22, 251–257. [Google Scholar] [CrossRef]
- Chakrabarty, S.; Sarkar, K.; Dev, S.; Das, T.; Mitra, K.; Sahu, S.; Gangopadhyay, S. Impact of rest breaks on musculoskeletal discomfort of Chikan embroiderers of West Bengal, India: A follow up field study. J. Occup. Health 2016, 58, 365–372. [Google Scholar] [CrossRef]
- Nejad, N.H.; Choobineh, A.; Rahimifard, H.; Haidari, H.R.; Tabatabaei, S.H.R. Musculoskeletal risk assessment in small furniture manufacturing workshops. Int. J. Occup. Saf. Ergon. 2013, 19, 275–284. [Google Scholar] [CrossRef]
- Williams, N.R.; Dickinson, C.E. Musculoskeletal complaints in lock assemblers, testers and inspectors. Occup. Med. (Lond.) 1997, 47, 479–484. [Google Scholar] [CrossRef]
- Chanchai, W.; Songkham, W.; Ketsomporn, P.; Sappakitchanchai, P.; Siriwong, W.; Robson, M.G. The impact of an ergonomics intervention on psychosocial factors and musculoskeletal symptoms among Thai Hospital Orderlies. Int. J. Environ. Res. Publ. Health 2016, 13, 464. [Google Scholar] [CrossRef] [PubMed]
- Liss, G.M.; Jesin, E.; Kusiak, R.A.; White, P. Musculoskeletal problems among Ontario dental hygienists. Am. J. Ind. Med. 1995, 28, 521–540. [Google Scholar] [CrossRef] [PubMed]
- Ramadan, P.A.; Ferreira, Jr. Risk factors associated with the reporting of musculoskeletal symptoms in workers at a laboratory of clinical pathology. Ann. Occup. Hyg. 2006, 50, 297–303. [Google Scholar] [CrossRef] [PubMed]
- Shadmehr, A.; Haddad, O.; Azarnia, S.; Sanamlo, Z. Disorders of the musculoskeletal system among Tehran, Iranian dentists. J. Musculoskelet. Pain 2014, 22, 256–259. [Google Scholar] [CrossRef]
- Guo, Q.; Wang, Y.; Xu, D.; Nossent, J.; Pavlos, N.J.; Xu, J. Rheumatoid arthritis: Pathological mechanisms and modern pharmacologic therapies. Bone Res. 2018, 6, 15. [Google Scholar] [CrossRef]
- Solovieva, S.; Vehmas, T.; Riihimäki, H.; Takala, E.-P.; Murtomaa, H.; Luoma, K.; Leino-Arjas, P. Finger osteoarthritis and differences in dental work Tasks. J. Dent. Res. 2006, 85, 344–348. [Google Scholar] [CrossRef]
- Reitemeier, B.J.; Neumann, K.; Schneevoigt, R.; Kleine, J.; Tzscheutschler, C.; Körnig, T. Zahnärztliche Handinstrumente—Ergonomische und hygienische Aspekte Zahnheilkunde Management Kultur (ZMK) 2012. Available online: https://www.zmk-aktuell.de/fachgebiete/hygiene/story/zahnaerztliche-handinstrumente--ergonomische-und-hygienische-aspekte__643.html (accessed on 29 April 2020).
- Assmus, H.; Antoniadis, G.; Bischoff, C. Carpal and cubital tunnel and other, rarer nerve compression syndromes. Dtsch. Arztebl. Int. 2015, 112, 14–25. [Google Scholar] [CrossRef]
- Lake, J. Musculoskeletal dysfunction associated with the practice of dentistry--proposed mechanisms and management: Literature review. Univ. Tor. Dent. J. 1995, 9, 9–11. [Google Scholar]
- De Sio, S.; Traversini, V.; Rinaldo, F.; Colasanti, V.; Buomprisco, G.; Perri, R.; Mormone, F.; La Torre, G.; Guerra, F. Ergonomic risk and preventive measures of musculoskeletal disorders in the dentistry environment: An umbrella review. PeerJ 2018, 6, e4154. [Google Scholar] [CrossRef]
- Valachi, B. Wrist Pian among Dental Professionals. Available online: https://posturedontics.com/identifying-your-wrist-pain-in-dentistry/ (accessed on 11 March 2020).
