The Effects of Indoor Pollutants Exposure on Allergy and Lung Inflammation: An Activation State of Neutrophils and Eosinophils in Sputum
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. FeNO Assessment and Allergy Skin Test
2.3. Sputum Induction and Processing
2.4. Flow Cytometry
2.5. Assessment of Indoor Air Quality in Classrooms and Building Inspection
2.6. Ethical Statement
2.7. Data Analysis
3. Results
3.1. Data Analysis for the Personal and Clinical Characteristics of School Children
3.2. Levels of Indoor Pollutants and Building Inspection Data
3.3. Chemometrics Analysis of the Biomarkers and Indoor Air Pollutants
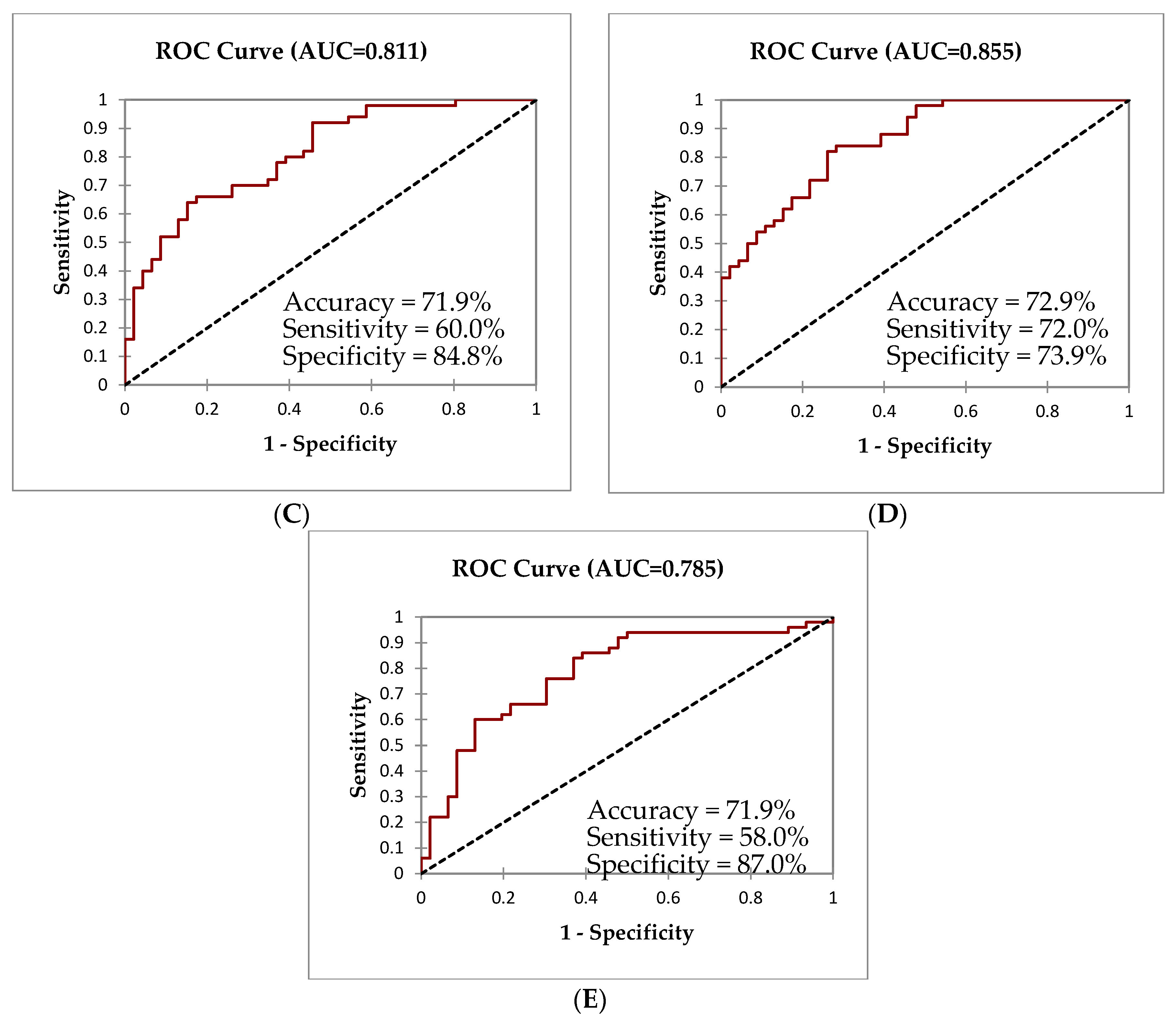
3.4. Binary Logistic Regression (LR)
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Naja, A.S.; Permaul, P.; Phipatanakul, W. Taming Asthma in School-Aged Children: A Comprehensive Review. J. Allergy Clin. Immunol. Pract. 2018, 6, 726–735. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, F.; Hossain, S.; Hossain, S.; Naieum, A.; Fakhruddin, M. Impact of Household Air Pollution on Human Health: Source Identification and Systematic Management Approach. SN Appl. Sci. 2019, 1, 1–19. [Google Scholar] [CrossRef] [Green Version]
- Gaikwad, A.; Shivhare, N. Indoor Air Pollution—A Threat. Int. J. Sci. Res. Rev. 2019, 7, 1463–1467. [Google Scholar]
- Tiotiu, A. Biomarkers in Asthma: State of the Art. Asthma Res. Pract. 2018, 4, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Carr, F. Use of Biomarkers to Identify Phenotypes and Endotypes of Severe Asthma. Ann. Allergy Asthma Immunol. 2018, 121, 414–420. [Google Scholar] [CrossRef] [Green Version]
- Licari, A.; Castagnoli, R. Asthma Endotyping and Biomarkers in Childhood Asthma. Pediatr. Allergy Immunol. Pulmonol. 2018, 31, 44–56. [Google Scholar] [CrossRef] [Green Version]
- Germic, N.; Frangez, Z.; Yousefi, S.; Simon, H.-U. Regulation of the Innate Immune System by Autophagy: Neutrophils, Eosinophils, Mast Cells, NK Cells. Cell Death Differ. 2019, 26, 703–714. [Google Scholar] [CrossRef]
- Grunwell, J.R.; Stephenson, S.T.; Tirouvanziam, R.; Brown, L.A.S. Children with Neutrophil-Predominant Severe Asthma Have Proinflammatory Neutrophils With Enhanced Survival and Impaired Clearance. J. Allergy Clin. Immunol. Pract. 2019, 7, 516–525.e6. [Google Scholar] [CrossRef]
- Johansson, M.W. Activation States of Blood Eosinophils in Asthma. Clin. Exp. Allergy 2014, 44, 482–498. [Google Scholar] [CrossRef] [Green Version]
- Kämpe, M.; Stolt, I.; Lampinen, M.; Janson, C.; Stålenheim, G.; Carlson, M. Patients with Allergic Rhinitis and Allergic Asthma Share the Same Pattern of Eosinophil and Neutrophil Degranulation after Allergen Challenge. Clin. Mol. Allergy 2011, 9, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Cowland, J.B.; Borregaard, N. Granulopoiesis and Granules of Human Neutrophils. Immunol. Rev. 2016, 273, 11–28. [Google Scholar] [CrossRef]
- Zhao, Y.; Zhang, H.; Yang, X.; Zhang, Y.; Feng, S.; Yan, X. Fine Particulate Matter (PM2.5) Enhances Airway Hyperresponsiveness (AHR) by Inducing Necroptosis in BALB/c Mice. Environ. Toxicol. Pharmacol. 2019, 68, 155–163. [Google Scholar] [CrossRef]
