A System Dynamics Simulation Applied to Healthcare: A Systematic Review
Abstract
1. Introduction
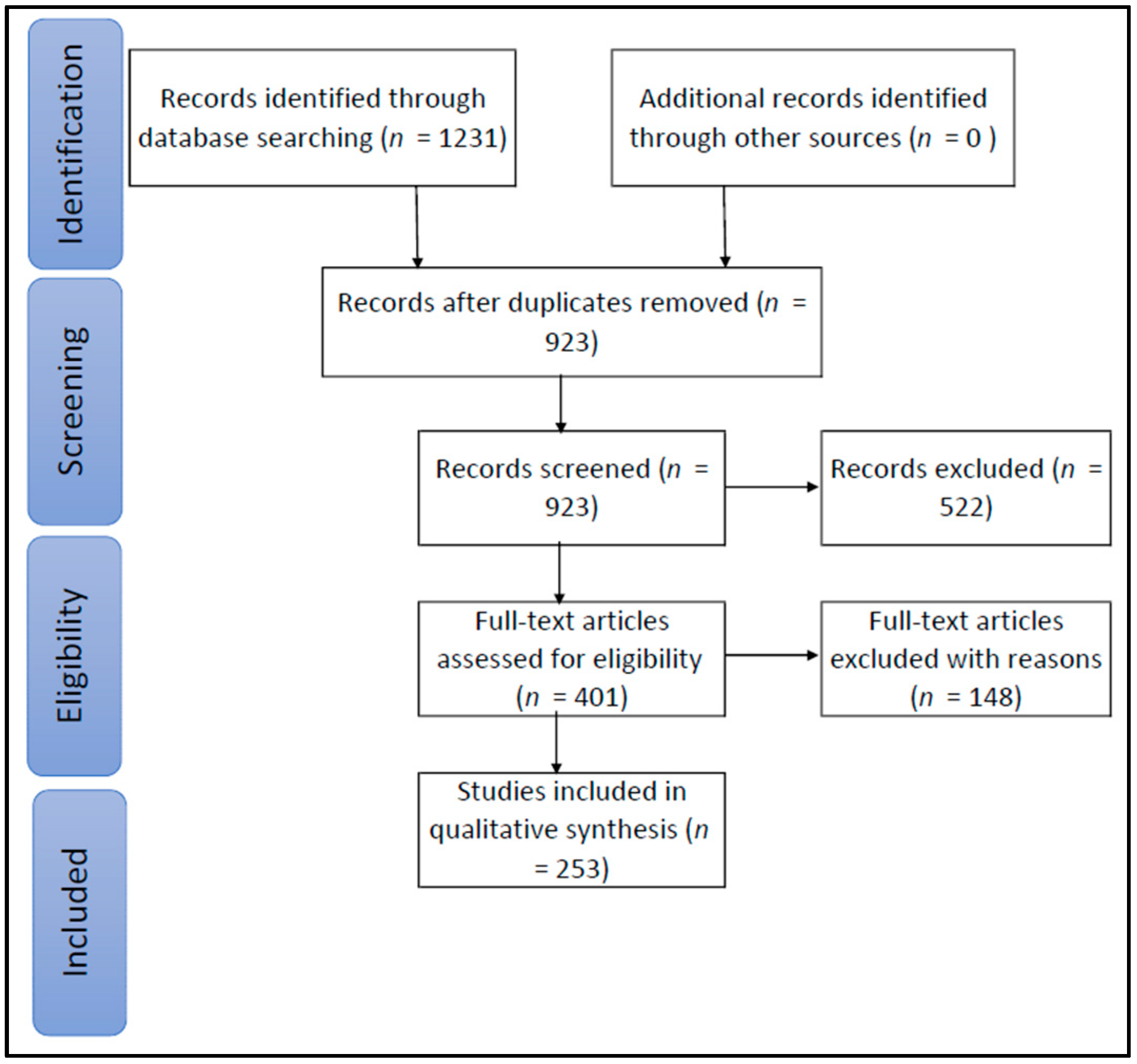
2. Evaluation of Review Papers
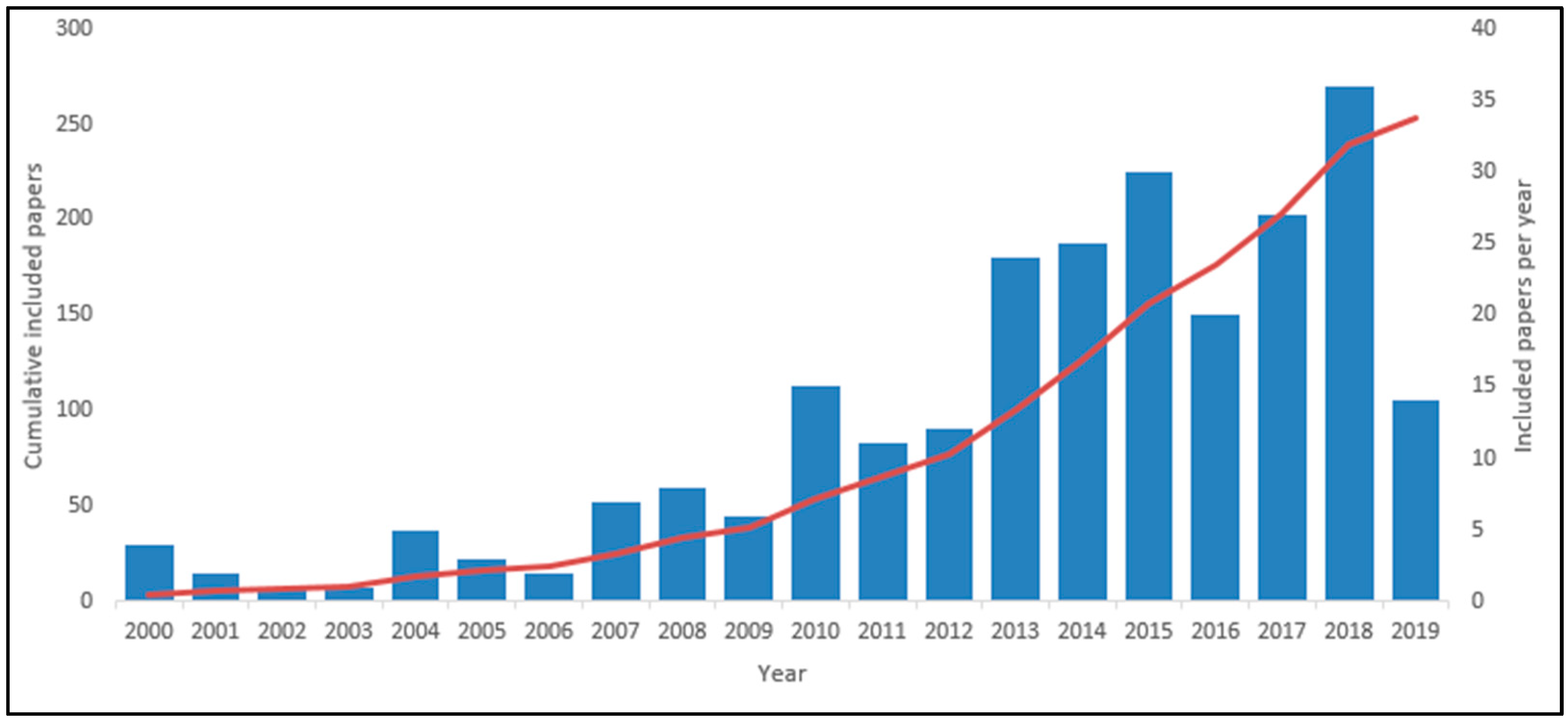
3. Methodology
- RQ1.
- What are the main problems in the healthcare sector that have been studied in the past using the SD approach?
- RQ2.
- How was the SD approach utilized to model and address complex healthcare problems?
- RQ3.
- What can be learned from the past SD simulation research in the healthcare area that will support high-quality research in the future?
