Caring for Family Caregivers of Geriatric Patients: Results of a Participatory Health Research Project on Actual State and Needs of Hospital-Based Care Professionals
Abstract
:1. Introduction
1.1. The German Situation
1.2. Context of the Study
1.3. Aim of the Study
2. Materials and Methods
2.1. Research Strategy
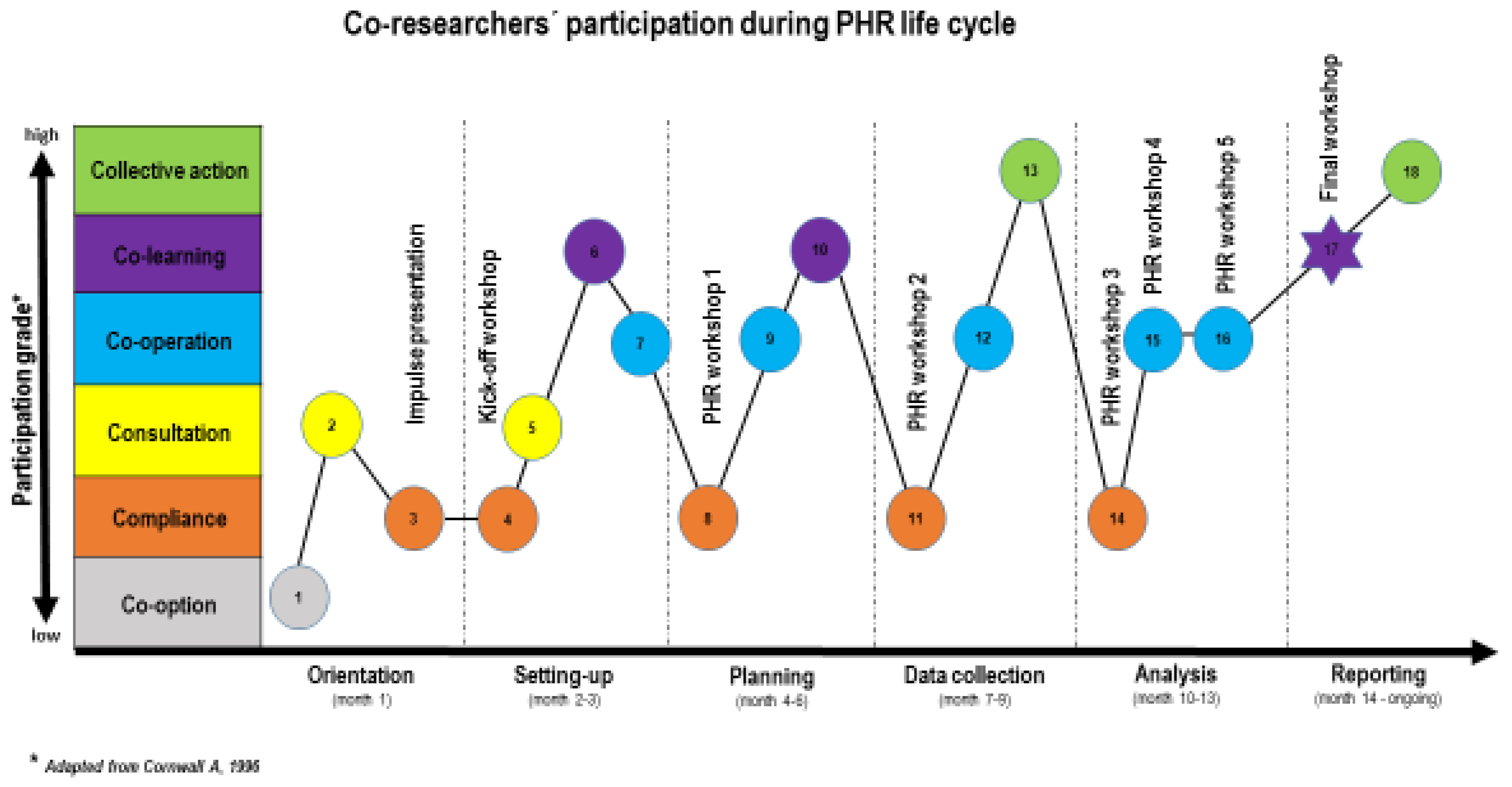
2.2. Formation of the Research Team, Roles, Research Activities
2.3. Documenting and Reflection
2.4. Ethical Considerations
| Phase | Timing (month) | Participation and Contribution | Activity and Methodology | Planned/Expected Outcome |
|---|---|---|---|---|
| Orientation | 1 | AR takes the lead, MDT provides impulses | Start-up: Literature exploration Explorative talks 2-day field visit (interviews, observations) | Gaining a theoretical and practice-based understanding Starting engagement with decision makers and MDT Showing and raising interest within the department Starting topic list to be reflected on in phase 2 |
| Setting-up | 2–3 | AR takes lead, MDT participates | Impulse presentation: (focus on family caregiving and caregiver needs) | Giving feedback concerning AR findings during orientation Raising awareness for caregiver support needs Stimulating the MDT to participate in the PHR process |
| AR prepares basic research requirements MDT takes the lead | Kick-off workshop: Impulse lecture (Focus on PHR strategy) Interactive focus group discussion (brain storming, mind mapping) | Understanding the goals and ethical criteria of PHR § Exploring problem, expectations, and goals of the PHR project Formulating research question AR and members of the MDT who decide to participate as co-researchers are forming the research team | ||
| Planning | 4–6 | AR prepares list of potential methods for qualitative data collection CF stimulates reflection CR ¶ decide on data collection methodology | Project workshop 1: Impulse lecture (emphasis on advantages and disadvantages) Interactive focus group discussion | Discussing pros and cons of potential methods of qualitative data collection Sharing experiences with previous research and exploring practicability within the department and per peer group Stimulating continuous professional development Specifying participant subgroups for data collection Selecting appropriate qualitative data collection methodology, and assigning a method for each participant subgroup |