- Hodgkins, S.R.; Ather, J.L.; Paveglio, S.A.; Allard, J.L.; Leclair, L.A.W.; Suratt, B.T.; Boyson, J.E.; Poynter, M.E. NO2 Inhalation Induces Maturation of Pulmonary CD11c+ Cells That Promote Antigen-Specific CD4+ T Cell Polarization. Respir. Res. 2010, 11, 1–18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Agache, I.; Akdis, C.A.; Agache, I.; Akdis, C.A. Precision Medicine and Phenotypes, Endotypes, Genotypes, Regiotypes, and Theratypes. J. Clin. Investig. 2019, 129, 1493–1503. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barnes, P.J. Targeting Cytokines to Treat Asthma and Chronic Obstructive Pulmonary Disease. Nat. Rev. Immunol. 2018, 18, 454–466. [Google Scholar] [CrossRef] [PubMed]
- Hanif, T.; Laulajainen-Hongisto, A.; Luukkainen, A.; Numminen, J.; Kääriäinen, J.; Myller, J.; Kalogjera, L.; Huhtala, H.; Kankainen, M.; Renkonen, R.; et al. Hierarchical Clustering in Evaluating Inflammatory Upper Airway Phenotypes; Increased Symptoms in Adults with Allergic Multimorbidity. Asian Pac. J. Allergy Immunol. 2019, 1–10. [Google Scholar] [CrossRef]
- Tinnevelt, G.H.; Jansen, J.J. Resolving Complex Hierarchies in Chemical Mixtures: How Chemometrics May Serve in Understanding the Immune System. Faraday Discuss. 2019, 218, 317–338. [Google Scholar] [CrossRef] [Green Version]
- Kelly, R.S.; Mcgeachie, M.J.; Lee-sarwar, K.A.; Kachroo, P.; Chu, S.H.; Virkud, Y.V.; Huang, M.; Litonjua, A.A.; Weiss, S.T.; Lasky-Su, J. Partial Least Squares Discriminant Analysis and Bayesian Networks for Metabolomic Prediction of Childhood Asthma. Metabolites 2018, 8, 68. [Google Scholar] [CrossRef] [Green Version]
- Hilvering, B.; Vijverberg, S.J.H.; Jansen, J.J.; Houben, L.; Schweizer, R.C.; Go, S.; Xue, L.; Pavord, I.D.; Lammers, J.-W.J.; Koenderman, L. Diagnosing Eosinophilic Asthma Using a Multivariate Prediction Model Based on Blood Granulocyte Responsiveness. Allergy 2017, 72, 1202–1211. [Google Scholar] [CrossRef]
- Norback, D.; Hashim, J.H.; Hashim, Z.; Cai, G.-H.; Sooria, V.; Ismail, S.A.; Wieslander, G. Respiratory Symptoms and Fractional Exhaled Nitric Oxide (FeNO) among Students in Penang, Malaysia in Relation to Sign of Dampness at School and Funfal DNA in School Dust. Sci. Total Environ. 2017, 577, 148–154. [Google Scholar] [CrossRef] [Green Version]
- Zhao, Z.; Sebastian, A.; Larsson, L.; Wang, Z.; Zhang, Z.; Norback, D. Asthmatic Symptoms among Pupils in Relation to Microbial Dust Exposure in Schools in Taiyuan, China. Pediatr. Allergy Immunol. 2008, 19, 455–465. [Google Scholar] [CrossRef] [PubMed]
- Dweik, R.A.; Boggs, P.B.; Erzurum, S.C.; Irvin, C.G.; Leigh, M.W.; Lundberg, J.O.; Olin, A.; Plummer, A.L.; Taylor, D.R. American Thoracic Society Documents An Official ATS Clinical Practice Guideline: Interpretation of Exhaled Nitric Oxide Levels (FENO) for Clinical Applications. Am. J. Respir. Crit. Care Med. 2011, 184, 602–615. [Google Scholar] [CrossRef] [Green Version]
- Australasian Society of Clinical Immunology and Allergy (ASCIA). Skin Prick Testing for the Diagnosis of Allergic Disease—A Manual for Practitioners. Available online: https://www.allergy.org.au/images/stories/pospapers/ASCIA_SPT_Manual_March_2016.pdf (accessed on 14 January 2018).
