Opposite Effects of Work-Related Physical Activity and Leisure-Time Physical Activity on the Risk of Diabetes in Korean Adults
Abstract
:1. Introduction
2. Methods
2.1. Data Collection
2.2. Assessment of DWPA and LTPA
2.3. Other Variables
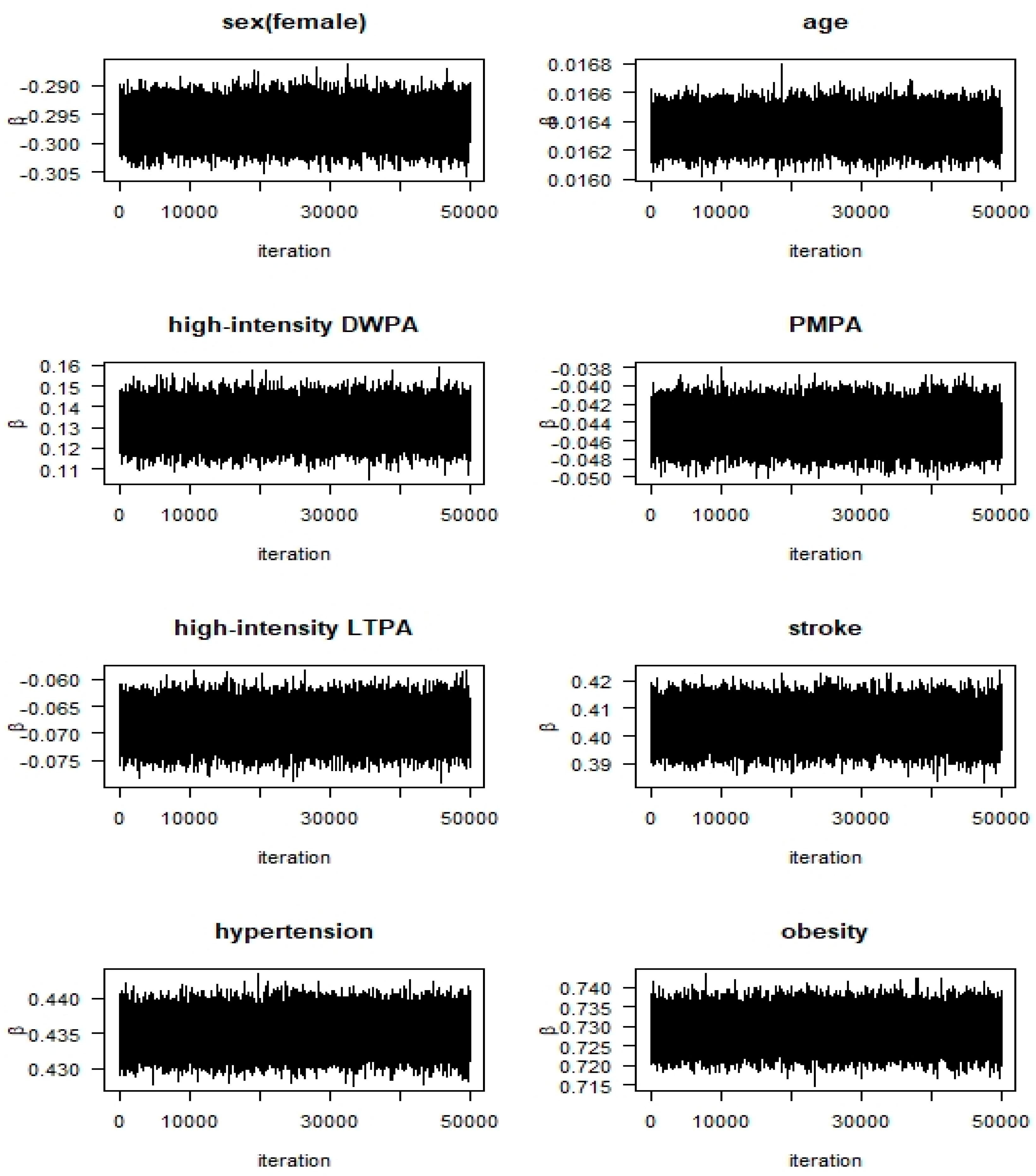
2.4. Statistical Analysis
3. Results
3.1. Characteristics of the Sample
3.2. Clinical Diagnosis of Diabetes
3.3. Factors Affecting the Risk of Diabetes
4. Discussion
5. Conclusions
Funding
Conflicts of Interest
References
- Chen, L.; Pei, J.H.; Kuang, J.; Chen, H.M.; Chen, Z.; Li, Z.W.; Yang, H.Z. Effect of lifestyle intervention in patients with type 2 diabetes: A meta-analysis. Metabolism 2015, 64, 338–347. [Google Scholar] [CrossRef] [PubMed]
- Lin, X.; Zhang, X.; Guo, J.; Roberts, C.K.; McJenzie, S.; Wu, W.C.; Liu, S.; Song, Y. Effects of exercise training on cardiorespiratory fitness and biomarkers of cardiometabolic health: A systematic review and meta-analysis of randomized controlled trials. J. Am. Heart Assoc. 2015, 4, e002014. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Colberg, S.R.; Sigal, R.J.; Yardley, J.E.; Riddell, M.C.; Dunstan, D.W.; Dempsey, P.C.; Horton, E.S.; Castorino, K.; Tate, D.F. Physical activity/exercise and diabetes: A position statement of the American diabetes association. Diabetes Care 2016, 39, 2065–2079. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Faienza, M.F.; Lassandro, G.; Chiarito, M.; Valente, F.; Ciaccia, L.; Giordano, P. How physical activity across the lifespan can reduce the impact of bone aging: A little review. Int. J. Environ. Res. Public Health 2020, 17, 1862. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brach, J.S.; Simonsick, E.M.; Kritchevsky, S. The association between physical function and lifestyle activity and exercise in the health, aging and body composition study. J. Am. Geriatr. Soc. 2004, 52, 502–509. [Google Scholar] [CrossRef]
