Intervertebral Disc Disease of the Lumbar Spine in Health Personnel with Occupational Exposure to Patient Handling—A Systematic Literature Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Strategy
- P: Health personnel
- I (E): Manual patient transfer, patient transfer with small or technical patient handling aids, performing nursing activities, job-title based exposure
- C: general population, other occupational groups, subgroups within HP, or self-comparison over time
- O: Specific disease of the lumbar spine such as disc degeneration, disc herniation, disc protrusion, disc bulging, spondylosis, modic changes, and endplate changes
- S: Any design involving a comparison group
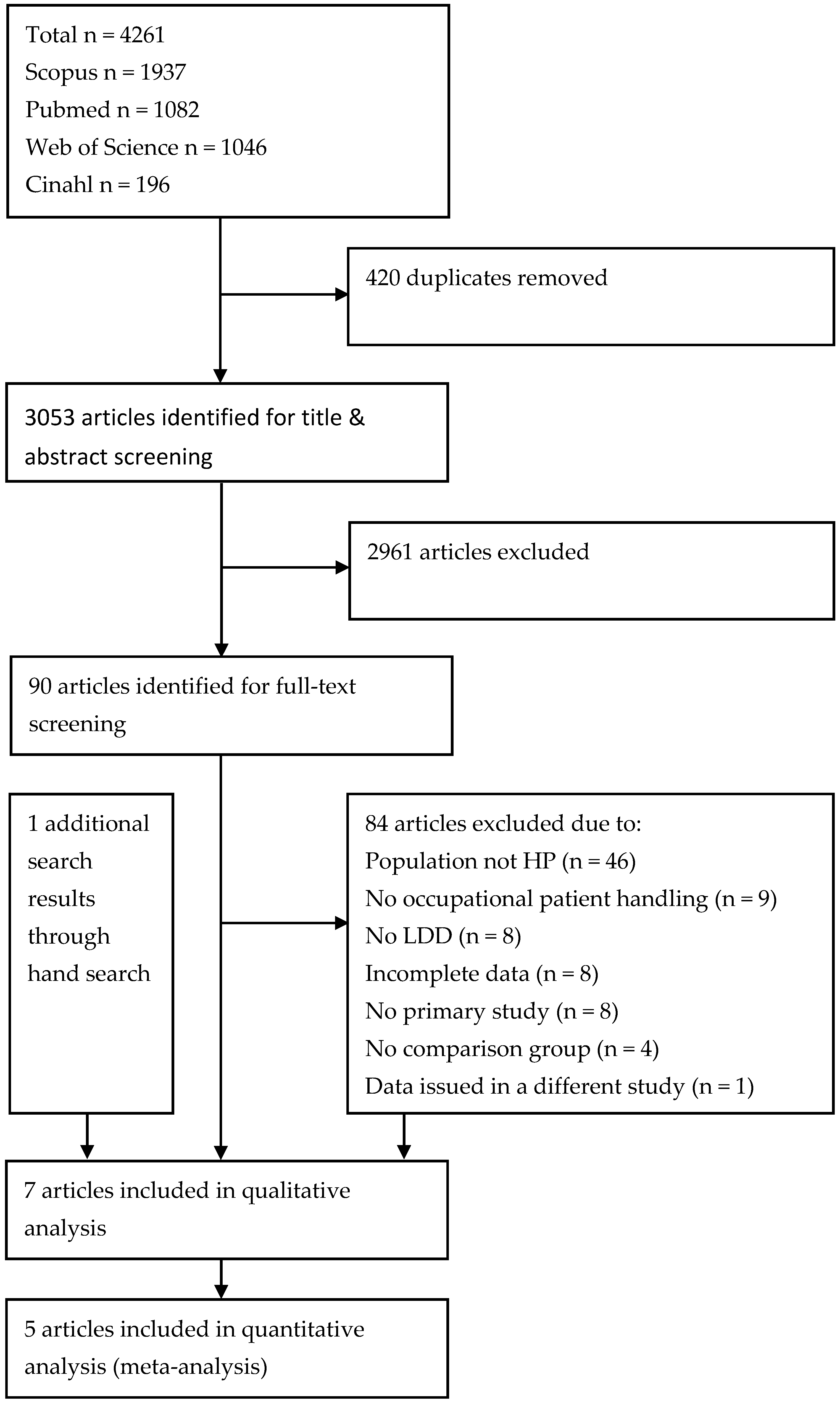
2.2. Study Selection
2.3. Quality Assessment
2.4. Data Extraction
2.5. Data Synthesis and Statistical Analysis
2.6. Publication Bias
2.7. Ethical Consideration
3. Results
3.1. Study Quality
3.2. Study Characteristics
3.3. Prevalence/Incidence Rates and Effects Measures of LDD in Individual Studies
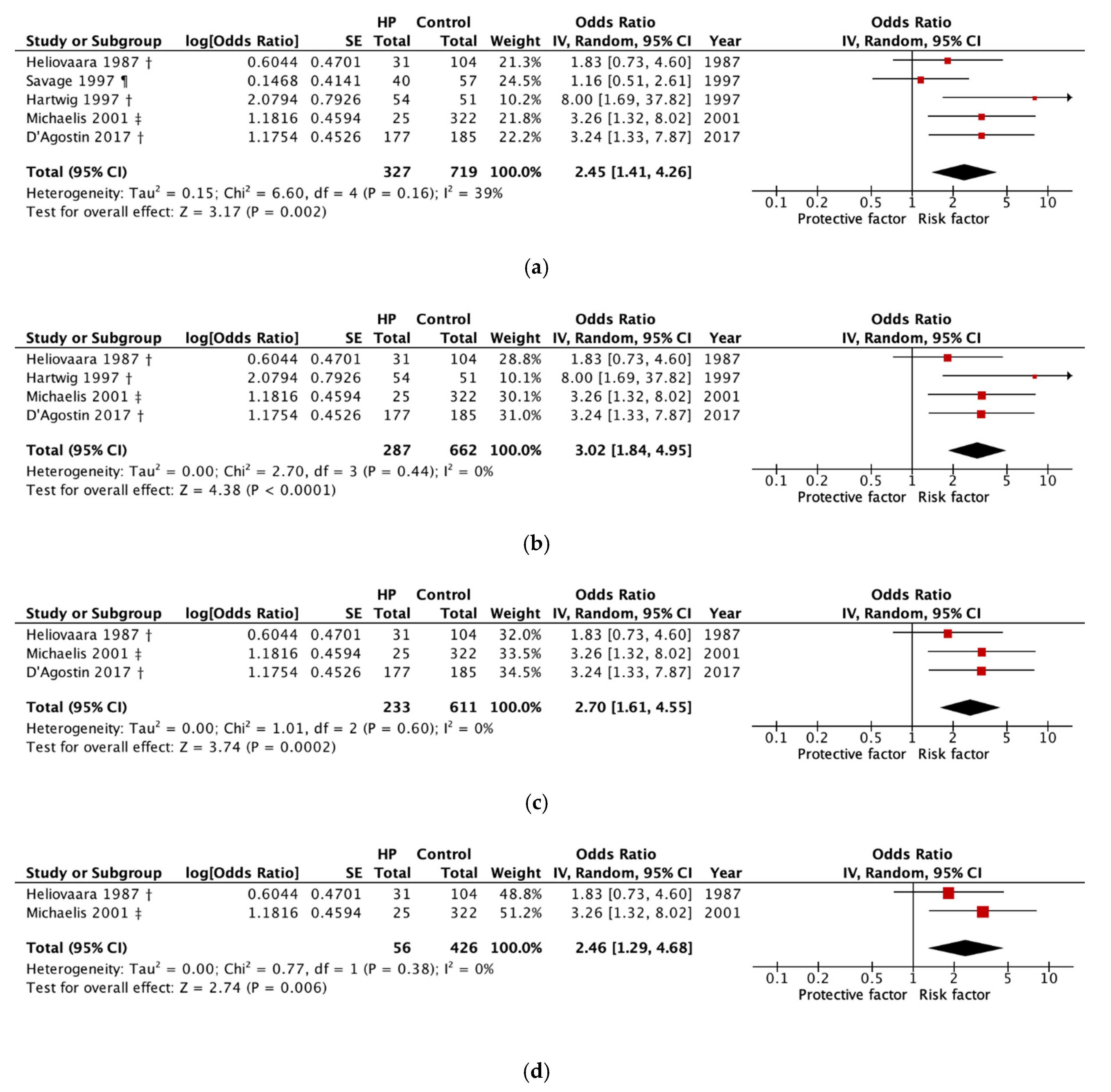
3.4. Meta-Analysis
3.5. Heterogeneity and Sensitivity Analysis
3.6. Publication Bias
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Andersson, G.B. Epidemiological features of chronic low-back pain. Lancet 1999, 354, 581–585. [Google Scholar] [CrossRef]
- Nasto, L.A.; Ngo, K.; Leme, A.S.; Robinson, A.R.; Dong, Q.; Roughley, P.; Usas, A.; Sowa, G.A.; Pola, E.; Kang, J.; et al. Investigating the role of DNA damage in tobacco smoking-induced spine degeneration. Spine J. 2014, 14, 416–423. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Schepper, E.I.; Damen, J.; van Meurs, J.B.; Ginai, A.Z.; Popham, M.; Hofman, A.; Koes, B.W.; Bierma-Zeinstra, S.M. The association between lumbar disc degeneration and low back pain: The influence of age, gender, and individual radiographic features. Spine 2010, 35, 531–536. [Google Scholar] [CrossRef] [PubMed]