| Data collection | 7–9 | CR take the lead, AR and CF support the decision-making process | Project workshop 2: Explorative focus group discussion | Determining plan of action for qualitative data collection (Gantt chart) Designing a ‘question catalogue’ (53 questions regarding caregiver needs, information, knowledge, skills, resources, mandate, and support offer). Preparing a checklist for data collection |
| CR take the lead, AF and CF support the process | Field work: within peer groups | Collecting qualitative data in each sub-group Offering technical, practical, and communicational support Supporting data storage | ||
| Analysis | 10–13 | AR leads the session CF provides practical impulses CR decide on further steps and new team composition | Project workshop 3: Interactive impulse session (emphasis on data analysis) | Gaining an understanding of the process of data analysis, required resources and team commitment Building a data analyzing team (from each profession one person is part of this team plus AR/CF) |
| AF, CF and CR analyze data | Project workshop 4–5: Structured analyzing process | Analyzing qualitative data per subgroup Merging data from subgroups Formulating conceptual recommendations | ||
| Critical reflection on PHR | 14 | CR, CF and AF share their experiences | Final workshop (closing down): Brain storming followed by mind mapping | Critically discussing participation grades and perceived benefits and limitations of the PHR approach in general and within their own roles (CR, CF and AR) |
| Reporting | 14 | CR report on the findings AR and CF support the reporting process | Final workshop (closing down): Data presentation | Final report: actual state and needs of the MDT with respect to holistic family caregiver support |
| 14-ongoing | Individual members of research team | Individual reporting activities | Presenting the findings within the hospital Disseminating new knowledge on findings and PHR process (publication, conference, regional geriatric working group) |
3. Results
3.1. Part 1: PHR Process
3.1.1. Orientation
3.1.2. Setting-Up
3.1.3. Planning
3.1.4. Data Collection
3.1.5. Analyses
3.2. Part 2: Outcomes
3.2.1. Outcome 1: The Actual State of Caregiver Support
3.2.2. Outcome 2: Needs of the Geriatric Team
3.3. Part 3: Critical Reflection
3.3.1. The PHR Approach
3.3.2. Participation Grades
3.3.3. Benefits and Limitations
3.3.4. Reporting
4. Discussion
Methodological Considerations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Eldercare Workforce Alliance. Family Caregivers: The Backbone of Our Eldercare System. Issue Brief. 2017. Available online: http://eldercareworkforce.org/wp-content/uploads/2018/03/Caregiving_Issue_Brief_Update_FINAL.pdf (accessed on 19 November 2019).
