Feasibility of 3-Dimensional Visual Guides for Preparing Pediatric Zirconia Crowns: An In Vitro Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
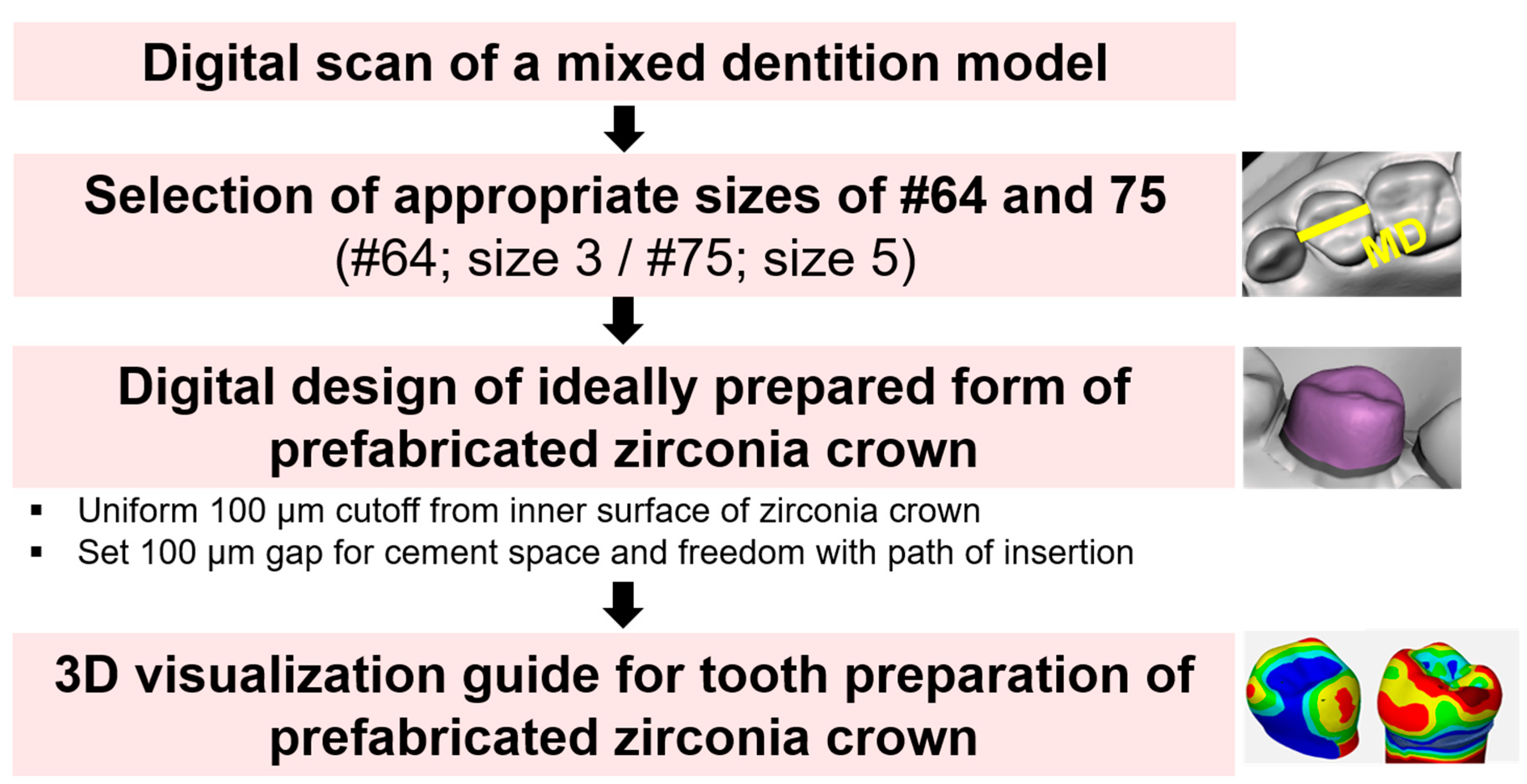
2.2. Digital Design of Preparation Guide
- Model A: Dentiform model;
- Model B: Digitally scanned PZC set model;
- Model C: Ideally prepared tooth model for PZC;
- Model D: Actually prepared tooth model for PZC.
2.3. Evaluating the Feasibility of the Preparation Guide for PZCs
2.3.1. Tooth Preparation Time
2.3.2. Harmony Score with Adjacent Teeth
- Point: Cases wherein the height differences between the marginal ridges of the PZC and the marginal ridges of the adjacent teeth were ≥ 2 mm on any of the mesial and distal side.
- Points: Cases wherein the height differences between the marginal ridges of the PZC and the marginal ridges of the adjacent teeth ranged between 1 mm and 2 mm on both the mesial and distal sides.
- Points: Cases wherein the height differences between the marginal ridges of the PZC and the marginal ridges of the adjacent teeth were < 1 mm on both the mesial and distal sides.