- Cheung, K.M.; Karppinen, J.; Chan, D.; Ho, D.W.; Song, Y.Q.; Sham, P.; Cheah, K.S.; Leong, J.C.; Luk, K.D. Prevalence and pattern of lumbar magnetic resonance imaging changes in a population study of one thousand forty-three individuals. Spine 2009, 34, 934–940. [Google Scholar] [CrossRef]
- Wang, F.; Cai, F.; Shi, R.; Wang, X.H.; Wu, X.T. Aging and age related stresses: A senescence mechanism of intervertebral disc degeneration. Osteoarthr. Cartil. 2016, 24, 398–408. [Google Scholar] [CrossRef] [Green Version]
- Russo, F.; Hartman, R.A.; Bell, K.M.; Vo, N.; Sowa, G.A.; Kang, J.D.; Vadala, G.; Denaro, V. Biomechanical Evaluation of Transpedicular Nucleotomy With Intact Annulus Fibrosus. Spine 2017, 42, E193–E201. [Google Scholar] [CrossRef]
- Teraguchi, M.; Yoshimura, N.; Hashizume, H.; Muraki, S.; Yamada, H.; Minamide, A.; Oka, H.; Ishimoto, Y.; Nagata, K.; Kagotani, R.; et al. Prevalence and distribution of intervertebral disc degeneration over the entire spine in a population-based cohort: The Wakayama Spine Study. Osteoarthr. Cartil. 2014, 22, 104–110. [Google Scholar] [CrossRef] [Green Version]
- Cannata, F.; Vadala, G.; Ambrosio, L.; Fallucca, S.; Napoli, N.; Papalia, R.; Pozzilli, P.; Denaro, V. Intervertebral disc degeneration: A focus on obesity and type 2 diabetes. Diabetes Metab. Res. Rev. 2020, 36, e3224. [Google Scholar] [CrossRef]
- Macedo, L.G.; Battie, M.C. The association between occupational loading and spine degeneration on imaging—A systematic review and meta-analysis. BMC Musculoskelet. Disord. 2019, 20, 489. [Google Scholar] [CrossRef]
- Estryn-Behar, M.; Kaminski, M.; Peigne, E.; Maillard, M.F.; Pelletier, A.; Berthier, C.; Delaporte, M.F.; Paoli, M.C.; Leroux, J.M. Strenuous working conditions and musculo-skeletal disorders among female hospital workers. Int. Arch. Occup. Environ. Health 1990, 62, 47–57. [Google Scholar] [CrossRef]
