Adolescent Endorsement of the “Weak-Not-Sick” Stereotype for Generalised Anxiety Disorder: Associations with Prejudice, Discrimination, and Help-Giving Intentions toward Peers
Abstract
1. Introduction
1.1. Background
1.2. Weak-Not-Sick: Mental Illness Stigma and Anxiety Disorders
1.3. The Present Study
2. Methods
2.1. Participants
2.2. Materials
“Katie is in 5th year. She loves reading, and often swaps books with her best friends from school. However, over the course of the last year, Katie has found it difficult to relax, and feels like she cannot sit still. She can’t stop thinking about the future and whether she will do well in her exams and get into her first-choice course in college, even though her exams are over a year away. When she sits down to study in the evenings she finds it difficult to concentrate on the work, and her teachers have noticed that she often seems distracted during class. Her friends and family have started to notice how tense she is, often about little things. When her mother is late home from work one day, Katie finds herself imagining the worst, that her mother has been in a car accident. She knows that the traffic is heavy and tries to relax, but she can’t stop worrying until her mother gets home safely. Her parents have also noticed that she has been very short-tempered lately, getting angry and slamming doors around the house. She doesn’t even enjoy reading anymore, because she finds her mind drifting toward her worries instead of the words on the page.”
2.3. Procedure
2.4. Data Processing
3. Analysis and Results
3.1. Do Adolescents Endorse the ‘Weak-Not-Sick’ (WNS) Stereotype for Hypothetical Peers Presented with Symptoms of GAD?
3.2. Does Greater Endorsement of the ‘Weak-Not-Sick’ Stereotype for Adolescent Peers with GAD Relate to Greater Prejudice and Discrimination and Less Help-Giving Intentions?
4. Discussion
Implications, Limitations and Directions for Future Research
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- APA. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Publishing: Washington, DC, USA, 2013. [Google Scholar]
- World Health Organization. Depression and Other Common Mental Disorders: Global Health Estimates; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Mendlowicz, M.V.; Stein, M.B. Quality of life in individuals with anxiety disorders. Am. J. Psychiatry 2000, 157, 669–682. [Google Scholar] [CrossRef] [PubMed]
- Wittchen, H.U.; Jacobi, F. Size and burden of mental disorders in Europe—A critical review and appraisal of 27 studies. Eur. Neuropsychopharmacol. 2005, 15, 357–376. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. International Classification of Diseases for Mortality and Morbidity Statistics (11th Revision); World Health Organization: Geneva, Switzerland, 2018; Available online: https://icd.who.int/browse11/l-m/en (accessed on 19 April 2020).
- Kasper, S. Anxiety disorders: Under-diagnosed and insufficiently treated. Int. J. Psychiatry Clin. Pract. 2006, 10 (Suppl. 1), 3–9. [Google Scholar] [CrossRef] [PubMed]
- Johnson, E.M.; Coles, M.E. Failure and delay in treatment-seeking across anxiety disorders. Community Ment. Health J. 2013, 49, 668–674. [Google Scholar] [CrossRef] [PubMed]
- ESEMeD/MHEDEA 2000 Investigators; Alonso, J.; Angermeyer, M.C.; Bernert, S.; Bruffaerts, R.; Brugha, T.S.; Gasquet, I. Use of mental health services in Europe: Results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatr. Scand. 2004, 109, 47–54. [Google Scholar] [CrossRef]
- Mackenzie, C.S.; Reynolds, K.; Cairney, J.; Streiner, D.L.; Sareen, J. Disorder-specific mental health service use for mood and anxiety disorders: Associations with age, sex, and psychiatric comorbidity. Depress. Anxiety 2012, 29, 234–242. [Google Scholar] [CrossRef]
- Benatti, B.; Camuri, G.; Dell’Osso, B.; Cremaschi, L.; Sembira, E.; Palazzo, M.; Oldani, L.; Dobrea, C.; Arici, C.; Primavera, D.; et al. Which factors influence onset and latency to treatment in generalized anxiety disorder, panic disorder, and obsessive–compulsive disorder? Int. Clin. Psychopharmacol. 2016, 31, 347–352. [Google Scholar] [CrossRef]
- Thompson, A.; Issakidis, C.; Hunt, C. Delay to seek treatment for anxiety and mood disorders in an Australian clinical sample. Behav. Chang. 2008, 25, 71–84. [Google Scholar] [CrossRef]
- Craske, M.G.; Stein, M.B. Anxiety. Lancet 2016, 388, 3048–3059. [Google Scholar] [CrossRef]
- Hoffman, D.L.; Dukes, E.M.; Wittchen, H.U. Human and economic burden of generalized anxiety disorder. Depress. Anxiety 2008, 25, 72–90. [Google Scholar] [CrossRef]
- Paus, T.; Keshavan, M.; Giedd, J.N. Why do many psychiatric disorders emerge during adolescence? Nat. Rev. Neurosci. 2008, 9, 947–957. [Google Scholar] [CrossRef]
- World Health Organization. Adolescent Mental Health; World Health Organization: Geneva, Switzerland, 2019; Available online: https://www.who.int/news-room/fact-sheets/detail/adolescent-mental-health (accessed on 21 July 2020).
