1. Introduction
Evidence supports the utility of abdominal massage (AM) and electrical stimulation (ES) in the treatment of functional constipation (FC) [
1,
2,
3,
4]. While manual lymph drainage (MLD) may be beneficial by promoting normal peristalsis and autonomic nervous system balance, ANS balance, these effects have not been previously investigated.
Functional constipation is described as difficult, incomplete and prolonged passage of dry, hardened stools through the bowel [
5,
6]. Symptoms include pain, abdominal distension, rectal fullness and strain during defecation [
6,
7,
8]. The incidence ranges from 2–28% and varies by region, age and gender and pathologic, behavioral and psychological factors [
9]. It is 2.2 times more prevalent among women than men, and occurs more frequently among elderly than younger people [
10]. When FC becomes chronic, individuals risk developing physical, mental and social disorders. Physical disorders include hemorrhoids, hernias, anal fissures, colonic muscle fiber laxity, colonic wall thickening and prolapse and headaches [
11]. Referred pain may occur when a bolus of hard feces compresses the left iliopsoas muscle and activates myofascial trigger points [
11]. Mental and social changes include fatigue, loss of appetite and reductions in social, leisure and work activities diminish the person’s quality of life [
12,
13].
Constipation may be organic or functional [
14]. Organic constipation occurs from pathologic conditions like neoplasms, partial intestinal obstructions, spinal cord compression, metabolic and neurological diseases and pharmacological interventions. Organic constipation often requires medical or pharmacologic management [
14,
15]. Functional constipation, termed idiopathic, is associated with environmental or behavioral factors like inadequate water or fiber consumption, reduced physical activity or exercise pattern changes and mental stress [
14]. Neuromuscular dysfunction of the defecation unit can lead to disordered or difficult defecation as a cause of FC [
16]. General treatments for FC include non-pharmaceuticals, pharmaceuticals and surgery. Non-pharmaceutical therapy includes lifestyle adjustments that promote good health habits to facilitate defecation such as dietary changes like increasing fiber and water consumption [
17,
18,
19]. Other non-pharmacologic approaches include reflex-therapy, biofeedback, massage, translumbar and transsacral magnetic stimulation–induced motor evoked potentials and electrical stimulation [
20,
21,
22]. When FC becomes chronic, like OC, it may require pharmacologic interventions [
23]. Pharmaceuticals mitigate symptoms, however once discontinued, FC tends to recur [
24]. Further, prolonged pharmaceutical usage may aggravate constipation and cause side-effects like fecal impaction and bowel perforation [
25]. Long-term pharmaceutical use may prevent the biome from cleaning toxins from the colon which increase colorectal cancer risk [
26]. Surgery is used in rare cases and is not a routine treatment [
27]. Thus, non-pharmaceutical treatments are safe and most preferred, with AM and ES the most prevalent.
Abdominal massage was used for several centuries to treat constipation [
1,
28]. It was popular in the early 20th century and a key component in PT curricula in many countries until its use declined by the 1950s. Interest in AM rose again in oncology and hospice and palliative care environments, due to fewer side effects than from other treatments [
29]. abdominal massage is a professional massage that directly stimulates the digestive tract by increasing intra-abdominal pressures and bowel activity [
30]. This induces rectal muscle waves that stimulate the somato-autonomic reflex and bowel sensation to promote rectal loading and peristalsis [
31]. abdominal massage improves FC among the elderly and individuals with multiple sclerosis, spinal cord injuries and profound disability [
12,
28,
32,
33]. However, AM effects remain controversial due to variations in treatment durations, pressures and patient characteristics and receptivity.
Evidence suggests ES improves FC; however, its mechanisms of action is unknown. Transcutaneous Electrical Nerve Stimulation (TENS) and Interferential Current (IFC) therapy are theorized to send targeted electrical currents to spinal ganglion areas that regulate peristalsis to accelerate colonic transit and increase antegrade contraction frequency [
5,
34,
35,
36]. Using ES over bowel tissues may cause reflex inhibition of Sympathetic Nervous System (SNS) activity that inhibits bowel mobility and motility [
35]. However, further study is required to determine ES mechanisms of action and optimal dosing parameters for various colonic diseases.