- Kaplan, R.M.; Deyo, R.A. Back pain in health care workers. Occup. Med. 1988, 3, 61–73. [Google Scholar] [PubMed]
- Venning, P.J.; Walter, S.D.; Stitt, L.W. Personal and job-related factors as determinants of incidence of back injuries among nursing personnel. J. Occup. Med. 1987, 29, 820–825. [Google Scholar] [PubMed]
- Videman, T.; Nurminen, T.; Tola, S.; Kuorinka, I.; Vanharanta, H.; Troup, J.D. Low-back pain in nurses and some loading factors of work. Spine 1984, 9, 400–404. [Google Scholar] [CrossRef] [PubMed]
- Ulin, S.S.; Chaffin, D.B.; Patellos, C.L.; Blitz, S.G.; Emerick, C.A.; Lundy, F.; Misher, L. A biomechanical analysis of methods used for transferring totally dependent patients. SCI Nurs A Publ. Am. Assoc. Spinal Cord. Inj. Nurses 1997, 14, 19–27. [Google Scholar]
- Bakker, E.W.; Verhagen, A.P.; van Trijffel, E.; Lucas, C.; Koes, B.W. Spinal mechanical load as a risk factor for low back pain: A systematic review of prospective cohort studies. Spine 2009, 34, E281-93. [Google Scholar] [CrossRef]
- Ribeiro, D.C.; Aldabe, D.; Abbott, J.H.; Sole, G.; Milosavljevic, S. Dose-response relationship between work-related cumulative postural exposure and low back pain: A systematic review. Ann. Occup. Hyg. 2012, 56, 684–696. [Google Scholar] [CrossRef]
- Burdorf, A.; Koppelaar, E.; Evanoff, B. Assessment of the impact of lifting device use on low back pain and musculoskeletal injury claims among nurses. Occup. Environ. Med. 2013, 70, 491–497. [Google Scholar] [CrossRef]
- Jager, M.; Jordan, C.; Theilmeier, A.; Wortmann, N.; Kuhn, S.; Nienhaus, A.; Luttmann, A. Lumbar-load analysis of manual patient-handling activities for biomechanical overload prevention among healthcare workers. Ann. Occup. Hyg. 2013, 57, 528–544. [Google Scholar] [CrossRef] [Green Version]
