Is China Moving toward Healthy Aging? A Tracking Study Based on 5 Phases of CLHLS Data
Abstract
:1. Introduction
2. Literature Review
3. Study Design
3.1. Data
3.2. Health Dimensions and Measurement Indicators
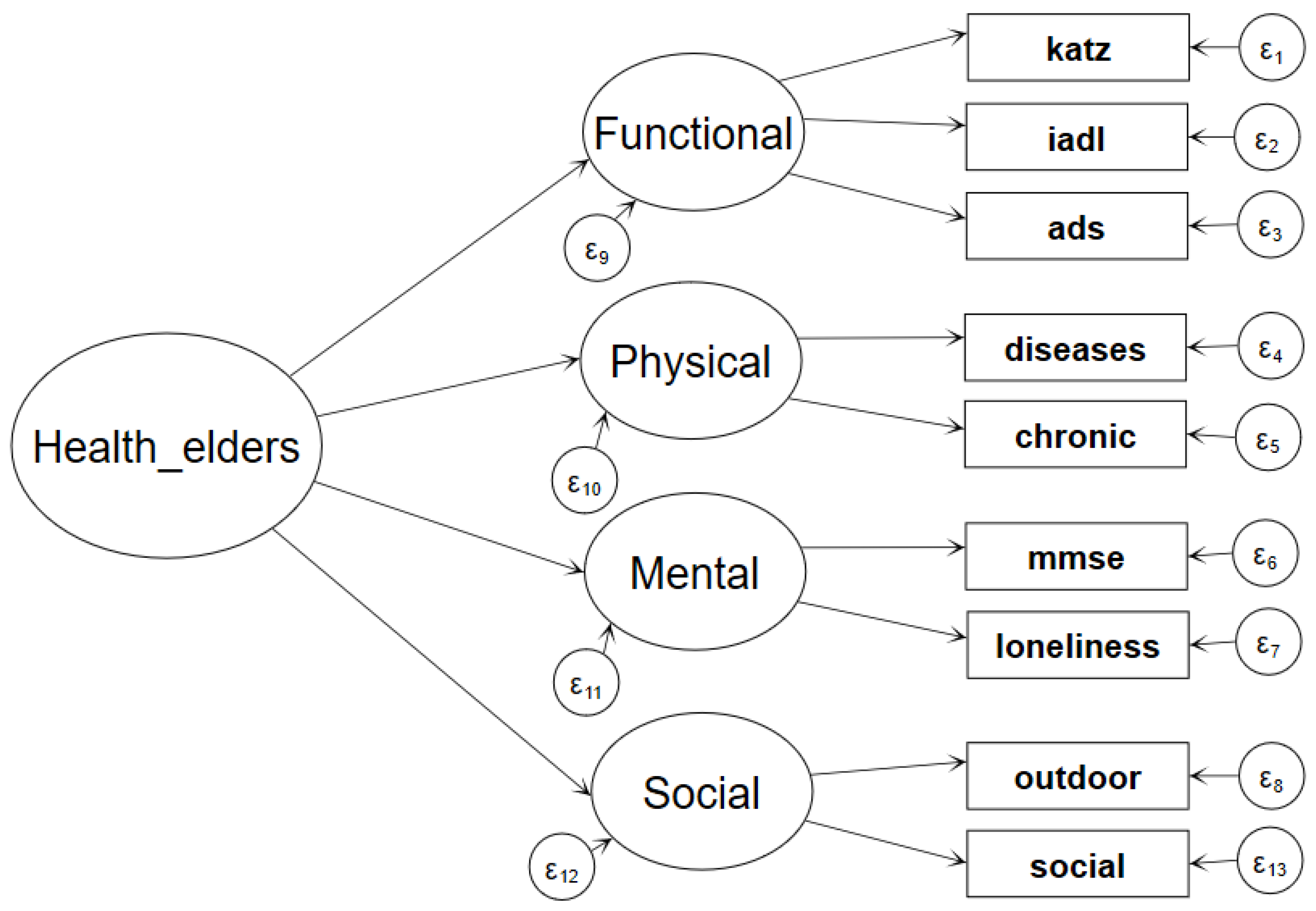
3.3. Measurement Model and Method
3.3.1. Second-Order Factor Model
3.3.2. Significance Test of the Latent Variable’s Mean Difference Using a Multiple-Group Comparison Sturctural Equaiton Modeling
4. Empirical Results
4.1. Descriptive Results
4.2. Second-Order Factor Model Estimation Results
4.3. SEM’s Multiple-Period Comparison Test Results
4.4. Further Subgroup Results
5. Discussion
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Wu, C.; Jiang, X. On the strategy of healthy aging. China Soc. Sci. 1996, 5, 52–64. [Google Scholar]
- Britta, B.; Anjana, B.; Abou, T.H.; Javier, V.; Rebekah, T. The Right to Health of Older People. Gerontologist 2016, 56 (Suppl. 2), S206–S217. [Google Scholar]
- Havighurst, R.J. Successful Aging. Gerontologist 1961, 1, 8–13. [Google Scholar] [CrossRef]
- WHO. World Report on Aging and Health; WHO Press: Geneva, Switzerland, 2016. [Google Scholar]
- Rao, K. Research on healthy aging and elderly health support system. Chin. J. Health Manag. 2013, 7, 149–150. [Google Scholar]
- Chen, X.; Smith, J.; Strauss, J.; Wang, Y.; Zhao, Y. China Health and Retirement Longitudinal Study (CHARLS); National School of Development, Peking University: Beijing, China, 2017. [Google Scholar]
- Liu, L. China Geriatric Health Research Report (2018); Social Sciences Literature Press: Beijing, China, 2019. [Google Scholar]
- Wang, X. Review and Prospect of research on healthy aging. Popul. Res. 1996, 3, 71–75. [Google Scholar]
- Gu, L.; Qiao, X. Analysis of the influencing factors of the self-assessment of the health of the elderly in China. J. Popul. 2006, 5, 27–31. [Google Scholar]
- Guo, W. The change of self-care life expectancy of the elderly in China. Popul. Dev. 2013, 40, 66–74. [Google Scholar]
- Li, C.; Liu, H.; Liang, Y.; Wang, H.; Li, Q. International comparison of healthy life expectancy and prediction of healthy life expectancy in China. China Popul. Sci. 2018, 1, 5–17. [Google Scholar]
- Zhe, T.; Xiang, M.; Fang, X. Healthy life expectancy and its changes of the elderly in Beijing. Chin. J. Epidemiol. 2005, 12, 767–771. [Google Scholar]
- Zhang, W.; Du, P. Regional Disparity in Healthy Life Expectancy for the Chinese Elderly: Expansion or Compression. Popul. Res. 2009, 33, 25–34. [Google Scholar]
- Zeng, Y.; Feng, Q. Trends of Disability and Mortality among the Oldest-Old in China. Popul. Res. 2017, 41, 22–32. [Google Scholar]
- Yu, Y.; Feng, J. The dynamic change of China’s elderly health and its implications for healthy aging. World Econ. Lit. 2017, 000, 1–16. [Google Scholar]
- Song, Y. Comprehensive Assessment of the Elderly, 2nd ed.; China Union Medical University Press: Beijing, China, 2019. [Google Scholar]
