Evaluating Residential Segregation’s Relation to the Clustering of Poor Health across American Cities
Abstract
:1. Introduction
1.1. Social Sources of Poor Health Clusters
1.2. Spatial Character of Racial/Ethnic Segregation
1.3. Racial/Ethnic Segregation’s Health Advantage?
1.4. Hypotheses
2. Materials and Methods
2.1. Dependent Variables
2.2. Spatial Racial/Ethnic Segregation Measures
2.3. Other Independent Predictors
2.4. Methods
3. Results
3.1. Descriptive Results
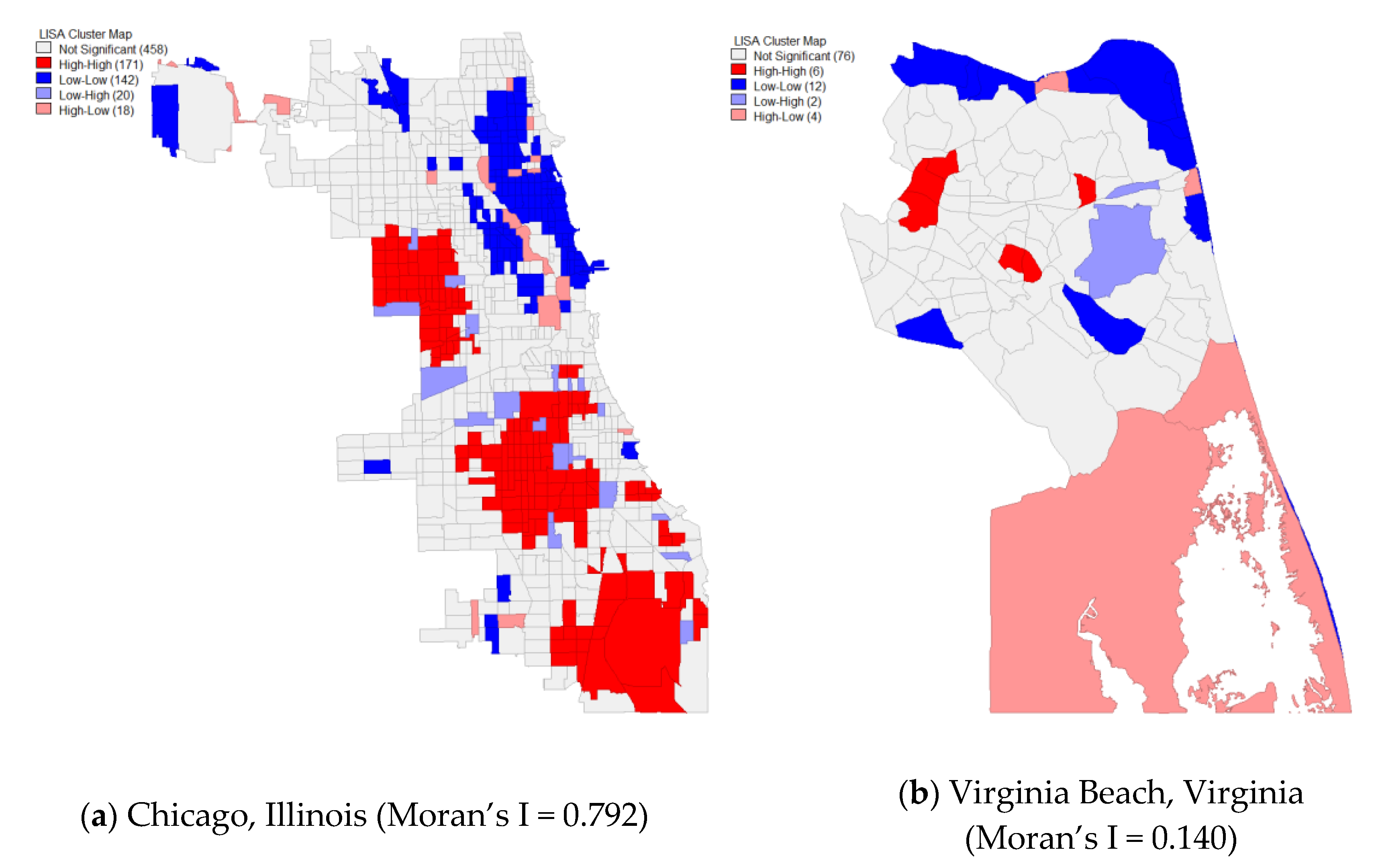
3.2. Exploratory Spatial Data Analysis
3.3. Multivariate Results
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Robert Woods Johnson Foundation. Metro Map: New Orleans, Louisiana—Infographic; Mapping Life Expectancy: Princeton, NJ, USA, 2013. [Google Scholar]
- Jylhä, M. What is self-rated health and why does it predict mortality? Towards a unified conceptual model. Soc. Sci. Med. 2009, 69, 307–316. [Google Scholar] [CrossRef] [PubMed]
- Hill, T.D.; Ross, C.E.; Angel, R.J. Neighborhood disorder, psychophysiological distress, and health. J. Health Soc. Behav. 2005, 46, 170–186. [Google Scholar] [CrossRef] [PubMed]
- Ross, C.E.; Mirowsky, J. Neighborhood disadvantage, disorder, and health. J. Health Soc. Behav. 2001, 258–276. [Google Scholar] [CrossRef] [Green Version]
- Hill, T.D.; Burdette, A.M.; Jokinen-Gordon, H.M.; Brailsford, J.M. Neighborhood disorder, social support, and self-esteem: Evidence from a sample of low-income women living in three cities: Neighborhood disorder, social support, and self-esteem. City Community 2013, 12, 380–395. [Google Scholar] [CrossRef]
- Almgren, G. Health Care Politics, Policy, and Services, Third Edition: A Social Justice Analysis; Springer: New York, NY, USA, 2017. [Google Scholar]
- Grady, S.C. Racial disparities in low birthweight and the contribution of residential segregation: A multilevel analysis. Soc. Sci. Med. 2006, 63, 3013–3029. [Google Scholar] [CrossRef]
- Grady, S.; Darden, J. Spatial Methods to Study Local Racial Residential Segregation and Infant Health in Detroit, Michigan. Ann. Assoc. Am. Geogr. 2012, 102, 922–931. [Google Scholar] [CrossRef]
- Massey, D.S.; Denton, N.A. American Apartheid: Segregation and the Making of the Underclass; Harvard University Press: Cambridge, MA, USA, 1993. [Google Scholar]
- Krysan, M.; Crowder, K. Cycle of Segregation: Social Processes and Residential Stratification; Russell Sage Foundation: New York, NY, USA, 2017. [Google Scholar]
- Denton, N.A.; Massey, D.S. Patterns of Neighborhood Transition in a Multiethnic World: U.S. Metropolitan Areas, 1970–1980. Demography 1991, 28, 41. [Google Scholar] [CrossRef]
- Sugrue, T.J. The Origins of the Urban Crisis: Race and Inequality in Postwar Detroit; Princeton University Press: Princeton, NJ, USA, 1996. [Google Scholar]
- Finch, B.K.; Thomas, K.; Beck, A.N. The Great Recession and adverse birth outcomes: Evidence from California, USA. Ssm - Popul. Health 2019, 9, 100470. [Google Scholar] [CrossRef]
- Sharkey, P. Stuck in Place: Urban Neighborhoods and the End of Progress Toward Racial Equality, 1st ed.; University of Chicago Press: Chicago, IL, USA, 2013. [Google Scholar]
- Acevedo-Garcia, D. Residential segregation and the epidemiology of infectious diseases. Soc. Sci. Med. 2000, 51, 1143–1161. [Google Scholar] [CrossRef]
