Dance Fitness Classes Improve the Health-Related Quality of Life in Sedentary Women
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethics Approval and Consent to Participate
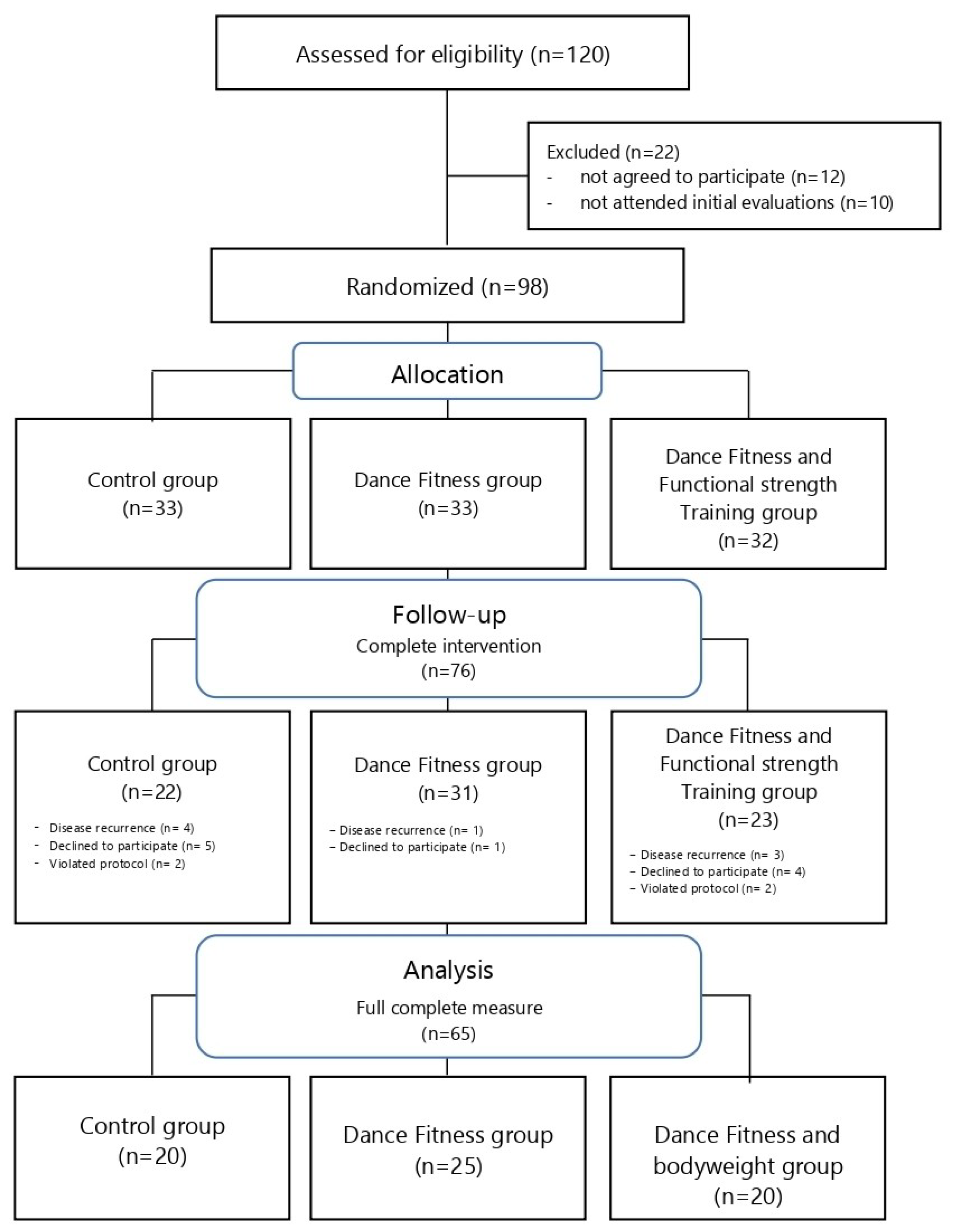
2.2. Participants
2.3. Interventions
2.4. Health-Related Quality of Life
2.5. Statistical Analysis
3. Results
3.1. Changes in HRQoL Dimensions from Baseline to Post-Intervention within the Groups
3.2. Comparisons between Study Groups Post-Intervention
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Llewellyn, C.; Ayers, S.; McManus, C.; Newman, S.P.; Petrie, K.; Revenson, T.; Weinman, J. Cambridge Handbook of Psychology, Health and Medicine; Cambridge University Press: Cambridge, UK, 2019; ISBN 131678326X. [Google Scholar]
- Chai, W.; Nigg, C.R.; Pagano, I.S.; Motl, R.W.; Horwath, C.; Dishman, R.K. Associations of quality of life with physical activity, fruit and vegetable consumption, and physical inactivity in a free living, multiethnic population in Hawaii: A longitudinal study. Int. J. Behav. Nutr. Phys. Act. 2010, 7, 83. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- CDC Applications for Prevention Research: Health-Related Quality of Life (HRQOL). Available online: https://www.cdc.gov/hrqol/index.htm (accessed on 1 December 2019).