- Jonker, J.T.; De Laet, C.; Franco, O.H.; Peters, A.; Mackenbach, J.; Nusselder, W.J. Physical activity and life expectance with and without diabetes: Life table analysis of the Framingham Heart Study. Diabetes Care 2006, 29, 38–43. [Google Scholar] [CrossRef]
- Kim, Y.H. Effect of physical activity promotion program on physical function and quality of life in elderly. J. Korean Biol. Nurs. Sci. 2008, 10, 11–18. [Google Scholar]
- Nakanishi, N.; Takatorige, T.; Suzuki, K. Daily life activity and risk of developing impaired fasting glucose or type 2 diabetes in middle-aged Japanese men. Diabetologia 2004, 47, 1768–1775. [Google Scholar] [CrossRef]
- Park, J.Y.; Kim, N.H. The relationship between physical activity and insulin resistance in the middle-aged adults. J. Korean Biol. Nurs. Sci. 2011, 13, 245–252. [Google Scholar]
- Wannamethee, S.G.; Shaper, A.G.; Aberti, K.G. Physical activity, metabolic factors, and the incidence of coronary heart disease and type 2 diabetes. Arch. Inter. Med. 2000, 160, 2108–2116. [Google Scholar] [CrossRef] [Green Version]
- Physical Activity Guidelines Advisory Committee; U.S. Department of Health and Human Services. 2018 Physical Activity Guidelines Advisory Committee Scientific Report. Available online: https://www.health.gov/PAGuidelines/ (accessed on 22 July 2020).
- World Health Organization. Global Recommendations on Physical Activity for Health. 2010. Available online: https://www.who.int/dietphysicalactivity/factsheet_recommendations/en/ (accessed on 23 July 2020).