- Gibbons, J.R.; Yang, T.-C. Self-Rated Health and Residential Segregation: How Does Race/Ethnicity Matter? J. Urban Health 2014, 91, 648–660. [Google Scholar] [CrossRef] [Green Version]
- Kramer, M.R.; Hogue, C.R. Is Segregation Bad for Your Health? Epidemiol. Rev. 2009, 31, 178–194. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Subramanian, S.; Acevedo-Garcia, D.; Osypuk, T.L. Racial residential segregation and geographic heterogeneity in black/white disparity in poor self-rated health in the US: A multilevel statistical analysis. Soc. Sci. Med. 2005, 60, 1667–1679. [Google Scholar] [CrossRef] [PubMed]
- White, K.; Borrell, L.N. Racial/ethnic residential segregation: Framing the context of health risk and health disparities. Health Place 2011, 17, 438–448. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Williams, D.R.; Collins, C. Racial Residential Segregation: A Fundamental Cause of Racial Disparities in Health. Public Health Rep 2001, 116, 404–416. [Google Scholar] [CrossRef]
- Yankauer, A. The relationship of fetal and infant mortality to residential segregation: An inquiry into social epidemiology. Am. Sociol. Rev. 1950, 15, 644–648. [Google Scholar] [CrossRef]
- Lobao, L.M.; Hooks, G.; Tickamyer, A.R. The sociology of spatial inequality; SUNY Press: Albany, NY, USA, 2007. [Google Scholar]
- Massey, D.S.; Denton, N.A. The Dimensions of Residential Segregation. Soc. Forces 1988, 67, 281. [Google Scholar] [CrossRef]
- Reardon, S.F.; O’Sullivan, D. Measures of Spatial Segregation. Sociol. Methodol. 2004, 34, 121–162. [Google Scholar] [CrossRef]
- Biello, K.B.; Ickovics, J.; Niccolai, L.; Lin, H.; Kershaw, T. Racial Differences in Age at First Sexual Intercourse: Residential Racial Segregation and the Black-White Disparity among U.S. Adolescents. Public Health Rep. 2013, 128, 23–32. [Google Scholar] [CrossRef] [Green Version]
- Yang, T.-C.; Zhao, Y.; Song, Q. Residential segregation and racial disparities in self-rated health: How do dimensions of residential segregation matter? Soc. Sci. Res. 2017, 61, 29–42. [Google Scholar] [CrossRef] [Green Version]
- Oka, M.; Wong, D.W.S. Capturing the Two Dimensions of Residential Segregation at the Neighborhood Level for Health Research. Front. Public Health 2014, 2. [Google Scholar] [CrossRef] [Green Version]
- Cromley, E.; McLafferty, S. GIS and Public Health, 2nd ed.; The Guilford Press: New York, NY, USA, 2012; ISBN 978-1-60918-750-7. [Google Scholar]
- Centers for Disease Control and Prevention. 500 Cities: Local Data for Better Health; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2017.
- Krieger, N.; Waterman, P.D.; Spasojevic, J.; Li, W.; Maduro, G.; Van Wye, G. Public Health Monitoring of Privilege and Deprivation With the Index of Concentration at the Extremes. Am. J. Public Health 2016, 106, 256–263. [Google Scholar] [CrossRef] [PubMed]
- Krieger, N.; Waterman, P.D.; Batra, N.; Murphy, J.S.; Dooley, D.P.; Shah, S.N. Measures of Local Segregation for Monitoring Health Inequities by Local Health Departments. Am J Public Health 2017, 107, 903–906. [Google Scholar] [CrossRef] [PubMed]
- Peterson, R.D.; Krivo, L.J. Divergent Social Worlds: Neighborhood Crime and the Racial-Spatial Divide; Russell Sage Foundation: New York, NY, USA, 2010. [Google Scholar]