- Adams, J.E.; Habbu, R. Tendinopathies of the hand and wrist. J. Am. Acad. Orthop. Surg. 2015, 23, 741–750. [Google Scholar] [CrossRef]
- Microsoft Corp. Microsoft Excel for Mac, Version 16.35; Microsoft Corp.: Washington, WA, USA, 2019. [Google Scholar]
- IBM Corp. IBM SPSS Statistics for Mac, Version 26.0; IBM Corp.: New York, NY, USA, 2019. [Google Scholar]
- Berufsbildung, B.-B.F. Neu Abgeschlossene Ausbildungsverträge—Ergebnisse der BIBB-Erhebung; BIBB—Bundesinstitut für Berufsbildung: Bonn, Germany, 2019. [Google Scholar]
- Fillingim, R.B.; King, C.D.; Ribeiro-Dasilva, M.C.; Rahim-Williams, B.; Riley, J.L., III. Sex, gender, and pain: A review of recent clinical and experimental findings. J. Pain 2009, 10, 447–485. [Google Scholar] [CrossRef] [PubMed]
- McGrath, P.A. Psychological aspects of pain perception. Arch. Oral Biol. 1994, 39, 55S–62S. [Google Scholar] [CrossRef]
- Murphy, A.; Berkley, K.; Holdcroft, A. Pain: Sex/gender differences. hormones, brain and behavior online. 2010, 5, 2853–2876. [Google Scholar] [CrossRef]
- Unruh, A.M. Gender variations in clinical pain experience. Pain 1996, 65, 123–167. [Google Scholar] [CrossRef]
- Marshall, E.D.; Duncombe, L.M.; Robinson, R.Q.; Kilbreath, S.L. Musculoskeletal symptoms in New South Wales dentists. Aust. Dent. J. 1997, 42, 240–246. [Google Scholar] [CrossRef]
- RKI. Gesundheitsberichtersteattung des Bundes gemeinsam getragen von RKI und Destatis—Gesundheit in Deutschland; Robert Koch Institut: Berlin, Germany, 2015. (In German) [Google Scholar]
- Steinke, M.B. Präsentismus: Das kann teuer werden. In Die BKK; Bundesanstalt für Arbeitsschutz und Arbeitsmedizin (baua): Dortmund, Berlin, Germany, 2011. [Google Scholar]
- Liebscher, R.B. Verteilung von Schmerz in Deutschland nach Körperregion und Geschlecht im Jahr 2017. Available online: https://de.statista.com/statistik/daten/studie/896807/umfrage/verteilung-von-schmerz-in-deutschland-nach-koerperregion-und-geschlecht/ (accessed on 3 October 2019).
