Musculoskeletal Complaints in Occupational Therapists Compared to the General Population: A Cross-Sectional Study in Germany
Abstract
:1. Introduction
2. Materials and Methods
2.1. Sample Size Calculation
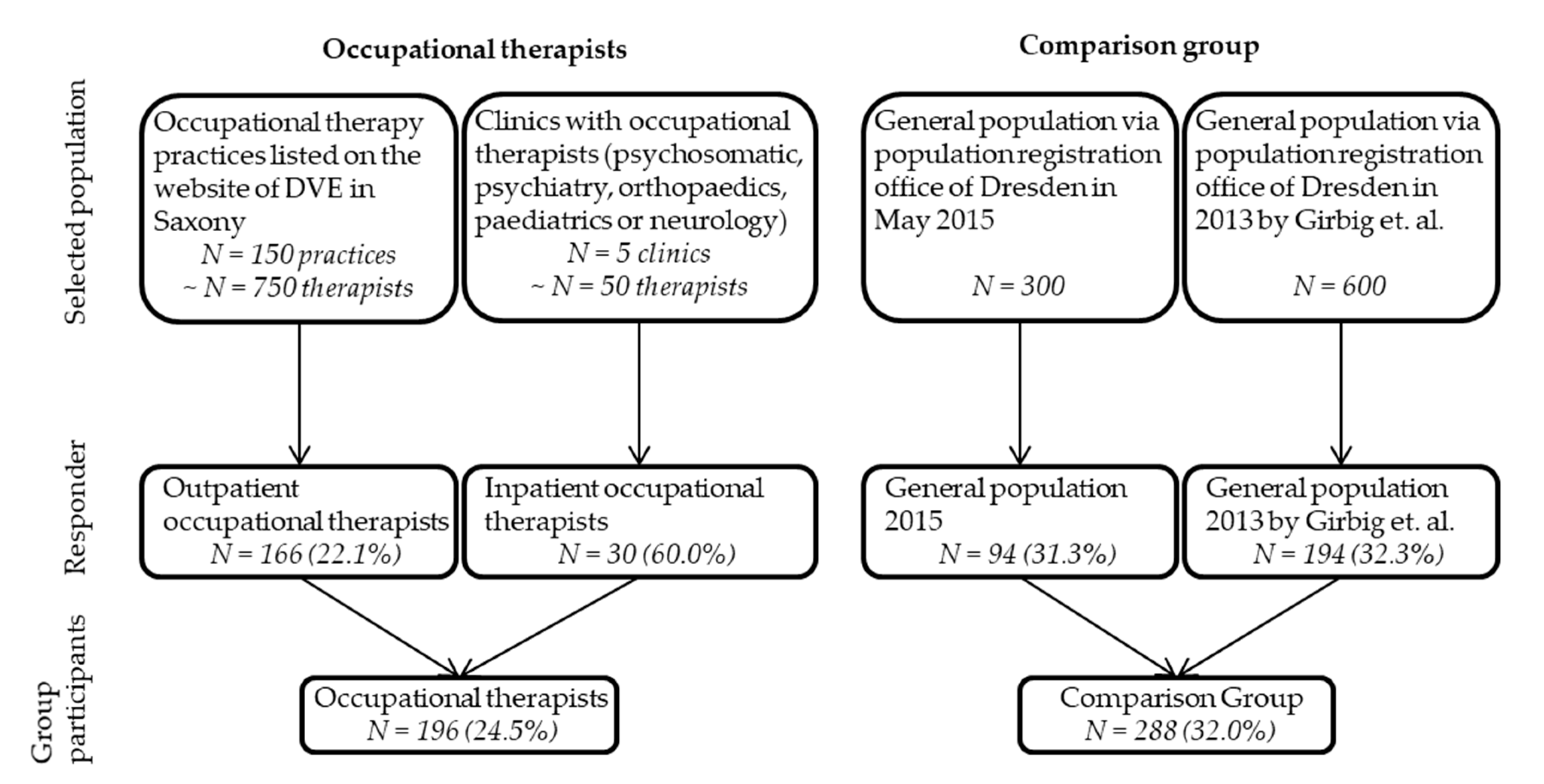
2.2. Participants
2.3. Data Collection
- German demographic standards [24];
- Adapted EPILIFT (German Lumbar Spine Study) questions to assess musculoskeletal exposures associated with work-related postures in general, and the back [25];
- Hand activity level (HAL, [26]) ratings for exposures associated with hand activity combined (measured on scales of 0–10 where the answer possibilities were: 0 = ”Hand idle most of the time; no regular exertions” to 10 = “Rapid, steady motion/difficulty keeping up or continuous exertion”);
- Normalized peak force (nPF, [27]) for exposures associated with hand strength (measured on scales of 0–10 where 0 = ”nothing at all” and 10 = ”extremely strong”) and;
2.4. Statistical Analyses
3. Results
3.1. Sociodemographic Characteristics
3.2. Descriptive Analysis of Work-Related Exposures
3.3. Prevalence of Musculoskeletal Complaints
3.4. Prevalence Ratios of Musculoskeletal Complaints
3.5. Sensitivity Analysis: Prevalence Ratios with Work-Related Exposures
4. Discussion
Strength and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Anderson, S.P.; Oakman, J. Allied Health Professionals and Work-Related Musculoskeletal Disorders: A Systematic Review. Saf. Health Work 2016, 7, 259–267. [Google Scholar] [CrossRef] [Green Version]
- DVE. Die Ergotherapie in Deutschland. Zahlen. Daten. Fakten; Deutscher Verband der Ergotherapeuten E. V.: Karlsbad, Deutschland, 2017. [Google Scholar]
- Smith, D.R.; Leggat, P.A.; Clark, M. Upper Body Musculoskeletal Disorders among Australian Occupational Therapy Students. Br. J.Occup. Ther. 2006, 69, 365–372. [Google Scholar] [CrossRef]
- Kamwendo, K. Adherence to Healthy Lifestyles: A Comparison of Occupational Therapy Students with Nursing and Physiotherapy Students. Scand. J. Occup. Ther. 2000, 7, 156–164. [Google Scholar] [CrossRef]
- Alnaser, M.Z. Occupational Therapy Practitioners with Occupational Musculoskeletal Injuries: Prevalence and Risk Factors. J. Occup. Rehabil. 2015, 25, 763–769. [Google Scholar] [CrossRef] [PubMed]
- Darragh, A.R.; Huddleston, W.; King, P. Work-related musculoskeletal injuries and disorders among occupational and physical therapists. Am. J. Occup. Ther. Off. Publ. Am. Occup. Ther. Assoc. 2009, 63, 351–362. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Campo, M.; Darragh, A.R. Impact of work-related pain on physical therapists and occupational therapists. Phys. Ther. 2010, 90, 905–920. [Google Scholar] [CrossRef] [PubMed]
- Passier, L.; McPhail, S. Work related musculoskeletal disorders amongst therapists in physically demanding roles: Qualitative analysis of risk factors and strategies for prevention. BMC Musculoskelet. Disord. 2011, 12, 24. [Google Scholar] [CrossRef] [Green Version]