- Hand, C. Measuring health-related quality of life in adults with chronic conditions in primary care settings: Critical review of concepts and 3 tools TT—Mesurer la qualité de vie liée à la santé des adultes souffrant de problèmes chroniques en milieux de soins. Can. Fam. Physician 2016, 62, e375–e383. [Google Scholar]
- Kokkonen, K.; Tasmuth, T.; Lehto, J.T.; Kautiainen, H.; Elme, A.; JÄÄSKELÄINEN, A.-S.; Saarto, T. Cancer patients’ symptom burden and health-related quality of life (HRQoL) at tertiary cancer center from 2006 to 2013: A cross-sectional study. Anticancer Res. 2019, 39, 271–277. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Trikkalinou, A.; Papazafiropoulou, A.K.; Melidonis, A. Type 2 diabetes and quality of life. World J. Diabetes 2017, 8, 120. [Google Scholar] [CrossRef]
- Kraai, I.H.; Vermeulen, K.M.; Hillege, H.L.; Jaarsma, T.; Hoekstra, T. Optimism and quality of life in patients with heart failure. Palliat. Support. Care 2018, 16, 725–731. [Google Scholar] [CrossRef] [Green Version]
- Busutil, R.; Espallardo, O.; Torres, A.; Martínez-Galdeano, L.; Zozaya, N.; Hidalgo-Vega, Á. The impact of obesity on health-related quality of life in Spain. Health Qual. Life Outcomes 2017, 15, 197. [Google Scholar] [CrossRef]
- Yao, Q.; Liu, C.; Zhang, Y.; Xu, L. Health-Related Quality of Life of People with Self-Reported Hypertension: A National Cross-Sectional Survey in China. Int. J. Environ. Res. Public Health 2019, 16, 1721. [Google Scholar] [CrossRef] [Green Version]
- Gavilán-Carrera, B.; Garcia da Silva, J.; Vargas-Hitos, J.A.; Sabio, J.M.; Morillas-de-Laguno, P.; Rios-Fernández, R.; Delgado-Fernández, M.; Soriano-Maldonado, A. Association of physical fitness components and health-related quality of life in women with systemic lupus erythematosus with mild disease activity. PLoS ONE 2019, 14, e0212436. [Google Scholar] [CrossRef] [Green Version]
- Nicholl, B.I.; Macfarlane, G.J.; Davies, K.A.; Morriss, R.; Dickens, C.; McBeth, J. Premorbid psychosocial factors are associated with poor health-related quality of life in subjects with new onset of chronic widespread pain—Results from the EPIFUND study. Pain 2009, 141, 119–126. [Google Scholar] [CrossRef] [Green Version]
- Korhonen, P.E.; Seppälä, T.; Järvenpää, S.; Kautiainen, H. Body mass index and health-related quality of life in apparently healthy individuals. Qual. Life Res. 2014, 23, 67–74. [Google Scholar] [CrossRef]
- Brouwer, W.; Meerding, W.-J.; Lamers, L.; Severens, H. The Relationship between Productivity and Health-Related QOL. Pharmacoeconomics 2005, 23, 209–218. [Google Scholar] [CrossRef] [PubMed]
- Anokye, N.K.; Trueman, P.; Green, C.; Pavey, T.G.; Taylor, R.S. Physical activity and health related quality of life. BMC Public Health 2012, 12, 624. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Buder, I.; Zick, C.; Waitzman, N. Health-related quality of life associated with physical activity: New estimates by gender and race and ethnicity. World Med. Health Policy 2016, 8, 409–420. [Google Scholar] [CrossRef]
- Biddle, S. Physical activity and mental health: Evidence is growing. World Psychiatry 2016, 15, 176–177. [Google Scholar] [CrossRef] [Green Version]