- Nikola Döring, J.B. Forschungsmethoden und Evaluation in den Sozial- und Humanwissenschaften, 5th ed.; Springer: Berlin, Germany, 2016. [Google Scholar]
- Hohwü, L.; Lyshol, H.; Gissler, M.; Jonsson, S.H.; Petzold, M.; Obel, C. Web-based versus traditional paper questionnaires: A mixed-mode survey with a Nordic perspective. J. Med. Internet Res. 2013, 15, e173. [Google Scholar] [CrossRef]
- van Gelder, M.M.; Bretveld, R.W.; Roeleveld, N. Web-based questionnaires: The future in epidemiology? Am. J. Epidemiol. 2010, 172, 1292–1298. [Google Scholar] [CrossRef]
- Decharat, S.; Phethuayluk, P.; Maneelok, S. Prevalence of musculoskeletal symptoms among dental health workers, southern Thailand. Adv. Prev. Med. 2016, 2016, 5494821. [Google Scholar] [CrossRef]
- Thornton, L.J.; Barr, A.E.; Stuart-Buttle, C.; Gaughan, J.P.; Wilson, E.R.; Jackson, A.D.; Wyszynski, T.C.; Smarkola, C. Perceived musculoskeletal symptoms among dental students in the clinic work environment. Ergonomics 2008, 51, 573–586. [Google Scholar] [CrossRef]
- Yi, J.; Hu, X.; Yan, B.; Zheng, W.; Li, Y.; Zhao, Z. High and specialty-related musculoskeletal disorders afflict dental professionals even since early training years. J. Appl. Oral Sci. 2013, 21, 376–382. [Google Scholar] [CrossRef]
| Personal Characteristics | DAs * |
|---|---|
| Sex | |
| Female | 401 (98.8%) |
| Male | 5 (1.2%) |
| Age (Years) | |
| (I50) | 28 (15) |
| Height (cm) | |
| (I50) | 166 (8) |
| Not reported in n (%) | 4 (1.0%) |
| Weight (kg) | |
| (I50) | 66 (18) |
| Not reported in n (%) | 5 (1.2%) |
| BMI (kg/m2) | |
| (I50) | 23.9 (5.8) |
| Not reported in n (%) | 8 (2.0%) |
| Handedness | |
| Right | 377 (92.9%) |
| Left | 29 (7.1%) |
| Work-Related Parameter | Das * |
|---|---|
| Professional group | |
| n (%) | |
| Qualified dental assistant | 322 (79.3) |
| Trainee qualified dental assistant | 84 (20.7) |
| Professional experience in years | |
| (I50) | 8 (15) |
| Not reported in n (%) | 19 (4.7) |
| Total working time by the week in hours | |
| (I50) | 38.5 (8) |
| Not reported in n (%) | 28 (6.9) |
| Treatment time by the week in hours | |
| (I50) | 30 (15) |
| Not reported in n (%) | 35 (8.6) |
| Administrative time by the week in hours | |
| (I50) | 4 (7) |
| Not reported in n (%) | 39 (9.6) |
| Body Regions | Lifetime Prevalence n (%) | 12-Month Prevalence n (%) | 7-Day Prevalence n (%) | |
|---|---|---|---|---|
| Shoulder | Left | 32 (7.9) | 33 (8.1) | 20 (4.9) |
| Right | 82 (20.2) | 86 (21.2) | 55 (13.5) | |
| Both | 211 (52.0) | 176 (43.3) | 106 (26.1) | |
| Elbow | Left | 8 (2.0) | 2 (0.5) | 1 (0.2) |
| Right | 25 (6.2) | 20 (4.9) | 13 (3.2) | |
| Both | 12 (3.0) | 11 (2.7) | 6 (1.5) | |
| Wrist | Left | 15 (3.7) | 13 (3.2) | 5 (1.2) |
| Right | 87 (21.4) | 70 (17.2) | 29 (7.1) | |
| Both | 71 (17.5) | 52 (12.8) | 28 (6.9) | |
| Hip | Left | 9 (2.2) | 10 (2.5) | 8 (2) |
| Right | 22 (5.4) | 20 (4.9) | 10 (2.5) | |
| Both | 41 (10.1) | 33 (8.1) | 19 (4.7) | |
| Knee | Left | 19 (4.7) | 19 (4.7) | 9 (2.2) |
| Right | 20 (4.9) | 22 (5.4) | 10 (2.5) | |
| Both | 43 (10.6) | 29 (7.1) | 10 (2.5) | |
| Ankle | Left | 11 (2.7) | 9 (2.2) | 6 (1.5) |
| Right | 9 (2.2) | 5 (1.2) | 5 (1.2) | |
| Both | 48 (11.8) | 39 (9.6) | 25 (6.2) | |