- Sampson, R.J. Great American city: Chicago and the enduring neighborhood effect; The University of Chicago Press: Chicago, IL, USA; London, UK, 2012; ISBN 978-0-226-73456-9. [Google Scholar]
- Curry, A.; Latkin, C.; Davey-Rothwell, M. Pathways to depression: The impact of neighborhood violent crime on inner-city residents in Baltimore, Maryland, USA. Soc. Sci. Med. 2008, 67, 23–30. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yu, E.; Lippert, A.M. Neighborhood Crime Rate, Weight-Related Behaviors, and Obesity: A Systematic Review of the Literature. Sociol. Compass 2016, 10, 187–207. [Google Scholar] [CrossRef]
- Campbell, E.; Salathé, M. Complex social contagion makes networks more vulnerable to disease outbreaks. Sci. Rep. 2013, 3. [Google Scholar] [CrossRef] [Green Version]
- Dean, L.T.; Subramanian, S.V.; Williams, D.R.; Armstrong, K.; Charles, C.Z.; Kawachi, I. The role of social capital in African–American women’s use of mammography. Soc. Sci. Med. 2014, 104, 148–156. [Google Scholar] [CrossRef] [Green Version]
- Gibbons, J.R.; Schiaffino, M.K. Determining the spatial heterogeneity underlying racial and ethnic differences in timely mammography screening. Int. J. Health Geogr. 2016, 15. [Google Scholar] [CrossRef] [Green Version]
- Wallace, R. Social disintegration and the spread of AIDS: Thresholds for propagation along “sociogeographic” networks. Soc. Sci. Med. 1991, 33, 1155–1162. [Google Scholar] [CrossRef]
- Cooksey-Stowers, K.; Schwartz, M.; Brownell, K. Food Swamps Predict Obesity Rates Better Than Food Deserts in the United States. Int. J. Environ. Res. Public Health 2017, 14, 1366. [Google Scholar] [CrossRef] [Green Version]
- McEntee, J.C.; Ogneva-Himmelberger, Y. Diesel particulate matter, lung cancer, and asthma incidences along major traffic corridors in MA, USA: A GIS analysis. Health Place 2008, 14, 817–828. [Google Scholar] [CrossRef]
- Moody, H.A.; Darden, J.T.; Pigozzi, B.W. The Relationship of Neighborhood Socioeconomic Differences and Racial Residential Segregation to Childhood Blood Lead Levels in Metropolitan Detroit. J. Urban Health 2016, 93, 820–839. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Do, D.P.; Frank, R.; Iceland, J. Black-white metropolitan segregation and self-rated health: Investigating the role of neighborhood poverty. Soc. Sci. Med. 2017, 187, 85–92. [Google Scholar] [CrossRef] [PubMed]
- Hero, J.O.; Zaslavsky, A.M.; Blendon, R.J. The United States Leads Other Nations In Differences By Income In Perceptions Of Health And Health Care. Health Aff. 2017, 36. [Google Scholar] [CrossRef] [PubMed]
- Quillian, L. Segregation and Poverty Concentration The Role of Three Segregations. Am. Sociol. Rev. 2012, 77, 354–379. [Google Scholar] [CrossRef]
- Bullard, R.D. Environmentalism and Social Justice. In Dumping in Dixie: Race, Class, and Environmental Quality; Westview Press: Boulder, CO, USA, 2000. [Google Scholar]
- Moody, H.; Grady, S.C. Lead Emissions and Population Vulnerability in the Detroit (Michigan, USA) Metropolitan Area, 2006–2013: A Spatial and Temporal Analysis. Int. J. Environ. Res. Public Health 2017, 14, 1445. [Google Scholar] [CrossRef] [Green Version]
- Sampson, R.J.; Winter, A.S. The Racial Ecology of Lead Poisoning. Du Bois Rev.: Soc. Sci. Res. Race 2016, 13, 261–283. [Google Scholar] [CrossRef] [Green Version]