- Haapanen, N.; Miilunpalo, S.; Vuori, I.; Oja, P.; Pasanen, M. Association of leisure time physical activity with the risk of coronary heart disease, hypertension and diabetes in middle-aged men and women. Int. J. Epidemiol. 1997, 26, 739–747. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Holtermann, A.; Hansen, J.V.; Burr, H.; Søgaard, K.; Sjøgaard, G. The health paradox of occupational and leisure-time physical activity. Br. J. Sports Med. 2012, 46, 291–295. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Okada, K.; Hayashi, T.; Tsumura, K.; Suematsu, C.; Endo, G.; Fujii, S. Leisure-time physical activity at weekends and the risk of Type 2 diabetes mellitus in Japanese men: The Osaka Health Survey. Diabet. Med. 2000, 17, 53–58. [Google Scholar] [CrossRef] [PubMed]
- Villegas, R.; Shu, X.O.; Li, H.; Yang, G.; Matthews, C.E.; Leitzmann, M.; Li, Q.; Cai, H.; Gao, Y.T.; Zheng, W. Physical activity and the incidence of type 2 diabetes in the Shanghai women’s health study. Int. J. Epidemiol. 2006, 35, 1553–1562. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aune, D.; Norat, T.; Leitzmann, M.; Tonstad, S.; Vatten, L.J. Physical activity and the risk type 2 diabetes: A systematic review and dose-response meta-analysis. Eur. J. Epidemiol. 2015, 30, 529–542. [Google Scholar] [CrossRef]
- Honda, T.; Kuwahara, K.; Nakagawa, T.; Yamamoto, S.; Hayash, T.; Mizoue, T. Leisure-time, occupational, and commuting physixal activity and risk of type 2 diabetes in Japanese workers: A cohort study. BMC Public Health 2015, 15, 1004. [Google Scholar] [CrossRef] [Green Version]
- Dickinson, S.; Colagiuri, S.; Faramus, E.; Petocz, P.; Brand-Miller, J.C. Postprandial hyperglycemia and insulin sensitivity differ among lean young adults of different ethnicities. J. Nutr. 2002, 132, 2574–2579. [Google Scholar] [CrossRef] [Green Version]
- Kataoka, M.; Venn, B.J.; Williams, S.M.; Te Morenga, L.A.; Heemels, I.M.; Mann, J.L. Glycaemic responses to glucose and rice in people of Chinese and European ethnicity. Diabet. Med. 2013, 30, e101–e107. [Google Scholar] [CrossRef]
- Venn, B.S.; Williams, S.M.; Mann, J.L. Comparison of postprandial glycaemia in Asians and Caucasians. Diabet. Med. 2010, 27, 1205–1208. [Google Scholar] [CrossRef]
- American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care 2014, 37 (Suppl. 1), S81–S90. [Google Scholar] [CrossRef] [Green Version]
- Won, J.C.; Lee, J.H.; Kim, J.H.; Kang, E.S.; Won, K.C.; Kim, D.J.; Lee, M.K. Diabetes fact sheet in Korea, 2016, an appraisal of current status. Diabetes Metab. J. 2018, 42, 415–424. [Google Scholar] [CrossRef] [PubMed]
- King, P.; Peacock, l.; Donnelly, R. The UK prospective diabetes study (UKPDS): Clinical and therapeutic implications for type 2 diabetes. Br. J. Clin. Pharmacol. 1999, 48, 643–648. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.T.; Chen, C.J.; Gregg, E.W.; Imperatore, G.; Narayan, K.M.V. Impaired fasting glucose and risk of diabetes in Taiwan: Follow-up over 3 years. Diabetes Res. Clin. Pract. 2003, 60, 177–182. [Google Scholar] [CrossRef]
- Shin, H.Y.; Lee, J.Y.; Song, J.; Lee, S.; Lee, J.; Lim, B.; Kim, H.; Huh, S. Cause-of-death statistics in the Republic of Korea, 2014. Korean Med. Assoc. 2016, 59, 221–232. [Google Scholar] [CrossRef] [Green Version]
- Kweon, S.; Kim, Y.; Jang, M.J.; Kim, Y.; Kim, K.; Choi, S.; Chun, C.; Khang, Y.H.; Oh, K. Data resource profile: The Korean National Health and Nutrition Examination Survey(KNHANES). Int. J. Epidemiol. 2014, 43, 69–77. [Google Scholar] [CrossRef] [Green Version]
