Bilateral Foot Orthoses Elicit Changes in Gait Kinematics of Adolescents with Down Syndrome with Flatfoot
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Ethical Aspects
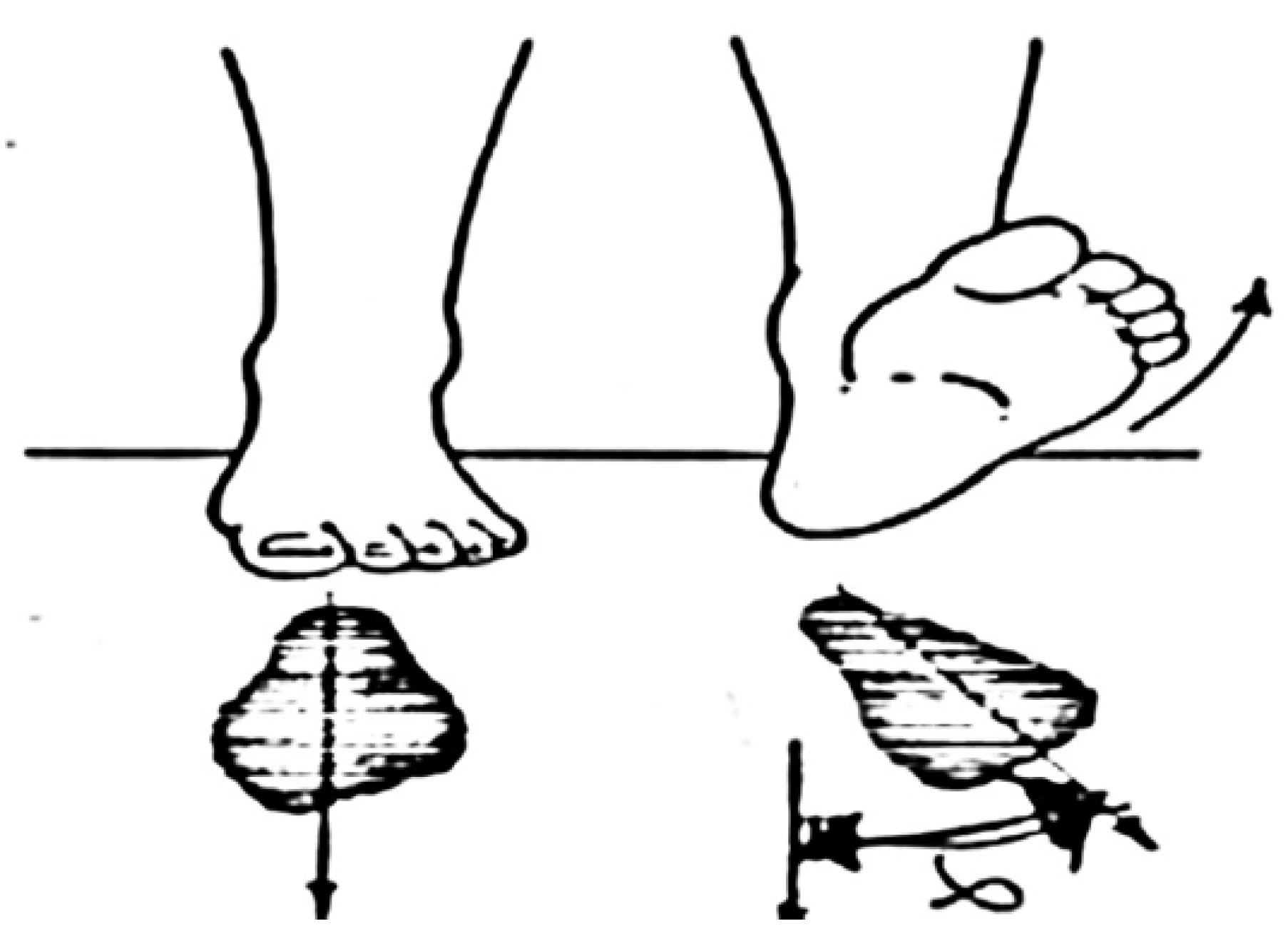
2.3. Procedures
- gait cycle (s)—mean temporal duration of the gait cycle that begins with initial heel contact and ends with the subsequent heel contact of the same limb;
- % stance (as a % of the gait cycle)—% of the gait cycle that begins with initial contact and ends at toe-off of the same limb;
- % double support (as a % of the gait cycle)—% of the gait cycle during which the feet are placed on the ground;
- mean velocity (m/s)—the mean velocity of progression for each limb;
- stride length (m)—distance between successive ground contacts of the same foot;
- step length (m)—longitudinal distance from one-foot strike to the next one;
- step width (m)—mediolateral distance between the two feet during double support.