- Weiszhar, Z.; Horvath, I. Induced Sputum Analysis: Step by Step. Breathe 2013, 9, 300–306. [Google Scholar] [CrossRef] [Green Version]
- Lay, J.C.; Peden, D.B.; Alexis, N.E. Flow Cytometry of Sputum: Assessing Inflammation and Immune Response Elements in the Bronchial Airways. Inhal. Toxicol. 2011, 23, 392–406. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Ruiter, K.; Van Staveren, S.; Hilvering, B.; Knol, E.; Vrisekoop, N.; Koenderman, L.; Yazdanbakhsh, M. A Field-Applicable Method for Flow Cytometric Analysis of Granulocyte Activation: Cryopreservation of Fixed Granulocytes. Cytom. Part A J. Quant. Cell Sci. 2018, 93, 540–547. [Google Scholar] [CrossRef] [PubMed]
- Duan, M.; Steinfort, D.P.; Smallwood, D.; Hew, M.; Chen, W.; Ernst, M.; Irving, L.B.; Anderson, G.P. CD11b Immunophenotyping Identifies Inflammatory Profiles in the Mouse and Human Lungs. Mucosal Immunol. 2016, 9, 550–563. [Google Scholar] [CrossRef] [Green Version]
- Tak, T.; Hilvering, B.; Tesselaar, K. Similar Activation State of Neutrophils in Sputum of Asthma Patients Irrespective of Sputum Eosinophilia. Clin. Exp. Immunol. 2015, 182, 204–212. [Google Scholar] [CrossRef] [Green Version]
- Maestre-Batlle, D.; Pena, O.M.; Hirota, J.A.; Gunawan, E.; Rider, C.F.; Sutherland, D.; Alexis, N.E.; Carlsten, C. Novel Flow Cytometry Approach to Identify Bronchial Epithelial Cells from Healthy Human Airways. Sci. Rep. 2017, 7, 1–9. [Google Scholar] [CrossRef]
- Suhaimi, N.F.; Jalaludin, J.; Bakar, S.A. Cysteinyl Leukotrienes as Biomarkers of Effect in Linking Exposure to Air Pollutants and Respiratory Inflammation among School Children. Ann. Trop. Med. Public Health 2017, 10, 423–431. [Google Scholar]
- Norback, D.; Markowicz, P.; Cai, G.; Hashim, Z.; Ali, F.; Zheng, Y.; Lai, X.; Spangfort, M.D.; Larsson, L.; Hashim, J.H. Endotoxin, Ergosterol, Fungal DNA and Allergens in Dust from Schools in Johor Bahru, Malaysia—Associations with Asthma and Respiratory Infections in Pupils. PLoS ONE 2014, 9, e88303. [Google Scholar] [CrossRef]
- Kamaruddin, A.S.; Jalaludin, J.; Choo, C.P. Indoor Air Quality and Its Association with Respiratory Health among Malay Preschool Children in Shah Alam and Hulu Langat, Selangor. Adv. Environ. Biol. 2015, 9, 17–26. [Google Scholar]
- Foldvary, V.; Beko, G.; Langer, S.; Arrhenius, K.; Petras, D. Effect of Energy Renovation on Indoor Air Quality in Multifamily Residential Buildings in Slovakia. Build. Environ. 2017, 122, 363–372. [Google Scholar] [CrossRef] [Green Version]
- Cai, G.; Hashim, J.H.; Hashim, Z.; Ali, F.; Bloom, E.; Larsson, L.; Lampa, E.; Norback, D. Fungal DNA, Allergens, Mycotoxins and Associations with Asthmatic Symptoms among Pupils in Schools from Johor Bahru, Malaysia. Pediatr. Allergy Immunol. 2011, 22, 290–297. [Google Scholar] [CrossRef] [PubMed]
- Szymanska, E.; Saccenti, E.; Smilde, A.K.; Westerhuis, J.A. Double-Check: Validation of Diagnostic Statistics for PLS-DA Models in Metabolomics Studies. Metabolomics 2012, 8, S3–S16. [Google Scholar] [CrossRef] [Green Version]
- Jolliffe, I.T.; Cadima, J. Principal Component Analysis: A Review and Recent Developments. Philos. Trans. R. Soc. A 2016, 374, 1–16. [Google Scholar] [CrossRef]
- Kim, H.; Eckel, S.P.; Kim, J.H.; Gilliland, F.D. Exhaled NO: Determinants and Clinical Application in Children With Allergic Airway Disease. Allergy Asthma Immunol. Res. 2016, 8, 12–21. [Google Scholar] [CrossRef] [Green Version]
- Xu, F.; Zou, Z.; Yan, S.; Li, F.; Kan, H.; Dan, N.; Gunilla, W.; Xu, J.; Zhao, Z. Fractional Exhaled Nitric Xide in Relation to Asthma, Allergic Rhinitis, and Atopic Dermatitis in Chinese Children. J. Asthma 2011, 48, 1001–1006. [Google Scholar] [CrossRef]