- Lee, W.J.; Sobrin, L.; Lee, M.J.; Kang, M.H.; Seong, M.; Cho, H. The relationship between diabetic retinopathy and diabetic nephropathy in a population-based study in Korea (KNHANES V-2, 3). Investig. Ophthalmol. Vis. Sci. 2014, 55, 6547–6553. [Google Scholar] [CrossRef] [Green Version]
- Lee, J.; Lee, C.; Min, J.; Kang, D.W.; Kim, J.Y.; Yang, H.I.; Park, J.; Lee, M.K.; Lee, M.Y.; Park, l.; et al. Development of the Korean global physical activity questionnaire: Reliability and validity study. Glob. Health Promot. 2019, 8. [Google Scholar] [CrossRef]
- Munkin, M.K.; Trivedi, P.K. Bayesian analysis of the ordered probit model with endogenous selection. J. Econom. 2008, 143, 334–348. [Google Scholar] [CrossRef]
- Oh, H.S. Important significant factors of health-related quality of life(EQ-5D) by age group in Korea based on KNHANES(2014). J. Korean Data Inf. Sci. Soc. 2017, 28, 297–308. [Google Scholar]
- Heidelberger, P.; Welch, P.D. Simulation run length control in the presence of an initial transient. Oper. Res. 1983, 31, 1109–1144. [Google Scholar] [CrossRef]
- Cowles, M.K.; Carlin, B.P. Markov Chain Monte Carlo convergence diagnostic: A comparative review. J. Am. Stat. Assoc. 1996, 91, 883–904. [Google Scholar] [CrossRef]
- Korean Diabetes Association. Treatment Guideline for Diabetes; KDA: Seoul, Korea, 2019. [Google Scholar]
- Steinbrecher, A.; Erber, E.; Grandinetti, A.; Nigg, C.; Kolonel, L.N.; Maskarinec, G. Physical activity and risk of type 2 diabetes among native Hawaiians, Japanese Americans and Caucasians: The multiethnic cohort. J. Phys. Act. Health 2012, 9, 634–641. [Google Scholar] [CrossRef] [PubMed]
- Hu, G.; Qiao, Q.; Silventoinen, K.; Eriksson, J.G.; Jousilahti, P.; Lindstrom, J.; Valle, T.T.; Nissinen, A.; Tuomilehto, J. Occupational, commuting, and leisure-time physical activity in relation to risk for Type 2 diabetes in middle-aged Finnish men and women. Diabetologia 2003, 46, 322–329. [Google Scholar] [CrossRef] [PubMed]
- Chien, K.L.; Chen, M.F.; Hsu, H.C.; Su, T.C.; Lee, Y.T. Sports activity and risk of type 2 diabetes in Chinese. Diabetes Res. Clin. 2009, 84, 311–318. [Google Scholar] [CrossRef]
- Jang, H.M.; Park, S.K.; Kim, I.A.; Baek, S.H. Association of work physical activity and leisure-time physical activity and metabolic syndrome in male adult workers: The sixth Korea National Health and Nutrition Examination Survey in 2014. Korean J. Fam. Pract. 2017, 7, 758–763. [Google Scholar] [CrossRef]
- Ku, P.W.; Chen, L.J.; Fox, K.R.; Chen, Y.H.; Liao, Y.; Lin, C.H. Leisure-time, domestic, and work-related physical activity and their prospective associations with all-cause mortality in patients with cardiovascular disease. Am. J. Cardiol. 2018, 121, 177–181. [Google Scholar] [CrossRef]
- Chen, L.J.; Stevenson, C.; Ku, P.W.; Chang, Y.K.; Chu, D.C. Relationships of leisure-time and non-leisure-time physical activity with depressive symptoms: A population-based study of Taiwanese older adults. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 1–28. [Google Scholar] [CrossRef] [Green Version]
- Chung, H.R.; Perez-Escamilla, R. Risk factors of type 2 diabetes among Korean adults: The 2001 Korean national health and nutrition examination survey. Nutr. Res. Pract. 2009, 3, 286–294. [Google Scholar] [CrossRef]