- Kenneth Rockwood, A.B.M.; MacKnight, C. Some mathematical models of frailty and their clinical implications. Rev. Clin. Gerontol. 2002, 12, 109–117. [Google Scholar] [CrossRef]
- Jiao, K. Health Status and Social Economic Factors of the Elderly; World Book Publishing Company: Cleveland, NY, USA, 2014. [Google Scholar]
- Rowe, J.W.; Kahn, R.L. Successful aging. Aging 1997, 10, 142. [Google Scholar]
- Baltes, P.B.; Lindenberger, U. Emergence of a powerful connection between sensory and cognitive functions across the adult life span: A new window to the study of cognitive aging? Psychol. Aging 1997, 12, 12–21. [Google Scholar] [CrossRef]
- WHO. Global Strategy on People-Centered and Integrated Health Services; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Gagnon, M.P.; Beogo, I.; Buyl, R. e-Health Interventions for Healthy Aging: A Systematic Review Protocol. Stud. Health Technol. Inform. 2016, 225, 954–955. [Google Scholar]
- Bowling, A.; Dieppe, P. What is successful ageing and who should define it? BMJ Br. Med. J. 2005, 331, 1548–1551. [Google Scholar] [CrossRef] [Green Version]
- Du, P.; Dong, T. Promoting healthy aging: Concept change and policy innovation. Sci. Res. Aging 2015, 12, 3–10. [Google Scholar]
- Wen, Y. Research on the Development Strategy of Healthy Aging; Shanghai Science and Technology Press: Shanghai, China, 2017. [Google Scholar]
- Wu, C. The Scientific and Social Significance of Healthy Aging, in Achieving Healthy Aging, Edited by China Society of Gerontology; China Labor Press: Beijing, China, 1995. [Google Scholar]
- Xiong, B.; Dong, Z. Healthy aging: The golden autumn project across the century. Med. Soc. 1995, 2, 18–22. [Google Scholar]
- Zhong, J.; Chen, Y. A preliminary analysis of the healthy life expectancy of some urban residents. Med. Soc. 1998, 4, 209–211. [Google Scholar]
- Feng, Y. Aging and Global Health; People’s Health Press: Beijing, China, 2018. [Google Scholar]
- Zheng, X. Health Evaluation of Aging Population in China. J. Peking Univ. 2000, 37, 144–151. [Google Scholar]
- Phelan, J.C.; Link, B.G.; Diez-Roux, A.; Kawachi, I.; Levin, B. Fundamental Causes of Social Inequalities in Mortality: A Test of the Theory. J. Health Soc. Behav. 2004, 45, 265–285. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Jia, H. Research on national social health measurement and its influencing factors—Empirical Evidence Based on mimic structural equation model. China Health Policy Res. 2018, 1, 28–36. [Google Scholar]
- Varshney, R.K.; Chabane, K.; Hendre, P.S.; Aggarwal, R.K.; Graner, A. Comparative assessment of EST-SSR, EST-SNP and AFLP markers for evaluation of genetic diversity and conservation of genetic resources using wild, cultivated and elite barleys. Plant Sci. 2007, 173, 638–649. [Google Scholar] [CrossRef] [Green Version]