- Ma’pol, A.; Hashim, J.H.; Norbäck, D.; Weislander, G.; Hashim, Z.; Isa, Z.M. FeNO Level and Allergy Status among School Children in Terengganu, Malaysia. J. Asthma 2019, 3, 1–18. [Google Scholar] [CrossRef]
- Norbäck, D.; Hisham, J.; Hashim, Z.; Sooria, V.; Aizat, S.; Wieslander, G. Ocular Symptoms and Tear Film Break up Time (BUT) among Junior High School Students in Penang, Malaysia—Associations with Fungal DNA in School Dust. Int. J. Hyg. Environ. Health 2017, 220, 697–703. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, D.; Huang, Z.; Huang, Y. Clinical Analysis of Fractional Exhaled and Nasal Nitric Oxide in Allergic Rhinitis Children. J. Allergy Ther. 2015, 6, 1–4. [Google Scholar] [CrossRef] [Green Version]
- Carlsen, H.K.; Boman, P.; Bjor, B.; Olin, A.-C.; Forsberg, B. Coarse Fraction Particle Matter and Exhaled Nitric Oxide in Non-Asthmatic Children. Int. J. Environ. Res. Public Health 2016, 13, 621. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kamaruddin, A.S.; Jalaludin, J.; Hamedon, T.R.; Hisamuddin, N.H. FeNO as a Biomarker for Airway Inflammation Due to Exposure to Air Pollutants among School Children Nearby Industrial Areas in Terengganu. Pertanika J. Sci. Technol. 2019, 27, 589–600. [Google Scholar]
- Gong, J.; Zhu, T.; Hu, M.; Wu, Z.; Zhang, J.J. Different Metrics (Number, Surface Area, and Volume Concentration) of Urban Particles with Varying Sizes in Relation to Fractional Exhaled Nitric Oxide (FeNO). J. Thorac. Dis. 2019, 11, 1714–1726. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Wang, W.; Niu, Y.; Xia, Y.; Lei, X.; Huo, J. The Effects of Fine Particulate Matter Constituents on Exhaled Nitric Oxide and DNA Methylation in the Arginase—Nitric Oxide Synthase Pathway. Environ. Int. 2019, 131, 105019. [Google Scholar] [CrossRef] [PubMed]
- Salam, M.T.; Byun, H.; Lurmann, F.; Breton, C.V.; Wang, X.; Eckel, S.P.; Gilliland, F.D.; Angeles, L. Genetic and Epigenetic Variations in Inducible Nitric Oxide Synthase Promoter, Particulate Pollution, and Exhaled Nitric Oxide Levels in Children. J. Allergy Clin. Immunol. 2012, 129, 232–239.e7. [Google Scholar] [CrossRef] [Green Version]
- ASHRAE. Ventilation for Acceptable Indoor Air Quality; American Society of Heating, Refrigerating and Air-Conditioning Engineers, Inc.: Atlanta, GA, USA, 2001. [Google Scholar]
- World Health Organization (WHO). Air Quality Guidelines—Global Update 2005; World Health Organizantion Regional Office for Europe: Copenhagen, Denmark, 2006. [Google Scholar]
- Schibuola, L.; Scarpa, M.; Tambani, C. Natural Ventilation Level Assessment in a School Building by CO2 Concentration Measures. Energy Procedia 2016, 101, 257–264. [Google Scholar] [CrossRef]
- Silvestre, C.M.; Andre, P.; Michel, T. Air Temperature and CO2 Variations in a Naturally Ventilated Classroom under a Nordic Climate. In Proceedings of the PLEA2009 26th Conference on Passive and Low Energy Architecture, Quebec, ON, Canada, 22–24 June 2009; pp. 1–6. [Google Scholar]
- Norbäck, D.; Hisham, J.; Hashim, Z.; Ali, F. Volatile Organic Compounds (VOC), Formaldehyde and Nitrogen Dioxide (NO2) in Schools in Johor Bahru, Malaysia: Associations with Rhinitis, Ocular, Throat and Dermal Symptoms, Headache and Fatigue. Sci. Total Environ. 2017, 592, 153–160. [Google Scholar] [CrossRef] [Green Version]
- Abidin, E.Z.; Semple, S.; Rasdi, I.; Ismail, S.N.S.; Ayres, J.G. The Relationship between Air Pollution and Asthma in Malaysian Schoolchildren. Air Qual. Atmos. Health 2014, 7, 421–432. [Google Scholar] [CrossRef]
