Photovoice-Based Assessment of Weight Management Experiences of Breast Cancer Patients Treated with Tamoxifen
Abstract
:1. Introduction
2. Materials and Methods
2.1. Recruitment and Study Participants
2.2. Ethical Consideration
2.3. Measurement
2.3.1. Training for Participants
- (1)
- What does weight management represent for me?
- (2)
- What helps me manage my weight in my life?
- (3)
- What comes in the way of weight management in my life?
- (4)
- What do I need to do in my life to control my weight?
2.3.2. Photo Shoots and Submission
2.3.3. Primary Data Analysis
2.3.4. Group Discussion by Theme
- (1)
- What do you see here?
- (2)
- What is really happening here?
- (3)
- How does this relate to our lives?
- (4)
- Why does this problem or this strength exist?
- (5)
- What can we do about this?
2.3.5. Comprehensive Discussion
2.3.6. Secondary Data Analysis
2.3.7. Credibility and Validity in Study
3. Results
3.1. General Characteristics of Participants
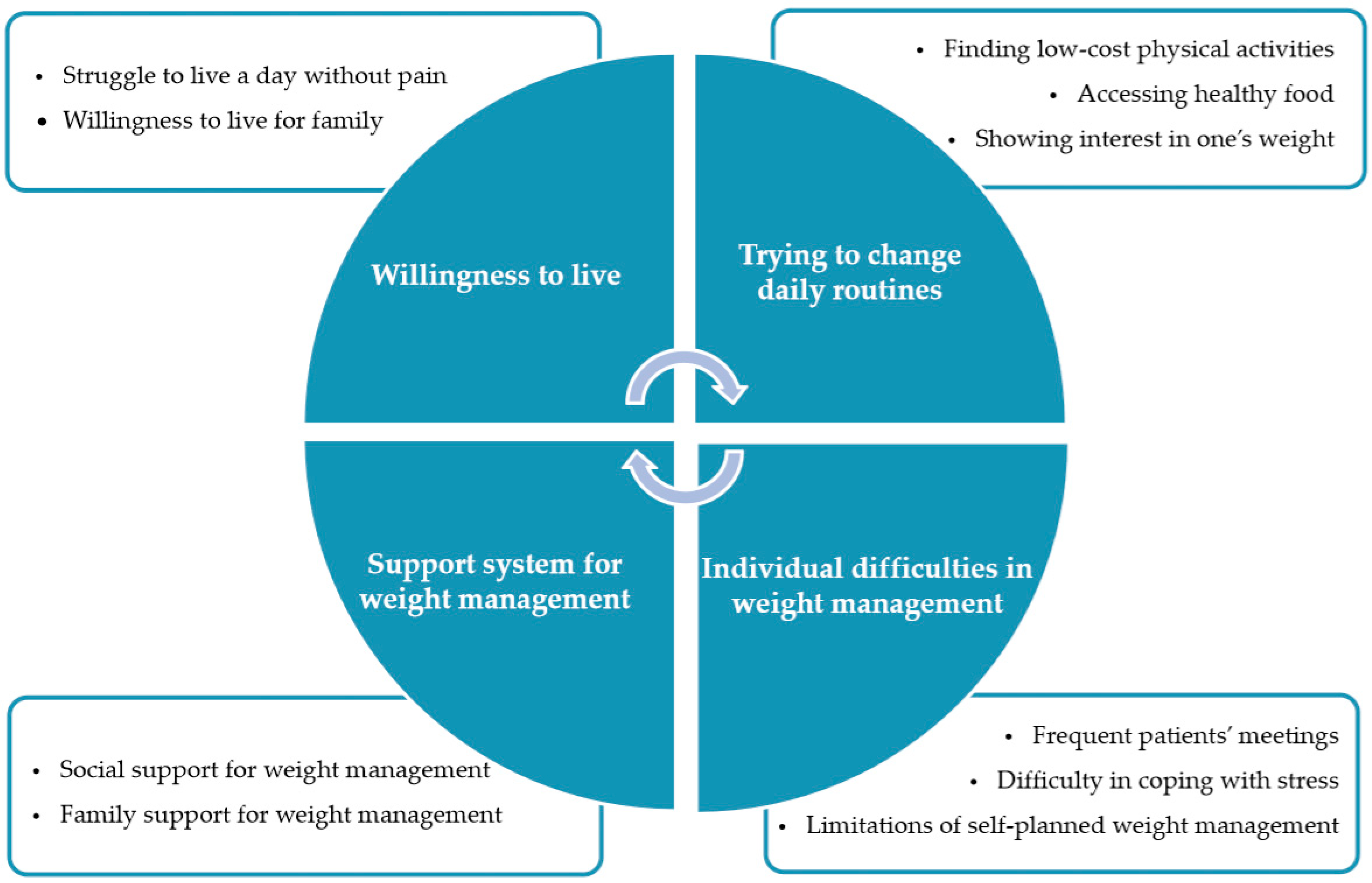
3.2. Photovoice Outcomes
3.2.1. Superordinate Theme 1: Willingness to Live
“To me, weight management means to live a healthy life even if I just have one day left to live. My goal is to live a healthy, pain-free life for at least a day rather than living long.”(Participant 1)
“Family is a goal in my life and I believe my family will be happy with me. If cancer comes back, putting me back in the hospital, it will certainly make my family sad more than anyone else. This is why I am determined to keep my weight under control for the sake of my family.”(Participant 9) (Figure 2)
3.2.2. Superordinate Theme 2: Trying to Change Daily Routine
“I started to go hiking for weight management. Going hiking is free of charge. I love the mountains, and once I get there, the clean mountain air refreshes me as if my pain instantly disappeared.”(Participant 3)
“Diet menus are of great help in maintaining my weight. Before I fell sick, my favorites were carbohydrate-rich foods, fried foods, and sweet stuff. I, probably, got breast cancer because of my dietary habits. So, I mainly blanch fresh seasonal vegetables before eating for my weight management.”(Participant 4) (Figure 3)
“The scale helps me maintain proper weight. I weigh myself once a day. While weighing myself, I also check the daily amount of food eaten or amount of exercise, along with plans for tomorrow’s weight management.”(Participant 5)