- Saunders, M.R.; Lee, H.; Maene, C.; Schuble, T.; Cagney, K.A. Proximity Does Not Equal Access: Racial Disparities in Access to High Quality Dialysis Facilities. J. Racial Ethn. Health Disparities 2014, 1, 291–299. [Google Scholar] [CrossRef]
- Logan, J.R. Separate and Unequal: The Neighborhood Gap for Blacks, Hispanics and Asians in Metropolitan America; US2010; Brown University: Providince, Rhode Island, 2011. [Google Scholar]
- Alexander, D.; Currie, J. Is it who you are or where you live? Residential segregation and racial gaps in childhood asthma. J. Health Econ. 2017, 55, 186–200. [Google Scholar] [CrossRef] [Green Version]
- White, K.; Haas, J.S.; Williams, D.R. Elucidating the Role of Place in Health Care Disparities: The Example of Racial/Ethnic Residential Segregation. Health Serv. Res. 2012, 47, 1278–1299. [Google Scholar] [CrossRef]
- Wilson, W.J. The Truly Disadvantaged: The Inner City, the Underclass, and Public Policy; University of Chicago Press: Chicago, IL, USA, 1987. [Google Scholar]
- Chang, V.W.; Hillier, A.E.; Mehta, N.K. Neighborhood racial isolation, disorder and obesity. Soc. Forces 2009, 87, 2063–2092. [Google Scholar] [CrossRef] [Green Version]
- Tigges, L.M.; Browne, I.; Green, G.P. Social isolation of the urban poor. Sociol. Q. 1998, 39, 53–77. [Google Scholar] [CrossRef]
- Walton, E. Residential segregation and birth weight among racial and ethnic minorities in the United States. J. Health Soc. Behav. 2009, 50, 427–442. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vega, W.A.; Ang, A.; Rodriguez, M.A.; Finch, B.K. Neighborhood protective effects on depression in Latinos. Am. J. Community Psychol. 2011, 47, 114–126. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.; Yi, S.S.; Lundy De La Cruz, N.; Trinh-Shevrin, C. Defining Ethnic Enclave and Its Associations with Self-Reported Health Outcomes Among Asian American Adults in New York City. J. Immigr. Minority Health 2017, 19, 138–146. [Google Scholar] [CrossRef] [Green Version]
- Osypuk, T.L.; Diez Roux, A.V.; Hadley, C.; Kandula, N.R. Are immigrant enclaves healthy places to live? The Multi-ethnic Study of Atherosclerosis. Soc. Sci. Med. 2009, 69, 110–120. [Google Scholar] [CrossRef] [Green Version]
- Bécares, L.; Nazroo, J. Social capital, ethnic density and mental health among ethnic minority people in England: A mixed-methods study. Ethn. Health 2013, 18, 544–562. [Google Scholar] [CrossRef]
- Bécares, L.; Nazroo, J.; Stafford, M. The buffering effects of ethnic density on experienced racism and health. Health Place 2009, 15, 700–708. [Google Scholar] [CrossRef]
- Bécares, L.; Cormack, D.; Harris, R. Ethnic density and area deprivation: Neighbourhood effects on Māori health and racial discrimination in Aotearoa/New Zealand. Soc. Sci. Med. 2013, 88, 76–82. [Google Scholar] [CrossRef]
- Pickett, K.E.; Wilkinson, R.G. People like us: Ethnic group density effects on health. Ethn. Health 2008, 13, 321–334. [Google Scholar] [CrossRef]
- Shaw, R.J.; Pickett, K.E. The association between ethnic density and poor self-rated health among US Black and Hispanic people. Ethn. Health 2011, 16, 225–244. [Google Scholar] [CrossRef]
- Palloni, A.; Arias, E. Paradox lost: Explaining the Hispanic adult mortality advantage. Demography 2004, 41, 385–415. [Google Scholar] [CrossRef] [PubMed]