- Guthold, R.; Stevens, G.A.; Riley, L.M.; Bull, F.C. Worldwide trends in insufficient physical activity from 2001 to 2016: A pooled analysis of 358 population-based surveys with 19 million participants. Lancet Glob. Health 2018, 6, e1077. [Google Scholar] [CrossRef] [Green Version]
- Church, T.S.; Thomas, D.M.; Tudor-Locke, C.; Katzmarzyk, P.T.; Earnest, C.P.; Rodarte, R.Q.; Martin, C.K.; Blair, S.N.; Bouchard, C. Trends over 5 decades in U.S. occupation-related physical activity and their associations with obesity. PLoS ONE 2011, 6, e19657. [Google Scholar] [CrossRef] [Green Version]
- Edwards, E.S.; Sackett, S.C. Psychosocial Variables Related to Why Women are Less Active than Men and Related Health Implications. Clin. Med. Insights Women’s Health 2016, 9, 47–56. [Google Scholar] [CrossRef] [Green Version]
- WHO Physical Activity Fact-Sheets. Available online: https://www.who.int/en/news-room/fact-sheets/detail/physical-activity (accessed on 1 January 2019).
- Søltoft, F.; Hammer, M.; Kragh, N. The association of body mass index and health-related quality of life in the general population: Data from the 2003 Health Survey of England. Qual. Life Res. 2009, 18, 1293. [Google Scholar] [CrossRef] [Green Version]
- Cla, T. Time to tackle the physical activity gender gap. Health (Irvine. Calif). 2018, 6, e1077-86. [Google Scholar]
- Burke, S.M.; Carron, A.V.; Eys, M.A.; Ntoumanis, N.; Estabrooks, P.A. Group versus individual approach? A meta-analysis of the effectiveness of interventions to promote physical activity. Sport Exerc. Psychol. Rev. 2006, 2, 19–35. [Google Scholar]
- Koch, S.C.; Riege, R.F.F.; Tisborn, K.; Biondo, J.; Martin, L.; Beelmann, A. Effects of Dance Movement Therapy and Dance on Health-Related Psychological Outcomes. A Meta-Analysis Update. Front. Psychol. 2019, 10, 1806. [Google Scholar] [CrossRef] [PubMed]
- Burkhardt, J.; Brennan, C. The effects of recreational dance interventions on the health and well-being of children and young people: A systematic review. Arts Health 2012, 4, 148–161. [Google Scholar] [CrossRef]
- Coaten, R.; Newman-Bluestein, D. Embodiment and Dementia–Dance Movement Psychotherapists. Dementia (London) 2013, 12, 677–681. [Google Scholar] [CrossRef] [Green Version]
- Pratt, R.R. Art, dance, and music therapy. Phys. Med. Rehabil. Clin. 2004, 15, 827–841. [Google Scholar] [CrossRef]
- Fong Yan, A.; Cobley, S.; Chan, C.; Pappas, E.; Nicholson, L.L.; Ward, R.E.; Murdoch, R.E.; Gu, Y.; Trevor, B.L.; Vassallo, A.J.; et al. The Effectiveness of Dance Interventions on Physical Health Outcomes Compared to Other Forms of Physical Activity: A Systematic Review and Meta-Analysis. Sports Med. 2018, 48, 933–951. [Google Scholar] [CrossRef]
- Eys, M.A.; Evans, M.B. Group dynamics in sport, exercise, and physical activity contexts. In Advances in Sport and Exercise Psychology, 4th ed.; Human Kinetics: Champaign, IL, USA, 2018; pp. 171–188. ISBN 1492566993. [Google Scholar]
- Fan, J.X.; Kowaleski-Jones, L.; Wen, M. Walking or dancing: Patterns of physical activity by cross-sectional age among US women. J. Aging Health 2013, 25, 1182–1203. [Google Scholar] [CrossRef] [Green Version]
- IHRSA. The 2019 IHRSA Health Club Consumer Report; Boston, MA, USA. Available online: https://www.ihrsa.org/publications/the-2019-ihrsa-health-club-consumer-report/ (accessed on 1 January 2019).