- Girbig, M.; Freiberg, A.; Deckert, S.; Druschke, D.; Kopkow, C.; Nienhaus, A.; Seidler, A. Work-related exposures and disorders among physical therapists: Experiences and beliefs of professional representatives assessed using a qualitative approach. J. Occup. Med. Toxicol. 2017, 12, 2. [Google Scholar] [CrossRef] [Green Version]
- Kotejoshyer, R.; Punnett, L.; Dybel, G.; Buchholz, B. Claim Costs, Musculoskeletal Health, and Work Exposure in Physical Therapists, Occupational Therapists, Physical Therapist Assistants, and Occupational Therapist Assistants: A Comparison Among Long-Term Care Jobs. Phys. Ther. 2019, 99, 183–193. [Google Scholar] [CrossRef] [Green Version]
- Rice, M.S.; Dusseau, J.M.; Miller, B.K. A Questionnaire of Musculoskeletal Injuries Associated With Manual Patient Lifting in Occupational Therapy Practitioners in the State of Ohio. Occup. Ther. Health Care 2011, 25, 95–107. [Google Scholar] [CrossRef]
- Holtermann, A.; Clausen, T.; Jorgensen, M.B.; Burdorf, A.; Andersen, L.L. Patient handling and risk for developing persistent low-back pain among female healthcare workers. Scand. J. Work Environ. Health 2013, 39, 164–169. [Google Scholar] [CrossRef] [Green Version]
- Campo, M.; Weiser, S.; Koenig, K.L.; Nordin, M. Work-related musculoskeletal disorders in physical therapists: A prospective cohort study with 1-year follow-up. Phys. Ther. 2008, 88, 608–619. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Darragh, A.R.; Campo, M.; King, P. Work-related activities associated with injury in occupational and physical therapists. Work (Read. Mass.) 2012, 42, 373–384. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Islam, M.S.; Habib, M.M.; Hafez, M.A.; Nahar, N.; Lindstrom-Hazel, D.; Rahman, M.K. Musculoskeletal complaints among physiotherapy and occupational therapy rehabilitation professionals in Bangladesh. Work (Read. Mass.) 2015, 50, 379–386. [Google Scholar] [CrossRef]
- Serranheira, F.; Sousa-Uva, M.; Sousa-Uva, A. Hospital nurses tasks and work-related musculoskeletal disorders symptoms: A detailed analysis. Work (Read. Mass.) 2015, 51, 401–409. [Google Scholar] [CrossRef] [PubMed]
- Park, J. Work-related musculoskeletal disorders among occupational therapists in Korea. J. Phys. Ther. Sci. 2015, 27, 3627–3629. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nordander, C.; Hansson, G.A.; Ohlsson, K.; Arvidsson, I.; Balogh, I.; Stromberg, U.; Rittner, R.; Skerfving, S. Exposure-response relationships for work-related neck and shoulder musculoskeletal disorders--Analyses of pooled uniform data sets. Appl. Ergon. 2016, 55, 70–84. [Google Scholar] [CrossRef]