- Gibbons, J.R.; Yang, T.-C. Connecting Across the Divides of Race/Ethnicity How Does Segregation Matter? Urban Aff. Rev. 2016, 52, 531–558. [Google Scholar] [CrossRef]
- Klinenberg, E. Race, Place, and Vulnerability Urban Neighborhoods and the Ecology of Support. In Heat Wave: A Social Autopsy of Disaster in Chicago; University of Chicago Press: Chicago, IL, USA, 2002. [Google Scholar]
- Marquez, B.; Elder, J.P.; Arredondo, E.M.; Madanat, H.; Ji, M.; Ayala, G.X. Social network characteristics associated with health promoting behaviors among Latinos. Health Psychol. 2014, 33, 544–553. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhou, M. Chinatown: The Socioeconomic Potential of an Urban Enclave; Temple University Press: Philadelphia, PA, USA, 1992. [Google Scholar]
- Brown, S.K. Delayed Spatial Assimilation: Multigenerational Incorporation of the Mexican-Origin Population in Los Angeles. City Community 2007, 6, 193–209. [Google Scholar] [CrossRef]
- Schiaffino, M.K.; Nara, A.; Mao, L. Language Services In Hospitals Vary By Ownership And Location. Health Aff. 2016, 35, 1399–1403. [Google Scholar] [CrossRef] [PubMed]
- Small, M.L. Villa Victoria: The Transformation of Social Capital in a Boston Barrio; University of Chicago Press: Chicago, IL, USA, 2004. [Google Scholar]
- Hunt, M.O.; Wise, L.A.; Jipguep, M.-C.; Cozier, Y.C.; Rosenberg, L. Neighborhood racial composition and perceptions of racial discrimination: Evidence from the Black Women’s Health Study. Soc. Psychol. Q. 2007, 70, 272–289. [Google Scholar] [CrossRef] [Green Version]
- Klinenberg, E. Heat Wave: A Social Autopsy of Disaster in Chicago; University of Chicago Press: Chicago, IL, USA, 2003. [Google Scholar]
- Wibowo, R.A. Harvard Public Health Magazine, Winter 2019; T.H.Chan School of Public Health: Boston, MA, USA, 2019. [Google Scholar]
- Blair, I.V.; Steiner, J.F.; Fairclough, D.L.; Hanratty, R.; Price, D.W.; Hirsh, H.K.; Wright, L.A.; Bronsert, M.; Karimkhani, E.; Magid, D.J.; et al. Clinicians’ Implicit Ethnic/Racial Bias and Perceptions of Care Among Black and Latino Patients. Ann. Fam. Med. 2013, 11, 43–52. [Google Scholar] [CrossRef] [Green Version]
- Wang, Y.; Holt, J.B.; Zhang, X.; Lu, H.; Shah, S.N.; Dooley, D.P.; Matthews, K.A.; Croft, J.B. Comparison of Methods for Estimating Prevalence of Chronic Diseases and Health Behaviors for Small Geographic Areas: Boston Validation Study, 2013. Prev. Chronic Dis. 2017, 14. [Google Scholar] [CrossRef] [Green Version]
- Zhang, X.; Holt, J.B.; Lu, H.; Wheaton, A.G.; Ford, E.S.; Greenlund, K.J.; Croft, J.B. Multilevel Regression and Poststratification for Small-Area Estimation of Population Health Outcomes: A Case Study of Chronic Obstructive Pulmonary Disease Prevalence Using the Behavioral Risk Factor Surveillance System. Am. J. Epidemiol. 2014, 179, 1025–1033. [Google Scholar] [CrossRef] [Green Version]
- Zhang, X.; Holt, J.B.; Yun, S.; Lu, H.; Greenlund, K.J.; Croft, J.B. Validation of Multilevel Regression and Poststratification Methodology for Small Area Estimation of Health Indicators From the Behavioral Risk Factor Surveillance System. Am. J. Epidemiol. 2015, 182, 127–137. [Google Scholar] [CrossRef] [Green Version]
- Center for Disease Control and Prevention. Center for Disease Control Measure Definitions; Center for Disease Control and Prevention: Atlanta, GA, USA, 2017.