- Schibye, B.; Hansen, A.F.; Hye-Knudsen, C.T.; Essendrop, M.; Bocher, M.; Skotte, J. Biomechanical analysis of the effect of changing patient-handling technique. Appl. Ergon. 2003, 34, 115–123. [Google Scholar] [CrossRef]
- Skotte, J.H.; Essendrop, M.; Hansen, A.F.; Schibye, B. A dynamic 3D biomechanical evaluation of the load on the low back during different patient-handling tasks. J. Biomech. 2002, 35, 1357–1366. [Google Scholar] [CrossRef]
- Engkvist, I.-L. Back injuries among nurses—A comparison of the accident processes after a 10-year follow-up. Saf. Sci. 2008, 46, 291–301. [Google Scholar] [CrossRef]
- Engkvist, I.L.; Hjelm, E.W.; Hagberg, M.; Menckel, E.; Ekenvall, L. Risk indicators for reported over-exertion back injuries among female nursing personnel. Epidemiology 2000, 11, 519–522. [Google Scholar] [CrossRef] [PubMed]
- Yassi, A.; Lockhart, K. Work-relatedness of low back pain in nursing personnel: A systematic review. Int. J. Occup. Environ. Health 2013, 19, 223–244. [Google Scholar] [CrossRef]
- Risbud, M.V.; Shapiro, I.M. Role of cytokines in intervertebral disc degeneration: Pain and disc content. Nat. Rev. Rheumatol. 2014, 10, 44–56. [Google Scholar] [CrossRef] [PubMed]
- Sakai, D.; Andersson, G.B. Stem cell therapy for intervertebral disc regeneration: Obstacles and solutions. Nat. Rev. Rheumatol. 2015, 11, 243–256. [Google Scholar] [CrossRef]
- Lu, J.; Wu, X.; Li, Y.; Kong, X. Surgical results of anterior corpectomy in the aged patients with cervical myelopathy. Eur. Spine J. 2008, 17, 129–135. [Google Scholar] [CrossRef] [Green Version]
- Wu, X.; Zhuang, S.; Mao, Z.; Chen, H. Microendoscopic discectomy for lumbar disc herniation: Surgical technique and outcome in 873 consecutive cases. Spine 2006, 31, 2689–2694. [Google Scholar] [CrossRef] [Green Version]
- Schäffler, A. Pschyrembel online. Available online: https://www.pschyrembel.de (accessed on 4 February 2020).