- Nordander, C.; Ohlsson, K.; Akesson, I.; Arvidsson, I.; Balogh, I.; Hansson, G.A.; Stromberg, U.; Rittner, R.; Skerfving, S. Exposure-response relationships in work-related musculoskeletal disorders in elbows and hands—A synthesis of group-level data on exposure and response obtained using uniform methods of data collection. Appl. Ergon. 2013, 44, 241–253. [Google Scholar] [CrossRef]
- Menzel, N.N.; Brooks, S.M.; Bernard, T.E.; Nelson, A. The physical workload of nursing personnel: Association with musculoskeletal discomfort. Int. J. Nurs. Stud. 2004, 41, 859–867. [Google Scholar] [CrossRef]
- Abramson, J.H. WINPEPI updated: Computer programs for epidemiologists, and their teaching potential. Epidemiol. Perspect. Innov. EP+I 2011, 8, 1. [Google Scholar] [CrossRef] [Green Version]
- Ellegast, R.; Bergmann, A.; Grifka, J.; Jaeger, M.; Michaelis, M.; Schäfer, K.; Seidler, A.; Bolm-Audorff, U. Methodology of the German Spine Studies: Data compilation of lifetime physical exposures and degenerative lumbar diseases in EPILIFT. In Proceedings of the 20th Congress of the International Ergonomics Association, Florence, Italy, 26–30 August 2018. [Google Scholar]
- Girbig, M.; Deckert, S.; Kopkow, C.; Latza, U.; Dulon, M.; Nienhaus, A.; Groneberg, D.; Seidler, A. Work-related complaints and diseases of physical therapists—Protocol for the establishment of a “Physical Therapist Cohort” (PTC) in Germany. J. Occup. Med. Toxicol. 2013, 8, 34. [Google Scholar] [CrossRef] [Green Version]
- Hoffmeyer-Zlotnik, J.H.; Glemser, A.; Heckel, C.; von der Heyde, C.; Quitt, H.; Hanefeld, U.; Herter-Eschweiler, R.; Mohr, S. Statistik und Wissenschaft: Demographische Standards Ausgabe 2010 (Band 17); Statistisches Bundesamt: Wiesbaden, Germany, 2010. [Google Scholar]
- Seidler, A.; Bergmann, A.; Jäger, M.; Ellegast, R.; Ditchen, D.; Elsner, G.; Grifka, J.; Haerting, J.; Hofmann, F.; Linhardt, O.; et al. Cumulative occupational lumbar load and lumbar disc disease–results of a German multi-center case-control study (EPILIFT). BMC Musculoskelet. Disord. 2009, 10, 48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Latko, W.A.; Armstrong, T.J.; Foulke, J.A.; Herrin, G.D.; Rabourn, R.A.; Ulin, S.S. Development and Evaluation of an Observational Method for Assessing Repetition in Hand Tasks. Am. Ind. Hyg. Assoc. J. 1997, 58, 278–285. [Google Scholar] [CrossRef]
- Borg, G. Psychophysical scaling with applications in physical work and the perception of exertion. Scand. J. Work Environ. Health 1990, 16 (Suppl. 1), 55–58. [Google Scholar] [CrossRef]
- Caffier, G.; Steinberg, U.; Liebers, F. Praxisorientiertes Methodeninventar Zur Belastungs-Und Beanspruchungsbeurteilung Im Zusammenhang Mit Arbeitsbedingten Muskel-Skelett-Erkrankungen; Wirtschaftsverl. NW, Verlag für Neue Wissenschart: Dortmund/Berlin, Deutschland, 1999. [Google Scholar]
- Kuorinka, I.; Jonsson, B.; Kilbom, A.; Vinterberg, H.; Biering-Sørensen, F.; Andersson, G.; Jørgensen, K. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl. Ergon. 1987, 18, 233–237. [Google Scholar] [CrossRef]