- Articles related to healthcare;
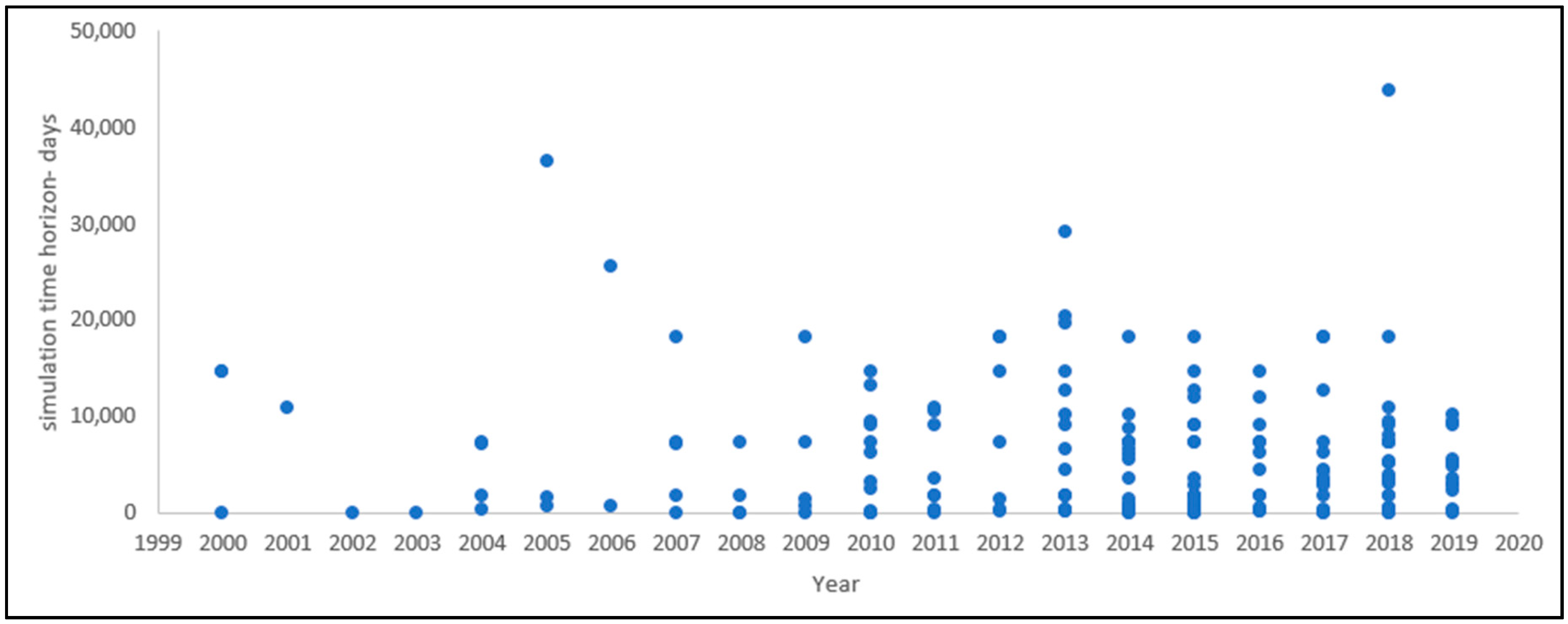
- Articles published from 2000 to 2019;
- Articles related to research questions;
- Articles written in English.
- Papers written in other languages;
- Chapters of books;
- Review papers;
- Articles from secondary sources that were not free or open access;
- Letters, newspaper articles, viewpoints, presentations, anecdotes, duplicated studies, short papers, and posters.
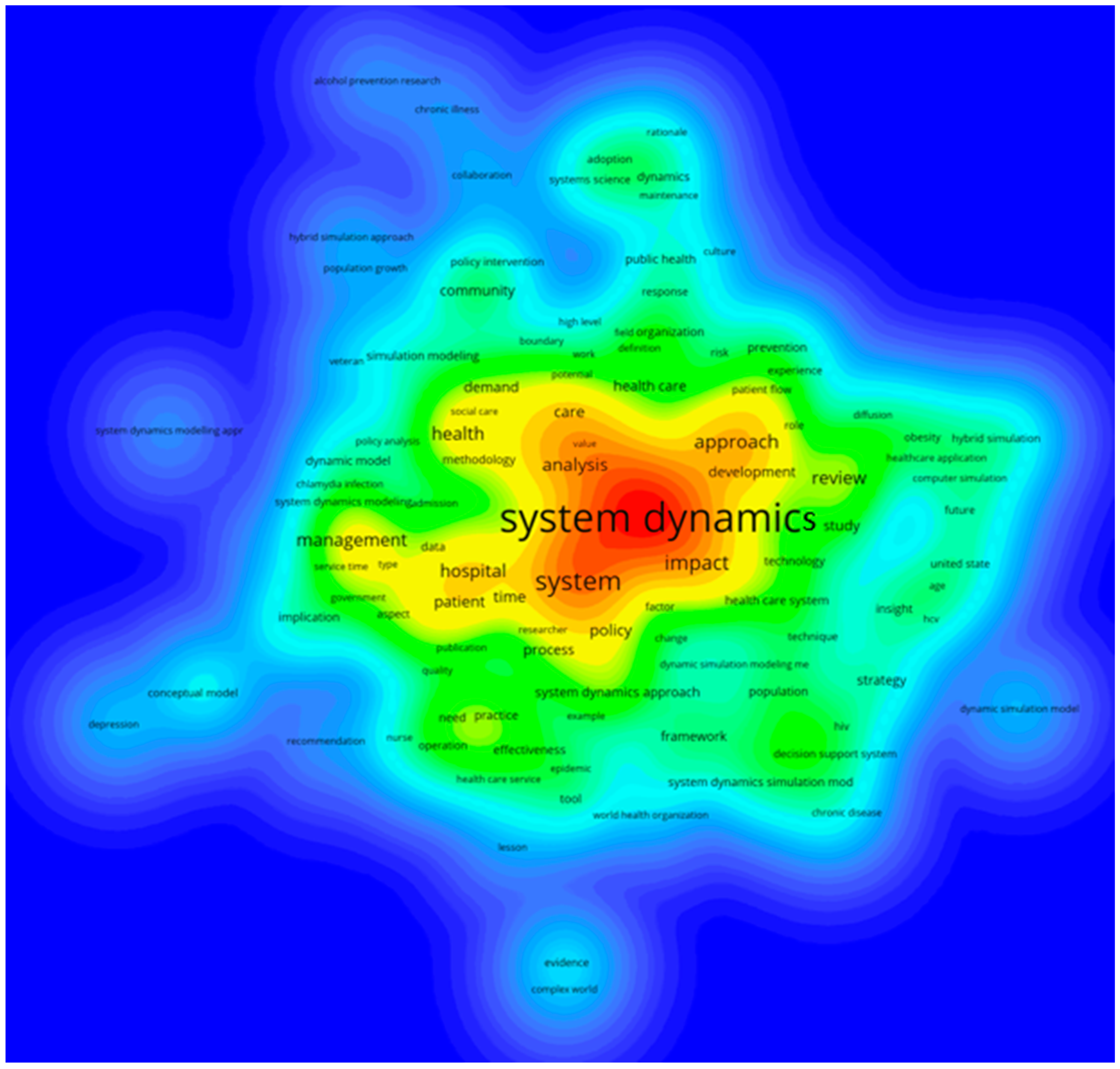
4. Results
5. Discussion
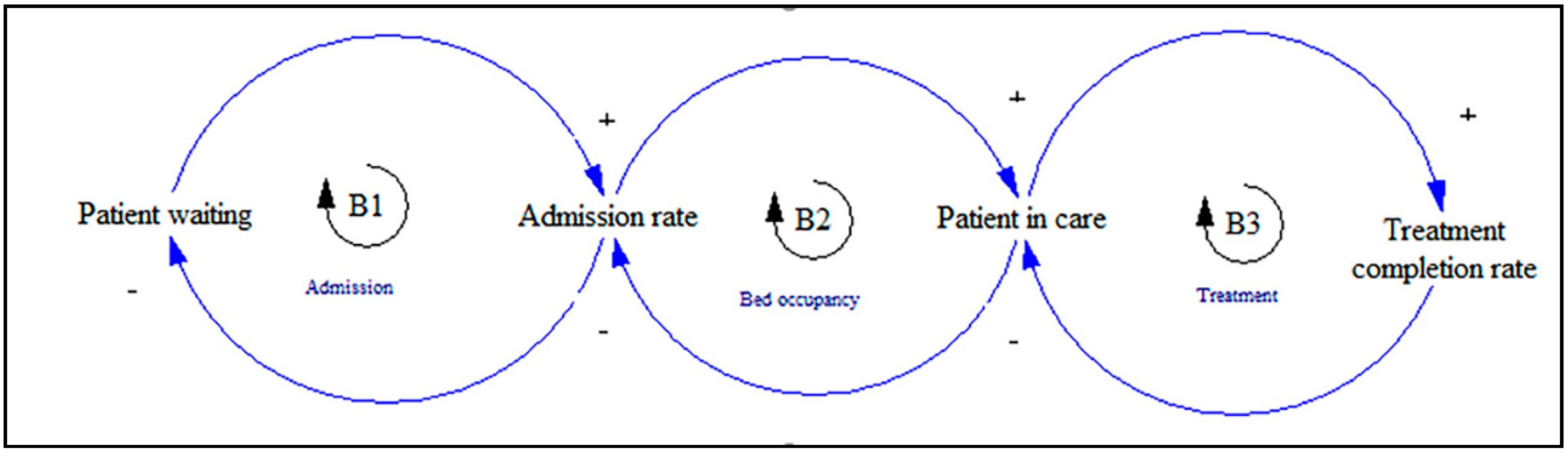
5.1. Patient Flow
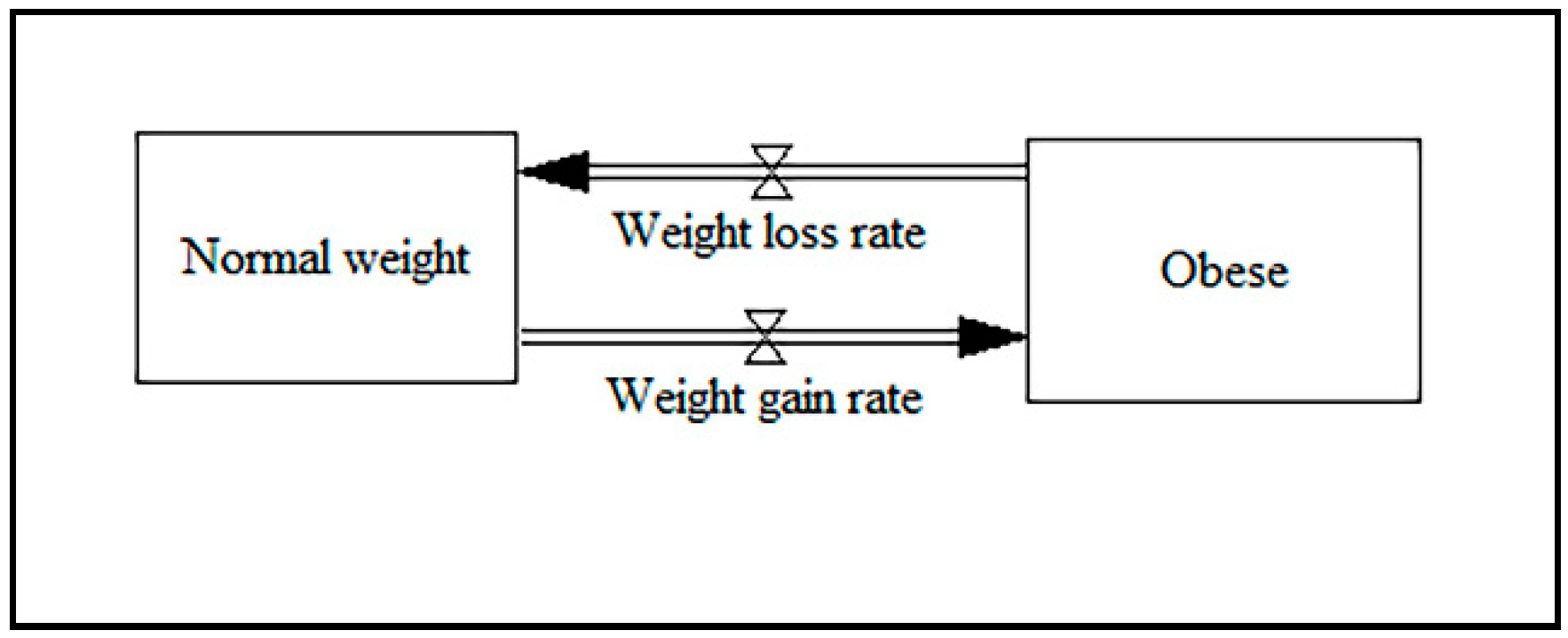
5.2. Obesity
5.3. HIV/AIDS and Tuberculosis
5.4. Workforce Demand
5.5. Chronic Diseases
5.6. Hybrid Modeling
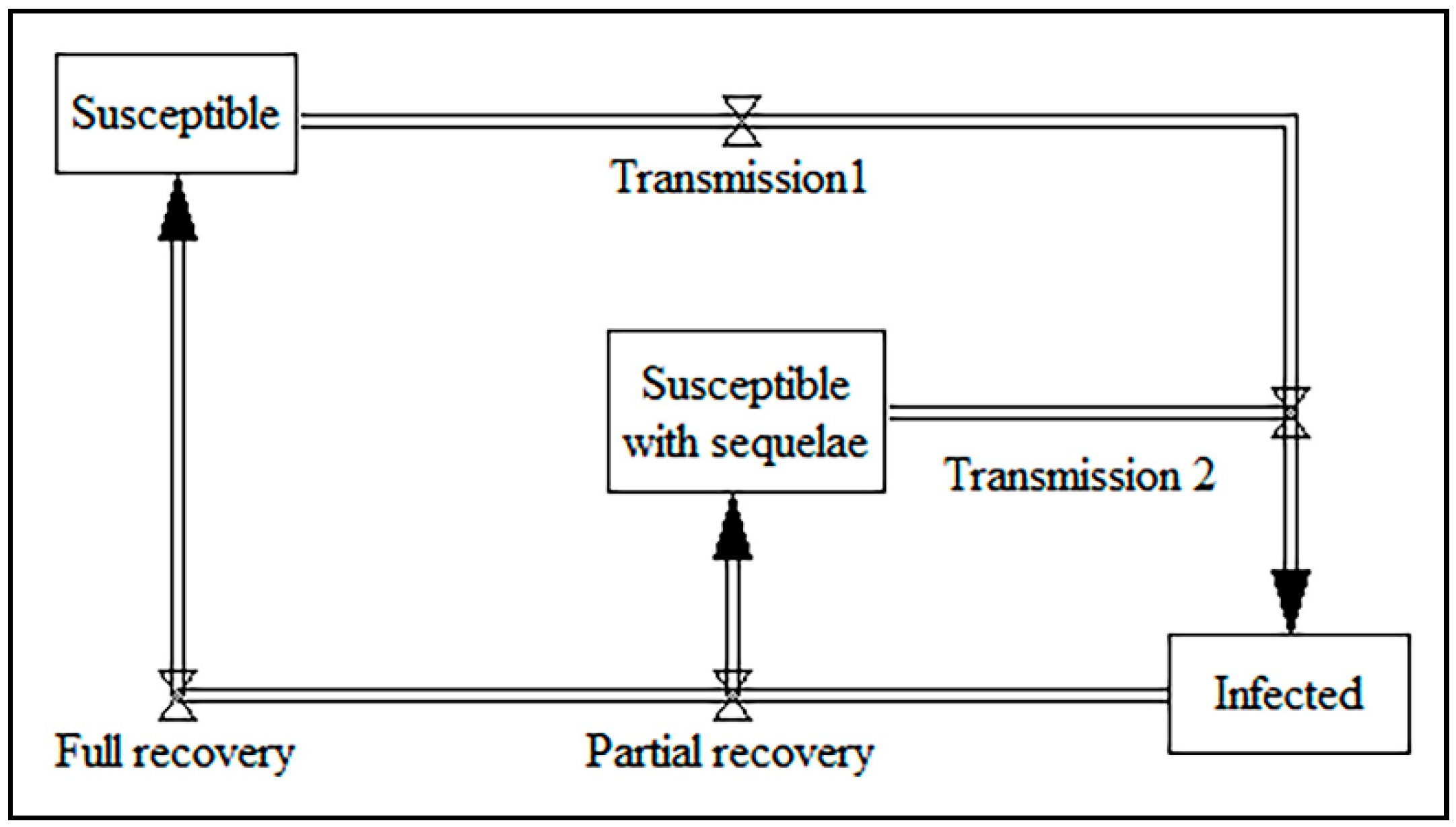
5.7. Chlamydia
5.8. Other Research Areas
6. Quality Assessment
- Direct structural tests, including empirical and theoretical tests;
- Structure-oriented behavioral tests, such as extreme condition tests and sensitivity tests;
- Behavioral pattern tests, considered to be model calibration [140].
7. Conclusions
- RQ1.
- What are the main problems in the healthcare sector that have been studied in the past using the SD approach? To answer this question, the included records have been reviewed, and the main problems were extracted and are represented in Table 4.
- RQ2.
- How was the SD approach utilized to model and address complex healthcare problems? To answer this question, essential aspects of the SD approach, including “core part of SD diagrams”, “key variables”, and “output variables” are represented in the Discussion section.
- RQ3.
- What can be learned from the past SD simulation research in the healthcare area that will support high-quality research in the future? In order to answer this question, the main aspects of high-quality SD research have been assessed in the quality assessment section, such as the clarity of the objectives and results, the description of the scenarios, the source of the input data, and model validation.