There are no current studies on the use of MLD for FC. The Vodder MLD technique was developed by a PT to facilitate lymphatic flow [
37]. Currently, MLD is used to treat lymphedema following cancer treatments and to reduce pain and alleviate edema caused by venous diseases, surgery, primary lymphedema and trauma [
5,
37,
38,
39,
40]. The MLD facilitates absorption of interstitial fluid into the lymph capillaries and lymphatic circulation. It also improves ANS balance by increasing Parasympathetic Nervous System (PNS) activity, which reduces physiologic stress and restores homeostasis [
37]. Increased PNS activity promotes relaxation of intestinal sphincter muscles and accelerates peristalsis which can relieve FC [
41,
42,
43]. An ANS imbalance is found with chronic Irritable Bowel Syndrome (IBS) which induces constipation or diarrhea [
44,
45]. The abdominal application of MLD is theorized to mitigate constipation by directly stimulating the bowel, presumably by reducing SNS activity, increasing PNS activity and restoring ANS balance. This treatment may relieve constipation and prevent recurrences since MLD provides direct stimulation to the bowel to promote motility and it may improve ANS balance [
46,
47,
48]. Therefore, this study first investigated the effects of abdominal MLD on ANS balance, anxiety and stress and bowel movement frequency (BMF) and time–duration (BMT), then compared the outcomes to AM and ES. The study provides preliminary guidance to PTs on the use of MLD, AM and ES for managing FC and recommendations for future studies on these interventions.
4. Discussion
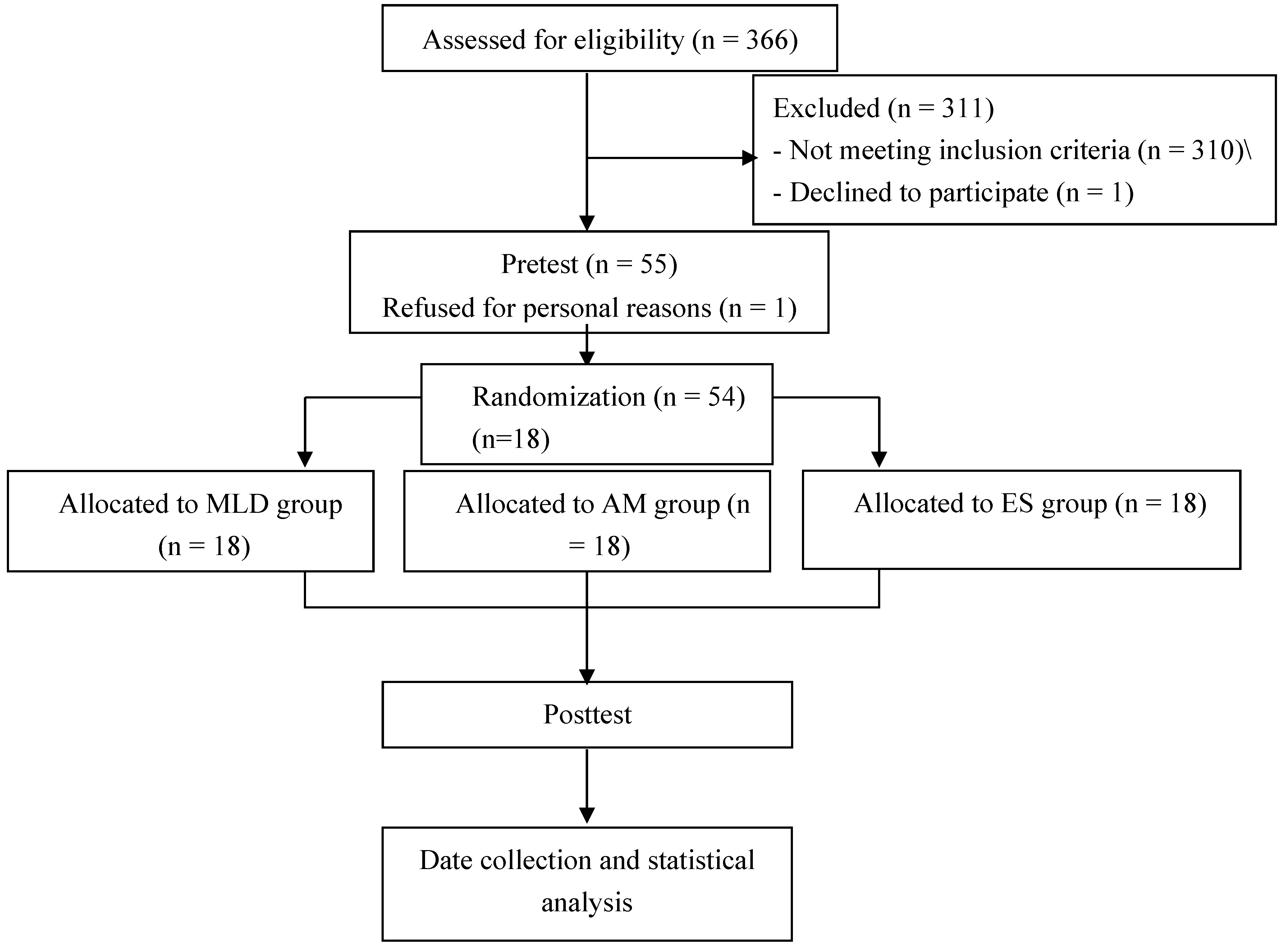
This single-blind randomized controlled study examined the effects of MLD on FC by measuring changes in ANS balance, anxiety and stress and bowel movement frequency and time–duration. The MLD outcomes were then compared to those of AM and ES. The effects of AM and ES on FC were previously studied independently, which did not allow direct comparisons of their outcomes. No prior studies were found that scientifically examined the effects of MLD on FC. However, it was theorized that MLD would improve FC since it could be performed on the abdomen and because it may normalize ANS balance to promote improved gastrointestinal function. This study was performed on college-aged adults in their 20s with FC symptoms.
Participants were age and gender matched, then randomly assigned to one of the three interventions. The study design used pre-and post-intervention measures which allowed direct comparisons of outcomes between the three interventions.
The ANS mediates bidirectional brain–gut interactions [
31,
47]. Therefore, methods that improve ANS balance may restore or normalize intestinal function [