- Mohamed, N.; Sulaiman, L.H.; Zakaria, T.A.; Kamarudin, A.S.; Rahim, D.A. Health Risk Assessment of PM10 Exposure among School Children and the Proposed API Level for Closing the School during Haze in Malaysia. Int. J. Public Health Res. 2016, 6, 685–694. [Google Scholar]
- Maestrelli, P.; De Fina, O.; Bertin, T.; Papiris, S.; Ruggieri, M.P.; Saetta, M.; Mapp, C.E.; Fabbri, L.M. Integrin Expression on Neutrophils and Mononuclear Cells in Blood and Induced Sputum in Stable Asthma. Allergy 1999, 54, 1303–1308. [Google Scholar] [CrossRef]
- Wark, P.; Gibson, P.; Fakes, K. Induced Sputum Eosinophils in the Assessment of Asthma and Chronic Cough. Respirology 2000, 5, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Belda, J.; Leigh, R.; Parameswaran, K.; Byrne, P.M.O.; Sears, M.R.; Hargreave, F.E. Induced Sputum Cell Counts in Healthy Adults. Am. J. Respir. Crit. Care Med. 2000, 161, 475–478. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Giudice, M.M.; Pedulla, M.; Brunese, F.P.; Capristo, A.F.; Capristo, C.; Tosca, M.A.; Leonardf, S.; Ciprandp, G. Neutrophilic Cells in Sputum of Allergic Asthmatic Children. Eur. J. Inflamm. 2010, 8, 151–156. [Google Scholar] [CrossRef]
- Hargreave, F.E.; Leigh, R. Induced Sputum, Eosinophilic Bronchitis, and Chronic Obstructive Pulmonary Disease. Am. J. Respir. Crit. Care Med. 1999, 160, S53–S57. [Google Scholar] [CrossRef]
- Kim, K.; Hwang, S.M.; Kim, S.M.; Park, S.W.; Jung, Y. Terminally Differentiating Eosinophils Express Neutrophil Primary Granule Proteins as Well as Eosinophil-Specific Granule Proteins in a Temporal Manner. Immune Netw. 2017, 17, 410–423. [Google Scholar] [CrossRef] [Green Version]
- Carr, T.F.; Berdnikovs, S.; Simon, H.-U.; Bochner, B.S.; Rosenwasser, L.J. Eosinophilic Bioactivities in Severe Asthma. World Allergy Organ. J. 2016, 9, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Berends, C.; Dijkhuizen, B.; Monchy, G.R.D.E.; Gerritsen, J.; Kauffman, H.F. Expression of CD35 (CRl) and CDllb (CR3) on Circulating Neutrophils and Eosinophils from Allergic Asthmatic Children. Clin. Exp. Allergy 1993, 23, 926–933. [Google Scholar] [CrossRef]
- Dallaire, M.; Ferland, C.; Page, N.; Lavigne, S.; Davoine, F.; Laviolette, M. Endothelial Cells Modulate Eosinophil Surface Markers and Mediator Release. Eur. Respir. J. 2003, 21, 918–924. [Google Scholar] [CrossRef] [Green Version]
- Lewis, S.M.; Treacher, D.F.; Edgeworth, J.; Mahalingam, G.; Brown, C.S.; Mare, T.A.; Stacey, M.; Beale, R.; Brown, K.A. Expression of CD11c and EMR2 on Neutrophils: Potential Diagnostic Biomarkers for Sepsis and Systemic Inflammation. Clin. Exp. Immunol. 2015, 182, 184–194. [Google Scholar] [CrossRef] [Green Version]
- Ducker, P.; Skubitz, K. Subcellular Neutrophils Localization of CD66, CD67, and NCA in Human Neutrophils. J. Leukoc. Biol. 1992, 52, 11–16. [Google Scholar] [CrossRef]
- Vidal, S.; Bellido-Casado, J.; Granel, C.; Crespo, A.; Plaza, V.; Juárez, C. Immunobiology Flow Cytometry Analysis of Leukocytes in Induced Sputum from Asthmatic Patients. Immunobiology 2012, 217, 692–697. [Google Scholar] [CrossRef]
- Zissler, U.M.; Bieren, J.E.; Jakwerth, C.A.; Chaker, A.M.; Schmidt-Weber, C.B. Current and Future Biomarkers in Allergic Asthma. Eur. J. Allergy Clin. Immunol. 2016, 71, 475–494. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lakschevitz, F.S. Identification of CD Marker Expression and Neutrophil Surface Marker Changes in Health and Disease Using High-Throughput Screening Flow Cytometry. Master’s Thesis, University of Toronto, Toronto, ON, Canada, 2016. [Google Scholar]
- Kinhult, J.; Egesten, A.; Uddman, R.; Cardell, L.O. PACAP Enhances the Expression of CD11b, CD66b and CD63 in Human Neutrophils. Peptides 2002, 23, 1735–1739. [Google Scholar] [CrossRef]