- Rothgang, H.; Müller, R. Pflegereport 2018 (Caregiving report 2018). Schriftenreihe 2018, 12. Available online: https://www.barmer.de/blob/170372/9186b971babc3f80267fc329d65f8e5e/data/dl-pflegereport-komplett.pdf (accessed on 19 November 2019).
- Family Caregivers Alliance. Definitions. 2019. Available online: https://www.caregiver.org/definitions (accessed on 19 November 2019).
- Candy, B.; Jones, L.; Drake, R.; Leurent, B.; King, M. Interventions for supporting informal caregivers of patients in the terminal phase of a disease. Cochrane Database Syst. Rev. 2011. [Google Scholar] [CrossRef] [Green Version]
- German Federal Statistic Office—Statistisches Bundesamt. Pflegestatistik 2017. Pflege im Rahmen der Pflegeversicherung (Caregiving Statistic 2017. Caregiving Based on the Caregiving Insurance) German Results; Destatis: Wiesbaden, Germany, 2018.
- Wetzstein, M.; Rommel, A.; Lange, C. Pflegende Angehörige—Deutschlands größter Pflegedienst (Family caregivers—Germany’s largest nursing service). In Gesundheitsberichterstattung Kompakt; Robert Koch Institut: Berlin, Germany, 2015. [Google Scholar]
- Nowossadeck, S.; Engstler, H.; Klaus, D. Pflege und Unterstützung durch Angehörige (Caring and Support. by Family Caregivers); Report Altersdaten 01/2016; Deutsches Zentrum für Altersfragen: Berlin, Germany, 2016. [Google Scholar]
- Tremont, G. Family caregiving in dementia. Med. Health 2011, 94, 36–38. [Google Scholar]
- Greenwood, N.; Mackenzie, A.; Cloud, G.C.; Wilson, N. Informal primary carers of stroke survivors living at home–challenges, satisfactions and coping: A systematic review of qualitative studies. Disabil. Rehabil. 2009, 31, 337–351. [Google Scholar] [CrossRef]
- German Ministry of Health—Bundesminsterium für Gesundheit. Nationales Gesundheitsziel Gesund Älter werden (National Health Goal Healthy Ageing); Kooperationsverbund gesundheitsziele.de BMG: Berlin, Germany, 2012. [Google Scholar]
- Ekwall, A.K.; Sivberg, B.; Hallberg, I.R. Loneliness as a predictor of quality of life among older caregivers. Issues and innovations in nursing practice. J. Adv. Nurs. 2005, 49, 23–32. [Google Scholar] [CrossRef] [Green Version]
- Pinquart, M.; Sörensen, S. Differences between caregivers and non-caregivers in psychological health and physical health: A meta-analysis. Psychol. Aging 2003, 18, 250–267. [Google Scholar] [CrossRef]
- Adelman, R.; Tmanova, L.; Delgado, D.; Dion, S.; Lachs, M.S. Caregiver Burden. A Clinical Review. JAMA 2014, 311, 1052–1060. [Google Scholar] [CrossRef]
- Fernandes, C.S.; Angelo, M. Family caregivers: What do they need? An integrative review. Rev. Esc. Enferm. USP 2016, 50, 672–678. [Google Scholar] [CrossRef] [Green Version]
- Simonic, A.; Furlan, M.; Ravnjak, T.; Dirkse, D. Caring for caregivers: A right way to do it? Curr. Opin. Support. Palliat Care 2012, 6, 379–385. [Google Scholar] [CrossRef] [PubMed]
- BGM- German Ministry of Health. Präventionsgesetz (prevention law). 2019. Available online: https://www.bundes-gesundheitsministerium.de/service/begriffe-von-a-z/p/praeventionsgesetz.html (accessed on 15 November 2019).