Author Contributions
Funding
Conflicts of Interest
References
- Brailsford, S.C.; Harper, P.R.; Patel, B.; Pitt, M. An analysis of the academic literature on simulation and modelling in health care. J. Simul. 2009, 3, 130–140. [Google Scholar] [CrossRef]
- Katsaliaki, K.; Mustafee, N. Applications of simulation within the healthcare context. J. Oper. Res. Soc. 2011, 62, 1431–1451. [Google Scholar] [CrossRef] [PubMed]
- Fone, D.; Hollinghurst, S.; Temple, M.; Round, A.; Lester, N.; Weightman, A.; Roberts, K.; Coyle, E.; Bevan, G.; Palmer, S. Systematic review of the use and value of computer simulation modelling in population health and health care delivery. J. Public Health 2003, 25, 325–335. [Google Scholar] [CrossRef] [PubMed]
- Forrester, J.W. System dynamics—The next fifty years. Syst. Dyn. Rev. J. Syst. Dyn. Soc. 2007, 23, 359–370. [Google Scholar] [CrossRef]
- Homer, J.B.; Hirsch, G.B. System dynamics modeling for public health: Background and opportunities. Am. J. Public Health 2006, 96, 452–458. [Google Scholar] [CrossRef]
- Sterman, J. Business Dynamics; Irwin/McGraw-Hil: New York, NY, USA, 2010. [Google Scholar]
- Sterman, J.D. System dynamics modeling: Tools for learning in a complex world. Calif. Manage. Rev. 2001, 43, 8–25. [Google Scholar] [CrossRef]
- Henderson, S.G.; Biller, B.; Hsieh, M.H.; Shortle, J.; Tew, J.D.; Barton, R.R.; Brailsford, S. Tutorial: Advances and challenges in healthcare simulation modeling. In Proceedings of the 2007 Winter Simulation Conference, Washington, DC, USA, 9–12 December 2007; pp. 1436–1448. [Google Scholar]
- Roberts, S.D. Tutorial on the Simulation of Healthcare Systems. In Proceedings of the Winter Simulation Conference, Phoenix, AZ, USA, 11–14 December 2011; pp. 1408–1419. [Google Scholar]
- Mingers, J.; White, L. A review of the recent contribution of systems thinking to operational research and management science. Eur. J. Oper. Res. 2010, 207, 1147–1161. [Google Scholar] [CrossRef]
- Mustafee, N.; Katsaliaki, K.; Taylor, S.J. Profiling literature in healthcare simulation. Simulation 2010, 86, 543–558. [Google Scholar] [CrossRef]
- Stahl, J.E. Modelling methods for pharmacoeconomics and health technology assessment. Pharmacoeconomics 2008, 26, 131–148. [Google Scholar] [CrossRef]
- Mielczarek, B. Review of modelling approaches for healthcare simulation. Oper. Res. Decis. 2016, 26, 55–72. [Google Scholar] [CrossRef]
- Cilenti, D.; Issel, M.; Wells, R.; Link, S.; Lich, K.H. System Dynamics Approaches and Collective Action for Community Health: An Integrative Review. Am. J. Community Psychol. 2019, 63, 527–545. [Google Scholar] [CrossRef] [PubMed]
- Allahi, F.; De Leeuw, S.; Sabet, E.; Kian, R.; Damiani, L.; Giribone, P.; Revetria, R.; Cianci, R. A review of system dynamics models applied in social and humanitarian researches. In Proceedings of the World Congress on Engineering 2018 (WCE 2018), London, UK, 4–6 July 2018. [Google Scholar]
- Kunc, M.; Mortenson, M.J.; Vidgen, R. A computational literature review of the field of System Dynamics from 1974 to 2017. J. Simul. 2018, 12, 115–127. [Google Scholar] [CrossRef]
- Torres, J.P. System Dynamics Review and publications 1985–2017: Analysis, synthesis and contributions. Syst. Dyn. Rev. 2019, 35, 160–176. [Google Scholar] [CrossRef]
- Gul, M.; Guneri, A.F. A comprehensive review of emergency department simulation applications for normal and disaster conditions. Comput. Ind. Eng. 2015, 83, 327–344. [Google Scholar] [CrossRef]
- Aboueljinane, L.; Sahin, E.; Jemai, Z. A review on simulation models applied to emergency medical service operations. Comput. Ind. Eng. 2013, 66, 734–750. [Google Scholar] [CrossRef]
- Salmon, A.; Rachuba, S.; Briscoe, S.; Pitt, M. A structured literature review of simulation modelling applied to Emergency Departments: Current patterns and emerging trends. Oper. Res. Health Care 2018, 19, 1–13. [Google Scholar] [CrossRef]
- He, L.; Madathil, S.C.; Oberoi, A.; Servis, G.; Khasawneh, M.T. A systematic review of research design and modeling techniques in inpatient bed management. Comput. Ind. Eng. 2019, 127, 451–466. [Google Scholar] [CrossRef]
- Zhang, X. Application of discrete event simulation in health care: A systematic review. BMC Health Serv. Res. 2018, 18, 687. [Google Scholar] [CrossRef]
- Atkinson, J.-A.; Wells, R.; Page, A.; Dominello, A.; Haines, M.; Wilson, A. Applications of system dynamics modelling to support health policy. Public Health Res Pr. 2015, 25, e2531531. [Google Scholar] [CrossRef]
- Günal, M.M.; Pidd, M. Discrete event simulation for performance modelling in health care: A review of the literature. J. Simul. 2010, 4, 42–51. [Google Scholar] [CrossRef]
- Brailsford, S.C.; Carter, M.W.; Jacobson, S.H. Five decades of healthcare simulation. In Proceedings of the 2017 Winter Simulation Conference (WSC), Las Vegas, NV, USA, 3–6 December 2017; pp. 365–384. [Google Scholar]
- Scholz, S.; Mittendorf, T. Modeling rheumatoid arthritis using different techniques—A review of model construction and results. Health Econ. Rev. 2014, 4, 18. [Google Scholar] [CrossRef] [PubMed]
- Saville, C.E.; Smith, H.K.; Bijak, K. Operational research techniques applied throughout cancer care services: A review. Health Syst. 2019, 8, 52–73. [Google Scholar] [CrossRef] [PubMed]
- Mustafee, N.; Katsaliaki, K.; Gunasekaran, A.; Williams, M.D.; Fakhimi, M.; Probert, J. Operations research within UK healthcare: A review. J. Enterp. Inf. Manag. 2013, 26, 21–49. [Google Scholar] [CrossRef]
- Long, K.M.; Meadows, G.N. Simulation modelling in mental health: A systematic review. J. Simul. 2018, 12, 76–85. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Health Care Interventions: Explanation and Elaboration. PLoS Med. 2009, 6, e1000100. [Google Scholar] [CrossRef]
- Brüssow, H. What is health? Microb. Biotechnol. 2013, 6, 341–348. [Google Scholar] [CrossRef]
- Health Care. Available online: https://en.wikipedia.org/wiki/Health_care (accessed on 20 November 2019).
- Steffen, G.E. Quality medical care: A definition. JAMA 1988, 260, 56–61. [Google Scholar] [CrossRef]
- Health System. Available online: https://en.wikipedia.org/wiki/Health_system (accessed on 20 November 2019).