- Jin, C.; Shelburne, C.P.; Li, G.; Riebe, K.J.; Sempowski, G.D.; Foster, W.M.; Abraham, S.N. Particulate Allergens Potentiate Allergic Asthma in Mice through Sustained IgE-Mediated Mast Cell Activation. J. Clin. Investig. 2011, 121, 941–955. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mattsson, E.; Persson, T.; Andersson, P.; Rollof, J.; Egesten, A. Peptidoglycan Induces Mobilization of the Surface Marker for Activation Marker CD66b in Human Neutrophils but Not in Eosinophils. Clin. Diagn. Lab. Immunol. 2003, 10, 485–488. [Google Scholar] [CrossRef] [Green Version]
- Banerjee, A.; Mondal, N.K.; Das, D.; Ray, M.R. Neutrophilic Inflammatory Response and Oxidative Stress in Premenopausal Women Chronically Exposed to Indoor Air Pollution from Biomass Burning. Inflammation 2012, 35, 671–683. [Google Scholar] [CrossRef]
- Ishii, H.; Hayashi, S.; Hogg, J.C.; Fujii, T.; Goto, Y.; Sakamoto, N.; Mukae, H.; Vincent, R.; Van Eeden, S.F. Alveolar Macrophage-Epithelial Cell Interaction Following Exposure to Atmospheric Particles Induces the Release of Mediators Involved in Monocyte Mobilization and Recruitment. Respir. Res. 2005, 6, 1–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hiraiwa, K.; Van Eeden, S.F. Contribution of Lung Macrophages to the Inflammatory Responses Induced by Exposure to Air Pollutants. Mediat. Inflamm. 2013, 2013, 1–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pillay, J.; Kamp, V.M.; Pennings, M.; Oudijk, E.; Leenen, L.P.; Ulfman, L.H. Acute-Phase Concentrations of Soluble Fibrinogen Inhibit Neutrophil Adhesion under Flow Conditions in Vitro through Interactions with ICAM-1 and MAC-1 (CD11b/ CD18). J. Thromb. Haemost. 2013, 11, 1172–1182. [Google Scholar] [CrossRef] [PubMed]
- Medoff, B.D.; Seung, E.; Hong, S.; Thomas, Y.; Sandall, B.P.; Duffield, J.S.; Kuperman, A.; Erle, D.J.; Luster, A.D.; Medoff, B.D.; et al. CD11b+ Myeloid Cells Are the Key Mediators of Th2 Cell Homing into the Airway in Allergic Inflammation. J. Immunol. 2009, 182, 623–635. [Google Scholar] [CrossRef] [Green Version]
- Guo, Y.; Hong, C.; Liu, Y.; Chen, H.; Huang, X.; Hong, M. Diagnostic Value of Fractional Exhaled Nitric Oxide for Asthma-Chronic Obstructive Pulmonary Disease Overlap Syndrome. Medicine (Baltimore) 2018, 97, 1–7. [Google Scholar] [CrossRef]
- Kobayashi, S.; Hanagama, M.; Yamanda, S.; Ishida, M.; Yanai, M. Inflammatory Biomarkers in Asthma-COPD Overlap Syndrome. Int. J. COPD 2016, 11, 2117–2123. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alving, K.; Malinovschi, A. Basic Aspects of Exhaled Nitric Oxide. In European Respiratory Monograph: Exhaled Biomarker; Horvath, I., DeJongste, J.C., Eds.; European Respiratory Society: Sheffield, UK, 2010; pp. 1–31. [Google Scholar] [CrossRef]
- Pelletier, M.; Maggi, L.; Micheletti, A.; Lazzeri, E.; Tamassia, N.; Costantini, C.; Cosmi, L.; Lunardi, C.; Annunziato, F.; Romagnani, S.; et al. Evidence for a Cross-Talk between Human Neutrophils and Th17 Cells. Blood 2010, 115, 335–343. [Google Scholar] [CrossRef]
- Ray, A.; Kolls, J.K. Neutrophilic Inflammation in Asthma and Association with Disease Severity. Trends Immunol. 2017, 38, 942–954. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Flexeder, C.; Fuertes, E.; Cyrys, J.; Bauer, C.; Koletzko, S.; Hoffmann, B.; Von Berg, A.; Heinrich, J. Effects of Air Pollution on Exhaled Nitric Oxide in Children: Results from the GINIplus and LISAplus Studies. Int. J. Hyg. Environ. Health 2014, 217, 483–491. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Hu, B.; Wang, L.; Wu, F.; Gao, W.; Wang, Y. Seasonal and Diurnal Variation in Particulate Matter (PM10 and PM2.5) at an Urban Site of Beijing: Analyses from a 9-Year Study. Environ. Sci. Pollut. Res. 2015, 22, 627–642. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Guinot, B.; Sai, S.; Ho, H.; Li, Y.; Cao, J.; Shen, Z.; Niu, X.; Zhao, Z.; Liu, S. Evaluation on Exposures to Particulate Matter at a Junior Secondary School: A Comprehensive Study on Health Risks and Effective Inflammatory Responses in Northwestern China. Environ. Geochem. Health 2017, 1–15. [Google Scholar] [CrossRef]