- Bontrup, C.; Taylor, W.R.; Fliesser, M.; Visscher, R.; Green, T.; Wippert, P.M.; Zemp, R. Low back pain and its relationship with sitting behaviour among sedentary office workers. Appl. Ergon. 2019, 81, 102894. [Google Scholar] [CrossRef]
- Koch, P.; Schablon, A.; Latza, U.; Nienhaus, A. Musculoskeletal pain and effort-reward imbalance--a systematic review. BMC Public Health 2014, 14, 37. [Google Scholar] [CrossRef] [Green Version]
- Plowman, S.A. Physical activity, physical fitness, and low back pain. Exerc. Sport Sci. Rev. 1992, 20, 221–242. [Google Scholar]
- Bletzer, J.; Gantz, S.; Voigt, T.; Neubauer, E.; Schiltenwolf, M. Chronic low back pain and psychological comorbidity: A review. Schmerz 2017, 31, 93–101. [Google Scholar] [CrossRef] [PubMed]
- Bjorck-van Dijken, C.; Fjellman-Wiklund, A.; Hildingsson, C. Low back pain, lifestyle factors and physical activity: A population based-study. J. Rehabil. Med. 2008, 40, 864–869. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stroup, D.F.; Berlin, J.A.; Morton, S.C.; Olkin, I.; Williamson, G.D.; Rennie, D.; Moher, D.; Becker, B.J.; Sipe, T.A.; Thacker, S.B. Meta-analysis of observational studies in epidemiology: A proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 2000, 283, 2008–2012. [Google Scholar] [CrossRef] [PubMed]
- Team, T.E. EndNote; EndNote X9; Clarivate Analytics: Philadelphia, PA, USA, 2013. [Google Scholar]
- Chung, Y.C.; Hung, C.T.; Li, S.F.; Lee, H.M.; Wang, S.G.; Chang, S.C.; Pai, L.W.; Huang, C.N.; Yang, J.H. Risk of musculoskeletal disorder among Taiwanese nurses cohort: A nationwide population-based study. BMC Musculoskelet. Disord. 2013, 14, 144. [Google Scholar] [CrossRef] [Green Version]
- Michaelis, M.; Hofmann, F.; Siegel, A.; Stössel, U. Bandscheibenprolaps und berufliche Belastungen unter besonderer Berücksichtigung des Krankenpflegeberufs. Ergebnisse einer Fall-Kontroll-Studie. Bandscheibenbedingte Erkrank. 2001, 3, 62–75. [Google Scholar]
- Schenk, P.; Laubli, T.; Hodler, J.; Klipstein, A. Magnetic resonance imaging of the lumbar spine: Findings in female subjects from administrative and nursing professions. Spine 2006, 31, 2701–2706. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [Green Version]
- Modesti, P.A.; Reboldi, G.; Cappuccio, F.P.; Agyemang, C.; Remuzzi, G.; Rapi, S.; Perruolo, E.; Parati, G. Panethnic Differences in Blood Pressure in Europe: A Systematic Review and Meta-Analysis. PLoS ONE 2016, 11, e0147601. [Google Scholar] [CrossRef] [Green Version]
- Review Manager (RevMan); 5.3; The Nordic Cochrane Centre, The Cochrane Collaboration: Copenhagen, Denmark, 2014.