- Idler, E.L.; Benyamini, Y. Self-Rated Health and Mortality: A Review of Twenty-Seven Community Studies. J. Health Soc. Behav. 1997, 38, 21. [Google Scholar] [CrossRef] [Green Version]
- Wu, S.; Wang, R.; Zhao, Y.; Ma, X.; Wu, M.; Yan, X.; He, J. The relationship between self-rated health and objective health status: A population-based study. Bmc Public Health 2013, 13, 320. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gibbons, J.R.; Barton, M.S.; Brault, E. Evaluating gentrification’s relation to neighborhood and city health. PLoS ONE 2018, 13, 1–18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, D.-R.; Wen, T.-H. Elucidating the changing socio-spatial dynamics of neighborhood effects on adult obesity risk in Taiwan from 2001 to 2005. Health Place 2010, 16, 1248–1258. [Google Scholar] [CrossRef] [PubMed]
- Hendricks, B.; Mark-Carew, M. Using exploratory data analysis to identify and predict patterns of human Lyme disease case clustering within a multistate region, 2010–2014. Spat. Spatio-Temporal Epidemiol. 2017, 20, 35–43. [Google Scholar] [CrossRef] [PubMed]
- Murray, A.T.; Grubesic, T.H.; Wei, R. Spatially significant cluster detection. Spat. Stat. 2014, 10, 103–116. [Google Scholar] [CrossRef]
- Anselin, L. Local indicators of spatial association—LISA. Geogr. Anal. 1995, 27, 93–115. [Google Scholar] [CrossRef]
- Geary, R.C. The contiguity ratio and statistical mapping. Inc. Stat. 1954, 5, 115–145. [Google Scholar] [CrossRef]
- Getis, A.; Ord, J.K. The Analysis of Spatial Association by Use of Distance Statistics. Geogr. Anal. 1992, 24, 189–206. [Google Scholar] [CrossRef]
- Anselin, L. Spatial Externalities, Spatial Multipliers, And Spatial Econometrics. Int. Reg. Sci. Rev. 2003, 26, 153–166. [Google Scholar] [CrossRef]
- Vogel, M. The Modifiable Areal Unit Problem in Person-Context Research. J. Res. Crime Delinq. 2016, 53, 112–135. [Google Scholar] [CrossRef]
- Hong, S.-Y.; O’Sullivan, D.; Sadahiro, Y. Implementing Spatial Segregation Measures in R. PLoS ONE 2014, 9, e113767. [Google Scholar] [CrossRef]
- Iceland, J.; Weinberg, D.H.; Steinmetz, E. Racial and Ethnic Residential Segregation in the United States 1980–2000; Census 2000; U.S. CENSUS BUREAU: Washington, DC, USA, 2002; p. 151.