2.3.3. Differences in the Amount of Tooth Reduction
2.4. Statistical Analysis
3. Results
3.1. Tooth Preparation Time
3.2. Harmony Score
3.3. Difference in the Amount of Tooth Reduction
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Vadiakas, G. Case definition, aetiology and risk assessment of early childhood caries (ECC): A revisited review. Eur. Arch. Paediatr. Dent. 2008, 9, 114–125. [Google Scholar] [CrossRef]
- Ripa, L.W. Nursing caries: A comprehensive review. Pediatr. Dent. 1988, 10, 268–282. [Google Scholar]
- Kindelan, S.; Day, P.; Nichol, R.; Willmott, N.; Fayle, S. UK National Clinical Guidelines in Paediatric Dentistry: Stainless steel preformed crowns for primary molars. Int. J. Paediatr. Dent. 2008, 18, 20–28. [Google Scholar] [CrossRef] [PubMed]
- Hickel, R.; Kaaden, C.; Paschos, E.; Buerkle, V.; Garcia-Godoy, F.; Manhart, J. Longevity of occlusally-stressed restorations in posterior primary teeth. Am. J. Dent. 2005, 18, 198–211. [Google Scholar] [PubMed]
- Lopez-Loverich, A.M.; Garcia, M.M.; Donly, K.J. Retrospective study of retention of stainless steel crowns and pre-veneered crowns on primary anterior teeth. Pediatr. Dent. 2015, 37, 530–534. [Google Scholar] [PubMed]
- Einwag, J.; Dünninger, P. Stainless steel crown versus multisurface amalgam restorations: An 8-year longitudinal clinical study. Quintessence Int. 1996, 27, 321–323. [Google Scholar]
- Sharaf, A.A.; Farsi, N.M. A clinical and radiographic evaluation of stainless steel crowns for primary molars. J. Dent. 2004, 32, 27–33. [Google Scholar] [CrossRef]
- Zimmerman, J.; Feigal, R.; Till, M.; Hodges, J.S. Parental attitudes on restorative materials as factors influencing current use in pediatric dentistry. Pediatr. Dent. 2009, 31, 63–70. [Google Scholar]
- Planells del Pozo, P.; Fuks, A. Zirconia crowns-an esthetic and resistant restorative alternative for ECC affected primary teeth. J. Clin. Pediatr. Dent. 2014, 38, 193–195. [Google Scholar] [CrossRef]
- Holsinger, D.M.; Wells, M.H.; Scarbecz, M.; Donaldson, M. Clinical evaluation and parental satisfaction with pediatric zirconia anterior crowns. Pediatr. Dent. 2016, 38, 192–197. [Google Scholar]
- Lee, J.M.; Lee, H.-S.; Nam, O.H.; Kim, M.S.; Choi, S.C. Three Dimensional Analysis of Primary Maxillary Central and Lateral Anterior Zirconia Crown. J. Korean. Acad. Pediatr. Dent. 2016, 43, 176–186. [Google Scholar] [CrossRef]
- Clark, L.; Wells, M.H.; Harris, E.F.; Lou, J. Comparison of amount of primary tooth reduction required for anterior and posterior zirconia and stainless steel crowns. Pediatr. Dent. 2016, 38, 42–46. [Google Scholar] [PubMed]
- Lee, H.; Chae, Y.K.; Lee, H.-S.; Choi, S.C.; Nam, O.H. Three-Dimensional Digitalized Surface and Volumetric Analysis of Posterior Prefabricated Zirconia Crowns for Children. J. Clin. Pediatr. Dent. 2019, 43, 231–238. [Google Scholar] [CrossRef] [PubMed]
- Giannetopoulos, S.; van Noort, R.; Tsitrou, E. Evaluation of the marginal integrity of ceramic copings with different marginal angles using two different CAD/CAM systems. J. Dent. 2010, 38, 980–986. [Google Scholar] [CrossRef]
- Kohorst, P.; Brinkmann, H.; Li, J.; Borchers, L.; Stiesch, M. Marginal accuracy of four-unit zirconia fixed dental prostheses fabricated using different computer-aided design/computer-aided manufacturing systems. Eur. J. Oral Sci. 2009, 117, 319–325. [Google Scholar] [CrossRef]
- Beuer, F.; Naumann, M.; Gernet, W.; Sorensen, J.A. Precision of fit: Zirconia three-unit fixed dental prostheses. Clin. Oral Investig. 2009, 13, 343–349. [Google Scholar] [CrossRef]
- Lee, H.; Chae, Y.K.; Choi, S.; Jih, M.K.; Lee, J.-W.; Choi, S.C.; Nam, O.H. Feasibility of a 3D Surgical Guide Technique for Impacted Supernumerary Tooth Extraction: A Pilot Study with 3D Printed Simulation Models. Appl. Sci. 2019, 9, 3905. [Google Scholar] [CrossRef] [Green Version]
- Hu, Y.K.; Xie, Q.Y.; Yang, C.; Xu, G.Z. Computer-designed surgical guide template compared with free-hand operation for mesiodens extraction in premaxilla using "trapdoor" method. Medicine (Baltimore) 2017, 96, e7310. [Google Scholar] [CrossRef]