- Higgins, J.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.; Welch, V. Cochrane Handbook for Systematic Reviews of Interventions, 2nd ed.; updated July 2019; John Wiley & Sons: Chichester, UK, 2019. [Google Scholar]
- Kunz, R.; Khan, K.S.; Kleijnen, J.; Antes, G. Systematische Übersichtsarbeiten und Meta-Analysen; Hans Huber: Bern, Switzerland, 2009; Volume 2, p. 146. [Google Scholar]
- Egger, M.; Davey Smith, G.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef] [Green Version]
- Heliovaara, M. Occupation and risk of herniated lumbar intervertebral disc or sciatica leading to hospitalization. J. Chronic Dis. 1987, 40, 259–264. [Google Scholar] [CrossRef]
- Hartwig, E.; Hoellen, I.; Liener, U.; Kramer, M.; Wickstroem, M.; Kinzl, L. Occupational disease 2108. Degeneration pattern in magnetic resonance tomography of the lumbar spine in patient with differential weight-bearing activity. Unfallchirurg 1997, 100, 888–894. [Google Scholar] [CrossRef] [PubMed]
- Savage, R.A.; Whitehouse, G.H.; Roberts, N. The relationship between the magnetic resonance imaging appearance of the lumbar spine and low back pain, age and occupation in males. Eur. Spine 1997, 6, 106–114. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- D’Agostin, F.; Negro, C. Symptoms and musculoskeletal diseases in hospital nurses and in a group of university employees: A cross-sectional study. Int. J. Occup. Saf. Ergon. 2017, 23, 274–284. [Google Scholar] [CrossRef] [PubMed]
- Makino, H.; Kawaguchi, Y.; Seki, S.; Nakano, M.; Yasuda, T.; Suzuki, K.; Ikegawa, S.; Kimura, T. Lumbar disc degeneration progression in young women in their 20’s: A prospective ten-year follow up. J. Orthop. Sci. 2017, 22, 635–640. [Google Scholar] [CrossRef]
- Thiede, M.; Liebers, F.; Seidler, A.; Gravemeyer, S.; Latza, U. Gender specific analysis of occupational diseases of the low back caused by carrying, lifting or extreme trunk flexion—Use of a prevention index to identify occupations with high prevention needs. Am. J. Ind. Med. 2014, 57, 233–244. [Google Scholar] [CrossRef] [Green Version]
- Mok, F.P.; Samartzis, D.; Karppinen, J.; Luk, K.D.; Fong, D.Y.; Cheung, K.M. ISSLS prize winner: Prevalence, determinants, and association of Schmorl nodes of the lumbar spine with disc degeneration: A population-based study of 2449 individuals. Spine 2010, 35, 1944–1952. [Google Scholar] [CrossRef] [Green Version]
- Hicks, G.E.; Morone, N.; Weiner, D.K. Degenerative lumbar disc and facet disease in older adults: Prevalence and clinical correlates. Spine 2009, 34, 1301–1306. [Google Scholar] [CrossRef] [Green Version]
- Wong, A.Y.; Karppinen, J.; Samartzis, D. Low back pain in older adults: Risk factors, management options and future directions. Scoliosis Spinal Disord. 2017, 12, 14. [Google Scholar] [CrossRef]
- Landau, K.; Landau, K.; Diaz-Meyer, M.; Weißert-Horn, M.; Jacobs, M.; Stern, H.; Raske, H. Zur Belastung und Beanspruchung beim Patiententransfer von Schwerstpflegebedürftigen. ASU Arbeitsmed. Soz. Med. Umweltmed. 2014, 49, 850–861. [Google Scholar]
- Freiberg, A.; Euler, U.; Girbig, M.; Nienhaus, A.; Freitag, S.; Seidler, A. Does the use of small aids during patient handling activities lead to a decreased occurrence of musculoskeletal complaints and diseases? A systematic review. Int. Arch. Occup. Environ. Health 2016, 89, 547–559. [Google Scholar] [CrossRef]
- Hegewald, J.; Berge, W.; Heinrich, P.; Staudte, R.; Freiberg, A.; Scharfe, J.; Girbig, M.; Nienhaus, A.; Seidler, A. Do Technical Aids for Patient Handling Prevent Musculoskeletal Complaints in Health Care Workers?-A Systematic Review of Intervention Studies. Int. J. Environ. Res. Public Health 2018, 15, 476. [Google Scholar] [CrossRef] [Green Version]