- Beesdo, K.; Knappe, S.; Pine, D.S. Anxiety and anxiety disorders in children and adolescents: Developmental issues and implications for DSM-V. Psychiatr. Clin. N. Am. 2009, 32, 483–524. [Google Scholar] [CrossRef] [PubMed]
- Woodward, L.J.; Fergusson, D.M. Life course outcomes of young people with anxiety disorders in adolescence. J. Am. Acad. Child Adolesc. Psychiatry 2001, 40, 1086–1093. [Google Scholar] [CrossRef] [PubMed]
- Cannon, M.; Coughlan, H.; Clarke, M.; Harley, M.; Kelleher, I. The Mental Health of Young People in Ireland: A report of the Psychiatric Epidemiology Research across the Lifespan (PERL) Group; Royal College of Surgeons in Ireland: Dublin, Ireland, 2013. [Google Scholar]
- Essau, C.A.; Lewinsohn, P.M.; Olaya, B.; Seeley, J.R. Anxiety disorders in adolescents and psychosocial outcomes at age 30. J. Affect. Disord. 2014, 163, 125–132. [Google Scholar] [CrossRef]
- Wolitzky-Taylor, K.; Dour, H.; Zinbarg, R.; Mineka, S.; Vrshek-Schallhorn, S.; Epstein, A.; Bobova, L.; Griffith, J.; Waters, A.; Nazarian, M.; et al. Experiencing core symptoms of anxiety and unipolar mood disorders in late adolescence predicts disorder onset in early adulthood. Depress. Anxiety 2014, 31, 207–213. [Google Scholar] [CrossRef] [PubMed]
- Merikangas, K.R.; He, J.P.; Burstein, M.; Swendsen, J.; Avenevoli, S.; Case, B.; Georgiades, K.; Heaton, L.; Swanson, S.; Olfson, M. Service utilization for lifetime mental disorders in US adolescents: Results of the National Comorbidity Survey–Adolescent Supplement (NCS-A). J. Am. Acad. Child Adolesc. Psychiatry 2011, 50, 32–45. [Google Scholar] [CrossRef] [PubMed]
- Corrigan, P.W.; Watson, A.C. Understanding the impact of stigma on people with mental illness. World Psychiatry 2002, 1, 16–20. [Google Scholar] [PubMed]
- Silke, C.; Swords, L.; Heary, C. The Development of an Empirical Model of Mental Health Stigma in Adolescents. Psychiatry Res. 2016, 242, 262–270. [Google Scholar] [CrossRef]
- Rickwood, D.; Deane, F.P.; Wilson, C.J.; Ciarrochi, J.V. Young people’s help-seeking for mental health problems. Aust. e-J. Adv. Ment. Health 2005, 4, 1–34. [Google Scholar] [CrossRef]
- Gulliver, A.; Griffiths, K.M.; Christensen, H. Perceived barriers and facilitators to mental health help-seeking in young people: A systematic review. BMC Psychiatry 2010, 10, 113. [Google Scholar] [CrossRef]
- Mukolo, A.; Heflinger, C.A.; Wallston, K.A. The stigma of childhood mental disorders: A conceptual framework. J. Am. Acad. Child Adolesc. Psychiatry 2010, 49, 92–103. [Google Scholar] [PubMed]