3.2.3. Superordinate Theme 3: Individual Difficulties in Weight Management
“I have four or five patients’ meetings to attend each month. I eat a lot there. It makes perfect sense in theory that I avoid overeating and achieve weight loss until I go there, but the problem is that I cannot help attending the meetings.”(Participant 8)
“It is the stress from my in-laws that prevents me from getting my weight under control. I turn to binge eating when stressed out.”(Participant 6)
“I am the only one in the family who works on weight control. To control my weight, I have to get up early in the morning or should exercise in a planned time segment of my daily routine. I am rather weak-willed and lazy, and I hardly go hiking, so I want to maintain weight by drinking detox juices and just keep burning fat.”(Participant 2) (Figure 4)
3.2.4. Superordinate Theme 4: Support System for Weight Management
“Treating breast cancer patients costs a lot, so many of them turn to hiking for financial reasons and give up other exercises. If the government builds sufficient voucher systems for exercise purposes, it will work out perfectly for us in terms of weight management. We can work out closer to home instead of going up the mountains.”(Participant 1) (Figure 5)
“The hospital recommends that breast cancer patients should take part in laughter therapy, but its effects are rather insignificant among the participants. Everyone has their own lifestyle.”(Participant 3)
“Energy exercises worked just great for me in managing my weight. But, there is no detailed information about which public healthcare center provides this program. I wish it was made easily accessible.”(Participant 5)
“It appears that weight management is not something I can achieve on my own, and I would like to receive help from my family to make it work.”(Participant 5)
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Worldwide Cancer Statistics. Cancer Research UK. 2018. Available online: http://www.cancerresearchuk.org/health-professional/cancer-statistics/worldwide-cancer (accessed on 2 October 2018).
- National Cancer Information Center. Cancer by Statistics. 2018. Available online: https://www.cancer.go.kr/lay1/S1T639C643/contents.do (accessed on 24 January 2018).