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Cioni, M. Gait analysis of individuals with Down syndrome. Phys. Medi. Rehabil. 2002, 16, 303. [Google Scholar]
- Lim, P.Q.; Shields, N.; Nikolopoulos, N.; Barrett, J.T.; Evans, A.M.; Taylor, N.F.; Munteanu, S.E. The association of foot structure and footwear fit with disability in children and adolescents with Down syndrome. J. Foot Ankle Res. 2015, 8, 4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- American Academy of Orthopaedic Surgeons. Down Syndrome: Musculoskeletal Effects. Available online: https://orthoinfo.aaos.org/en/diseases--conditions/down-syndrome-musculoskeletal-effects (accessed on 31 December 2019).
- Ancillao, A.; van der Krogt, M.M.; Buizer, A.I.; Witbreuk, M.M.; Cappa, P.; Harlaar, J. Analysis of gait patterns pre- and post- Single Event Multilevel Surgery in children with Cerebral Palsy by means of Offset-Wise Movement Analysis Profile and Linear Fit Method. Hum. Mov. Sci. 2017, 55, 145–155. [Google Scholar] [CrossRef] [PubMed]
- Ancillao, A.; Rossi, S.; Cappa, P. Analysis of Knee Strength Measurements Performed by a Hand-Held Multicomponent Dynamometer and Optoelectronic System. IEEE Trans. Instrum. Meas. 2016, 66, 85–92. [Google Scholar] [CrossRef] [Green Version]
- Ancillao, A. Interpretation of Gait Analysis Data by Means of Synthetic Descriptors and a New Method for the Analysis of the Offset. In Modern Functional Evaluation Methods for Muscle Strength and Gait Analysis; Springer: Cham, Switzerland, 2018; pp. 89–121. [Google Scholar] [CrossRef]
- Galli, M.; Rigoldi, C.; Brunner, R.; Virji-Babul, N.; Giorgio, A. Joint stiffness, and gait pattern evaluation in children with Down syndrome. Gait Posture 2008, 28, 502–506. [Google Scholar] [CrossRef] [PubMed]
- Galli, M.; Cimolin, V.; Rigoldi, C.; Kleiner, A.F.R.; Condoluci, C.; Albertini, G. Use of the Gait Profile Score for the Quantification of Gait Pattern in Down Syndrome. J. Dev. Phys. Disabil. 2015, 27, 609–615. [Google Scholar] [CrossRef]
- Galli, M.; Cimolin, V.; Patti, P.; Ferrario, D.; Heaney, G.; Albertini, G.; Freedland, R. Quantifying established clinical assessment measures using 3D-movement analysis in individuals with Down syndrome. Disabil. Rehabil. 2010, 32, 1768–1774. [Google Scholar] [CrossRef]
- Cioni, M.; Cocilovo, A.; Rossi, F.; Paci, D.; Valle, M.S. Analysis of ankle kinetics during walking in individuals with Down syndrome. Am. J. Ment. Retard. 2001, 106. [Google Scholar] [CrossRef]
- Galli, M.; Cimolin, V.; Pau, M.; Costici, P.; Albertini, G. Relationship between flat foot condition and gait pattern alterations in children with Down syndrome. J. Intellect. Disabil. Res. 2013, 58, 269–276. [Google Scholar] [CrossRef]
- Galli, M.; Cimolin, V.; Rigoldi, C.; Pau, M.; Costici, P.; Albertini, G. The effects of low arched feet on foot rotation during gait in children with Down syndrome. J. Intellect. Disabil. Res. 2013, 58, 758–764. [Google Scholar] [CrossRef]
- Rigoldi, C.; Galli, M.; Albertini, G. Gait development during lifespan in subjects with Down syndrome. Res. Dev. Disabil. 2011, 32, 158–163. [Google Scholar] [CrossRef] [PubMed]