- Berkman, L.F.; Kawachi, I.; Glymour, M.M. Social Epidemiology, 2nd ed.; Oxford University Press: New York, NY, USA, 2014. [Google Scholar]
- Boardman, J.D. Stress and physical health: The role of neighborhoods as mediating and moderating mechanisms. Soc. Sci. Med. 2004, 58, 2473–2483. [Google Scholar] [CrossRef] [PubMed]
- Pickett, K.E.; Pearl, M. Multilevel analyses of neighbourhood socioeconomic context and health outcomes: A critical review. J. Epidemiol. Community Health 2001, 55, 111–122. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clogg, C.; Petkova, E.; Haritou, A. Statistical Methods for Comparing Regression Coefficients Between Models. Am. J. Sociol. 1995, 100, 1261–1293. [Google Scholar] [CrossRef]
- Mobley, L.R.; Root, E.D.; Finkelstein, E.A.; Khavjou, O.; Farris, R.P.; Will, J.C. Environment, Obesity, and Cardiovascular Disease Risk in Low-Income Women. Am. J. Prev. Med. 2006, 30, 327–332.e1. [Google Scholar] [CrossRef]
- Grady, S.C.; Ramírez, I.J. Mediating medical risk factors in the residential segregation and low birthweight relationship by race in New York City. Health Place 2008, 14, 661–677. [Google Scholar] [CrossRef]
- John, D.A.; De Castro, A.B.; Martin, D.P.; Duran, B.; Takeuchi, D.T. Does an immigrant health paradox exist among Asian Americans? Associations of nativity and occupational class with self-rated health and mental disorders. Soc. Sci. Med. 2012, 75, 2085–2098. [Google Scholar] [CrossRef] [Green Version]
- Roberto, E. The Divergence Index: A Decomposable Measure of Segregation and Inequality. arXiv 2015, arXiv:1508.01167 [physics, stat]. [Google Scholar]
| Mean | Standard Deviation | Min | Max | ||
|---|---|---|---|---|---|
| Dependent Variable | |||||
| Poor Health Clustering (Queens Weighting) | 0.37 | 0.21 | 0.00 | 0.83 | |
| Independent Variables | |||||
| Spatial Information Theory Index | White/Black | 0.18 | 0.12 | 0.02 | 0.69 |
| White/Hispanic | 0.13 | 0.08 | 0.01 | 0.43 | |
| White/Asian | 0.12 | 0.07 | 0.01 | 0.54 | |
| Spatial Isolation Index | Black/White | 0.32 | 0.25 | 0.01 | 0.96 |
| Hispanic/White | 0.39 | 0.25 | 0.04 | 0.98 | |
| Asian/White | 0.19 | 0.17 | 0.02 | 0.85 | |
| Gini Coefficient | 0.21 | 0.05 | 0.08 | 0.38 | |
| Proportion Foreign-Born | 0.17 | 0.11 | 0.01 | 0.72 | |
| Proportion Female Headed Households | 0.41 | 0.20 | 0.34 | 0.47 | |
| Proportion Residing in Same Housing | 0.29 | 0.05 | 0.14 | 0.50 | |
| Median Age | 35.71 | 3.64 | 25.3 | 47.47 | |
| Proportion Home Owner | 0.57 | 0.11 | 0.19 | 0.85 | |
| Socio-Economic Status | 0.00 | 1.00 | −1.88 | 3.28 | |
| Southern | 0.31 | 0.46 | 0.00 | 1.00 | |
| Western | 0.39 | 0.49 | 0.00 | 1.00 | |
| Midwestern | 0.20 | 0.40 | 0.00 | 1.00 | |
| Total Population | 225,222 | 475,118.9 | 42,342 | 8,341,152 | |
| Primary City | 0.68 | 0.47 | 0.00 | 1.00 | |
| N = 498 | |||||
| Overall | Low-Low Cluster | High-High Cluster | ||||
|---|---|---|---|---|---|---|
| Tract Statistics | Mean | St. Dev. | Mean | St. Dev. | Mean | St. Dev. |
| Proportion Poor Self-Rated Physical Health | 0.13 | 0.04 | 0.08 | 0.02 | 0.18 | 0.03 |
| Proportion Black | 0.20 | 0.27 | 0.08 | 0.12 | 0.35 | 0.35 |
| Proportion White | 0.45 | 0.29 | 0.67 | 0.21 | 0.22 | 0.23 |
| Proportion Asian | 0.06 | 0.10 | 0.08 | 0.10 | 0.03 | 0.08 |
| Proportion Hispanic | 0.23 | 0.24 | 0.12 | 0.15 | 0.34 | 0.32 |
| Proportion Foreign-Born | 0.18 | 0.15 | 0.13 | 0.11 | 0.19 | 0.16 |
| Proportion Female Headed Households | 0.41 | 0.05 | 0.42 | 0.05 | 0.38 | 0.05 |
| Proportion Residing in Same Housing | 0.03 | 0.30 | 0.04 NS | 0.49 | 0.03 NS | 0.05 |
| Proportion Home Owner | 0.51 | 0.24 | 0.61 | 0.24 | 0.39 | 0.18 |