- Waki, K.; Noda, M.; Sasaki, S.; Matsumura, Y.; Takahashi, Y.; Isogawa, A.; Ohashi, Y.; Kadowaki, T.; Tsugane, S. Alcohol consumption and other risk factors for self-reported diabetes among middle-aged Japanese: A population-based prospective study in the JPHC study cohort I. Diabet. Med. 2005, 22, 323–331. [Google Scholar] [CrossRef]
- Kim, S.M.; Yoon, D.K.; Lee, J.S.; Baik, S.H.; Lee, J.; Choi, D.S.; Na, J.K.; Choi, K.M.; Han, J.H. Prevalence of diabetes and impaired fasting glucose in Korea. Diabetes Care 2006, 29, 226–231. [Google Scholar] [CrossRef] [Green Version]
- Njolstad, I.; Arnesen, E.; Lund-Larsen, P.G. Sex differences in risk factors for clinical diabetes mellitus in a general population: A 12-year follow-up of the Finnmark Study. Am. J. Epidemiol. 1998, 147, 49–58. [Google Scholar] [CrossRef] [PubMed]
- Harreiter, J.; Kautzky-Willer, A. Sex and gender differences in prevention of type 2 diabetes. Front. Endocrinol. 2018, 9, 220. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Factors | Variables | Levels | N | wtd % | Mean (sd) | wtd Mean (sd) |
|---|---|---|---|---|---|---|
| FBG | Normal (<100) | 2837 | 62.85 | |||
| FBG IFG (100–125) | 1385 | 28.89 | ||||
| Diabetes (≥126) | 439 | 8.27 | ||||
| socio- demographic factors | sex | male | 2069 | 49.52 | ||
| female | 2562 | 50.48 | ||||
| residence | urban | 3793 | 84.61 | |||
| rural | 868 | 15.39 | ||||
| marital status | unmarried | 322 | 8.73 | |||
| married | 4339 | 91.27 | ||||
| occupation | no | 1744 | 32.6 | |||
| yes | 2917 | 67.4 | ||||
| age | 30~80(year) | 54.66 (13.83) | 51.54 (13.26) | |||
| household income (monthly) | 1–10 1: <10%–10: >90% | 6.31 (3.20) | 6.73 (3.06) | |||
| education | 1–8 1:unschooled– 8:graduate level | 5.22 (1.63) | 5.47 (1.56) | |||
| health behaviors | drinking | never | 523 | 9.23 | ||
| yes | 4138 | 90.77 | ||||
| smoking | never | 2761 | 55.38 | |||
| <5 pack | 89 | 2.13 | ||||
| ≥5 pack | 1811 | 42.49 | ||||
| high-intensity DWPA | no | 4614 | 98.54 | |||
| yes | 47 | 14.6 | ||||
| moderate-intensity DWPA | no | 4402 | 93.75 | |||
| yes | 259 | 6.25 | ||||
| PMPA | no | 2209 | 47.73 | |||
| yes | 2452 | 52.17 | ||||
| high-intensity LTPA | no | 4217 | 88.32 | |||
| yes | 444 | 11.68 | ||||
| moderate-intensity LTPA | no | 3588 | 75.20 | |||
| yes | 1078 | 24.53 | ||||
| sedentary time (hour per day) | 7.92 (3.53) | 7.91 (3.55) | ||||
| sleeping time (hour per day) | 7.02 (1.36) | 7.00 (1.31) | ||||
| stress (1: hardly– 4: very much) | 2.13 (0.72) | 2.16 (0.71) | ||||
| chronic diseases | stroke | no | 4546 | 98.06 | ||
| yes | 115 | 1.94 | ||||
| heart disease | no | 4515 | 97.62 | |||
| yes | 146 | 2.38 | ||||
| hypercholesterolemia | no | 3451 | 76.11 | |||
| yes | 1210 | 23.89 | ||||
| hypertension | normal | 1873 | 43.42 | |||
| pre-hypertension | 1197 | 26.69 | ||||
| hypertension | 1591 | 29.89 | ||||
| obesity | normal(BMI < 25) | 3004 | 64.50 | |||
| overweight (BMI25–30) | 1427 | 30.61 | ||||
| obesity (BMI ≥ 30) | 230 | 4.89 | ||||
| FBG | Diabetes Diagnosis | Wald F † | p-Value | |
|---|---|---|---|---|
| Yes (wtd%) | No (wtd%) | |||
| normal | 48(1.26) | 2789(98.74) | 111.27 | 0.000 |
| IFG | 153(9.46) | 1232(90.54) | ||
| diabetes | 280(61.55) | 159(38.45) | ||
| Frequency | Normal | IFG | Diabetes |
|---|---|---|---|
| observed frequency(weighted) | 0.6285 | 0.2889 | 0.0827 |
| estimated frequency | 0.6059 | 0.3009 | 0.0933 |
| Factors | Variables | (SE) | Marginal Effects | ||
|---|---|---|---|---|---|
| Normal (SE) | IFG (SE) | Diabetes (SE) | |||
| Demographic factors | sex (female) | −0.2963 (0.0023) | 0.1178 (0.0009) | −0.0621 (0.0003) | −0.0563 (0.0006) |