31,
47]. While no studies were found that reported ANS measures for college-aged students with FC, there is evidence that individuals with IBS-C exhibit an ANS imbalance from increased SNS activity and decreased PNS function [
65,
66]. The ANS balance in this study was assessed using HRV measures of TP, HFnu, LFnu and LF/HF ratios, which are valid and reliable measures [
67,
68]. In only the MLD group, TP improved significantly and clinically representing improved ANS balance. The LFnu, HFnu and LF/HF ratios improved significantly and clinically in the MLD and AM groups, while only LFnu improved in the ES group. Since people with IBS have reductions in the ANS balance, these improvements can be interpreted overall as a positive outcome [
67]. Overall, the MLD group had significantly higher improvements in TP than the AMA and ES groups, and larger, but not statistically significant improvements, for HFnu, LFnu and LF/HF ratios compared with AM or ES. These results are the first to imply MLD better improved PNS activity and overall ANS balance compared to the other treatments.
The improved outcomes for MLD compared to AM on ANS measures may be due to differences between the protocol methods. First, MLD begins at the neck, in the area over the vagus nerve, then it proceeds to the descending colon and finally, is performed over the ascending and transverse colon [
37]. Thus, beginning treatment over the vagus nerve may initiate or enhance ANS activity prior to beginning MLD over the abdomen. Second, the gentle pressures used to the dermis over the abdomen during MLD may not cause abdominal or thoracic cavity pressure changes like the moderate pressures used in AM. However, the subjects actively engage in deep breathing during abdominal MLD which may internally stimulate abdominal and thoracic cavity pressure changes to promote colonic motility and peristalsis. Thus, the combination of vagus nerve stimulation and the subject’s deep breathing during MLD abdominal procedures, may provide the superior changes in ANS balance.
Gastrointestinal (GI) functions are influenced by PNS activity, and stimulation of the PNS through MLD, AM and ES are believed to provide FC relief by increasing intestinal motility and digestive secretions and relaxing GI canal sphincters [
69]. Since MLD and AM are direct-types of therapy designed specifically to target the digestive tract, this may explain why they had better effects than ES on most study measures [
30]. Alternatively, ES provides indirect stimulation and further study is required to determine its mechanisms of action and optimal dosing for frequency, waveform, site, intensity and treatment durations in various populations.