- Thanakwang, K.; Soonthorndhada, K. Mechanisms by Which Social Support Networks Influence Healthy Aging Among Thai Community-Dwelling Elderly. J. Aging Health 2011, 23, 1352–1378. [Google Scholar] [CrossRef] [PubMed]
- Qiang, L.; Zhe, T. Application of multi state life table method in the study of healthy life expectancy of the elderly. China Popul. Sci. 2002, 1, 40–48. [Google Scholar]
- Wu, C. Some Thoughts on methodology of research on healthy aging. China Popul. Sci. 2001, s1, 101–106. [Google Scholar]
- Wu, Y.; Dang, J. China Report of the Development on Aging Cause; Social Sciences Academic Press: Beijing, China, 2013. [Google Scholar]
- Qian, J. Measurement research on four dimensions of social effects of healthy aging of the elderly population in China. Sci. Res. Aging 2013, 1, 75–81. [Google Scholar]
- Smith, J.P.; Strauss, J.; Zhao, Y. Healthy aging in China. J. Econ. Ageing 2014, 4, 37–43. [Google Scholar] [CrossRef] [Green Version]
- Mu, G. Health Problems in the Process of Population Aging, in Achieving Healthy Aging, Edited by China Society of Gerontology; China Labor Press: Beijing, China, 1995. [Google Scholar]
- WHO. China Country Assessment Report on Ageing and Health; WHO Press: Geneva, Switzerland, 2016. [Google Scholar]
- Zhang, W.; Wang, D. The health status of the Chinese elderly and changes since 1990s: Evidence from population censuses and sampling surveys. China Popul. Dev. Stud. 2019, 2, 369–383. [Google Scholar] [CrossRef] [Green Version]
- Hou, J. Structural Equation Model and Its Application; Education Science Press: Beijing, China, 2004. [Google Scholar]
- Guo, B. Study on the influencing factors of health service utilization of the elderly in rural areas from the perspective of healthy aging. Chin. Med. Ethics 2019, 32, 105–109. [Google Scholar]
- WHO. Active Ageing: A Policy Framework. Aging Male 2002, 5, 1–37. [Google Scholar] [CrossRef]
- Li, Z.; Gao, G. An Empirical Study on social participation of urban elderly in the context of active aging. Learn. Pract. 2009, 12, 116–123. [Google Scholar]
- Dang, J. Survey Report on the Living Conditions of the Elderly in Urban and Rural Areas of China; Social Sciences Literature Press: Beijing, China, 2018. [Google Scholar]
- Wang, M.; Bi, X.; Ye, H. Growth hybrid model: Analysis of individual development trends in different categories. Sociol. Stud. 2014, 29, 220–241. [Google Scholar]
- Zhu, H.; Huang, X. Positive aging attitude: Individual difference, group effect, and time change. Soc. Secur. Res. 2013, 5, 32–39. [Google Scholar]
- Fogel, R.W. Supplement: Aging, Health, and Public Policy || Changes in the Process of Aging during the Twentieth Century: Findings and Procedures of the Early Indicators Project. Popul. Dev. Rev. 2004, 30, 19–47. [Google Scholar]
- Chatterji, S.; Byles, J.; Cutler, D.; Seeman, T.; Verdes, E. Health, functioning, and disability in older adults-present status and future implications. Lancet 2015, 385, 563–575. [Google Scholar] [CrossRef] [Green Version]