- Spielholz, P.; Bao, S.; Howard, N.; Silverstein, B.; Fan, J.; Smith, C.; Salazar, C. Reliability and validity assessment of the hand activity level threshold limit value and strain index using expert ratings of mono-task jobs. J. Occup. Environ. Hyg. 2008, 5, 250–257. [Google Scholar] [CrossRef] [PubMed]
- American Conference of Governmental Industrial Hygienists ACGIH. Documentation of the Threshold Limit Values for Physical Agents, 7th ed.; American Conference of Governmental Industrial Hygienists ACGIH: Washington, DC, USA, 2001. [Google Scholar]
- Spiegelman, D.; Hertzmark, E. Easy SAS calculations for risk or prevalence ratios and differences. Am. J. Epidemiol. 2005, 162, 199–200. [Google Scholar] [CrossRef] [Green Version]
- King, P.; Huddleston, W.; Darragh, A.R. Work-related musculoskeletal disorders and injuries: Differences among older and younger occupational and physical therapists. J. Occup. Rehabil. 2009, 19, 274–283. [Google Scholar] [CrossRef]
- Leggat, P.A.; Smith, D.R.; Clark, M.J. Prevalence and correlates of low back pain among occupational therapy students in Northern Queensland. Can. J. Occup. Ther. Rev. Can. Ergother. 2008, 75, 35–41. [Google Scholar] [CrossRef]
- Harrington, J.M.; Carter, J.T.; Birrell, L.; Gompertz, D. Surveillance case definitions for work related upper limb pain syndromes. Occup. Environ. Med. 1998, 55, 264–271. [Google Scholar] [CrossRef] [Green Version]
- Kapellusch Jm, J.M.; Gerr, F.E.; Malloy, E.J.; Garg, A.; Harris-Adamson, C.; Bao, S.S.; Burt, S.E.; Dale, A.M.; Eisen, E.A.; Evanoff, B.A.; et al. Exposure-response relationships for the ACGIH threshold limit value for hand-activity level: Results from a pooled data study of carpal tunnel syndrome. Scand. J. Work Environ. Health 2014, 40, 610–620. [Google Scholar] [CrossRef] [Green Version]
- Garg, A.; Kapellusch, J.; Hegmann, K.; Wertsch, J.; Merryweather, A.; Deckow-Schaefer, G.; Malloy, E.J. The Strain Index (SI) and Threshold Limit Value (TLV) for Hand Activity Level (HAL): Risk of carpal tunnel syndrome (CTS) in a prospective cohort. Ergonomics 2012, 55, 396–414. [Google Scholar] [CrossRef] [PubMed]
- Violante, F.S.; Farioli, A.; Graziosi, F.; Marinelli, F.; Curti, S.; Armstrong, T.J.; Mattioli, S.; Bonfiglioli, R. Carpal tunnel syndrome and manual work: The OCTOPUS cohort, results of a ten-year longitudinal study. Scand. J. Work Environ. Health 2016, 42, 280–290. [Google Scholar] [CrossRef] [Green Version]
- Ellegast, R.; Hermanns, I.; Schiefer, C. Workload Assessment in Field Using the Ambulatory CUELA System. In Digital Human Modeling; Duffy, V.G., Ed.; Springer: Berlin/Heidelberg, Germany, 2009; pp. 221–226. [Google Scholar]
- Gyer, G.; Michael, J.; Inklebarger, J. Occupational hand injuries: A current review of the prevalence and proposed prevention strategies for physical therapists and similar healthcare professionals. J. Integr. Med. 2018, 16, 84–89. [Google Scholar] [CrossRef] [PubMed]