| residence (rural) | 0.0105 (0.0021) | −0.0040 (0.0008) | 0.0027 (0.0005) | 0.0013 (0.0003) | |
| marital status (married) | 0.2340 (0.0031) | −0.0855 (0.0011) | 0.0608 (0.0008) | 0.0247 (0.0003) | |
| occupation (yes) | 0.0727 (0.0018) | −0.0275 (0.0007) | 0.0187 (0.0005) | 0.0088 (0.0002) | |
| age | 0.0164 (0.0000) | −0.0062 (0.0000) | 0.0042 (0.0000) | 0.0020 (0.0000) | |
| household income | 0.0140 (0.0003) | −0.0053 (0.0001) | 0.0036 (0.0001) | 0.0017 (0.0000) | |
| education | −0.0585 (0.0006) | 0.0222 (0.0002) | −0.0150 (0.0002) | −0.0072 (0.0001) | |
| health behaviors | Drinking (yes) | −0.1163 (0.0026) | 0.0458 (0.0010) | −0.0277 (0.0005) | −0.0181 (0.0005) |
| Smoking (<5pack) | 0.2553 (0.0052) | −0.0997 (0.0021) | 0.0619 (0.0012) | 0.0378 (0.0009) | |
| Smoking (≥5pack) | 0.1601 (0.0021) | −0.0611 (0.0008) | 0.0408 (0.0005) | 0.0203 (0.0003) | |
| high-intensity DWPA (yes) | 0.1318 (0.0063) | −0.0510 (0.0025) | 0.0330 (0.0015) | 0.0179 (0.0009) | |
| moderate-intensity DWPA (yes) | 0.0309 (0.0032) | −0.0118 (0.0012) | 0.0079 (0.0008) | 0.0039 (0.0004) | |
| PMPA (yes) | −0.0449 (0.0015) | 0.0171 (0.0006) | −0.0115 (0.0004) | −0.0055 (0.0002) | |
| high-intensity LTPA (yes) | −0.0675 (0.0025) | 0.0254 (0.0009) | −0.0174 (0.0007) | −0.0080 (0.0003) | |
| moderate-intensity LTPA (yes) | −0.0156 (0.0019) | 0.0059 (0.0007) | −0.0040 (0.0005) | −0.0019 (0.0002) | |
| sedentary time | 0.0004 (0.0002) | −0.0002 (0.0001) | 0.0001 (0.0001) | 0.0000 (0.0000) | |
| sleeping time | −0.0140 (0.0006) | 0.0053 (0.0002) | −0.0036 (0.0001) | −0.0017 (0.0001) | |
| stress | 0.0133 (0.0011) | −0.0050 (0.0004) | 0.0034 (0.0003) | 0.0016 (0.0001) | |
| diseases | Stroke (yes) | 0.4039 (0.0049) | −0.1589 (0.0019) | 0.0929 (0.0009) | 0.0660 (0.0010) |
| heart disease (yes) | 0.1608 (0.0044) | −0.0623 (0.0017) | 0.0401 (0.0011) | 0.0222 (0.0007) | |
| hypercholesterolemia (yes) | 0.2279 (0.0017) | −0.0877 (0.0007) | 0.0571 (0.0004) | 0.0306 (0.0003) | |
| pre-hypertension (yes) | 0.2246 (0.0019) | −0.0864 (0.0007) | 0.0563 (0.0005) | 0.0301 (0.0003) | |
| Hypertension (yes) | 0.4354 (0.0020) | −0.1673 (0.0008) | 0.1072 (0.0005) | 0.0601 (0.0003) | |
| Overweight (yes) | 0.3212 (0.0016) | −0.1236 (0.0006) | 0.0799 (0.0004) | 0.0437 (0.0002) | |
| Obesity (yes) | 0.7281 (0.0033) | −0.2842 (0.0012) | 0.1422 (0.0004) | 0.1420 (0.0009) | |
© 2020 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oh, H.S. Opposite Effects of Work-Related Physical Activity and Leisure-Time Physical Activity on the Risk of Diabetes in Korean Adults. Int. J. Environ. Res. Public Health 2020, 17, 5812. https://doi.org/10.3390/ijerph17165812
Oh HS. Opposite Effects of Work-Related Physical Activity and Leisure-Time Physical Activity on the Risk of Diabetes in Korean Adults. International Journal of Environmental Research and Public Health. 2020; 17(16):5812. https://doi.org/10.3390/ijerph17165812
Chicago/Turabian StyleOh, Hyun Sook. 2020. "Opposite Effects of Work-Related Physical Activity and Leisure-Time Physical Activity on the Risk of Diabetes in Korean Adults" International Journal of Environmental Research and Public Health 17, no. 16: 5812. https://doi.org/10.3390/ijerph17165812
APA StyleOh, H. S. (2020). Opposite Effects of Work-Related Physical Activity and Leisure-Time Physical Activity on the Risk of Diabetes in Korean Adults. International Journal of Environmental Research and Public Health, 17(16), 5812. https://doi.org/10.3390/ijerph17165812