- DAK. DAK-Pflege-Report 2015. So pflegt Deutschland (That is how Germany cares). 2015. Available online: www.dak.de/dak/download/pflegereport-2015-praesentation-1702994.pdf (accessed on 7 November 2019).
- AOK. Pflegekurse (Caregiver Training). 2015. Available online: https://plus.aok.de/fileadministrator/user_upload/AOK-PLUS/05-Content-PDF/Flyer-Pflegekurse.pdf (accessed on 10 November 2019).
- Schmidt, M.; Schneekloth, U. Abschlussbericht zur Studie “Wirkungen des Pflege-Weiterentwicklungsgesetzes”. TNS Intratest Sozialforschung, München. 2011. Available online: https://www.bundesgesundheitsministerium.de/fileadmin/Dateien/Publikationen/Pflege/Berichte/Abschlussbericht_zur_Studie_Wirkungen_des_Pflege-Weiterentwicklungsgesetzes.pdf (accessed on 21 November 2019).
- Küttel, C.; Schäfer-Keller, P.; Brunner, C.; Conca, A.; Schütz, P.; Frei, I.A. Daily routine of informal caregivers-needs and concerns with regard to the discharge of their elderly family members from the hospital setting—A qualitative study. Pflege 2015, 28, 111–121. [Google Scholar] [CrossRef] [PubMed]
- Lüdecke, D.; Mnich, E.; Kofahl, C. The impact of sociodemographic factors on the utilization of support services for family caregivers of elderly dependents—Results from the German sample of the EUROFAMCARE study. Psychosoc. Med. 2012, 9, 1–11. [Google Scholar] [CrossRef]
- Singotani, R.G.; Karapinar, F.; Brouwers, C.; Wagner, C.; De Bruijne, M.C. Towards a patient journey perspective on causes of unplanned readmissions using a classification framework: Results of a systematic review with narrative synthesis. BMC Med. Res. Methodol. 2019, 19, 189. [Google Scholar] [CrossRef]
- Bookman, A.; Harrington, M. Family Caregivers: A Shadow Workforce in the Geriatric Health Care System? J. Health Polit. Policy Law 2007, 32, 684–697. [Google Scholar] [CrossRef] [Green Version]
- Berg-Weger, M.; McGartland Rubio, D.; Tebb, S.S. Living with and Caring for Older Family Members. J. Gerontol. Soc. Work 2000, 33, 47–62. [Google Scholar] [CrossRef]
- Pinquart, M.; Sörensen, S. Correlates of Physical Health of Informal Caregivers: A Meta-Analysis. J. Gerontol. B Psychol. Sci. Soc. Sci. 2007, 62, 126–137. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bom, J.; Bakx, P.; Schut, F.; Van Doorslaer, E. The Impact of Informal Caregiving for Older Adults on the Health of Various Types of Caregivers: A Systematic Review. Gerontologist 2019, 59, e629–e642. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dorant, E.; Krieger, T. Contextual Exploration of a New Family Caregiver Support Concept for Geriatric Settings Using a Participatory Health Research Strategy. Int. J. Environ. Res. Public Health 2017, 14, 1467. [Google Scholar] [CrossRef] [Green Version]
- Spinuzzi, C. The Methodology of Participatory Design. Tech. Commun. 2015, 52, 162–174. [Google Scholar]
- Oetzel, J.; Springett, J.; Wallerstein, N.; Parajon, L.; Sia, I.; Wieland, M.; Reese, A.; Reddy, R. Evaluating participatory Health Research. In Participatory Health Research: Voices from Around the World; Wright, M., Kongast, K., Eds.; Springer: Cham, Switzerland, 2018. [Google Scholar]
- Minkler, M.; Wallerstein, N. Community-Based Participatory Research for Health, 3rd ed.; John Wiley & Sons: New York, NY, USA, 2011. [Google Scholar]
- Cornwall, A.; Jewkes, R. What is participatory research? Soc. Sci. Med. 1995, 41, 1667–1676. [Google Scholar] [CrossRef]