- Hwang, E.; Yi, M. Factors influencing quality of life in patients with breast cancer on hormone therapy. J. Korean Acad. Nurs. 2014, 44, 108. [Google Scholar] [CrossRef] [PubMed]
- Korean Breast Cancer Society. 2018 Breast Cancer Facts & Figures. 2018. Available online: http://www.kbcs.or.kr/sub02/sub04.html (accessed on 31 December 2018).
- Neven, P.; Jongen, L.; Lintermans, A.; Van Asten, K.; Blomme, C.; Lambrechts, D.; Poppe, A.; Wildiers, H.; Dieudonne, A.-S.; Brouckaert, O.; et al. Tamoxifen metabolism and efficacy in breast cancer: A prospective multicenter trial. Clin. Cancer Res. 2018, 24, 2312–2318. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Burstein, H.J.; Lacchetti, C.; Anderson, H.; Buchholz, T.A.; Davidson, N.E.; Gelmon, K.A.; Giordano, S.H.; Hudis, C.A.; Solky, A.J.; Stearns, V.; et al. Adjuvant endocrine therapy for women with hormone receptor–positive breast cancer: American society of clinical oncology clinical practice guideline focused update. J. Clin. Oncol. 2014, 32, 2255–2269. [Google Scholar] [CrossRef] [PubMed]
- Björner, S.; Rosendahl, A.H.; Tryggvadottir, H.; Simonsson, M.; Jirstrom, K.; Borgquist, S.; Rose, C.; Ingvar, C.; Jernström, H. Coffee is associated with lower breast tumor IGF1R levels in normal-weight patients and improved prognosis following tamoxifen or radiotherapy treatment. Front. Endocrinol. 2018, 9, 306. [Google Scholar] [CrossRef]
- Gathirua-Mwangi, W.G.; Zollinger, T.W.; Murage, M.J.; Pradhan, K.R.; Champion, V. Adult BMI change and risk of breast cancer: National Health and Nutrition Examination Survey (NHANES) 2005–2010. Breast Cancer 2015, 22, 648–656. [Google Scholar] [CrossRef] [Green Version]
- Boker, L.K.; Levine, H.; Derazne, E.; Molina-Hazan, V.; Kark, J.D. Measured adolescent body mass index and adult breast cancer in a cohort of 951,480 women. Breast Cancer Res. Treat. 2016, 158, 157–167. [Google Scholar] [CrossRef]
- Arnold, M.; Freisling, H.; Stolzenberg-Solomon, R.; Kee, F.; O’Doherty, M.G.; Ordóñez-Mena, J.M.; Wilsgaard, T.; May, A.M.; Bueno-De-Mesquita, H.B.; Tjonneland, A.; et al. Overweight duration in older adults and cancer risk: A study of cohorts in Europe and the United States. Eur. J. Epidemiol. 2016, 31, 893–904. [Google Scholar] [CrossRef] [Green Version]
- Demark-Wahnefried, W.; Campbell, K.L.; Hayes, S.; Hayes, S.C. Weight management and its role in breast cancer rehabilitation. Cancer 2012, 118, 2277–2287. [Google Scholar] [CrossRef] [Green Version]
- Pakiz, B.; Flatt, S.W.; Bardwell, W.A.; Rock, C.L.; Mills, P.J. Effects of a weight loss intervention on body mass, fitness, and inflammatory biomarkers in overweight or obese breast cancer survivors. Int. J. Behav. Med. 2011, 18, 333–341. [Google Scholar] [CrossRef] [Green Version]
- Key, T.J.; Appleby, P.N.; Reeves, G.K.; Roddam, A.; Dorgan, J.F.; Longcope, C.; Stanczyk, F.Z.; Stephenson, H.E.; Falk, R.T., Jr.; Miller, R.; et al. Endogenous hormones breast cancer collaborative group. Body mass index, serum sex hormones, and breast cancer risk in postmenopausal women. J. Natl. Cancer Inst. 2003, 95, 1218–1226. [Google Scholar] [CrossRef]