- Yap, M.B.; Jorm, A.F. The influence of stigma on first aid actions taken by young people for mental health problems in a close friend or family member: Findings from an Australian national survey of youth. J. Affect. Disord. 2011, 134, 473–477. [Google Scholar] [CrossRef] [PubMed]
- Heary, C.; Hennessy, E.; Swords, L. Stigma associated with disease and disability during childhood and adolescence: A developmental approach. In The Stigma of Disease and Disability: Understanding Causes and Overcoming Injustices; Corrigan, P., Ed.; American Psychological Association: Washington, DC, USA, 2014; pp. 205–222. [Google Scholar]
- Wright, A.; Harris, M.G.; Jorm, A.F.; Cotton, S.M.; Harrigan, S.M.; McGorry, P.D.; Wiggers, J.H.; Hurworth, R.E. Recognition of depression and psychosis by young Australians and their beliefs about treatment. Med. J. Aust. 2005, 183, 18–23. [Google Scholar] [CrossRef] [PubMed]
- Kroger, J. Identity Development: Adolescence through Adulthood; Sage Publications: New York, NY, USA, 2007. [Google Scholar]
- Rubin, K.H.; Bukowski, W.M.; Bowker, J. Children in Peer Groups. In Handbook of Child Psychology and Developmental Science; Lerner, R.M., Bornstein, M.H., Leventhal, T., Eds.; Wiley: Hoboken, NJ, USA, 2015; Volume 4, pp. 175–222. [Google Scholar]
- Amarasuriya, S.D.; Reavley, N.J.; Rossetto, A.; Jorm, A.F. Helping intentions of undergraduates towards their depressed peers: A cross-sectional study in Sri Lanka. BMC Psychiatry 2017, 17, 40. [Google Scholar] [CrossRef]
- Angermeyer, M.C.; Matschinger, H. Public attitude towards psychiatric treatment. Acta Psychiatr. Scand. 1996, 94, 326–336. [Google Scholar] [CrossRef] [PubMed]
- Phelan, J.C.; Link, B.G. The growing belief that people with mental illnesses are violent: The role of the dangerousness criterion for civil commitment. Soc. Psychiatry Psychiatr. Epidemiol. 1998, 33, S7–S12. [Google Scholar] [CrossRef]
- Link, B.G.; Yang, L.H.; Phelan, J.C.; Collins, P.Y. Measuring mental illness stigma. Schizophr. Bull. 2004, 30, 511–541. [Google Scholar] [CrossRef]
- Crisp, A.H.; Gelder, M.G.; Rix, S.; Meltzer, H.I.; Rowlands, O.J. Stigmatisation of people with mental illnesses. Br. J. Psychiatry 2000, 177, 4–7. [Google Scholar] [CrossRef]
- Wood, L.; Birtel, M.; Alsawy, S.; Pyle, M.; Morrison, A. Public perceptions of stigma towards people with schizophrenia, depression, and anxiety. Psychiatry Res. 2014, 220, 604–608. [Google Scholar] [CrossRef]
- Curcio, C.; Corboy, D. Stigma and anxiety disorders: A systematic review. Stigma Health 2020, 5, 125–137. [Google Scholar] [CrossRef]