- Ponzoni, E. Windows of understanding: Broadening access to knowledge production through participatory action research. Qual. Res. 2016, 16, 557–574. [Google Scholar] [CrossRef] [Green Version]
- Wright, M. Was ist partizipative Gesundheitsforschung? (What is participatory health research?). Präv. Gesundh. 2013, 8, 122. [Google Scholar] [CrossRef]
- Bush, P.L.; Pluye, P.; Loignon, C.; Granikov, V.; Wright, M.T.; Pelletier, J.; Bartlett-Esquilant, G.; Macaulay, A.C.; Haggerty, J.; Parry, S.; et al. Organizational participatory research: A systematic mixed studies review exposing its extra benefits and the key factors associated with them. Implement. Sci. 2017, 12, 119. [Google Scholar] [CrossRef]
- Greenwood, D.J.; Foote Whyte, W.; Harkavy, I. Participatory Action Research as a Process and as a Goal. Hum. Relat. 1993, 46, 175–192. [Google Scholar] [CrossRef]
- Minkler, M. Ethical challenges for the “outside” researcher in community-based participatory research. Health Educ. Behav. 2004, 31, 684–697. [Google Scholar] [CrossRef]
- Carlson, E.; Nygren, F.; Wennick, A. Critical Friends: Health Professionals’ Experiences of Collegial Feedback in a Clinical Setting. J. Contin. Educ. Health Prof. 2018, 38, 179–183. [Google Scholar] [CrossRef]
- Dahlgren, L.O.; Eriksson, B.E.; Gyllenhammar, H.; Korkeila, M.; Saaf-Rothoff, A.; Wernerson, A.; Seeberger, A. To be and to have a critical friend in medical teaching. Med. Educ. 2006, 40, 72–78. [Google Scholar] [CrossRef]
- Stenhouse, L. An introduction to Curriculum Research and Development; Heinemann: London, UK, 1975. [Google Scholar]
- Salsberg, J.; Macridis, S.; Bengoeche, E.G.; Macaulay, A.C.; Moore, S. The shifting dynamics of social roles and project ownership over the lifecycle of a community based participatory research project. Fam. Pract. 2017, 34, 305–312. [Google Scholar] [CrossRef] [Green Version]
- Bratteteig, T.; Wagner, I. Unpacking the Notion of Participation in Participatory Design. Comput. Supported Coop. Work 2016, 25, 425–475. [Google Scholar] [CrossRef]
- Leask, C.F.; Sandlund, M.; Skelton, D.A.; Altenburg, T.M.; Cardon, G.; Chinapaw, M.J.M.; de Bourdeaudhuij, I.; Verloigne, M.; Chastin, S.F.M. GrandStand, Safe Step and Teenage Girls on the Move Research Groups. Framework, principles and recommendations for utilising participatory methodologies in the co-creation and evaluation of public health interventions. Res. Involv. Engagem. 2019, 5, 2. [Google Scholar] [CrossRef]
- Cornwall, A. Towards participatory practice: Participatory rural appraisal (PRA) and the participatory process. In Participatory Research in Health: Issues and Experiences; De Koning, K., Martin, M., Eds.; Vistaar Publications: New Delhi, India, 1996; p. 96. [Google Scholar]
- Guba, E.; Lincoln, Y. Fourth Generation Evaluation; Sage: Newbury Park, CA, USA, 1989. [Google Scholar]
- Morse, J.M. Critical Analysis of Strategies for Determining Rigor in Qualitative Inquiry. Qual. Health Res. 2015, 25, 1212–1222. [Google Scholar] [CrossRef]
- O’Brien, B.C.; Harris, I.B.; Beckman, T.J.; Reed, D.A.; Cook, D.A. Standards for Reporting Qualitative Research. Acad. Med. 2014, 89, 1245–1251. [Google Scholar] [CrossRef]
- ICPHR—International Collaboration for Participatory Health Research. Position Paper 2: Participatory Health Research: A Guide to Ethical Principals and Practice. Berlin International Collaboration for Participatory Health Research, 2013. Available online: http://www.icphr.org/uploads/2/0/3/9/20399575/ichpr_position_paper_2_ethics_-_version_october_2013.pdf (accessed on 21 November 2019).