- Rock, C.L.; Doyle, C.; Demark-Wahnefried, W.; Meyerhardt, J.; Courneya, K.S.; Schwartz, A.L.; Bandera, E.V.; Hamilton, K.K.; Grant, B.; McCullough, M.; et al. Nutrition and physical activity guidelines for cancer survivors. CA Cancer J. Clin. 2012, 62, 275–276. [Google Scholar] [CrossRef] [Green Version]
- Lavie, C.J.; Laddu, D.; Arena, R.; Ortega, F.B.; Alpert, M.A.; Kushner, R.F. Healthy weight and obesity prevention: JACC health promotion series. J. Am. Coll. Cardiol. 2018, 72, 1506–1531. [Google Scholar] [CrossRef]
- Frank, L.; Kerr, J.; Sallis, J.F.; Miles, R.; Chapman, J.E. A hierarchy of sociodemographic and environmental correlates of walking and obesity. Prev. Med. 2008, 47, 172–178. [Google Scholar] [CrossRef] [PubMed]
- Kang, H.-S.; Han, J.; Kim, J.; Lee, H.-B.; Shin, H.-C.; Han, W.; Noh, N.-Y.; Moon, H.-G. Analysis of the relationship between body mass index and breast cancer incidence in Korean women. J. Breast Dis. 2016, 4, 64–69. [Google Scholar] [CrossRef]
- Kenzik, K.M.; Demark-Wahnefried, W.; Ganz, P.A.; Colditz, G.; Rock, C.L.; Rogers, L.Q. Changes in body mass index and physical activity predict changes in vitality during a weight loss trial in breast cancer survivors. Ann. Behav. Med. 2018, 52, 999–1009. [Google Scholar] [CrossRef] [PubMed]
- Rhee, Y.-S. Qualitative study on experience of health behavior among Korean low-income breast cancer survivors. J. Korea Acad. Coop. Soc. 2015, 16, 3188–3198. [Google Scholar] [CrossRef] [Green Version]
- Heo, S.-M.; Heo, N. Experiences of self-management support among breast cancer survivors. Korean J. Adult Nurs. 2016, 28, 470–481. [Google Scholar] [CrossRef] [Green Version]
- Kim, S.; Son, H. Appearance management experiences of breast cancer patients—A grounded theory approach. J. Korean Soc. Cloth. Text. 2017, 41, 556–574. [Google Scholar] [CrossRef]
- Lee, S.; Gedleh, A.; Hill, J.A.; Qaiser, S.; Umukunda, Y.; Odiyo, P.; Kitonyi, G.; Dimaras, H. In their own words: A qualitative study of Kenyan breast cancer survivors’ knowledge, experiences, and attitudes regarding breast cancer genetics. J. Glob. Oncol. 2018, 4, 1–9. [Google Scholar] [CrossRef]
- Andersen, E.R.; Eilertsen, G.; Myklebust, A.M.; Eriksen, S. Women’s experience of acute skin toxicity following radiation therapy in breast cancer. J. Multidiscip. Health 2018, 11, 139–148. [Google Scholar] [CrossRef] [Green Version]
- Owusu, C.; Antognoli, E.; Nock, N.L.; Hergenroeder, P.; Austin, K.; Bennet, E.; Berger, N.A.; Cerne, S.; Foraker, K.; Heine, K.; et al. Perspective of older African-American and Non-Hispanic white breast cancer survivors from diverse socioeconomic backgrounds toward physical activity: A qualitative study. J. Geriatr. Oncol. 2018, 9, 235–242. [Google Scholar] [CrossRef] [PubMed]
- Levkovich, I.; Cohen, M.; Karkabi, K. The experience of fatigue in breast cancer patients 1–12 month post-chemotherapy: A qualitative study. Behav. Med. 2017, 45, 7–18. [Google Scholar] [CrossRef]