- Weschler, C.J.; Wells, J.R.; Poppendieck, D.; Hubbard, H.; Pearce, T.A. Workgroup Report: Indoor Chemistry and Health. Environ. Health Perspect. 2006, 114, 442–446. [Google Scholar] [CrossRef] [Green Version]
- Salthammer, T. Formaldehyde Sources, Formaldehyde Concentrations and Air Exchange Rates in European Housings. Build. Environ. 2019, 150, 219–232. [Google Scholar] [CrossRef]
- Hua, A.K. Applied Chemometric Approach in Identification Sources of Air Quality Pattern in Selangor, Malaysia. Sains Malays. 2018, 47, 471–479. [Google Scholar] [CrossRef]
- Askariyeh, M.H.; Venugopal, M.; Khreis, H.; Birt, A. Near-Road Traffic-Related Air Pollution: Resuspended PM2.5 from Highways and Arterials. Int. J. Environ. Res. Public Health 2020, 17, 2851. [Google Scholar] [CrossRef] [PubMed]
- Othman, M.; Latif, M.T.; Matsumi, Y. The Exposure of Children to PM2.5 and Dust in Indoor and Outdoor School Classrooms in Kuala Lumpur City Centre. Ecotoxicol. Environ. Saf. 2019, 170, 739–749. [Google Scholar] [CrossRef] [PubMed]
- Rufo, J.C.; Madureira, J.; Fernandes, E.O.; Moreira, A.; Rufo, C.; Roberto, R. Volatile Organic Compounds in Asthma Diagnosis: A Systematic Review and Meta-Analysis. Allergy 2016, 71, 175–188. [Google Scholar] [CrossRef] [PubMed] [Green Version]




| Characteristics | Doctor Diagnosed Asthma (n = 50) | Healthy (n = 46) | p-Value |
|---|---|---|---|
| Female (%) | 44.2 | 55.8 | 0.094 |
| Male (%) | 61.4 | 38.6 | |
| Atopic (%) | 65.0 | 35.0 | <0.001 ** |
| Non atopic (%) | 30.6 | 69.4 | |
| Parental with asthma/allergy (%) | 65.9 | 34.1 | 0.020 * |
| Parental without asthma/allergy (%) | 41.8 | 58.2 | |
| School area—urban (%) | 60.4 | 39.6 | 0.102 |
| School area—suburban (%) | 43.8 | 56.3 | |
| Clinical characteristics | |||
| FeNO levels (ppb) | 56 (66.5) | 23 (32.3) | 0.002 * |
| Eosinophil count (%) | 11.6 (11.3) | 10.2 (9.2) | 0.259 |
| Neutrophil count (%) | 11.6 (5.0) | 13.4 (14.0) | 0.130 |
| Parameter | Urban n = 16 | Suburban n = 16 | p-Value | ||||
|---|---|---|---|---|---|---|---|
| Median (IQR) | Min | Max | Median (IQR) | Min | Max | ||
| Temperature (°C) | 29.0 (2.0) | 28.0 | 32.0 | 27.5 (1.0) | 27.0 | 28.0 | <0.001 ** |
| Relative Humidity (%) | 74.7 (9.5) | 63.6 | 88.1 | 81.4 (7.5) | 74.8 | 88.1 | <0.001 ** |
| Formaldehyde (mg/m3) | 13.2 (9.3) | 5.2 | 19.5 | 3.1 (5.2) | 2.1 | 15.9 | <0.001 ** |
| CO2 (ppm) | 453.0 (34.5) | 417.0 | 468.0 | 455.5 (25.5) | 402.0 | 471.0 | 0.462 |
| NO2 (µg/m3) | 32.0 (7.0) | 15.0 | 45.0 | 19.0 (22.5) | 16.0 | 48.0 | <0.001 ** |
| PM2.5 (µg/m3) | 24.6 (2.4) | 17.9 | 26.5 | 22.0 (1.9) | 16.8 | 26.9 | <0.001 ** |
| PM10 (µg/m3) | 41.6 (7.5) | 34.7 | 48.0 | 37.0 (4.9) | 32.3 | 44.9 | <0.001 ** |
| Biomarkers and Indoor Pollutants | Eosinophils | Neutrophils | ||||||
|---|---|---|---|---|---|---|---|---|
| F1 | F2 | F3 | F4 | F1 | F2 | F3 | F4 | |
| FeNO levels | 0.194 | −0.575 | 0.501 | 0.235 | 0.653 | −0.306 | −0.108 | −0.120 |
| CD11b | 0.528 | 0.083 | −0.398 | 0.059 | 0.571 | −0.053 | 0.175 | 0.685 |
| CD35 | 0.559 | 0.129 | 0.432 | 0.348 | 0.337 | 0.213 | 0.612 | −0.445 |
| CD63 | −0.193 | 0.379 | 0.070 | 0.732 | −0.665 | 0.394 | 0.117 | −0.288 |
| CD66b | 0.285 | −0.465 | 0.561 | −0.419 | 0.727 | 0.067 | −0.235 | −0.039 |