- Beauchamp, T.L.; Childress, J.F. Principles of Biomedical Ethics, 3rd ed.; Oxford University Press: New York, NY, USA, 1989. [Google Scholar]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef] [Green Version]
- Nowell, L.S.; Norris, J.M.; White, D.E.; Moules, N.J. Thematic Analysis: Striving to Meet the Trustworthiness Criteria. Int. J. Qual. Methods 2017, 16, 1–13. [Google Scholar] [CrossRef]
- Bauer, M.; Fitzgerald, L.; Haesler, E.; Manfrin, M. Hospital discharge planning for frail older people and their family. Are we delivering best practice? A review of the evidence. J. Clin. Nurs. 2009, 18, 2539–2546. [Google Scholar] [CrossRef]
- Ewing, G.; Grande, G.E. Providing Comprehensive, Person-Centred Assessment and Support for Family Carers Towards the End of Life: 10 Recommendations for Achieving Organisational Change; Hospice: London, UK, 2018. [Google Scholar]
- Røen, I.; Stifoss-Hanssen, H.; Grande GKaasa, S.; Sand, K.; Knudsen, A.K. Supporting carers: Health care professionals in need of system improvements and education—A qualitative study. BMC Palliat. Care 2019, 18, 58. [Google Scholar] [CrossRef]
- Braye, S.; McDonnell, L. Balancing powers: University researchers thinking critically about participatory research with young fathers. Qual. Res. 2012, 13, 265–284. [Google Scholar] [CrossRef]
- Nguyen, T.; Palisano, R.J.; Graham, I. Perspectives and Experiences with Engaging Youth and Families in Research. Phys. Occup. Ther. Pediatrics 2019, 39, 310–323. [Google Scholar] [CrossRef]
- Wallerstein, N.B.; Duran, B. Using community-based participatory research to address health disparities. Health Promot. Pract. 2006, 7, 312–323. [Google Scholar] [CrossRef]
- Smith, L.; Bratini, L.; Chambers, D.A.; Jensen, R.V.; Romero, L. Between idealism and reality: Meeting the challenges of participatory action research. Action Res. 2010, 8, 407–425. [Google Scholar] [CrossRef]
- Schulz, A.J.; Israel, B.A.; Lantz, P. Instrument for evaluating dimensions of group dynamics within community-based participatory research partnerships. Eval. Program. Plan. 2003, 26. [Google Scholar] [CrossRef]
- Bandelow, N.C. Governance im Gesundheitswesen: Systemintegration zwischen Verhandlung und hierarchischer Steuerung. In Governance und Gesellschaftliche Integration; Lange, S., Schimank, U., Eds.; Governance; VS Verlag für Sozialwissenschaften: Wiesbaden, Germany, 2004; Volume 2. [Google Scholar] [CrossRef]

© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Krieger, T.; Specht, R.; Errens, B.; Hagen, U.; Dorant, E. Caring for Family Caregivers of Geriatric Patients: Results of a Participatory Health Research Project on Actual State and Needs of Hospital-Based Care Professionals. Int. J. Environ. Res. Public Health 2020, 17, 5901. https://doi.org/10.3390/ijerph17165901
Krieger T, Specht R, Errens B, Hagen U, Dorant E. Caring for Family Caregivers of Geriatric Patients: Results of a Participatory Health Research Project on Actual State and Needs of Hospital-Based Care Professionals. International Journal of Environmental Research and Public Health. 2020; 17(16):5901. https://doi.org/10.3390/ijerph17165901
Chicago/Turabian StyleKrieger, Theresia, Regina Specht, Babette Errens, Ulrike Hagen, and Elisabeth Dorant. 2020. "Caring for Family Caregivers of Geriatric Patients: Results of a Participatory Health Research Project on Actual State and Needs of Hospital-Based Care Professionals" International Journal of Environmental Research and Public Health 17, no. 16: 5901. https://doi.org/10.3390/ijerph17165901