- Bok, S.-K.; Lee, H.; Kim, B.-O.; Ahn, S.Y.; Song, Y.; Park, I. The Effect of Different Foot Orthosis Inverted Angles on Plantar Pressure in Children with Flexible Flatfeet. PLoS ONE 2016, 11, e0159831. [Google Scholar] [CrossRef] [PubMed]
- Wenger, D.R.; Mauldin, D.; Speck, G.; Morgan, D.; Lieber, R.L. Corrective shoes and inserts as treatment for flexible flatfoot in infants and children. J. Bone Jt. Surg. Am. Vol. 1989, 71, 800–810. [Google Scholar] [CrossRef] [Green Version]
- Hsieh, R.-L.; Peng, H.-L.; Lee, W.-C. Short-term effects of customized arch support insoles on symptomatic flexible flatfoot in children. Medicine 2018, 97, e10655. [Google Scholar] [CrossRef]
- Külcü, D.G.; Yavuzer, G.; Sarmer, S.; Ergin, S. Immediate Effects of Silicone Insoles on Gait Pattern in Patients with Flexible Flatfoot. Foot Ankle Int. 2007, 28, 1053–1056. [Google Scholar] [CrossRef]
- Selby-Silverstein, L.; Hillstrom, H.J.; Palisano, R.J. The effect of foot orthoses on standing foot posture and gait of young children with Down Syndrome. Neurorehabilitation 2001, 16, 183–193. [Google Scholar] [CrossRef]
- Looper, J.; Benjamin, D.; Nolan, M.; Schumm, L. What to Measure When Determining Orthotic Needs in Children with Down Syndrome. Pediatr. Phys. Ther. 2012, 24, 313–319. [Google Scholar] [CrossRef]
- Ancillao, A. Stereophotogrammetry in Functional Evaluation: History and Modern Protocols. In Systematic Industrial Maintenance to Boost the Quality Management Programs; Springer Science and Business Media LLC: Berlin/Heidelberg, Germany, 2017; pp. 1–29. [Google Scholar]
- Ancillao, A. Interpretation of Gait Analysis Data by Means of Synthetic Descriptors and a New Method for the Analysis of the Offset. In Systematic Industrial Maintenance to Boost the Quality Management Programs; Springer Science and Business Media LLC: Berlin/Heidelberg, Germany, 2017; pp. 89–121. [Google Scholar]
- Autorizzazione Generale al Trattamento dei Dati Personali per Scopi di Ricerca Scientifica. Available online: https://www.garanteprivacy.it/home/docweb/-/docweb-display/docweb/1878276 (accessed on 1 March 2012).
- Davis, R.B.; Õunpuu, S.; Tyburski, D.; Gage, J.R.; Iii, R.B.D. A gait analysis data collection and reduction technique. Hum. Mov. Sci. 1991, 10, 575–587. [Google Scholar] [CrossRef]
- Jung, D.-Y.; Koh, E.-K.; Kwon, O.-Y.; Yi, C.-H.; Oh, J.; Weon, J.-H. Effect of Medial Arch Support on Displacement of the Myotendinous Junction of the Gastrocnemius During Standing Wall Stretching. J. Orthop. Sports Phys. Ther. 2009, 39, 867–874. [Google Scholar] [CrossRef] [Green Version]
- Baker, R.; McGinley, J.L.; Schwartz, M.H.; Beynon, S.; Rozumalski, A.; Graham, H.K.; Tirosh, O. The Gait Profile Score and Movement Analysis Profile. Gait Posture 2009, 30, 265–269. [Google Scholar] [CrossRef]
- Chan, Y.H. Biostatistics 101: Data presentation. Singap. Med J. 2003, 44, 280–285. [Google Scholar]
- Celletti, C.; Galli, M.; Cimolin, V.; Castori, M.; Tenore, N.; Albertini, G.; Camerota, F. Use of the Gait Profile Score for the evaluation of patients with joint hypermobility syndrome/Ehlers–Danlos syndrome hypermobility type. Res. Dev. Disabil. 2013, 34, 4280–4285. [Google Scholar] [CrossRef] [PubMed]