- Bräuninger, I. The efficacy of dance movement therapy group on improvement of quality of life: A randomized controlled trial. Arts Psychother. 2012, 39, 296–303. [Google Scholar] [CrossRef]
- Barranco-Ruiz, Y.; Mandic, S.; Paz-Viteri, S.; Guerendiain, M.; Sandoval, F.; Villa-González, E. A short dance-exercise intervention as a strategy for improving quality of life in inactive workers. Health Educ. J. 2017, 76. [Google Scholar] [CrossRef]
- Zamuner, A.R.; Moreno, M.A.; Camargo, T.M.; Graetz, J.P.; Rebelo, A.C.; Tamburus, N.Y.; da Silva, E. Assessment of Subjective Perceived Exertion at the Anaerobic Threshold with the Borg CR-10 Scale. J. Sport. Sci. Med. 2011, 10, 130–136. [Google Scholar]
- Alonso, J.; Prieto, L.; Anto, J.M. The Spanish version of the SF-36 Health Survey (the SF-36 health questionnaire): An instrument for measuring clinical results. Med. Clin. (Barc) 1995, 104, 771–776. [Google Scholar] [PubMed]
- Ware, J.E., Jr. SF-36 health survey update. Spine (Phila. Pa. 1976) 2000, 25, 3130–3139. [Google Scholar] [CrossRef] [PubMed]
- Shanahan, J.; Coman, L.; Ryan, F.; Saunders, J.; O’Sullivan, K.; Bhriain, O.N.; Clifford, A.M. To dance or not to dance? A comparison of balance, physical fitness and quality of life in older Irish set dancers and age-matched controls. Public Health 2016, 141, 56–62. [Google Scholar] [CrossRef] [PubMed]
- Connolly, M.K.; Quin, E.; Redding, E. Dance 4 your life: Exploring the health and well-being implications of a contemporary dance intervention for female adolescents. Res. Danc. Educ. 2011, 12, 53–66. [Google Scholar] [CrossRef]
- Duberg, A.; Hagberg, L.; Sunvisson, H.; Möller, M. Influencing self-rated health among adolescent girls with dance intervention: A randomized controlled trial. JAMA Pediatr. 2013, 167, 27–31. [Google Scholar] [CrossRef] [Green Version]
- Mala, A.; Karkou, V.; Meekums, B. Dance/Movement Therapy (D/MT) for depression: A scoping review. Arts Psychother. 2012, 39, 287–295. [Google Scholar] [CrossRef] [Green Version]
- Mandelbaum, R.; Lo, A.C. Examining dance as an intervention in Parkinson’s disease: A systematic review. Am. J. Danc. Ther. 2014, 36, 160–175. [Google Scholar] [CrossRef]
- Kaltsatou, A.; Kouidi, E.; Fountoulakis, K.; Sipka, C.; Theochari, V.; Kandylis, D.; Deligiannis, A. Effects of exercise training with traditional dancing on functional capacity and quality of life in patients with schizophrenia: A randomized controlled study. Clin. Rehabil. 2015, 29, 882–891. [Google Scholar] [CrossRef]
- Domene, P.A.; Moir, H.J.; Pummell, E.; Knox, A.; Easton, C. The health-enhancing efficacy of Zumba® fitness: An 8-week randomised controlled study. J. Sports Sci. 2016, 34, 1396–1404. [Google Scholar] [CrossRef] [Green Version]
- Notarnicola, A.; Maccagnano, G.; Pesce, V.; Tafuri, S.; Leo, N.; Moretti, B. Is the Zumba fitness responsible for low back pain? Musculoskelet. Surg. 2015, 99, 211–216. [Google Scholar] [CrossRef]
- Cugusi, L.; Wilson, B.; Serpe, R.; Medda, A.; Deidda, M.; Gabba, S.; Satta, G.; Chiappori, P.; Mercuro, G. Cardiovascular effects, body composition, quality of life and pain after a Zumba fitness program in Italian overweight women. J. Sports Med. Phys. Fitness 2016, 56, 328–335. [Google Scholar] [PubMed]