- Yoshioka, K.; Reavley, N.J.; MacKinnon, A.J.; Jorm, A.F. Stigmatising attitudes towards people with mental disorders: Results from a survey of Japanese high school students. Psychiatry Res. 2014, 215, 229–236. [Google Scholar] [CrossRef] [PubMed]
- Hanlon, H.R.; Swords, L. Overthinkers, attention-seekers and wallflowers: Peer perceptions of clinical anxiety disorders in adolescence. J. Public Ment. Health 2019, 18, 4–13. [Google Scholar] [CrossRef]
- Hennessy, E.; Swords, L.; Heary, C. Children’s understanding of psychological problems displayed by their peers: A review of the literature. Child Care Health Dev. 2008, 34, 4–9. [Google Scholar] [CrossRef] [PubMed]
- Yap, M.B.; Wright, A.; Jorm, A.F. The influence of stigma on young people’s help-seeking intentions and beliefs about the helpfulness of various sources of help. Soc. Psychiatry Psychiatr. Epidemiol. 2011, 46, 1257–1265. [Google Scholar] [CrossRef]
- Reavley, N.J.; Jorm, A.F. Associations between beliefs about the causes of mental disorders and stigmatising attitudes: Results of a national survey of the Australian public. Aust. N. Z. J. Psychiatry 2014, 48, 764–771. [Google Scholar] [CrossRef] [PubMed]
- Kaushik, A.; Kostaki, E.; Kyriakopoulos, M. The stigma of mental illness in children and adolescents: A systematic review. Psychiatry Res. 2016, 243, 469–494. [Google Scholar] [CrossRef]
- Arbanas, G. Adolescents’ attitudes toward schizophrenia, depression, and PTSD. J. Psychosoc. Nurs. Ment. Health Serv. 2008, 46, 45–51. [Google Scholar] [CrossRef]
- Reavley, N.J.; Jorm, A.F. Recognition of mental disorders and beliefs about treatment and outcome: Findings from an Australian national survey of mental health literacy and stigma. Aust. N. Z. J. Psychiatry 2011, 45, 947–956. [Google Scholar] [CrossRef]
- Calear, A.L.; Batterham, P.J.; Griffiths, K.M.; Christensen, H. Generalized anxiety disorder stigma in adolescents: Personal and perceived stigma levels and predictors. Stigma Health 2017, 2, 208–217. [Google Scholar] [CrossRef]
- Batterham, P.J.; Griffiths, K.M.; Barney, L.J.; Parsons, A. Predictors of generalized anxiety disorder stigma. Psychiatry Res. 2013, 206, 282–286. [Google Scholar] [CrossRef]
- Anderson, K.N.; Jeon, A.B.; Blenner, J.A.; Wiener, R.L.; Hope, D.A. How people evaluate others with social anxiety disorder: A comparison to depression and general mental illness stigma. Am. J. Orthopsychiatry 2015, 85, 131–138. [Google Scholar] [CrossRef]
- Griffiths, K.M.; Christensen, H.; Jorm, A.F.; Evans, K.; Groves, C. Personal Depression Stigma Scale [Database record]. PsycTESTS 2004. [Google Scholar] [CrossRef]