- Vanderby, S.; Carter, M.W. An evaluation of the applicability of system dynamics to patient flow modelling. J. Oper. Res. Soc. 2010, 61, 1572–1581. [Google Scholar] [CrossRef]
- Rashwan, W.; Abo-Hamad, W.; Arisha, A. A system dynamics view of the acute bed blockage problem in the Irish healthcare system. Eur. J. Oper. Res. 2015, 247, 276–293. [Google Scholar] [CrossRef]
- Rashwan, W.; Ragab, M.; Abo-Hamad, W.; Arisha, A. Evaluating policy interventions for delayed discharge: A system dynamics approach. In Proceedings of the 2013 Winter Simulation Conference: Making Decisions in a Complex World, Washington, DC, USA, 8–11 December 2013; pp. 2463–2474. [Google Scholar]
- Grida, M.; Zeid, M. A system dynamics-based model to implement the Theory of Constraints in a healthcare system. Simulation 2019, 95, 593–605. [Google Scholar] [CrossRef]
- Lane, D.C.; Monefeldt, C.; Rosenhead, J.V. Looking in the wrong place for healthcare improvements: A system dynamics study of an accident and emergency department. J. Oper. Res. Soc. 2000, 51, 518–531. [Google Scholar] [CrossRef]
- Brailsford, S.C.; Lattimer, V.A.; Tarnaras, P.; Turnbull, J.C. Emergency and on-demand health care: Modelling a large complex system. J. Oper. Res. Soc. 2004, 55, 34–42. [Google Scholar] [CrossRef]
- Cooke, D.; Rohleder, T.; Rogers, P. A dynamic model of the systemic causes for patient treatment delays in emergency departments. J. Model. Manag. 2010, 5, 287–301. [Google Scholar] [CrossRef]
- Kumar, S. Modeling patient flow operation of a US urban county hospital. Technol. Health Care 2011, 19, 247–260. [Google Scholar] [CrossRef] [PubMed]
- Taylor, K.; Dangerfield, B. Modelling the feedback effects of reconfiguring health services. J. Oper. Res. Soc. 2005, 56, 659–675. [Google Scholar] [CrossRef][Green Version]
- German, J.D.; Miña, J.K.P.; Alfonso, C.M.N.; Yang, K.-H. A study on shortage of hospital beds in the Philippines using system dynamics. In Proceedings of the 2018 5th International Conference on Industrial Engineering and Applications (ICIEA), Singapore, 26–28 April 2018; pp. 72–78. [Google Scholar]
- Wolstenholme, E.; Monk, D.; McKelvie, D.; Arnold, S. Coping but not coping in health and social care: Masking the reality of running organisations beyond safe design capacity. Syst. Dyn. Rev. 2007, 23, 371–389. [Google Scholar] [CrossRef]
- Abdel-Hamid, T.K. Modeling the dynamics of human energy regulation and its implications for obesity treatment. Syst. Dyn. Rev. J. Syst. Dyn. Soc. 2002, 18, 431–471. [Google Scholar] [CrossRef]
- Frerichs, L.M.; Araz, O.M.; Huang, T.T.-K. Modeling social transmission dynamics of unhealthy behaviors for evaluating prevention and treatment interventions on childhood obesity. PLoS ONE 2013, 8, e82887. [Google Scholar] [CrossRef]
- Liu, S.; Osgood, N.; Gao, Q.; Xue, H.; Wang, Y. Systems simulation model for assessing the sustainability and synergistic impacts of sugar-sweetened beverages tax and revenue recycling on childhood obesity prevention. J. Oper. Res. Soc. 2016, 67, 708–721. [Google Scholar] [CrossRef]
- Powell, K.E.; Kibbe, D.L.; Ferencik, R.; Soderquist, C.; Phillips, M.A.; Vall, E.A.; Minyard, K.J. Systems thinking and simulation modeling to inform childhood obesity policy and practice. Public Health Rep. 2017, 132, 33S–38S. [Google Scholar] [CrossRef]
- Roberts, N.; Li, V.; Atkinson, J.-A.; Heffernan, M.; McDonnell, G.; Prodan, A.; Freebairn, L.; Lloyd, B.; Nieuwenhuizen, S.; Mitchell, J. Can the Target Set for Reducing Childhood Overweight and Obesity Be Met? A System Dynamics Modelling Study in New South Wales, Australia. Syst. Res. Behav. Sci. 2019, 36, 36–52. [Google Scholar] [CrossRef]
- Sabounchi, N.S.; Hovmand, P.S.; Osgood, N.D.; Dyck, R.F.; Jungheim, E.S. A novel system dynamics model of female obesity and fertility. Am. J. Public Health 2014, 104, 1240–1246. [Google Scholar] [CrossRef] [PubMed]
- Jalali, M.; Rahmandad, H.; Bullock, S.; Ammerman, A. Dynamics of obesity interventions inside organizations. In Proceedings of the 32nd International Conference of the System Dynamics Society, Delft, The Netherlands, 20–24 July 2014. [Google Scholar]
- Meisel, J.D.; Sarmiento, O.L.; Olaya, C.; Lemoine, P.D.; Valdivia, J.A.; Zarama, R. Towards a novel model for studying the nutritional stage dynamics of the Colombian population by age and socioeconomic status. PLoS ONE 2018, 13, e0191929. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.-J.; Xue, H.; Liu, S.; Huang, T.T.K.; Wang, Y.C.; Wang, Y. Obesity trend in the United States and economic intervention options to change it: A simulation study linking ecological epidemiology and system dynamics modeling. Public Health 2018, 161, 20–28. [Google Scholar] [CrossRef]
- Abidin, N.Z.; Zulkepli, J.H.; Zaibidi, N.Z. The effect of food portion sizes on the obesity prevention using system dynamics modelling. In AIP Conference Proceedings, Proceedings of Statistics and Operational Research International Conference; American Institute of Physics: College Park, MD, USA, 2014; Volume 1613, pp. 436–443. [Google Scholar]
- Allender, S.; Owen, B.; Kuhlberg, J.; Lowe, J.; Nagorcka-Smith, P.; Whelan, J.; Bell, C. A community based systems diagram of obesity causes. PLoS ONE 2015, 10, e0129683. [Google Scholar] [CrossRef] [PubMed]
- Miller, R.L.; Levine, R.L.; McNall, M.A.; Khamarko, K.; Valenti, M.T. A dynamic model of client recruitment and retention in community-based HIV prevention programs. Health Promot. Pract. 2011, 12, 135–146. [Google Scholar] [CrossRef]
- Dangerfield, B.C.; Fang, Y.; Roberts, C.A. Model-based scenarios for the epidemiology of HIV/AIDS: The consequences of highly active antiretroviral therapy. Syst. Dyn. Rev. J. Syst. Dyn. Soc. 2001, 17, 119–150. [Google Scholar] [CrossRef]
- Kok, S.; Rutherford, A.R.; Gustafson, R.; Barrios, R.; Montaner, J.S.; Vasarhelyi, K. Optimizing an HIV testing program using a system dynamics model of the continuum of care. Health Care Manag. Sci. 2015, 18, 334–362. [Google Scholar] [CrossRef]
- Lebcir, R.M.; Atun, R.A.; Coker, R.J. System Dynamic simulation of treatment policies to address colliding epidemics of tuberculosis, drug resistant tuberculosis and injecting drug users driven HIV in Russia. J. Oper. Res. Soc. 2010, 61, 1238–1248. [Google Scholar] [CrossRef]
- Atun, R.A.; Lebcir, R.M.; McKee, M.; Habicht, J.; Coker, R.J. Impact of joined-up HIV harm reduction and multidrug resistant tuberculosis control programmes in Estonia: System dynamics simulation model. Health Policy 2007, 81, 207–217. [Google Scholar] [CrossRef]
- Lounsbury, D.W.; Schwartz, B.; Palma, A.; Blank, A. Simulating patterns of patient engagement, treatment adherence, and viral suppression: A system dynamics approach to evaluating HIV care management. AIDS Patient Care STDs 2015, 29, S55–S63. [Google Scholar] [CrossRef] [PubMed]
- Zou, X.; Xu, Y.; Chen, W.; Xia, Y.; Liu, Y.; Gong, C.; Ling, L. Strategies to control HIV and HCV in methadone maintenance treatment in Guangdong Province, China: A system dynamic modeling study. Subst. Abuse Treat. Prev. Policy 2018, 13, 1. [Google Scholar] [CrossRef] [PubMed]
- Shariatpanahi, S.P.; Jafari, A.; Sadeghipour, M.; Azadeh-Fard, N.; Majidzadeh-A, K.; Farahmand, L.; Ansari, A.M. Assessing the effectiveness of disease awareness programs: Evidence from Google Trends data for the world awareness dates. Telemat. Inform. 2017, 34, 904–913. [Google Scholar] [CrossRef]
- Barber, P.; López-Valcárcel, B.G. Forecasting the need for medical specialists in Spain: Application of a system dynamics model. Hum. Resour. Health 2010, 8, 24. [Google Scholar] [CrossRef]
- Lodi, A.; Tubertini, P.; Grilli, R.; Mazzocchetti, A.; Ruozi, C.; Senese, F. Needs forecast and fund allocation of medical specialty positions in Emilia-Romagna (Italy) by system dynamics and integer programming. Health Syst. 2016, 5, 213–236. [Google Scholar] [CrossRef]
- Wu, M.-H.; Yu, J.-Y.; Huang, C.-H. Theoretical system dynamics modeling for Taiwan pediatric workforce in an era of national health insurance and low birth rates. Pediatr. Neonatol. 2013, 54, 389–396. [Google Scholar] [CrossRef] [PubMed]