- Battie, M.C.; Joshi, A.B.; Gibbons, L.E.; Group, I.D.S.P. Degenerative Disc Disease: What is in a Name? Spine 2019, 44, 1523–1529. [Google Scholar] [CrossRef] [PubMed]
- Modic, M.T.; Obuchowski, N.A.; Ross, J.S.; Brant-Zawadzki, M.N.; Grooff, P.N.; Mazanec, D.J.; Benzel, E.C. Acute low back pain and radiculopathy: MR imaging findings and their prognostic role and effect on outcome. Radiology 2005, 237, 597–604. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, Y.X.J.; Wu, A.M.; Ruiz Santiago, F.; Nogueira-Barbosa, M.H. Informed appropriate imaging for low back pain management: A narrative review. J. Orthop. Transl. 2018, 15, 21–34. [Google Scholar] [CrossRef] [PubMed]
| Author, Year | Selection (Max. 4 +) | Comparability (Max. 2 +) | Outcome (Max. 3 +) | Study Quality * |
|---|---|---|---|---|
| Heliovaara, 1987 [45] | +++ | ++ | ++ | ++ |
| Hartwig et al., 1997 [46] | - | - | + | + |
| Savage et al., 1997 [47] | ++ | - | +++ | + |
| Michaelis et al., 2002 [37] | +++ | ++ | ++ | +++ |
| Chung et al., 2013 [36] | +++ | ++ | +++ | +++ |
| D’Agostin & Negro, 2017 [48] | ++++ | - | +++ | + |
| Makino et al., 2017 [49] | ++ | + | +++ | ++ |
| Author, Year | Random Sequence Generation (Selection Bias) | Allocation Concealment (Selection Bias) | Blinding of Participants and Personnel (Performance Bias) | Blinding of Outcome Assessment (Detection Bias) | Incomplete Outcome Data (Attrition Bias) | Selective Reporting (Reporting Bias) |
|---|---|---|---|---|---|---|
| Heliovaara, 1987 [45] | High | High | High | Unclear | Low | Low |
| Hartwig et al., 1997 [46] | High | High | High | Unclear | Low | Low |
| Savage et al., 1997 [47] | High | High | High | Unclear | High | Low |
| Michaelis et al., 2002 [37] | High | High | High | Unclear | Low | Low |
| Chung et al., 2013 [36] | High | High | High | Unclear | Low | Low |
| D’Agostin & Negro, 2017 [48] | High | High | High | Unclear | Low | Low |
| Makino et al., 2017 [49] | High | High | High | Unclear | High | Low |
| Exposure Group | Comparison Group | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Author (Year), Study Design | Aim of Study | Year and Country of Data Collection | Sample Size in Analysis N (F (%)) | Occupation N (F (%)) | Age in Years (Range or Mean (SD) At Baseline) | Occupation N (F (%)) | Age in Years (Range or Mean (SD) at Baseline) | Explanatory Variable | Outcome Assessment | Prevalence of Degenerative Findings N (%) | Effect Measure (95% CI) or (p-Value) |
| Heliovaara (1987), Longitudinal study [45] | Identify risk groups for herniated lumbar intervertebral disc or sciatica and to generate causal hypotheses | 1966–1972, (follow-up end 1980), Finland | 135 (100) | Nurses and related medical workers 31 (100) | 20–59 # | White-collar workers 104 (100) | 20–59 # | Job-title (NYK 1983) | ICD-8 725.10 or 725.19 | Herniated lumbar disc: Nurses and related medical workers 9/31 (29.03); White-collar workers 19/104 (18,27) | RR a = 2.2 (p ≥ 0.05) |
| Hartwig et al. (1997), cross-sectional study [46] | Clarify if different degeneration patterns occur in burdened and non-burdened patients | 1994–1995, Germany | 105 (n/a) | Nurses 54 (n/a) | 35–50 # | General population, (no spine-burdening activity) with chronic back problems 51 (n/a) | 35–50 # | Job-title | MRI | Disc degeneration: Nurses 52/54 (96.30); General population with chronic back problems 39/51 (76.47) | OR b = 8.00 (1.69, 37.82) * (RevMan) |
| Savage et al. (1997), cross-sectional study [47] | Undertake a critical review of the potential role of MRI in the evaluation of LBP | ≤1997, United Kingdom | 73 (0.0) | Hospital porters 16 (0.0) | 20–58 # | Office staff 57 (0.0) | 20–58 # | Job-title | MRI | Disc degeneration, disc herniation, facet joint hypertrophy or evidence of nerve root compression: Hospital porters 7/16 (43.75); Ambulance men 12/24 (50.00); Office staff 25/57 (43.86) | OR b = 1.00 (0.33, 3.04) (RevMan) |