| CO2 | −0.346 | −0.329 | −0.456 | 0.084 | −0.287 | −0.506 | 0.123 | −0.360 |
| NO2 | 0.771 | −0.116 | −0.118 | 0.375 | 0.470 | 0.301 | 0.657 | −0.412 |
| PM10 | 0.102 | 0.582 | 0.584 | −0.035 | 0.074 | 0.684 | −0.523 | −0.047 |
| PM2.5 | −0.053 | 0.699 | −0.061 | −0.490 | −0.409 | 0.503 | −0.099 | 0.502 |
| Formaldehyde | 0.788 | 0.380 | 0.100 | 0.123 | 0.322 | 0.746 | 0.467 | −0.089 |
| Eigenvalue | 2.10 | 1.81 | 1.49 | 1.30 | 2.42 | 1.93 | 1.43 | 1.32 |
| Variability (%) | 21.0 | 18.1 | 14.9 | 13.0 | 24.2 | 19.3 | 14.3 | 13.2 |
| Cumulative % | 21.0 | 39.0 | 54.0 | 67.0 | 24.2 | 43.4 | 57.8 | 71.0 |
| Variable | Β | SE | p-Value | R2 |
|---|---|---|---|---|
| Eosinophils | ||||
| Cluster 1 | ||||
| Constant | −0.860 | 0.409 | 0.035 * | 0.494 |
| FeNO Levels | 0.615 | 0.222 | 0.006 * | |
| CD66b | −0.850 | 0.250 | <0.001 ** | |
| CO2 | 0.457 | 0.191 | 0.016 * | |
| Atopy | 0.893 | 0.377 | 0.018 * | |
| Parental Asthma/Allergy | 0.643 | 0.319 | 0.044 * | |
| Area—Urban | 0.747 | 0.354 | 0.035 * | |
| Cluster 2 | ||||
| Constant | −0.109 | 0.536 | 0.840 | 0.504 |
| CD11b | 0.454 | 0.260 | 0.018 * | |
| NO2 | 1.305 | 0.375 | 0.002 * | |
| Formaldehyde | −0.684 | 0.440 | 0.120 | |
| Atopy | 0.993 | 0.378 | 0.009 * | |
| Parental Asthma/Allergy | 0.916 | 0.424 | 0.031 * | |
| Cluster 3 | ||||
| Constant | −1.387 | 0.462 | 0.003 * | 0.377 |
| CD35 | −0.097 | 0.189 | 0.608 | |
| CD63 | −0.080 | 0.166 | 0.042 * | |
| PM10 | −0.379 | 0.212 | 0.074 | |
| PM2.5 | −0.378 | 0.181 | 0.037 * | |
| Atopy | 0.909 | 0.377 | 0.015 * | |
| Parental Asthma/Allergy | 0.842 | 0.350 | 0.016 * | |
| Neutrophils | ||||
| Cluster 1 | ||||
| Constant | −1.039 | 0.490 | 0.034 * | 0.510 |
| CD35 | −0.054 | 0.169 | 0.751 | |
| CD63 | −0.632 | 0.256 | 0.014 * | |
| CD66b | −1.794 | 0.858 | 0.036 * | |
| CO2 | 0.230 | 0.200 | 0.250 | |
| PM10 | −0.253 | 0.218 | 0.244 | |
| PM2.5 | −0.582 | 0.234 | 0.013 * | |
| Atopy | 1.134 | 0.439 | 0.010 * | |
| Parental Asthma/Allergy | 0.944 | 0.404 | 0.021 * | |
| Area—Urban | 1.348 | 0.514 | 0.009 * | |
| Cluster 3 | ||||
| Constant | −0.876 | 0.432 | 0.042 * | 0.298 |
| FeNO Levels | 0.063 | 0.171 | 0.712 | |
| CD11b | 0.390 | 0.197 | 0.047 * |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mohd Isa, K.N.; Hashim, Z.; Jalaludin, J.; Lung Than, L.T.; Hashim, J.H. The Effects of Indoor Pollutants Exposure on Allergy and Lung Inflammation: An Activation State of Neutrophils and Eosinophils in Sputum. Int. J. Environ. Res. Public Health 2020, 17, 5413. https://doi.org/10.3390/ijerph17155413
Mohd Isa KN, Hashim Z, Jalaludin J, Lung Than LT, Hashim JH. The Effects of Indoor Pollutants Exposure on Allergy and Lung Inflammation: An Activation State of Neutrophils and Eosinophils in Sputum. International Journal of Environmental Research and Public Health. 2020; 17(15):5413. https://doi.org/10.3390/ijerph17155413
Chicago/Turabian StyleMohd Isa, Khairul Nizam, Zailina Hashim, Juliana Jalaludin, Leslie Thian Lung Than, and Jamal Hisham Hashim. 2020. "The Effects of Indoor Pollutants Exposure on Allergy and Lung Inflammation: An Activation State of Neutrophils and Eosinophils in Sputum" International Journal of Environmental Research and Public Health 17, no. 15: 5413. https://doi.org/10.3390/ijerph17155413
APA StyleMohd Isa, K. N., Hashim, Z., Jalaludin, J., Lung Than, L. T., & Hashim, J. H. (2020). The Effects of Indoor Pollutants Exposure on Allergy and Lung Inflammation: An Activation State of Neutrophils and Eosinophils in Sputum. International Journal of Environmental Research and Public Health, 17(15), 5413. https://doi.org/10.3390/ijerph17155413