Although, not previously studied among college-aged adults with FC, anxiety and mental stress contribute to pathogenic factors that trigger and maintain GI symptoms in people with IBS [
70,
71,
72]. The STAI anxiety measures improved slightly following each intervention, but changes were not significant either within or between groups. While reductions in anxiety were highest from MLD compared to AM or ES, all pre-and post-measures remained in the “mildly high state” anxiety category. The lack of statistical significance between groups may require more sensitive measurement tools, longer treatments durations and follow-up times or a larger sample. Alternatively, changes in SRI stress measures were statistically higher within all groups, but not significantly different between groups. These results suggest that all interventions produced sufficient comfort and relaxation to reduce psychological stress among people with FC [
13]. These interventions may increase the body’s vitality by improving homeostasis and elevating PNS activity. Since the PNS contains approximately 80% of sensory fibers, this increase in feelings of well-being may indirectly contribute to positive psychological changes.
For the bowel movement journal entries, MLD and AM groups had statistically significant increases in BMF, and all three groups had significant increases in BMT. However, between group differences were again not significant possibly due to the small sample. Although not previously studied, MLD was found in this study to significantly improved BMF and BMT which is associated with reduced constipation. Although, effects of AM and ES on BMF and BMT were extensively studied, the results remain controversial as some studies found positive outcomes while others did not [
2,
12,
32,
33,
73]. Hence, more controlled trials are required to determine the effects of AM and ES for various colon diseases in different populations. For adults in their 20s with FC, this study found that AM was effective on both BMF and BMD, while ES was effective on BMF alone.
Abdominal massage effects on FC are controversial. Kim et al. reported constipation was reduced after 10 days among older people, whereas another study reported it was not effective even after 4 weeks of treatment [
54,
74]. However, in the current study, a four-day-a-week, four-week intervention was found effective for constipation relief. Both MLD and AM are considered direct stimulation methods, although MLD uses light pressure to the dermis over the abdomen, while AM uses moderate pressure to the abdomen. Both techniques are thought to move stool manually along the digestive tract and to increase intestinal motility by stimulating the somato-autonomic reflex that mitigates tension, thereby alleviating constipation [
75]. Previous studies also found that AM with both light and moderate pressures was effective [
13,
28,
33,
54,
74].
The study initially examined the primary measures independently, but ANS activity and psychological factors appear to have related and coordinated effects on bowel movement factors. First, the ANS links the central nervous system and gut, and ANS dysfunction alters normal bowel habits [
45,
61]. In addition, anxiety and mental stress contribute to elevated cortisol concentrations which advance insulin resistance to hyperinsulinemia, and insulin promotes SNS activity [
76,
77]. Evidence finds that IBS-C is associated with elevated insulin levels and activation of SNS activity which affects bowel movement characteristics [
78]. Additionally, chronic or excessive stress induces chronic vagal suppression which increases SNS activity [
70]. Therefore, the study also examined correlations between overall ANS improvements with anxiety, stress and with BMF and BMT following the interventions.
Increases in HFnu, signifying increased PNS activity, significantly correlated with reductions in stress, anxiety and BMT and with increased BMF. Reductions in the LF/HF ratio, signifying improved ANS Balance, significantly correlated with reductions in BMT, stress and anxiety and increased BMF. The shorter BMT significantly correlated with lower stress and anxiety and increased BMF. Like previous studies, the present study supports correlations between increased PNS activity and lower constipation and anxiety [
79,
80]. The elevated HFnu, signifying lower SNS activity and the reduced LF/HF ratio following MLD, AM—and to a lesser extent ES—support an increase in PNS activity and restoration of ANS balance. These results support ANS improvements from the study interventions were ultimately correlated with improvements in stress and anxiety and mitigation of constipation symptoms.
This study limitations include: the small sample size which may have contributed to the lack of statistical significance for between groups measures; There was a known wide variability and ambiguity in each individual’s definition of constipation and loose stools; FC occurs more frequently among women, however both men and women were included in this study, so a future study of men and women separately would provide better generalizability; and it was not possible to determine any short or long-term outcomes from the treatments since the final measures were taken one week after the interventions. Therefore, based on study findings, future studies may wish to examine differences between genders, ages, longer treatment durations, short and long-term treatment effects and individuals with various colon diseases. Future studies could also examine the effects of combining these interventions to determine if there are earlier effects or longer lasting improvements.