- Galli, M.; Pacifici, I.; Cimolin, V.; de Pandis, M.F.; Vagnini, A.; le Pera, D.; Sova, I.; Albertini, G.; Stocchi, F.; Franceschini, M. Use of the gait profile score for the quantification of the effects of robot-assisted gait training in patients with Parkinson’s disease. In 2016 IEEE 2nd International Forum on Research and Technologies for Society and Industry Leveraging a better tomorrow (RTSI); Institute of Electrical and Electronics Engineers (IEEE): Piscataway, NJ, USA, 2016; pp. 1–4. [Google Scholar]
- Brockett, C.L.; Chapman, G. Biomechanics of the ankle. Orthop. Trauma 2016, 30, 232–238. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Evans, D. Calcaneo-Valgus Deformity. J. Bone Jt. Surg. Br. Vol. 1975, 57, 270–278. [Google Scholar] [CrossRef]
- Smith, B.; Ashton-Miller, J.A.; Ulrich, B.D. Gait adaptations in response to perturbations in adults with Down syndrome. Gait Posture 2010, 32, 149–154. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Variable | Adolescents (N = 12) | Adults (N = 17) |
|---|---|---|
| Age (years) | 13.8 ± 2.6 | 26.9 ± 8.3 |
| Gender (Male/Female) | 5 (41.7%)/7 (58.3%) | 11 (64.7%)/6 (353%) |
| Weight (kg) | 50.0 ± 13.7 | 59.3 ± 14.2 |
| Height (cm) | 142.5 ± 10.9 | 148.3 ± 9.0 |
| Body mass index (kg/m2) | 24.5 ± 5.1 | 26.7 ± 4.4 |
| Intelligence Quotient | 67.0 ± 11.4 | 69.1 ± 9.3 |
| Parameters | Adolescents (N = 12) | Adults (N = 17) | ||||
|---|---|---|---|---|---|---|
| WB | WSI | p-Value | WB | WSI | p-Value | |
| Right gait cycle (s) | 1.14 ± 0.16 | 1.17 ± 0.11 | 0.295 | 1.26 ± 0.16 | 1.27 ± 0.14 | 0.743 |
| Left gait cycle (s) | 1.14 ± 0.15 | 1.16 ± 0.1 | 0.442 | 1.26 ± 0.15 | 1.28 ± 0.15 | 0.783 |
| Right % stance (as a % of the gait cycle) | 62.95 ± 4.12 | 64.41 ± 3.45 | 0.372 | 62.27 ± 3.62 | 63.54 ± 2.83 | 0.148 |
| Left % stance (as a % of the gait cycle) | 63.20 ± 4.69 | 63.34 ± 2.97 | 0.735 | 62.44 ± 1.79 | 64.02 ± 2.91 | 0.068 |
| Right % double support (as a % of the gait cycle) | 12.83 ± 3.59 | 13.74 ± 3.39 | 0.644 | 12.50 ± 2.54 | 14.07 ± 2.50 | 0.085 |
| Left % double support (as a % of the gait cycle) | 13.00 ± 4.61 | 13.87 ± 2.95 | 0.518 | 12.56 ± 2.38 | 13.9 ± 2.60 | 0.179 |
| Mean velocity (m/s) | 0.75 ± 0.22 | 0.83 ± 0.15 | 0.265 | 0.73 ± 0.20 | 0.79 ± 0.22 | 0.436 |
| Right stride length (m) | 0.85 ± 0.18 | 0.97 ± 0.14 | 0.060 | 0.89 ± 0.18 | 0.99 ± 0.22 | 0.202 |
| Left stride length (m) | 0.84 ± 0.18 | 0.95 ± 0.16 | 0.116 | 0.88 ± 0.18 | 0.98 ± 0.21 | 0.129 |
| Right step length (m) | 0.42 ± 0.09 | 0.48 ± 0.08 | 0.123 | 0.44 ± 0.10 | 0.49 ± 0.10 | 0.185 |
| Left step length (m) | 0.42 ± 0.10 | 0.49 ± 0.08 | 0.069 | 0.44 ± 0.08 | 0.49 ± 0.11 | 0.196 |
| Step width (m) | 0.15 ± 0.06 | 0.14 ± 0.06 | 0.711 | 0.15 ± 0.04 | 0.15 ± 0.06 | 0.850 |
| Parameters | Adolescents (N = 12) | Adults (N = 17) | ||||
|---|---|---|---|---|---|---|
| WB | WSI | p-Value | WB | WSI | p-Value | |
| Right GVS pelvic obliquity (°) | 3.4 ± 1.15 | 3.18 ± 1.28 | 0.552 | 2.59 ± 1.33 | 2.56 ± 1.03 | 0.945 |
| Left GVS pelvic obliquity (°) | 3.38 ± 1.30 | 3.47 ± 1.47 | 0.767 | 2.84 ± 1.09 | 2.6 ± 0.75 | 0.918 |
| Right GVS pelvic tilt (°) | 4.03 ± 3.01 | 5.46 ± 2.88 | 0.138 | 4.89 ± 3.57 | 5.32 ± 3.54 | 0.654 |
| Left GVS pelvic tilt (°) | 4.10 ± 3.06 | 5.60 ± 2.91 | 0.187 | 5.1 ± 3.41 | 5.37 ± 3.41 | 0.809 |
| Right GVS pelvic rotation (°) | 5.04 ± 1.38 | 4.88 ± 1.18 | 0.869 | 3.89 ± 1.24 | 4.83 ± 1.31 | 0.060 |