- Vanderby, S.A.; Carter, M.W.; Latham, T.; Feindel, C. Modelling the future of the Canadian cardiac surgery workforce using system dynamics. J. Oper. Res. Soc. 2014, 65, 1325–1335. [Google Scholar] [CrossRef]
- Samah, A.A.; Wah, L.K.; Desa, M.I.; Majid, H.A.; Azmi, N.F.M.; Salleh, N.; Bakar, A.A.; Manual, A. Decision Support System Using System Dynamics Simulation Modelling for Projection of Dentist Supply. In Proceedings of the 2014 International Conference on Computer Assisted System in Health, Kuala Lumpur, Malaysia, 19–21 December 2014; pp. 22–25. [Google Scholar]
- Ansah, J.P.; De Korne, D.; Bayer, S.; Pan, C.; Jayabaskar, T.; Matchar, D.B.; Lew, N.; Phua, A.; Koh, V.; Lamoureux, E. Future requirements for and supply of ophthalmologists for an aging population in Singapore. Hum. Resour. Health 2015, 13, 86. [Google Scholar] [CrossRef]
- Taba, S.T.; Atkinson, S.R.; Lewis, S.; Chung, K.S.K.; Hossain, L. A systems life cycle approach to managing the radiology profession: An Australian perspective. Aust. Health Rev. 2015, 39, 228–239. [Google Scholar] [CrossRef]
- De Silva, D. How many doctors should we train for Sri Lanka? System dynamics modelling for training needs. Ceylon Med. J. 2017, 62, 233–237. [Google Scholar] [CrossRef]
- Ishikawa, T.; Fujiwara, K.; Ohba, H.; Suzuki, T.; Ogasawara, K. Forecasting the regional distribution and sufficiency of physicians in Japan with a coupled system dynamics—Geographic information system model. Hum. Resour. Health 2017, 15, 64. [Google Scholar] [CrossRef] [PubMed]
- Abas, Z.A.; Ramli, M.R.; Desa, M.I.; Saleh, N.; Hanafiah, A.N.; Aziz, N.; Abidin, Z.Z.; Shibghatullah, A.S.; Rahman, A.F.N.A.; Musa, H. A supply model for nurse workforce projection in Malaysia. Health Care Manag. Sci. 2018, 21, 573–586. [Google Scholar] [CrossRef] [PubMed]
- Morii, Y.; Ishikawa, T.; Suzuki, T.; Tsuji, S.; Yamanaka, M.; Ogasawara, K.; Yamashina, H. Projecting future supply and demand for physical therapists in Japan using system dynamics. Health Policy Technol. 2019, 8, 118–127. [Google Scholar] [CrossRef]
- Anderson, G.; Horvath, J. The growing burden of chronic disease in America. Public Health Rep. 2004, 119, 263–270. [Google Scholar] [CrossRef]
- Bernell, S.; Howard, S.W. Use your words carefully: What is a chronic disease? Front. Public Health 2016, 4, 159. [Google Scholar] [CrossRef]
- De Andrade, L.; Lynch, C.; Carvalho, E.; Rodrigues, C.G.; Vissoci, J.R.N.; Passos, G.F.; Pietrobon, R.; Nihei, O.K.; de Barros Carvalho, M.D. System dynamics modeling in the evaluation of delays of care in ST-segment elevation myocardial infarction patients within a tiered health system. PLoS ONE 2014, 9, e103577. [Google Scholar] [CrossRef]
- Tejada, J.J.; Ivy, J.S.; King, R.E.; Wilson, J.R.; Ballan, M.J.; Kay, M.G.; Diehl, K.M.; Yankaskas, B.C. Combined DES/SD model of breast cancer screening for older women, II: Screening-and-treatment simulation. IIE Trans. 2014, 46, 707–727. [Google Scholar] [CrossRef]
- Liew, H.P. Potential Roles of Screening Mammography and Clinical Breast Examination in Affecting Breast Cancer Trends in Nebraska. Health Behav. Policy Rev. 2018, 5, 56–64. [Google Scholar] [CrossRef]
- Palma, A.; Lounsbury, D.W.; Schlecht, N.F.; Agalliu, I. A system dynamics model of serum prostate-specific antigen screening for prostate cancer. Am. J. Epidemiol. 2015, 183, 227–236. [Google Scholar] [CrossRef]
- Hallberg, S.; Claeson, M.; Holmström, P.; Paoli, J.; Larkö, A.-M.W.; Gonzalez, H. Developing a simulation model for the patient pathway of cutaneous malignant melanoma. Oper. Res. Health Care 2015, 6, 23–30. [Google Scholar] [CrossRef]
- Kenealy, T.; Rees, D.; Sheridan, N.; Moffitt, A.; Tibby, S.; Homer, J. A ‘whole of system’approach to compare options for CVD interventions in counties Manukau. Aust. N. Z. J. Public Health 2012, 36, 263–268. [Google Scholar] [CrossRef] [PubMed]
- Lich, K.H.; Tian, Y.; Beadles, C.A.; Williams, L.S.; Bravata, D.M.; Cheng, E.M.; Bosworth, H.B.; Homer, J.B.; Matchar, D.B. Strategic planning to reduce the burden of stroke among veterans: Using simulation modeling to inform decision making. Stroke 2014, 45, 2078–2084. [Google Scholar] [CrossRef] [PubMed]
- Recio, A.; Linares, C.; Díaz, J. System dynamics for predicting the impact of traffic noise on cardiovascular mortality in Madrid. Environ. Res. 2018, 167, 499–505. [Google Scholar] [CrossRef] [PubMed]
- Loyo, H.K.; Batcher, C.; Wile, K.; Huang, P.; Orenstein, D.; Milstein, B. From model to action: Using a system dynamics model of chronic disease risks to align community action. Health Promot. Pract. 2013, 14, 53–61. [Google Scholar] [CrossRef]
- Kunc, M.; Kazakov, R. Competitive dynamics in pharmaceutical markets: A case study in the chronic cardiac disease market. J. Oper. Res. Soc. 2013, 64, 1790–1799. [Google Scholar] [CrossRef]
- Brittin, J.; Araz, O.M.; Nam, Y.; Huang, T.-K. A system dynamics model to simulate sustainable interventions on chronic disease outcomes in an urban community. J. Simul. 2015, 9, 140–155. [Google Scholar] [CrossRef]
- Kang, H.; Nembhard, H.B.; Ghahramani, N.; Curry, W. A system dynamics approach to planning and evaluating interventions for chronic disease management. J. Oper. Res. Soc. 2018, 69, 987–1005. [Google Scholar] [CrossRef]
- Zare Mehrjerdi, Y. A dynamic systems approach to weight related health problems. Int. J. Qual. Reliab. Manag. 2013, 30, 571–589. [Google Scholar] [CrossRef]
- Sugiyama, T.; Goryoda, S.; Inoue, K.; Sugiyama-Ihana, N.; Nishi, N. Construction of a simulation model and evaluation of the effect of potential interventions on the incidence of diabetes and initiation of dialysis due to diabetic nephropathy in Japan. BMC Health Serv. Res. 2017, 17, 833. [Google Scholar] [CrossRef]
- Milstein, B.; Jones, A.; Homer, J.B.; Murphy, D.; Essien, J.; Seville, D. Peer reviewed: Charting plausible futures for diabetes prevalence in the United States: A role for system dynamics simulation modeling. Prev. Chronic. Dis. 2007, 4, 1–8. [Google Scholar]
- Jones, A.P.; Homer, J.B.; Murphy, D.L.; Essien, J.D.; Milstein, B.; Seville, D.A. Understanding diabetes population dynamics through simulation modeling and experimentation. Am. J. Public Health 2006, 96, 488–494. [Google Scholar] [CrossRef] [PubMed]
- Montazemi, A.R.; Pittaway, J.; Saremi, H.Q. Assessment of Ubiquitous Healthcare Information Systems Benefits. In Proceedings of the AMCIS, Lima, Peru, 12–15 August 2010; p. 121. [Google Scholar]
- Guariguata, L.; Guell, C.; Samuels, T.A.; Rouwette, E.; Woodcock, J.; Hambleton, I.R.; Unwin, N. Systems Science for Caribbean Health: The development and piloting of a model for guiding policy on diabetes in the Caribbean. Health Res. Policy Syst. 2016, 14, 79. [Google Scholar] [CrossRef] [PubMed]
- Ansah, J.P.; Koh, V.; Chiu, C.-T.; Chei, C.-L.; Zeng, Y.; Yin, Z.-X.; Shi, X.-M.; Matchar, D.B. Projecting the Number of Elderly with Cognitive Impairment in China Using a Multi-State Dynamic Population Model. Syst. Dyn. Rev. 2017, 33, 89–111. [Google Scholar] [CrossRef]
- Thompson, J.P.; Riley, C.M.; Eberlein, R.L. Modelling for Insight: The Case of Dementia in Singapore. Syst. Res. Behav. Sci. 2014, 31, 227–235. [Google Scholar] [CrossRef]
- Hwang, W.-S.; Choi, Y.-H. Socio-economic impact of the mHealth adoption in managing diabetes. Technol. Anal. Strateg. Manag. 2019, 31, 791–802. [Google Scholar] [CrossRef]
- Homer, J.; Hirsch, G.; Minniti, M.; Pierson, M. Models for collaboration: How system dynamics helped a community organize cost-effective care for chronic illness. Syst. Dyn. Rev. J. Syst. Dyn. Soc. 2004, 20, 199–222. [Google Scholar] [CrossRef]
- Brailsford, S.C.; Desai, S.M.; Viana, J. Towards the holy grail: Combining system dynamics and discrete-event simulation in healthcare. In Proceedings of the Winter Simulation Conference, Baltimore, MD, USA, 5–8 December 2010; pp. 2293–2303. [Google Scholar]
- Chahal, K.; Eldabi, T. Applicability of hybrid simulation to different modes of governance in UK healthcare. In Proceedings of the 2008 Winter Simulation Conference, Miami, FL, USA, 7–10 December 2008; pp. 1469–1477. [Google Scholar]