- Angermeyer, M.C.; Matschinger, H. The stigma of mental illness: Effects of labelling on public attitudes towards people with mental disorder. Acta Psychiatr. Scand. 2003, 108, 304–309. [Google Scholar] [CrossRef] [PubMed]
- Kelly, C.M.; Jorm, A.F. Adolescents’ intentions to offer assistance to friends with depression or conduct disorder: Associations with psychopathology and psychosocial characteristics. Early Interv. Psychiatry 2007, 1, 150–156. [Google Scholar] [CrossRef]
- Cavallo, J.V.; Zee, K.S.; Higgins, E.T. Giving the help that is needed: How regulatory mode impacts social support. Personal. Soc. Psychol. Bull. 2016, 42, 1111–1128. [Google Scholar] [CrossRef]
- Hayes, A.F. Introduction to Mediation, Moderation and Conditional Process Analysis: A Regression-Based Approach; The Guilford Press: New York, NY, USA, 2017. [Google Scholar]
- Reavley, N.J.; Jorm, A.F. Young people’s stigmatizing attitudes towards people with mental disorders: Findings from an Australian national survey. Aust. N. Z. J. Psychiatry 2011, 45, 1033–1039. [Google Scholar] [CrossRef]
- Corrigan, P.W. Mental health stigma as social attribution: Implications for research methods and attitude change. Clin. Psychol. Sci. Pract. 2000, 7, 48–67. [Google Scholar] [CrossRef]
- Greitemeyer, T.; Rudolph, U. Help Giving and Aggression from an Attributional Perspective: Why and When We Help or Retaliate 1. J. Appl. Soc. Psychol. 2003, 33, 1069–1087. [Google Scholar] [CrossRef]
- Yamauchi, H.; Lee, K. An Attribution—Emotion Model of Helping Behavior. Psychol. Rep. 1999, 84, 1073–1074. [Google Scholar]
- Michaels, P.J.; Corrigan, P.W. Measuring mental illness stigma with diminished social desirability effects. J. Ment. Health 2013, 22, 218–226. [Google Scholar] [CrossRef]
| Stereotype Statement | M (SD) | Achieved Range | Disagree or Strongly Disagree | Neither Agree nor Disagree | Agree or Strongly Agree |
|---|---|---|---|---|---|
| “…could snap out of it if they wanted” | 2.26 (1.16) | 1–5 | 64.8% | 18.2% | 17% |
| “…a sign of personal weakness” | 2.12 (1.12) | 1–5 | 65.8% | 19.6% | 14.6% |
| “…not a real medical illness” | 2.12 (1.11) | 1–5 | 65.5% | 23% | 11.5% |
| Variable | M (SD) | Achieved Range | Weak Not Sick | Anger | Pity | Fear | Social Distance | Likelihood to Help |
|---|---|---|---|---|---|---|---|---|
| Weak not Sick | 2.15 (0.88) | 1–5 | 1 | 0.441 ** | −0.181 * | 0.215 ** | 0.347 ** | −0.332 ** |
| Anger | 4.65 (1.95) | 3–13 | 1 | −0.268 * | 0.366 ** | 0.429 ** | −0.284 ** | |