- Oshio, T.; Shimizutani, S. Health capacity to work and its long-term trend among the Japanese elderly. J. Jpn. Int. Econ. 2019, 51, 76–86. [Google Scholar] [CrossRef] [Green Version]
- Young, Y.; Frick, K.D.; Phelan, E.A. Can Successful Aging and Chronic Illness Coexist in the Same Individual? A Multidimensional Concept of Successful Aging. J. Am. Med. Dir. Assoc. 2009, 10, 87–92. [Google Scholar] [CrossRef]


| Health Dimension | Indicator Variables |
|---|---|
| Functional status | ADL: six items, reflecting the abilities of self-care, including bathing, dressing, indoor activities, going to the toilet, eating, and controlling urination and defecation. Three points were given to those who did not need help, 2 points were given to those who needed help for one part, and 1 point was given to those who needed help for more than two parts. The scores of the 6 items of respondents were summed with a maximum of 18 points and a minimum of 6 points. IADL: Eight items, including whether the individual could visit their neighbor’s house, lift 5 kg of weight, wash clothes, cook, etc. Three points were given to those who could do it, 2 points were given to those who had certain difficulties, and 1 point was given to those who could not do it. The scores for the 8 items of the respondents were summed with a minimum of 8 points and a maximum of 24 points. ADS: six items measuring body function limitations: whether the hand could touch the back waist, whether the hand could touch the neck root, whether the individual could stand up from the chair, whether the individual could pick up a book from the ground, the steps required to rotate in situ, and whether the arm could be lifted. Completing the task with both hands received 3 points, one hand received 2 points, and neither hand received 1 point. After summing the scores, the maximum value was 18 points, and the minimum value was 6 points. |
| Physical health | Diseases: Number of serious diseases in the previous two years. Serious disease referred to the need for hospitalization or being bedridden at home. Chronic: Number of chronic diseases; each elderly person was required to report whether they had the listed chronic diseases. |
| Mental health | MMSE: Measured cognitive function in elderly individuals and included five aspects: orientation ability (general ability), response ability, attention and calculation abilities, recall ability, and language, understanding and self-coordination abilities, for a total of 24 questions. Seven points were given to the question, “How many food names can you say in one minute?” One point was given to the other 23 correctly answered questions, and 0 points were given to the incorrectly answered questions. The total score was 30. Loneliness: the elders were asked, “Do you often feel lonely?” Values of 1–5 represented always, often, sometimes, rarely and never. |