- Rossettini, G.; Rondoni, A.; Schiavetti, I.; Tezza, S.; Testa, M. Prevalence and risk factors of thumb pain in Italian manual therapists: An observational cross-sectional study. Work (Read. Mass.) 2016, 54, 159–169. [Google Scholar] [CrossRef] [Green Version]
- Grooten, W.J.; Wernstedt, P.; Campo, M. Work-related musculoskeletal disorders in female Swedish physical therapists with more than 15 years of job experience: Prevalence and associations with work exposures. Physiother. Theory Pract. 2011, 27, 213–222. [Google Scholar] [PubMed]
- Rozenfeld, V.; Ribak, J.; Danziger, J.; Tsamir, J.; Carmeli, E. Prevalence, risk factors and preventive strategies in work-related musculoskeletal disorders among Israeli physical therapists. Physiother. Res. Int. J. Res. Clin. Phys. Ther. 2010, 15, 176–184. [Google Scholar] [CrossRef]
- West, D.; Gardner, D. Occupational injuries of physiotherapists in North and Central Queensland. Aust. J. Physiother. 2001, 47, 179–186. [Google Scholar] [CrossRef] [Green Version]
- Sherehiy, B.; Karwowski, W.; Marek, T. Relationship between risk factors and musculoskeletal disorders in the nursing profession: A systematic review. Occup. Ergon. 2004, 4, 241–279. [Google Scholar]
- Salik, Y.; Ozcan, A. Work-related musculoskeletal disorders: A survey of physical therapists in Izmir-Turkey. BMC Musculoskelet. Disord. 2004, 5, 27. [Google Scholar] [CrossRef] [Green Version]
- Rottenecker, J. Beschäftigungs- und Bildungssituation in den Therapieberufen. Available online: https://www.hv-gesundheitsfachberufe.de/wp-content/uploads/Impulsvortrag_Rottenecker.pdf (accessed on 19 January 2020).

| Occupational Therapists (n = 196) | Comparison Group (n = 288) | p Value | |
|---|---|---|---|
| Sex; n (%) | |||
| Female | 182 (92.9) | 152 (53.3) | |
| Male | 14 (7.1) | 133 (46.7) | |
| Total | 196 | 285 | <0.001 |
| Age; Mean (SD) | 37.4 (9.6) | 41.4 (12.8) | |
| Total; n | 196 | 285 | <0.001 |
| BMI; Mean (SD) | 25.0 (5.3) | 25.2 (5.0) | |
| Total | 194 | 281 | 0.689 |
| Education; n (%) | |||
| Secondary school | 0 (0.0) | 1 (0.3) | |
| High school | 11 (5.6) | 17 (5.9) | |
| Vocational | 167 (85.2) | 44 (15.3) | |
| University | 18 (9.2) | 30 (10.4) | |
| Missing | 0 (0.0) | 196 (67.4) | <0.001 |
| Working setting (sector) 1; n (%) | not applicable | ||
| Inpatient | 23 (11.7) | ||
| semi-residential | 13 (6.6) | ||
| outpatient | 170 (86.7) | ||
| other | 31 (15.8) |
| Body Area | Occupational Therapists (n = 196) | Comparison Group (n = 285) | ||||
|---|---|---|---|---|---|---|
| Total | Women | Men | Total | Women | Men | |
| Neck/Cervical spine | 149/187 (79.7%) | 141/174 (81.0%) | 8/13 (61.5%) | 185/253 (73.1%) | 111/141 (78.7%) | 73/111 (65.8%) |
| Shoulders | 128/184 (69.6%) | 122/171 (71.3%) | 6/13 (46.2%) | 144/230 (62.6%) | 91/127 (71.7%) | 52/102 (51.0%) |