- Rossmeissl, A.; Lenk, S.; Hanssen, H.; Donath, L.; Schmidt-Trucksäss, A.; Schäfer, J. ZumBeat: Evaluation of a Zumba Dance Intervention in Postmenopausal Overweight Women. Sports 2016, 4, 5. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Donath, L.; Roth, R.; Hohn, Y.; Zahner, L.; Faude, O. The effects of Zumba training on cardiovascular and neuromuscular function in female college students. Eur. J. Sport Sci. 2014, 14, 569–577. [Google Scholar] [CrossRef] [PubMed]
- Stonnington, C.M.; Krell-Roesch, J.; Locke, D.E.C.; Hentz, J.G.; Dueck, A.C.; Geda, Y.E.; Tariot, P.N.; Caselli, R.J. Impact of Zumba on Cognition and Quality of Life is Independent of APOE4 Carrier Status in Cognitively Unimpaired Older Women: A 6-Month Randomized Controlled Pilot Study. Am. J. Alzheimer’s Dis. Other Dementias 2020, 35, 1533317519868370. [Google Scholar] [CrossRef]
- Assunção Júnior, J.C.; de Almeida Silva, H.J.; da Silva, J.F.C.; da Silva Cruz, R.; de Almeida Lins, C.A.; de Souza, M.C. Zumba dancing can improve the pain and functional capacity in women with fibromyalgia. J. Bodyw. Mov. Ther. 2018, 22, 455–459. [Google Scholar] [CrossRef]
- Vendramin, B.; Bergamin, M.; Gobbo, S.; Cugusi, L.; Duregon, F.; Bullo, V.; Zaccaria, M.; Neunhaeuserer, D.; Ermolao, A. Health benefits of Zumba fitness training: A systematic review. PM&R 2016, 8, 1181–1200. [Google Scholar]
- Chavarrias, M.; Carlos-Vivas, J.; Pérez-Gómez, J. Health benefits of zumba: A systematic review. J. Sport Health Res. 2018, 10, 327–337. [Google Scholar]
- Jha, P.; Khurana, S.; Ali, K.; Ahmad, I.; Verma, S. Effects of concurrent training on physical health and performance. Comp. Exerc. Physiol. 2017, 14, 1–6. [Google Scholar] [CrossRef]
- Chau, J.Y.; Grunseit, A.C.; Chey, T.; Stamatakis, E.; Brown, W.J.; Matthews, C.E.; Bauman, A.E.; van der Ploeg, H.P. Daily sitting time and all-cause mortality: A meta-analysis. PLoS ONE 2013, 8, e80000. [Google Scholar] [CrossRef] [Green Version]
- Barranco-Ruiz, Y.; Villa-González, E. Health-Related Physical Fitness Benefits in Sedentary Women Employees after an Exercise Intervention with Zumba Fitness®. Int. J. Environ. Res. Public Health 2020, 17, 2632. [Google Scholar] [CrossRef] [Green Version]
- Gilbert, M.; Chaubet, P.; Karelis, A.; Dancause, K.N. Perceptions of group exercise courses and instructors among Quebec adults. BMJ Open Sport Exerc. Med. 2017, 3, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Graupensperger, S.; Gottschall, J.S.; Benson, A.J.; Eys, M.; Hastings, B.; Evans, M.B. Perceptions of groupness during fitness classes positively predict recalled perceptions of exertion, enjoyment, and affective valence: An intensive longitudinal investigation. Sport. Exerc. Perform. Psychol. 2019. [Google Scholar] [CrossRef]
- Tarr, B.; Launay, J.; Dunbar, R.I.M. Music and social bonding: “self-other” merging and neurohormonal mechanisms. Front. Psychol. 2014, 5, 1096. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tarr, B.; Launay, J.; Cohen, E.; Dunbar, R. Synchrony and exertion during dance independently raise pain threshold and encourage social bonding. Biol. Lett. 2015, 11, 20150767. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tarr, B.; Launay, J.; Dunbar, R.I.M. Silent disco: Dancing in synchrony leads to elevated pain thresholds and social closeness. Evol. Hum. Behav. 2016, 37, 343–349. [Google Scholar] [CrossRef] [Green Version]