- Wang, C.C.; Burris, M.A. Photovoice: Concept, methodology, and use for participatory needs assessment. Health Educ. Behav. 1997, 24, 369–387. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cordova, D. Accepting and Embracing My Disability-Describing the Life Experiences of Latinas/os with Physical Disabilities Who have Abused Substances; Michigan State University: East Lansing, MI, USA, 2010. [Google Scholar]
- Hergenrather, K. Photovoice as community-based participatory research: A qualitative review. Am. J. Health Behav. 2009, 33, 686–698. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Poudrier, J.; Mac-Lean, R.T. ‘We’ve fallen into the cracks’: Aboriginal women’s experiences with breast cancer through photovoice. Nurs. Inq. 2009, 16, 306–317. [Google Scholar] [CrossRef]
- Lopez, E.D.S.; Eng, E.; Randall-David, E.; Robinson, N. Quality-of-life concerns of African American breast cancer survivors within Rural North Carolina: Blending the techniques of photovoice and grounded theory. Qual. Health Res. 2005, 15, 99–115. [Google Scholar] [CrossRef]
- Wallerstein, N.; Bernstein, E. Empowerment education: Freire’s ideas adapted to health education. Health Educ. Q. 1988, 15, 379–394. [Google Scholar] [CrossRef]
- Morse, J.M.; Field, P.A. Qualitative Research Methods for Health Professionals; SAGE Publications: Thousand Oaks, CA, USA, 1995; Volume 2. [Google Scholar]
- Latz, A.O. Photovoice Research in Education and Beyond: A Practical Guide from Theory to Exhibition; Taylor & Francis: New York, NY, USA, 2017. [Google Scholar]
- Wang, C.C. Photovoice: A participatory action research strategy applied to women’s health. J. Women Health 1999, 8, 185–192. [Google Scholar] [CrossRef]
- Smith, J.A.; Flowers, P.; Larkin, M. Interpretative Phenomenological Analysis: Theory, Method and Research; SAGE Publications: London, UK, 2009; pp. 1–217. [Google Scholar]
- Guba, E.G.; Lincoln, Y.S. Fourth Generation Evaluation; SAGE Publications: Newbury Park, CA, USA, 1989. [Google Scholar]
- Sandelowski, M. The problem of rigor in qualitative research. Adv. Nurs. Sci. 1986, 8, 27–37. [Google Scholar] [CrossRef]
- Sinicrope, P.S.; Brockman, T.A.; Patten, C.A.; Frost, M.H.; Vierkant, R.; Petersen, L.R.; Rock, E.; Clark, L.P.; Vachon, C.M.; Fredericksen, Z.S.; et al. Factors associated with breast cancer prevention communication between mothers and daughters. J. Women Health 2008, 17, 1017–1023. [Google Scholar] [CrossRef] [Green Version]
- Baek, M.-J. The life of breast cancer survivors in long term survival period. J. Korean Soc. Wellness 2017, 12, 447–458. [Google Scholar] [CrossRef]
- Runowicz, C.D.; Leach, C.R.; Henry, N.L.; Henry, K.S.; Mackey, H.T.; Cowens-Alvarado, R.L.; Cannady, R.S.; Pratt-Chapman, M.L.; Edge, S.B.; Jacobs, L.A.; et al. American cancer society/American society of clinical oncology breast cancer survivorship care guideline. CA Cancer J. Clin. 2015, 66, 43–73. [Google Scholar] [CrossRef] [PubMed]
- National Comprehensive Cancer Network. NCCN Guidelines for Patients. 2018. Available online: https://www.nccn.org/professionals/physician_gls/default.aspx#detection (accessed on 12 July 2019).