| 81 (n/a) | Ambulance men 24 (0.0) | 20–58 # | Office staff 57 (0.0) | 20–58 # | OR b = 1.28 (0.49, 3.34) (RevMan) | ||||||
| Michaelis et al. (2001), case control study [37] | Identify overrepresented occupational groups in patients with detectable damage to the intervertebral discs. | 1990–1992, Germany | 677 (n/a) | Nurses and geriatric nurses 8 (n/a) | 47.9 $ (11.5) | Working (not nursing) general population ¥ 669 (n/a) | 47.9 $ (11.5) | Years of Service <10 | MRI/CT | Herniated disc: Nurses and geriatric nurses <10: 5/8 (62.5); ≥10: 13/17 (76.47); Working general population ¥ 329/669 (49.18) | OR b = 1.72 (0.40, 7.27) |
| 686 (n/a) | Nurses and geriatric nurses 17 (n/a) | Years of Service ≥10 | OR b = 3.36 (1.08, 10.41) | ||||||||
| D’Agostin & Negro (2017), Cross-sectional study [48] | Gain insight into the prevalence of MSDs in nursing | 2011–2012, Italy | 362 (68.23) $ | Nurses 177 (76.8) | 42.3 (10.2) | University staff (computer users) 185 (60.0) | 38.7 (12.0) | Job-title | MRI, CT, US, ENG, X-ray | Lumbar disc herniation: Nurses 20/177 (11.30); University staff 7/185 (3.78) | OR b = 3.11 (1.28, 7.56) * (RevMan) |
| Chung et al. (2013), prospective incidence study [36] | Assess the incidence of MSDs among a Taiwanese nurse cohort compared with non-nurses | 2004–2010, Taiwan | 15,658 (98.65) $ | Nurses 3914 (98.65) $ | 33.98 (7.68) $ | Working (not nursing) and non-working subjects 11,744 (98.65) $ | 34.01 (7.69) $ | Job-title (NHIRD) | ICD-9-CM (721.3) ICD-9-CM (722.10) | Herniated intervertebral disc: Nurses: 1.45; Working (not nursing) and non-working subjects: 0.64 | OR b = 2.48 (1.82, 3.38) * |
| Lumbar spondylosis: Nurses: 1.07; Working (not nursing) and non-working subjects: 0.81 | OR b = 1.36 (1.00, 1.84) * | ||||||||||
| Makino et al. (2017), prospective cohort study [49] | Clarify the process and features of lumbar disc degeneration progression in young women | 1996–2003 (9,8 (7–14) follow-up), Japan | 345 (100) at baseline | Nurses 345 (100) | 20.9 (20–22) | -- | -- | Job-title | MRI | Disc degeneration: 107/345 (31.0) | -- |
| 84 (100) at follow-up | Nurses (OP/IC) 51 (100) | 30.6 # (28–35) | Nurses (Clinic or others) 33 (100) | 30.6 # (28–35) | OP or IC ward | Disc degeneration: (n/a) | RR b = 0.79 (0.46, 1.37) | ||||
| Nurses n/a (100) | Nurses n/a (100) | Years of service >5 | Disc degeneration: (n/a) | RR b = 1.30 (0.73, 2.30) | |||||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schröder, C.; Nienhaus, A. Intervertebral Disc Disease of the Lumbar Spine in Health Personnel with Occupational Exposure to Patient Handling—A Systematic Literature Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2020, 17, 4832. https://doi.org/10.3390/ijerph17134832
Schröder C, Nienhaus A. Intervertebral Disc Disease of the Lumbar Spine in Health Personnel with Occupational Exposure to Patient Handling—A Systematic Literature Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2020; 17(13):4832. https://doi.org/10.3390/ijerph17134832
Chicago/Turabian StyleSchröder, Christofer, and Albert Nienhaus. 2020. "Intervertebral Disc Disease of the Lumbar Spine in Health Personnel with Occupational Exposure to Patient Handling—A Systematic Literature Review and Meta-Analysis" International Journal of Environmental Research and Public Health 17, no. 13: 4832. https://doi.org/10.3390/ijerph17134832
APA StyleSchröder, C., & Nienhaus, A. (2020). Intervertebral Disc Disease of the Lumbar Spine in Health Personnel with Occupational Exposure to Patient Handling—A Systematic Literature Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 17(13), 4832. https://doi.org/10.3390/ijerph17134832