| Socio-Economic Status | 0.00 | 1.69 | −1.61 | 0.93 | 2.03 | 1.54 |
| Tract Population | 4246.23 | 2100.47 | 4551.12 | 2515.77 | 3672.88 | 1722.78 |
| Number of Tracts | 29305 | 3519 | 3690 | |||
| Spatial Information Theory Index | Spatial Isolation Index | |||||
|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | |
| White Black | White Hispanic | White Asian | Black White | Hispanic White | Asian White | |
| Segregation | 0.100 | 0.331 *** | −0.193 | 0.029 | 0.150 ** | –0.210 *** |
| (0.096) | (0.123) | (0.140) | (0.043) | (0.059) | (0.068) | |
| Gini Coeff. | 2.235 *** | 2.101 *** | 2.258 *** | 2.263*** | 2.244 *** | 2.207 *** |
| (0.198) | (0.204) | (0.196) | (0.196) | (0.195) | (0.195) | |
| Proportion Foreign Born | −0.044 | −0.051 | −0.052 | −0.049 | −0.217 ** | 0.142 |
| (0.085) | (0.084) | (0.084) | (0.085) | (0.107) | (0.104) | |
| Proportion Female-Headed Household | −1.556 *** | −1.355 *** | −1.631 *** | −1.619 *** | −1.239 ** | −1.275 ** |
| (0.505) | (0.508) | (0.506) | (0.510) | (0.519) | (0.510) | |
| Proportion Residing in Same Household | −0.426 * | −0.342 | −0.547 ** | −0.443 * | −0.333 | −0.633 *** |
| (0.229) | (0.226) | (0.224) | (0.232) | (0.228) | (0.223) | |
| Median Age | 0.006* | 0.005* | 0.006 * | 0.006* | 0.008 ** | 0.003 |
| (0.003) | (0.003) | (0.003) | (0.003) | (0.003) | (0.003) | |
| SES | −0.004 | −0.003 | 0.006 | −0.003 | −0.014 | −0.003 |
| (0.011) | (0.010) | (0.012) | (0.011) | (0.011) | (0.010) | |
| Home Owner | −0.177 | −0.140 | −0.227 * | −0.195 | −0.201 | −0.238 * |
| (0.139) | (0.136) | (0.134) | (0.138) | (0.133) | (0.133) | |
| Southern | 0.007 | 0.014 | 0.014 | 0.007 | 0.004 | 0.020 |
| (0.033) | (0.032) | (0.032) | (0.034) | (0.032) | (0.032) | |
| Western | 0.058* | 0.064** | 0.053* | 0.058* | 0.046 | 0.076** |
| (0.030) | (0.030) | (0.030) | (0.030) | (0.030) | (0.031) | |
| Mid Western | 0.053 | 0.060 * | 0.060* | 0.055* | 0.065 ** | 0.069** |
| (0.033) | (0.032) | (0.033) | (0.033) | (0.033) | (0.033) | |
| Total Population (logged) | 0.089 *** | 0.082*** | 0.100 *** | 0.093 *** | 0.088*** | 0.103*** |
| (0.014) | (0.013) | (0.013) | (0.013) | (0.013) | (0.013) | |
| Primary City | −0.031 | −0.033 * | −0.028 | −0.029 | −0.026 | −0.023 |
| (0.019) | (0.019) | (0.019) | (0.019) | (0.019) | (0.019) | |
| Constant | −0.504 * | −0.541 ** | −0.528 * | −0.535 ** | −0.728 *** | −0.596 ** |
| (0.274) | (0.270) | (0.271) | (0.272) | (0.280) | (0.270) | |
| Adjusted R2 | 0.453 | 0.460 | 0.454 | 0.452 | 0.459 | 0.462 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gibbons, J.; Yang, T.-C.; Brault, E.; Barton, M. Evaluating Residential Segregation’s Relation to the Clustering of Poor Health across American Cities. Int. J. Environ. Res. Public Health 2020, 17, 3910. https://doi.org/10.3390/ijerph17113910
Gibbons J, Yang T-C, Brault E, Barton M. Evaluating Residential Segregation’s Relation to the Clustering of Poor Health across American Cities. International Journal of Environmental Research and Public Health. 2020; 17(11):3910. https://doi.org/10.3390/ijerph17113910
Chicago/Turabian StyleGibbons, Joseph, Tse-Chuan Yang, Elizabeth Brault, and Michael Barton. 2020. "Evaluating Residential Segregation’s Relation to the Clustering of Poor Health across American Cities" International Journal of Environmental Research and Public Health 17, no. 11: 3910. https://doi.org/10.3390/ijerph17113910
APA StyleGibbons, J., Yang, T.-C., Brault, E., & Barton, M. (2020). Evaluating Residential Segregation’s Relation to the Clustering of Poor Health across American Cities. International Journal of Environmental Research and Public Health, 17(11), 3910. https://doi.org/10.3390/ijerph17113910