- Helander, E.; Vuorinen, A.-L.; Wansink, B.; Korhonen, I. Are breaks in daily self-weighing associated with weight gain? PLoS ONE 2014, 9, e113164. [Google Scholar] [CrossRef] [PubMed]
- Yang, J. The actual experiences of the living world among cancer patients. J. Korean Acad. Nurs. 2008, 38, 140–151. [Google Scholar] [CrossRef]
- Brunet, J.; Taran, S.; Burke, S.; Sabiston, C.M. A qualitative exploration of barriers and motivators to physical activity participation in women treated for breast cancer. Disabil. Rehabil. 2013, 35, 2038–2045. [Google Scholar] [CrossRef]
- Doerksen, S.E.; McAuley, E. Social cognitive determinants of dietary behavior change in University Employes. Front. Public Health 2014, 2. [Google Scholar] [CrossRef] [Green Version]
- Stolley, M.R.; Sharp, L.K.; Fantuzzi, G.; Arroyo, C.; Sheean, P.; Schiffer, L.A.; Campbell, R.T.; Gerber, B. Study design and protocol for moving forward: A weight loss intervention trial for African-American breast cancer survivors. BMC Cancer 2015, 15, 1018. [Google Scholar] [CrossRef] [Green Version]
- Byeon, J.Y.; Kang, M.J.; Park, J.H.; Min, J.H.; Jeon, J.Y.; Byeon, Y.J. Exercise program based on preferences of breast cancer survivors. Korean J. Sport Stud. 2018, 57, 611–624. [Google Scholar] [CrossRef]




| ID | Age | Marital Status | Stage of Disease | Type of Operation | Chemotherapy | Radiation Therapy | Duration of Tamoxifen Therapy | Weight Gain after Tamoxifen Therapy | Weight Gain Degree (kg) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 54 | Married | 1 | Total mastectomy | Yes | No | 5 | Yes | 2 |
| 2 | 53 | Married | 2 | Total mastectomy | Yes | No | 8 | Yes | 2 |
| 3 | 60 | Married | 3 | Total mastectomy | Yes | Yes | 5 | Yes | 4 |
| 4 | 62 | Married | 2 | Total mastectomy | Yes | Yes | 7 | Yes | 10 |
| 5 | 55 | Married | 2 | Total mastectomy | Yes | No | 5 | Yes | 10 |
| 6 | 57 | Married | 2 | Total mastectomy | Yes | No | 6 | Yes | 2 |
| 7 | 65 | Married | 1 | Total mastectomy | Yes | No | 5 | Yes | 2 |
| 8 | 64 | Married | 1 | Subtotal mastectomy | Yes | Yes | 5 | Yes | 7 |
| 9 | 62 | Married | 3 | Total mastectomy | Yes | Yes | 7 | Yes | 4 |
| Superordinate Themes | Subordinate Themes |
|---|---|
| Willingness to live | Struggle to live a day without pain |
| Willingness to live for family | |
| Trying to change daily routine | Finding low-cost physical activities |
| Accessing healthy food | |
| Showing interest in one’s weight | |
| Individual difficulties in weight management | Frequent patients’ meetings |
| Difficulty in coping with stress | |
| Limitations of self-planned weight management | |
| Support system for weight management | Social support for weight management |
| Family support for weight management |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, J.S.; Han, J.-W.; Choi, J.H.; Lee, K.C. Photovoice-Based Assessment of Weight Management Experiences of Breast Cancer Patients Treated with Tamoxifen. Int. J. Environ. Res. Public Health 2020, 17, 4359. https://doi.org/10.3390/ijerph17124359
Park JS, Han J-W, Choi JH, Lee KC. Photovoice-Based Assessment of Weight Management Experiences of Breast Cancer Patients Treated with Tamoxifen. International Journal of Environmental Research and Public Health. 2020; 17(12):4359. https://doi.org/10.3390/ijerph17124359
Chicago/Turabian StylePark, Jung Suk, Jeong-Won Han, Jin Hyuk Choi, and Kyoung Chun Lee. 2020. "Photovoice-Based Assessment of Weight Management Experiences of Breast Cancer Patients Treated with Tamoxifen" International Journal of Environmental Research and Public Health 17, no. 12: 4359. https://doi.org/10.3390/ijerph17124359
APA StylePark, J. S., Han, J. -W., Choi, J. H., & Lee, K. C. (2020). Photovoice-Based Assessment of Weight Management Experiences of Breast Cancer Patients Treated with Tamoxifen. International Journal of Environmental Research and Public Health, 17(12), 4359. https://doi.org/10.3390/ijerph17124359