- Boas, A.A.V. Well-Being and Quality of Working Life of University Professors in Brazil Quality of Life and Quality of Working Life; InTech: Rijeka, Croatia, 2017; pp. 187–210. ISBN 9535134450. [Google Scholar]


| Quality of Life Dimensions | Number of Items | Number of Answer Options | Summary of Content and Meaning |
|---|---|---|---|
| General Health (GH) | 5 | 5 | Personal valuation of health including current health, future health prospects, and resistance to illness. |
| Physical Functioning (PF) | 10 | 3 | Extent to which health limits physical activities such as self-care, walking, climbing stairs, bending, picking up or carrying weights, and moderate and intense efforts. |
| Social Functioning (SF) | 2 | 5 | Extent to which physical or emotional health problems interfere with normal social life. |
| Physical Role (PR) | 4 | 2 | Extent to which physical health interferes with work and other daily activities, including less than desired performance, limitation in the type of activities performed, or difficulty in performing activities. |
| Emotional Role (ER) | 3 | 2 | Degree to which emotional problems interfere with work or other daily activities, including reduced time spent on those activities, less than desired performance, and decreased care while working. |
| Bodily Pain (BP) | 2 | 5 | The intensity of pain and its effect on regular work, both outside the home and at home. |
| Vitality (V) | 4 | 6 | Feeling of energy and vitality, compared to the feeling of exhaustion. |
| Mental Health (MH) | 5 | 6 | General mental health, including depression, anxiety, behavioral and emotional control, and the overall positive effect. |
| Declared evolution of health (DEH) | 1 | 5 | Current health assessment compared to a year ago. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barranco-Ruiz, Y.; Paz-Viteri, S.; Villa-González, E. Dance Fitness Classes Improve the Health-Related Quality of Life in Sedentary Women. Int. J. Environ. Res. Public Health 2020, 17, 3771. https://doi.org/10.3390/ijerph17113771
Barranco-Ruiz Y, Paz-Viteri S, Villa-González E. Dance Fitness Classes Improve the Health-Related Quality of Life in Sedentary Women. International Journal of Environmental Research and Public Health. 2020; 17(11):3771. https://doi.org/10.3390/ijerph17113771
Chicago/Turabian StyleBarranco-Ruiz, Yaira, Susana Paz-Viteri, and Emilio Villa-González. 2020. "Dance Fitness Classes Improve the Health-Related Quality of Life in Sedentary Women" International Journal of Environmental Research and Public Health 17, no. 11: 3771. https://doi.org/10.3390/ijerph17113771
APA StyleBarranco-Ruiz, Y., Paz-Viteri, S., & Villa-González, E. (2020). Dance Fitness Classes Improve the Health-Related Quality of Life in Sedentary Women. International Journal of Environmental Research and Public Health, 17(11), 3771. https://doi.org/10.3390/ijerph17113771