| Elbows | 41/179 (22.9%) | 38/166 (22.9%) | 3/13 (23.1%) | 42/250 (16.8%) | 23/136 (16.9%) | 19/113 (16.8%) |
| Wrists | 89/181 (49.2%) | 85/168 (50.6%) | 4/13 (30.8%) | 69/216 (31.9%) | 41/118 (34.7%) | 28/98 (28.6%) |
| Thumbs | 95/181 (52.5%) | 89/168 (53.0%) | 6/13 (46.2%) | 36/205 (17.6%) | 23/109 (21.1%) | 13/96 (13.5%) |
| Lower back | 135/185 (73.0%) | 128/172 (74.4%) | 7/13 (53.8%) | 169/249 (67.9%) | 98/135 (72.6%) | 70/113 (61.9%) |
| Knee | 66/182 (36.3%) | 64/169 (37.9%) | 2/13 (15.4%) | 114/238 (47.9%) | 57/125 (45.6%) | 56/112 (50.0%) |
| Body Area | Total PR (95% CI) | Women PR (95% CI) | Men PR (95% CI) |
|---|---|---|---|
| Neck/Cervical spine | 1.0 (0.9–1.1) | 1.0 (0.9–1.15) | 0.9 (0.6–1.4) |
| Shoulders | 1.0 (0.9–1.2) | 1.0 (0.9–1.16) | 0.9 (0.5–1.7) |
| Elbows | 1.5 (1.0–2.2) | 1.6 (1.0–2.58) | 1.5 (0.5–4.3) |
| Wrists | 1.4 (1.1–1.8) | 1.5 (1.1–1.94) | 1.1 (0.5–2.6) |
| Thumbs | 2.7 (1.9–3.8) | 2.6 (1.8–3.82) | 3.2 (1.4–7.2) |
| Lower back | 1.0 (0.9–1.2) | 1.0 (0.9–1.17) | 0.8 (0.5–1.4) |
| Knee | 0.8 (0.6–1.0) | 0.9 (0.7–1.21) | 0.3 (0.1–1.1) |
| Afflicted Body Areas | Neck PR (95% CI); n/N | Shoulders PR (95% CI); n/N | Elbows PR (95% CI); n/N | Wrists PR (95% CI); n/N | Thumbs PR (95% CI); n/N |
|---|---|---|---|---|---|
| Reference (CG) | 1.0 (Ref); 185/253 | 1.0 (Ref); 144/230 | 1.0 (Ref); 42/250 | 1.0 (Ref); 69/216 | 1.0 (Ref); 36/205 |
| below AL (OT) | 1.0 (0.9–1.1) 66/86 | 0.9 (0.8–1.1) 53/83 | 1.1 (0.6–1.9); 14/82 | 1.2 (0.9–1.7); 35/81 | 2.3 (1.5–3.5); 36/81 |
| between AL and TLV (OT) | 1.1 (0.9–1.3) 36/42 | 1.0 (0.8–1.3) 31/44 | 1.0 (0.4–2.2); 6/41 | 1.7 (1.2–2.3); 25/43 | 2.8 (1.8–4.4); 23/43 |
| above TLV (OT) | 1.0 (0.9–1.2) 45/57 | 1.1 (0.9–1.3) 42/55 | 2.3 (1.5–3.7); 20/54 | 1.5 (1.1–2.1); 29/55 | 3.2 (2.2–4.7); 35/55 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zenker, R.; Girbig, M.; Hegewald, J.; Gilewitsch, I.; Wagner, M.; Nienhaus, A.; Seidler, A. Musculoskeletal Complaints in Occupational Therapists Compared to the General Population: A Cross-Sectional Study in Germany. Int. J. Environ. Res. Public Health 2020, 17, 4916. https://doi.org/10.3390/ijerph17144916
Zenker R, Girbig M, Hegewald J, Gilewitsch I, Wagner M, Nienhaus A, Seidler A. Musculoskeletal Complaints in Occupational Therapists Compared to the General Population: A Cross-Sectional Study in Germany. International Journal of Environmental Research and Public Health. 2020; 17(14):4916. https://doi.org/10.3390/ijerph17144916
Chicago/Turabian StyleZenker, Ronny, Maria Girbig, Janice Hegewald, Irina Gilewitsch, Mandy Wagner, Albert Nienhaus, and Andreas Seidler. 2020. "Musculoskeletal Complaints in Occupational Therapists Compared to the General Population: A Cross-Sectional Study in Germany" International Journal of Environmental Research and Public Health 17, no. 14: 4916. https://doi.org/10.3390/ijerph17144916