| Social health | Outdoor: Participation in outdoor activities, values 1–5 represent never, occasionally, at least once a month, at least once a week, and almost every day. Social: Participation in organized social activities, values 1–5 represent never, occasionally, at least once a month, at least once a week, and almost every day. |
| Variables | Frequency | Mean | S.D. | Minimum | Maximum |
|---|---|---|---|---|---|
| ADL | 64,317 | 16.89 | 2.490 | 6 | 18 |
| IADL | 64,770 | 18.05 | 6.100 | 8 | 24 |
| ADS | 64,025 | 15.76 | 2.880 | 6 | 18 |
| MMSE | 63,946 | 20.67 | 8.720 | 1 | 30 |
| Loneliness | 57,542 | 3.940 | 1.010 | 1 | 5 |
| Outdoor | 64,839 | 3.140 | 1.830 | 1 | 5 |
| Social | 64,812 | 1.280 | 0.820 | 1 | 5 |
| Chronic | 65,055 | 1.120 | 1.340 | 0 | 21 |
| Diseases | 63,465 | 0.280 | 0.780 | 0 | 30 |
| Dimensions and Indicators | (1) | (2) | (3) | (4) | (5) | |
|---|---|---|---|---|---|---|
| 2002 | 2005 | 2008 | 2011 | 2014 | ||
| Elderly Health (second order) | Functional Status | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Physical Health | −0.078 *** | −0.089 *** | −0.063 *** | −0.044 *** | −0.068 *** | |
| (−13.28) | (−14.47) | (−10.23) | (−3.44) | (−4.44) | ||
| Mental Health | 0.195 *** | 0.196 *** | 0.191 *** | 0.204 *** | 0.170 *** | |
| (21.65) | (20.25) | (20.16) | (16.77) | (11.77) | ||
| Social Health | 0.192 *** | 0.221 *** | 0.180 *** | 0.203 *** | 0.195 *** | |
| (26.24) | (26.26) | (23.31) | (18.81) | (14.44) | ||
| Functional Status | ADL | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| cons. | 17.174 *** | 17.293 *** | 17.420 *** | 17.232 *** | 17.310 *** | |
| (1155.00) | (1131.16) | (1209.35) | (829.82) | (703.74) | ||
| IADL | 4.906 *** | 4.664 *** | 4.920 *** | 4.518 *** | 4.706 *** | |
| (107.83) | (98.21) | (97.07) | (72.01) | (61.23) | ||
| cons. | 18.726 *** | 18.952 *** | 18.970 *** | 19.181 *** | 19.404 *** | |
| (406.73) | (404.59) | (400.27) | (311.01) | (257.15) | ||
| ADS | 1.493 *** | 1.506 *** | 1.796 *** | 1.366 *** | 1.444 *** | |
| (83.74) | (85.77) | (89.81) | (63.22) | (54.26) | ||
| cons. | 16.197 *** | 16.199 *** | 16.074 *** | 16.322 *** | 16.323 *** | |
| (831.41) | (806.63) | (758.67) | (647.92) | (523.72) | ||
| Physical Health | Serious illness | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| cons. | 0.233 *** | 0.269 *** | 0.228 *** | 0.351 *** | 0.398 *** | |
| (41.07) | (47.71) | (40.02) | (30.16) | (27.96) | ||
| Chronic disease | 2.334 *** | 2.084 *** | 1.317 *** | 1.542 *** | 0.823 *** | |
| (11.90) | (12.24) | (7.17) | (3.00) | (2.77) | ||
| cons. | 1.126 *** | 1.177 *** | 0.982 *** | 1.176 *** | 1.185 *** | |
| (101.44) | (99.68) | (96.43) | (74.41) | (62.64) | ||
| Mental Health | Lonely feeling | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| cons. | 3.933 *** | 3.959 *** | 3.939 *** | 3.985 *** | 3.945 *** | |