- Viana, J. Reflections on two approaches to hybrid simulation in healthcare. In Proceedings of the Winter Simulation Conference 2014, Savannah, GA, USA, 8–11 December 2014; pp. 1585–1596. [Google Scholar]
- Brailsford, S.C.; Hilton, N.A. A Comparison of Discrete Event Simulation and System Dynamics for Modelling Health Care Systems; University of Southampton: Southampton, UK, 2001. [Google Scholar]
- Laker, L.F.; Torabi, E.; France, D.J.; Froehle, C.M.; Goldlust, E.J.; Hoot, N.R.; Kasaie, P.; Lyons, M.S.; Barg-Walkow, L.H.; Ward, M.J. Understanding emergency care delivery through computer simulation modeling. Acad. Emerg. Med. 2018, 25, 116–127. [Google Scholar] [CrossRef]
- Marshall, D.A.; Burgos-Liz, L.; IJzerman, M.J.; Crown, W.; Padula, W.V.; Wong, P.K.; Pasupathy, K.S.; Higashi, M.K.; Osgood, N.D. Selecting a dynamic simulation modeling method for health care delivery research—Part 2: Report of the ISPOR Dynamic Simulation Modeling Emerging Good Practices Task Force. Value Health 2015, 18, 147–160. [Google Scholar] [CrossRef]
- Gunal, M.M. A guide for building hospital simulation models. Health Syst. 2012, 1, 17–25. [Google Scholar] [CrossRef]
- Morgan, J.S.; Belton, V.; Howick, S. Lessons from mixing OR methods in practice: Using DES and SD to explore a radiotherapy treatment planning process. Health Syst. 2016, 5, 166–177. [Google Scholar] [CrossRef]
- Abdelghany, M.; Eltawil, A.B. Individual versus integrated simulation techniques in healthcare applications. In Proceedings of the 2014 IEEE International Conference on Industrial Engineering and Engineering Management, Selangor Darul Ehsan, Malaysia, 9–12 December 2014; pp. 1214–1218. [Google Scholar]
- Abdelghany, M.; Eltawil, A.B. Linking approaches for multi-methods simulation in healthcare systems planning and management. Int. J. Ind. Syst. Eng. 2017, 26, 275–290. [Google Scholar] [CrossRef]
- Chahal, K.; Eldabi, T.; Young, T. A conceptual framework for hybrid system dynamics and discrete event simulation for healthcare. J. Enterp. Inf. Manag. 2013, 26, 50–74. [Google Scholar] [CrossRef]
- Djanatliev, A.; German, R. Prospective healthcare decision-making by combined system dynamics, discrete-event and agent-based simulation. In Proceedings of the 2013 Winter Simulation Conference: Simulation: Making Decisions in a Complex World, Washington, DC, USA, 8–11 December 2013; pp. 270–281. [Google Scholar]
- Zulkepli, J.; Eldabi, T. Towards a framework for conceptual model hybridization in healthcare. In Proceedings of the 2015 Winter Simulation Conference (WSC), Huntington Beach, CA, USA, 6–9 December 2015; pp. 1597–1608. [Google Scholar]
- Townshend, J.R.P.; Turner, H.S. Analysing the effectiveness of Chlamydia screening. J. Oper. Res. Soc. 2000, 51, 812–824. [Google Scholar] [CrossRef]
- Evenden, D.; Harper, P.R.; Brailsford, S.C.; Harindra, V. System Dynamics modeling of Chlamydia infection for screening intervention planning and cost-benefit estimation. IMA J. Manag. Math. 2005, 16, 265–279. [Google Scholar] [CrossRef]
- Evenden, D.; Harper, P.R.; Brailsford, S.C.; Harindra, V. Improving the cost-effectiveness of Chlamydia screening with targeted screening strategies. J. Oper. Res. Soc. 2006, 57, 1400–1412. [Google Scholar] [CrossRef]
- Viana, J.; Brailsford, S.C.; Harindra, V.; Harper, P.R. Combining discrete-event simulation and system dynamics in a healthcare setting: A composite model for Chlamydia infection. Eur. J. Oper. Res. 2014, 237, 196–206. [Google Scholar] [CrossRef]
- Teng, Y.; Kong, N.; Tu, W. Optimizing strategies for population-based chlamydia infection screening among young women: An age-structured system dynamics approach. BMC Public Health 2015, 15, 639. [Google Scholar] [CrossRef]
- Chalmers, J.; Ritter, A. Subsidising patient dispensing fees: The cost of injecting equity into the opioid pharmacotherapy maintenance system. Drug Alcohol Rev. 2012, 31, 911–917. [Google Scholar] [CrossRef]
- Karanfil, Ö.; Barlas, Y. A dynamic simulator for the management of disorders of the body water homeostasis. Oper. Res. 2008, 56, 1474–1492. [Google Scholar] [CrossRef]
- Hosseinichimeh, N.; Wittenborn, A.K.; Rick, J.; Jalali, M.S.; Rahmandad, H. Modeling and estimating the feedback mechanisms among depression, rumination, and stressors in adolescents. PLoS ONE 2018, 13, e0204389. [Google Scholar] [CrossRef]
- Wittenborn, A.K.; Rahmandad, H.; Rick, J.; Hosseinichimeh, N. Depression as a systemic syndrome: Mapping the feedback loops of major depressive disorder. Psychol. Med. 2016, 46, 551–562. [Google Scholar] [CrossRef]
- Lee, K.A.; Dziadkowiec, O.; Meek, P. A systems science approach to fatigue management in research and health care. Nurs. Outlook 2014, 62, 313–321. [Google Scholar] [CrossRef] [PubMed]
- Apostolopoulos, Y.; Lemke, M.K.; Barry, A.E.; Lich, K.H. Moving alcohol prevention research forward—Part I: Introducing a complex systems paradigm. Addiction 2018, 113, 353–362. [Google Scholar] [CrossRef] [PubMed]
- Apostolopoulos, Y.; Lemke, M.K.; Barry, A.E.; Lich, K.H. Moving alcohol prevention research forward—Part II: New directions grounded in community-based system dynamics modeling. Addiction 2018, 113, 363–371. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Yu, Y. Feedback complexity analysis on community health service based on system dynamic. In Proceedings of the 2012 International Symposium on Management of Technology (ISMOT), Hangzhou, China, 8–9 November 2012; pp. 71–75. [Google Scholar]
- Lingard, H.; Turner, M. Promoting construction workers’ health: A multi-level system perspective. Constr. Manag. Econ. 2017, 35, 239–253. [Google Scholar] [CrossRef]
- Sönmez, S.; Apostolopoulos, Y.; Lemke, M.K.; Hsieh, Y.-C.J.; Karwowski, W. Complexity of occupational health in the hospitality industry: Dynamic simulation modeling to advance immigrant worker health. Int. J. Hosp. Manag. 2017, 67, 95–105. [Google Scholar] [CrossRef]
- Faezipour, M.; Ferreira, S. A system dynamics perspective of patient satisfaction in healthcare. Procedia Comput. Sci. 2013, 16, 148–156. [Google Scholar] [CrossRef]
- Lyons, G.J.; Duggan, J. System dynamics modelling to support policy analysis for sustainable health care. J. Simul. 2015, 9, 129–139. [Google Scholar] [CrossRef]
- Newell, B.; Siri, J. A role for low-order system dynamics models in urban health policy making. Environ. Int. 2016, 95, 93–97. [Google Scholar] [CrossRef]
- Friel, S.; Pescud, M.; Malbon, E.; Lee, A.; Carter, R.; Greenfield, J.; Cobcroft, M.; Potter, J.; Rychetnik, L.; Meertens, B. Using systems science to understand the determinants of inequities in healthy eating. PLoS ONE 2017, 12, e0188872. [Google Scholar] [CrossRef]
- Metcalf, S.S.; Northridge, M.E.; Widener, M.J.; Chakraborty, B.; Marshall, S.E.; Lamster, I.B. Modeling social dimensions of oral health among older adults in urban environments. Health Educ. Behav. 2013, 40, 63S–73S. [Google Scholar] [CrossRef] [PubMed]
- Schröttner, J.; Herzog, A. Development of a system dynamics model for cost estimation for the implantation and revision of hip joint endoprosthesis. In Proceedings of the XII Mediterranean Conference on Medical and Biological Engineering and Computing, Chalkidiki, Greece, 27–30 May 2010; pp. 566–569. [Google Scholar]
- Djanatliev, A.; German, R.; Kolominsky-Rabas, P.; Hofmann, B.M. Hybrid simulation with loosely coupled system dynamics and agent-based models for prospective health technology assessments. In Proceedings of the Winter Simulation Conference, Berlin, Germany, 9–12 December 2012; pp. 1–12. [Google Scholar]
- Goh, Y.M.; Love, P.E.; Stagbouer, G.; Annesley, C. Dynamics of safety performance and culture: A group model building approach. Accid. Anal. Prev. 2012, 48, 118–125. [Google Scholar] [CrossRef] [PubMed]
- Vallerotonda, R.; Leva, A.; Silvia, M.A. Modeling and Training: How System Dynamics is Usable in OSH and MAH Frameworks. Chem. Eng. Trans. 2018, 67, 325–330. [Google Scholar] [CrossRef]
- Edaibat, E.A.; Dever, J.; Stuban, S.M. System dynamics simulation modeling of health information exchange (HIE) adoption and policy intervention: A case study in the State of Maryland. Oper. Res. Health Care 2017, 12, 60–70. [Google Scholar] [CrossRef]