| Pity | 11.90 (1.91) | 3–15 | 1 | −0.054 | −0.337 ** | 0.330 ** | ||
| Fear | 5.82 (2.32) | 3–12 | 1 | 0.250 ** | −0.203 * | |||
| Social distance | 11.03 (3.86) | 6–24 | 1 | −0.345 ** | ||||
| Likelihood to help | 4.39 (0.891) | 1–5 | 1 |
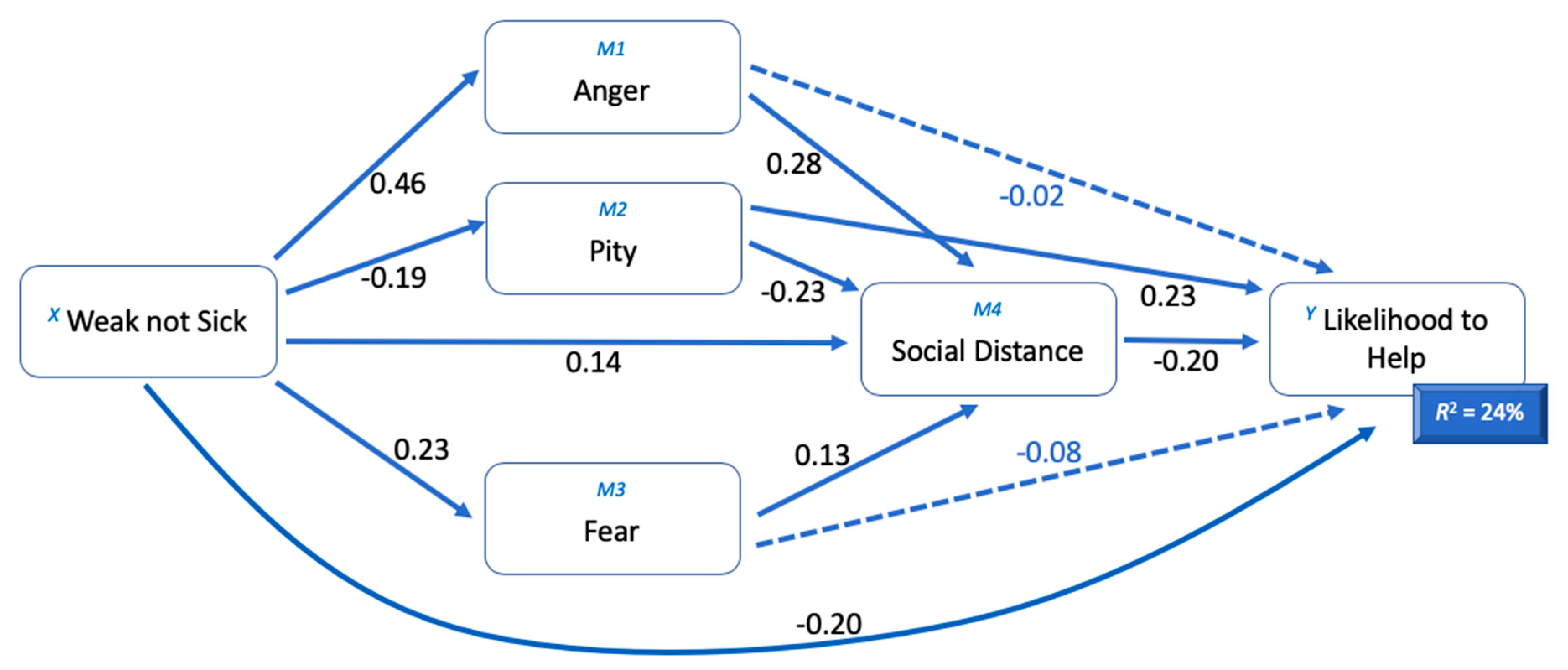
| Variable | Anger | Pity | Fear | Social Distance | Likelihood to Help | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Coeff. | SE | p | Coeff. | SE | p | Coeff. | SE | p | Coeff. | SE | p | Coeff. | SE | p | |
| Weak not sick | 0.4584 | 0.0583 | 0.0000 | −0.1882 | 0.0655 | 0.0045 | 0.2345 | 0.0642 | 0.0003 | 0.1407 | 0.0643 | 0.0298 | −0.2036 | 0.0694 | 0.0037 |
| Anger | 0.2830 | 0.0693 | 0.0001 | −0.0180 | 0.0767 | 0.8150 | |||||||||
| Pity | −0.2322 | 0.0590 | 0.0001 | 0.2273 | 0.0652 | 0.0006 | |||||||||
| Fear | 0.1326 | 0.0621 | 0.0338 | −0.0827 | 0.0669 | 0.2177 | |||||||||
| Social distance | −0.1983 | 0.0726 | 0.0068 | ||||||||||||
| R2 = 0.2200 F (1219) = 61.78 p = 0.0000 | R2 = 0.0363 F (1219) = 8.258 p = 0.0045 | R2 = 0.0573 F (1219) = 13.32 p = 0.0003 | R2 = 0.2911 F (4219) = 22.18 p = 0.0000 | R2 = 0.2353 F (5219) = 13.23 p = 0.0000 | |||||||||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hanlon, H.R.; Swords, L. Adolescent Endorsement of the “Weak-Not-Sick” Stereotype for Generalised Anxiety Disorder: Associations with Prejudice, Discrimination, and Help-Giving Intentions toward Peers. Int. J. Environ. Res. Public Health 2020, 17, 5415. https://doi.org/10.3390/ijerph17155415
Hanlon HR, Swords L. Adolescent Endorsement of the “Weak-Not-Sick” Stereotype for Generalised Anxiety Disorder: Associations with Prejudice, Discrimination, and Help-Giving Intentions toward Peers. International Journal of Environmental Research and Public Health. 2020; 17(15):5415. https://doi.org/10.3390/ijerph17155415
Chicago/Turabian StyleHanlon, Holly R., and Lorraine Swords. 2020. "Adolescent Endorsement of the “Weak-Not-Sick” Stereotype for Generalised Anxiety Disorder: Associations with Prejudice, Discrimination, and Help-Giving Intentions toward Peers" International Journal of Environmental Research and Public Health 17, no. 15: 5415. https://doi.org/10.3390/ijerph17155415
APA StyleHanlon, H. R., & Swords, L. (2020). Adolescent Endorsement of the “Weak-Not-Sick” Stereotype for Generalised Anxiety Disorder: Associations with Prejudice, Discrimination, and Help-Giving Intentions toward Peers. International Journal of Environmental Research and Public Health, 17(15), 5415. https://doi.org/10.3390/ijerph17155415