| Left GVS pelvic rotation (°) | 5.16 ± 2.04 | 5.74 ± 1.98 | 0.598 | 3.84 ± 1.14 | 4.63 ± 1.15 | 0.058 |
| Right GVS hip adduction/abduction (°) | 5.62 ± 2.70 | 5.72 ± 2.96 | 0.947 | 4.57 ± 3.00 | 5.00 ± 3.44 | 0.480 |
| Left GVS hip adduction/abduction (°) | 6.84 ± 3.23 | 7.27 ± 3.56 | 0.921 | 4.11 ± 2.28 | 5.16 ± 3.55 | 0.293 |
| Right GVS hip flexion/extension (°) | 9.25 ± 4.62 | 9.67 ± 5.44 | 1.000 | 9.31 ± 4.42 | 9.60 ± 4.28 | 0.904 |
| Left GVS hip flexion/extension (°) | 9.92 ± 4.26 | 10.06 ± 5.12 | 0.921 | 9.06 ± 3.44 | 9.08 ± 4.50 | 0.718 |
| Right GVS hip rotation (°) | 11.27 ± 6.5 | 10.64 ± 4.61 | 1.000 | 14.53 ± 11.43 | 14.31 ± 10.98 | 0.836 |
| Left GVS hip rotation (°) | 15.84 ± 6.97 | 17.5 ± 10.38 | 0.817 | 12.29 ± 7.06 | 11.91 ± 7.76 | 0.986 |
| Right GVS knee flexion/extension (°) | 10.81 ± 5.6 | 10.65 ± 3.87 | 0.817 | 12.93 ± 5.42 | 12.25 ± 5.48 | 0.642 |
| Left GVS knee flexion/extension (°) | 12.55 ± 5.49 | 10.74 ± 3.37 | 0.510 | 12.55 ± 5.86 | 11.35 ± 6.34 | 0.502 |
| Right GVS ankle dorsi/plantarflexion (°) | 8.50 ± 3.43 | 9.15 ± 2.86 | 0.644 | 6.74 ± 1.71 | 7.37 ± 2.34 | 0.642 |
| Left GVS ankle dorsi/plantarflexion (°) | 8.08 ± 3.08 | 8.82 ± 3.56 | 0.531 | 6.74 ± 2.04 | 7.87 ± 2.85 | 0.191 |
| Right GVS foot progression (°) | 17.75 ± 6.19 | 9.98 ± 3.69 | 0.008 | 14.3 ± 7.13 | 10.99 ± 6.19 | 0.191 |
| Left GVS foot progression (°) | 19.20 ± 8.06 | 11.71 ± 4.86 | 0.027 | 15.34 ± 7.84 | 10.81 ± 6.06 | 0.063 |
| Right GPS (°) | 10.17 ± 1.86 | 9.03 ± 1.63 | 0.124 | 10.21 ± 3.35 | 9.64 ± 3.43 | 0.705 |
| Left GPS (°) | 11.49 ± 2.26 | 10.65 ± 2.17 | 0.207 | 9.63 ± 3.02 | 9.07 ± 2.71 | 0.558 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Galafate, D.; Pournajaf, S.; Condoluci, C.; Goffredo, M.; Di Girolamo, G.; Manzia, C.M.; Pellicciari, L.; Franceschini, M.; Galli, M. Bilateral Foot Orthoses Elicit Changes in Gait Kinematics of Adolescents with Down Syndrome with Flatfoot. Int. J. Environ. Res. Public Health 2020, 17, 4994. https://doi.org/10.3390/ijerph17144994
Galafate D, Pournajaf S, Condoluci C, Goffredo M, Di Girolamo G, Manzia CM, Pellicciari L, Franceschini M, Galli M. Bilateral Foot Orthoses Elicit Changes in Gait Kinematics of Adolescents with Down Syndrome with Flatfoot. International Journal of Environmental Research and Public Health. 2020; 17(14):4994. https://doi.org/10.3390/ijerph17144994
Chicago/Turabian StyleGalafate, Daniele, Sanaz Pournajaf, Claudia Condoluci, Michela Goffredo, Gabriella Di Girolamo, Carlotta Maria Manzia, Leonardo Pellicciari, Marco Franceschini, and Manuela Galli. 2020. "Bilateral Foot Orthoses Elicit Changes in Gait Kinematics of Adolescents with Down Syndrome with Flatfoot" International Journal of Environmental Research and Public Health 17, no. 14: 4994. https://doi.org/10.3390/ijerph17144994
APA StyleGalafate, D., Pournajaf, S., Condoluci, C., Goffredo, M., Di Girolamo, G., Manzia, C. M., Pellicciari, L., Franceschini, M., & Galli, M. (2020). Bilateral Foot Orthoses Elicit Changes in Gait Kinematics of Adolescents with Down Syndrome with Flatfoot. International Journal of Environmental Research and Public Health, 17(14), 4994. https://doi.org/10.3390/ijerph17144994