- Sarnat, H.; Arad, P.; Hanauer, D.; Shohami, E. Communication strategies used during pediatric dental treatment: A pilot study. Pediatr. Dent. 2001, 23, 337–342. [Google Scholar]
- Davidovich, E.; Wated, A.; Shapira, J.; Ram, D. The influence of location of local anesthesia and complexity/duration of restorative treatment on children's behavior during dental treatment. Pediatr. Dent. 2013, 35, 333–336. [Google Scholar]
- Getz, T.; Weinstein, P. The effect of structural variables on child behavior in the operatory. Pediatr. Dent. 1981, 3, 262–266. [Google Scholar] [PubMed]
- Farwell, D.G.; Reilly, D.F.; Weymuller, E.A., Jr.; Greenberg, D.L.; Staiger, T.O.; Futran, N.A. Predictors of perioperative complications in head and neck patients. Arch. Otolaryngol. Head Neck Surg. 2002, 128, 505–511. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Green, S.M.; Hummel, C.B.; Wittlake, W.A.; Rothrock, S.G.; Hopkins, G.A.; Garrett, W. What is the optimal dose of intramuscular ketamine for pediatric sedation? Acad. Emerg. Med. 1999, 6, 21–26. [Google Scholar] [CrossRef] [PubMed]
- Ashima, G.; Sarabjot, K.B.; Gauba, K.; Mittal, H.C. Zirconia crowns for rehabilitation of decayed primary incisors: An esthetic alternative. J. Clin. Pediatr. Dent. 2014, 39, 18–22. [Google Scholar] [CrossRef]
- McClure, A.R.; Roomian, T.C.; Eisen, S.E.; Kugel, G.; Amato, R.B. Jumpstart Mirror Trainer: A New Device for Teaching Mirror Skills to First-Year Dental Students. J. Dent. Educ. 2019, 83, 1199–1204. [Google Scholar] [CrossRef]
- Lugassy, D.; Levanon, Y.; Pilo, R.; Shelly, A.; Rosen, G.; Meirowitz, A.; Brosh, T. Predicting the clinical performance of dental students with a manual dexterity test. PLoS ONE 2018, 13, e0193980. [Google Scholar] [CrossRef] [Green Version]
- Eichenberger, M.; Biner, N.; Amato, M.; Lussi, A.; Perrin, P. Effect of Magnification on the Precision of Tooth Preparation in Dentistry. Oper. Dent. 2018, 43, 501–507. [Google Scholar] [CrossRef]






| Tooth | Without Preparation Guide (min) | With Preparation Guide (min) | p-Value |
|---|---|---|---|
| Maxillary first molar | 6.39 ± 2.40 | 5.28 ± 1.75 | <0.0001 * |
| Mandibular second molar | 5.63 ± 2.05 | 4.98 ± 1.81 | 0.013 * |
| Score | Without Preparation Guide n (%) | With Preparation Guide n (%) | p-Value |
|---|---|---|---|
| Maxillary first molar | |||
| 1 | 5 (25%) | 0 (0%) | 0.044 * |
| 2 | 5 (25%) | 5 (25%) | |
| 3 | 10 (50%) | 15 (75%) | |
| Mandibular second molar | |||
| 1 | 3 (15%) | 1 (5%) | 0.535 |
| 2 | 7 (35%) | 6 (30%) | |
| 3 | 10 (50%) | 13 (65%) | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kang, H.Y.; Lee, H.; Chae, Y.K.; Hong, S.-J.; Jeong, Y.Y.; Lee, K.E.; Kim, M.S.; Lee, H.-S.; Choi, S.C.; Nam, O.H. Feasibility of 3-Dimensional Visual Guides for Preparing Pediatric Zirconia Crowns: An In Vitro Study. Int. J. Environ. Res. Public Health 2020, 17, 5732. https://doi.org/10.3390/ijerph17165732
Kang HY, Lee H, Chae YK, Hong S-J, Jeong YY, Lee KE, Kim MS, Lee H-S, Choi SC, Nam OH. Feasibility of 3-Dimensional Visual Guides for Preparing Pediatric Zirconia Crowns: An In Vitro Study. International Journal of Environmental Research and Public Health. 2020; 17(16):5732. https://doi.org/10.3390/ijerph17165732
Chicago/Turabian StyleKang, Ho Yeon, Hyeonjong Lee, Yong Kwon Chae, Seoung-Jin Hong, Yun Yeong Jeong, Ko Eun Lee, Mi Sun Kim, Hyo-Seol Lee, Sung Chul Choi, and Ok Hyung Nam. 2020. "Feasibility of 3-Dimensional Visual Guides for Preparing Pediatric Zirconia Crowns: An In Vitro Study" International Journal of Environmental Research and Public Health 17, no. 16: 5732. https://doi.org/10.3390/ijerph17165732
APA StyleKang, H. Y., Lee, H., Chae, Y. K., Hong, S.-J., Jeong, Y. Y., Lee, K. E., Kim, M. S., Lee, H.-S., Choi, S. C., & Nam, O. H. (2020). Feasibility of 3-Dimensional Visual Guides for Preparing Pediatric Zirconia Crowns: An In Vitro Study. International Journal of Environmental Research and Public Health, 17(16), 5732. https://doi.org/10.3390/ijerph17165732