| Disease | Occurrence n (%) | Occurrence before Start of Profession n (%) | Occurence after Start of Profession n (%) | Occurence after xx Years |
|---|---|---|---|---|
| Total | 140 (34.5) | |||
| Rheumatism | 12 (3.0) | 2 (0.5) | 7 (1.7) | 15 (20) |
| Osteoarthritis | 26 (6.4) | 1 (0.2) | 20 (4.9) | 18 (13) |
| Carpal Tunnel Syndrome | 12 (3.0) | 8 (2.0) | 7 (16) | |
| Disc Prolapse | 51 (12.6) | 2 (0.5) | 31 (7.6) | 12 (15) |
| Tendovaginitis | 46 (11.3) | 8 (2.0) | 24 (5.9) | 4 (7) |
| Flexor Tendovaginitis | 6 (1.5) | 1 (0.2) | 3 (0.7) | 14.5 (19) |
| Cubital Tunnel Syndrome | 1 (0.2) | 0 | 1 (0.2) | 0 |
| Cervical Spine Syndrome | 67 (16.5) | 9 (2.2) | 46 (11.3) | 10 (10) |
| Thoracic Spine Syndrome | 24 (5.9) | 4 (1.0) | 14 (3.4) | 10 (10) |
| Lumbar Spine Syndrome | 54 (13.3) | 3 (0.7) | 33 (8.1) | 10 (12) |
| Correlation Parameter | Age | BMI | Body Height | Body Weight | ||||
|---|---|---|---|---|---|---|---|---|
| Spearman Correlation Coefficient r | p-Value | Spearman Correlation Coefficient r | p-Value | Spearman Correlation Coefficient r | p-Value | Spearman Correlation Coefficient r | p-Value | |
| Specific medical Conditions (in total) | 0.48 | 0.001 * | −0.03 | 0.59 | 0.04 | 0.37 | 0.001 | 0.99 |
| Lifetime prevalence of MSD (in total) | 0.10 | 0.04 * | 0.07 | 0.19 | 0.06 | 0.24 | 0.09 | 0.09 |
| 12-month prevalence of MSD (in total) | 0.05 | 0.37 | 0.08 | 0.12 | 0.10 | 0.04 * | 0.12 | 0.02 * |
| 7-day prevalence of MSD (in total) | −0.01 | 0.88 | −0.03 | 0.55 | 0.12 | 0.04 * | 0.01 | 0.83 |
| Body Regions | Lifetime Prevalence | 12-Month Prevalence | 7-Day Prevalence |
|---|---|---|---|
| Total | 98.5 | 97.5 | 86.9 |
| Neck | 90.9 | 85.2 | 61.8 |
| Shoulder | 80.0 | 70.2 | 44.6 |
| Upper back | 56.9 | 48.0 | 29.3 |
| Lower Back | 68.7 | 60.1 | 40.6 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ohlendorf, D.; Haas, Y.; Naser, A.; Haenel, J.; Maltry, L.; Holzgreve, F.; Erbe, C.; Betz, W.; Wanke, E.M.; Brüggmann, D.; et al. Prevalence of Muscular Skeletal Disorders among Qualified Dental Assistants. Int. J. Environ. Res. Public Health 2020, 17, 3490. https://doi.org/10.3390/ijerph17103490
Ohlendorf D, Haas Y, Naser A, Haenel J, Maltry L, Holzgreve F, Erbe C, Betz W, Wanke EM, Brüggmann D, et al. Prevalence of Muscular Skeletal Disorders among Qualified Dental Assistants. International Journal of Environmental Research and Public Health. 2020; 17(10):3490. https://doi.org/10.3390/ijerph17103490
Chicago/Turabian StyleOhlendorf, Daniela, Yvonne Haas, Antonia Naser, Jasmin Haenel, Laura Maltry, Fabian Holzgreve, Christina Erbe, Werner Betz, Eileen M. Wanke, Dörthe Brüggmann, and et al. 2020. "Prevalence of Muscular Skeletal Disorders among Qualified Dental Assistants" International Journal of Environmental Research and Public Health 17, no. 10: 3490. https://doi.org/10.3390/ijerph17103490
APA StyleOhlendorf, D., Haas, Y., Naser, A., Haenel, J., Maltry, L., Holzgreve, F., Erbe, C., Betz, W., Wanke, E. M., Brüggmann, D., Nienhaus, A., & Groneberg, D. A. (2020). Prevalence of Muscular Skeletal Disorders among Qualified Dental Assistants. International Journal of Environmental Research and Public Health, 17(10), 3490. https://doi.org/10.3390/ijerph17103490