- Merrill, J.A.; Deegan, M.; Wilson, R.V.; Kaushal, R.; Fredericks, K. A system dynamics evaluation model: Implementation of health information exchange for public health reporting. J. Am. Med. Inform. Assoc. 2013, 20, e131–e138. [Google Scholar] [CrossRef] [PubMed]
- Alkayid, K.; Hasan, H.; Meloche, J.A. Simulating information exchanges to investigate the utility of public health web sites. Transform. Gov. People Process Policy 2009, 3, 271–288. [Google Scholar] [CrossRef]
- Barlas, Y. Formal aspects of model validity and validation in system dynamics. Syst. Dyn. Rev. J. Syst. Dyn. Soc. 1996, 12, 183–210. [Google Scholar] [CrossRef]
- Koelling, P.; Schwandt, M.J. Health systems: A dynamic system-benefits from system dynamics. In Proceedings of the Winter Simulation Conference, Orlando, FL, USA, 4 December 2005; p. 7. [Google Scholar] [CrossRef]






| Reference | Area of Application | Simulation Method | Number of Papers Included |
|---|---|---|---|
| [1] | Healthcare | Operations research approaches | 342 |
| [2] | Healthcare | Different simulation methods | 251 |
| [3] | Healthcare delivery and population health | Simulation techniques | 182 |
| [11] | Healthcare | Different simulation methods | 201 |
| [13] | Healthcare | Different simulation methods | 232 |
| [16] | All fields | System dynamics | 800 |
| [17] | All fields | System dynamics | 1441 |
| [18] | Emergency departments | Different simulation methods | 106 |
| [19] | Emergency medical services (EMS) | Simulation models | 24 |
| [20] | Emergency departments | Different simulation methods | 254 |
| [21] | Inpatient bed management | Modeling techniques | 92 |
| [22] | Healthcare | Discrete-event simulation | 211 |
| [23] | Health policy | System dynamics | 6 |
| [24] | Healthcare | Discrete-event simulation | Not mentioned |
| [25] | Healthcare | Simulation methodologies | Not applicable |
| [26] | Rheumatoid arthritis | Modeling techniques | 58 |
| [27] | Cancer care | Operations research approaches | 90 |
| [28] | UK healthcare | Operations research approaches | 142 |
| [29] | Mental health | Different simulation methods | 160 |
| Row | Set |
|---|---|
| Test set 1 | (Health OR health care OR medical care) |
| Test set 2 | (System dynamics OR SD) |
| Search 1 | #1 AND #2 |
| Test set 3 | (Disease OR illness OR treatment OR injury OR morbidity) |
| Search 2 | #3 AND #2 |
| Row | Set |
|---|---|
| Test set 1 | (System dynamics OR SD) |
| Test set 2 | (Disorder OR stress) |
| Test set 3 | (Drug OR medication) |
| Test set 4 | (Human body OR human behavior) |
| Search 3 | #1 AND (#2 OR #3 OR #4) |
| Category | Subcategory | Number of Included Papers |
|---|---|---|
| Aging and population | Healthcare demand | 3 |
| Evolution of population | 1 | |
| Communicable diseases | HIV/AIDS, tuberculosis | 11 |
| Chlamydia | 5 | |
| Hepatitis C | 2 | |
| Influenza | 2 | |
| Ebola virus | 1 | |
| Foot-and-mouth disease | 1 | |
| Middle East Respiratory Syndrome (MERS) Coronavirus (CoV) | 1 | |
| Severe acute respiratory syndrome coronavirus (SARS-CoV) | 1 | |
| Other infectious diseases | 11 | |
| Cost and price in healthcare | Pharmaceutical fees | 1 |
| Cost–benefit analysis | 1 | |
| Insurance economics | 1 | |
| Patient dispensing fees | 1 | |
| Performance-based payment system | 1 | |
| Disorder and stress | Obesity | 14 |
| Depression | 3 | |
| Body Water Homeostasis | 1 | |
| Fatigue | 1 | |
| Post-traumatic stress disorder (PTSD) | 1 | |
| Workplace stress | 1 | |
| Drugs and medications | Alcohol misuse | 3 |
| Opioid use and misuse | 2 | |
| Nicotine product | 1 | |
| Pain medicine | 1 | |
| Use/abuse of drugs | 1 | |
| Healthcare operations | Patient flow | 17 |
| Emergency department | 7 | |
| Hospital | 3 | |
| Patient service centers | 2 | |
| Behavior of nurses | 1 | |
| Clinical knowledge | 1 | |
| Clinical workforce | 1 | |
| Neonatal care services | 1 | |
| Outpatient clinics | 1 | |
| Patient access to general practice | 1 | |
| Radiotherapy department | 1 | |
| Referrals system | 1 | |
| Telehealth | 1 | |
| Healthcare systems | System improvement | 4 |
| Mental health care | 2 | |
| Urban health | 2 | |
| Community health services | 2 | |
| Construction workers’ health | 1 | |
| Curative and preventive services | 1 | |
| Healthcare delivery systems | 1 | |
| Healthcare affordability and accessibility | 1 | |
| Immigrant worker health | 1 | |
| Military psychological health system | 1 | |
| National healthcare system | 1 | |
| One Health concept | 1 | |
| Public health | 1 | |
| Rural minority health | 1 | |
| Sustainability in healthcare | 1 | |
| Sustainable health care | 1 | |
| Youth health | 1 | |
| Other healthcare systems | 4 | |
| Human body and behavior | Body weight | 1 |
| Functional loss | 1 | |
| Healthy eating | 1 | |
| Lower back pain (LBP) | 1 | |
| Oral health care | 2 | |
| Medical treatment and devices | Chemotherapy | 1 |
| Childhood immunization | 1 | |
| Disease awareness | 1 | |
| Eyecare services | 1 | |
| Hip joint endoprosthesis | 1 | |
| Home hemodialysis (BASIC-HHD) | 1 | |
| Knee implants | 1 | |
| Maintenance procedure | 1 | |
| Mobile stroke units | 1 | |
| Prospective Health Technology Assessment (ProHTA) | 1 | |
| Non-communicable diseases | Diabetes | 7 |
| Cancer | 4 | |
| Cardiovascular disease | 4 | |
| Dementia | 3 | |
| Intellectual disabilities (ID) | 2 | |
| Asthma | 1 | |
| Cognitive impairment | 1 | |
| End-stage renal disease | 1 | |
| Hernia | 1 | |
| Other chronic diseases | 7 | |
| Healthcare process and policy | Health interventions | 5 |
| Long-term care policy | 2 | |
| Care planning | 1 | |
| Clinical decision thresholds | 1 | |
| Lean deployment strategies | 1 | |
| Policy implementation | 1 | |
| Strategic planning | 1 | |
| Successful health programs | 1 | |
| Workforce planning | 1 | |
| Safety in healthcare | Occupational safety and health | 2 |
| Risk of adverse events | 1 | |
| System safety | 1 | |
| Simulation in healthcare | Simulations comparison | 7 |
| Hybrid modeling | 6 | |
| Introduction to system dynamics | 1 | |
| Specialty in neonatology, obstetrics, gynecology | Infant mortality | 4 |
| Cesarean delivery | 1 | |
| Supply and demand in healthcare | Workforce demand | 12 |
| Supply chain | 3 | |
| Care supply and demand | 1 | |
| Blood supply chain | 1 | |
| Internal service supply chains | 1 | |
| Medical demand | 1 | |
| Need for facilities | 1 | |
| Technology and information in healthcare | Electronic health records | 4 |
| Health information exchange (HIE) | 3 | |
| Cybersecurity | 1 | |
| Health information technology | 1 | |
| Health information systems | 1 | |
| Sharing of information | 1 |
| Row | Quality Criteria |
|---|---|
| 1 | Presenting clear objectives |
| 2 | Presenting clear scenarios and interventions |
| 3 | Presenting clear outcomes variables by graphs, charts, or tables |
| 4 | Describing the development of an SD model/framework or presenting a detailed model/framework |
| 5 | Presenting and explaining model parameters |
| 6 | Improving the quality of data by using stakeholders’ engagement, surveys, interviews, and databases |
| 7 | Validating models |
| 8 | Presenting clear results |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Davahli, M.R.; Karwowski, W.; Taiar, R. A System Dynamics Simulation Applied to Healthcare: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 5741. https://doi.org/10.3390/ijerph17165741
Davahli MR, Karwowski W, Taiar R. A System Dynamics Simulation Applied to Healthcare: A Systematic Review. International Journal of Environmental Research and Public Health. 2020; 17(16):5741. https://doi.org/10.3390/ijerph17165741
Chicago/Turabian StyleDavahli, Mohammad Reza, Waldemar Karwowski, and Redha Taiar. 2020. "A System Dynamics Simulation Applied to Healthcare: A Systematic Review" International Journal of Environmental Research and Public Health 17, no. 16: 5741. https://doi.org/10.3390/ijerph17165741
APA StyleDavahli, M. R., Karwowski, W., & Taiar, R. (2020). A System Dynamics Simulation Applied to Healthcare: A Systematic Review. International Journal of Environmental Research and Public Health, 17(16), 5741. https://doi.org/10.3390/ijerph17165741