| (459.47) | (458.21) | (453.11) | (368.46) | (302.53) | ||
| MMSE | 20.444 *** | 22.208 *** | 21.856 *** | 21.899 *** | 24.200 *** | |
| (21.96) | (20.57) | (20.20) | (16.94) | (11.91) | ||
| cons. | 22.752 *** | 22.956 *** | 22.341 *** | 23.046 *** | 23.523 *** | |
| (439.16) | (412.91) | (428.45) | (316.10) | (278.18) | ||
| Social Health | Social activities | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| cons. | 1.299 *** | 1.333 *** | 1.278 *** | 1.310 *** | 1.330 *** | |
| (185.78) | (174.80) | (181.33) | (132.93) | (106.89) | ||
| Outdoor activities | 5.155 *** | 4.290 *** | 4.780 *** | 4.399 *** | 4.538 *** | |
| (25.96) | (26.29) | (23.30) | (18.45) | (14.41) | ||
| cons. | 3.441 *** | 3.304 *** | 3.224 *** | 3.256 *** | 3.243 *** | |
| (233.20) | (221.89) | (212.26) | (159.01) | (128.81) | ||
| Goodness of fit indices | N | 14149 | 13855 | 13961 | 7860 | 5216 |
| RMSEA | 0.056 | 0.058 | 0.047 | 0.049 | 0.044 | |
| CFI | 0.968 | 0.965 | 0.975 | 0.974 | 0.980 | |
| TLI | 0.951 | 0.945 | 0.960 | 0.959 | 0.968 | |
| SRMR | 0.055 | 0.044 | 0.031 | 0.047 | 0.039 | |
| R2 | 0.943 | 0.907 | 0.966 | 0.909 | 0.916 | |
| Results | Period | Five Periods | Four Periods | Three Periods | Two Periods |
|---|---|---|---|---|---|
| Mean differences test of Health_elders(latent variable) | 2002 | 0.000 | |||
| 2005 | 0.033 ** | 0.000 | |||
| (2.41) | (.) | ||||
| 2008 | −0.011 | −0.049 *** | 0.000 | ||
| (−0.80) | (−3.45) | (.) | |||
| 2011 | 0.065 *** | 0.029 * | 0.078 *** | 0.000 | |
| (4.03) | (1.80) | (4.89) | (.) | ||
| 2014 | 0.119 *** | 0.082 *** | 0.131 *** | 0.055 *** | |
| (6.41) | (4.38) | (7.04) | (2.65) | ||
| Measurement model estimation results | second order | omitted | omitted | omitted | omitted |
| first order | omitted | omitted | omitted | omitted | |
| Goodness of fit indices | N | 55,041 | 40,892 | 27,037 | 13,076 |
| RMSEA | 0.064 | 0.063 | 0.062 | 0.057 | |
| CFI | 0.934 | 0.937 | 0.939 | 0.953 | |
| TLI | 0.931 | 0.933 | 0.933 | 0.945 | |
| SRMR | 0.055 | 0.051 | 0.048 | 0.055 | |
| R2 (CD) | 0.920 | 0.917 | 0.922 | 0.931 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, Y.; Meng, Y. Is China Moving toward Healthy Aging? A Tracking Study Based on 5 Phases of CLHLS Data. Int. J. Environ. Res. Public Health 2020, 17, 4343. https://doi.org/10.3390/ijerph17124343
Yang Y, Meng Y. Is China Moving toward Healthy Aging? A Tracking Study Based on 5 Phases of CLHLS Data. International Journal of Environmental Research and Public Health. 2020; 17(12):4343. https://doi.org/10.3390/ijerph17124343
Chicago/Turabian StyleYang, Yinan, and Yingying Meng. 2020. "Is China Moving toward Healthy Aging? A Tracking Study Based on 5 Phases of CLHLS Data" International Journal of Environmental Research and Public Health 17, no. 12: 4343. https://doi.org/10.3390/ijerph17124343





