Greater Engagement with Health Information Is Associated with Adoption and Maintenance of Healthy Lifestyle Behaviours in People with MS
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Data Collection and Measurement
2.2.1. Demographics
2.2.2. Clinical Variables
2.2.3. Health Communication
2.2.4. Lifestyle Behaviours
2.3. Statistical Analysis
Adoption and Maintenance of Lifestyle Behaviours
3. Results
3.1. Cohort Characteristics
3.2. Cross-Sectional Associations
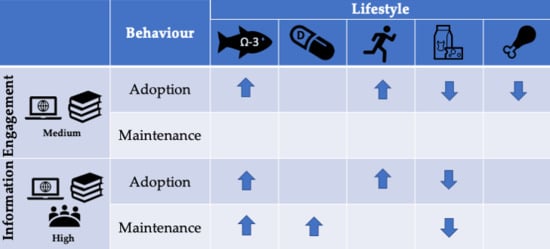
3.3. Adopting Lifestyle Behaviours
3.4. Maintaining Lifestyle Behaviours
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Compston, A.; Coles, A. Multiple sclerosis. Lancet 2008, 372, 1502–1517. [Google Scholar] [CrossRef]
- Ziemssen, T. Multiple sclerosis beyond edss: Depression and fatigue. J. Neurol. Sci. 2009, 277 (Suppl. 1), S37–S41. [Google Scholar] [CrossRef]
- Simmons, R. Life issues in multiple sclerosis. Nat. Rev. Neurosci. 2010, 6, 603–610. [Google Scholar] [CrossRef] [PubMed]
- Waubant, E.; Lucas, R.; Mowry, E.; Graves, J.; Olsson, T.; Alfredsson, L.; Langer-Gould, A. Environmental and genetic risk factors for ms: An integrated review. Ann. Clin. Transl. Neurol. 2019, 6, 1905–1922. [Google Scholar] [CrossRef] [PubMed]
- Olsson, T.; Barcellos, L.F.; Alfredsson, L. Interactions between genetic, lifestyle and environmental risk factors for multiple sclerosis. Nat. Rev. Neurol. 2017, 13, 25–36. [Google Scholar] [CrossRef]
- Yadav, V.; Shinto, L.; Bourdette, D. Complementary and alternative medicine for the treatment of multiple sclerosis. Expert Rev. Clin. Immunol. 2010, 6, 381–395. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Noar, S.M.; Grant Harrington, N.; Van Stee, S.K.; Shemanski Aldrich, R. Tailored health communication to change lifestyle behaviors. Am. J. Lifestyle Med. 2011, 5, 112–122. [Google Scholar] [CrossRef]
- Weymann, N.; Harter, M.; Petrak, F.; Dirmaier, J. Health information, behavior change, and decision support for patients with type 2 diabetes: Development of a tailored, preference-sensitive health communication application. Patient Prefer Adherence 2013, 7, 1091–1099. [Google Scholar] [CrossRef] [Green Version]
- Hadgkiss, E.J.; Jelinek, G.A.; Weiland, T.J.; Rumbold, G.; Mackinlay, C.A.; Gutbrod, S.; Gawler, I. Health-related quality of life outcomes at 1 and 5 years after a residential retreat promoting lifestyle modification for people with multiple sclerosis. Neurol. Sci. 2013, 34, 187–195. [Google Scholar] [CrossRef] [Green Version]
- Taggart, J.; Williams, A.; Dennis, S.; Newall, A.; Shortus, T.; Zwar, N.; Denney-Wilson, E.; Harris, M.F. A systematic review of interventions in primary care to improve health literacy for chronic disease behavioral risk factors. BMC Fam. Pract. 2012, 13, 49. [Google Scholar] [CrossRef] [Green Version]
- Motl, R.W.; Dlugonski, D.; Wójcicki, T.R.; McAuley, E.; Mohr, D.C. Internet intervention for increasing physical activity in persons with multiple sclerosis. Mult. Scler. J. 2011, 17, 116–128. [Google Scholar] [CrossRef] [PubMed]
- Marrie, R.A.; Salter, A.R.; Tyry, T.; Fox, R.J.; Cutter, G.R. Preferred sources of health information in persons with multiple sclerosis: Degree of trust and information sought. J. Med. Internet Res. 2013, 15, e67. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Webb, T.; Joseph, J.; Yardley, L.; Michie, S. Using the internet to promote health behavior change: A systematic review and meta-analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. J. Med. Internet Res. 2010, 12, e4. [Google Scholar] [CrossRef] [Green Version]
- Li, M.P.; Jelinek, G.A.; Weiland, T.J.; Mackinlay, C.A.; Dye, S.; Gawler, I. Effect of a residential retreat promoting lifestyle modifications on health-related quality of life in people with multiple sclerosis. Qual. Prim. Care 2010, 18, 379–389. [Google Scholar] [PubMed]
- Naidoo, D.; Schembri, A.; Cohen, M. The health impact of residential retreats: A systematic review. BMC Complement Med. Ther. 2018, 18, 8. [Google Scholar] [CrossRef]
- Barnard, E.; Brown, C.R.; Weiland, T.J.; Jelinek, G.A.; Marck, C.H. Understanding barriers, enablers, and long-term adherence to a health behavior intervention in people with multiple sclerosis. Disabil. Rehabil. 2020, 42, 822–832. [Google Scholar] [CrossRef]
- Hadgkiss, E.J.; Jelinek, G.A.; Weiland, T.J.; Pereira, N.G.; Marck, C.H.; van der Meer, D.M. Methodology of an international study of people with multiple sclerosis recruited through web 2.0 platforms: Demographics, lifestyle, and disease characteristics. Neurol. Res. Int. 2013, 2013, 580596. [Google Scholar]
- Weiland, T.J.; De Livera, A.M.; Brown, C.R.; Jelinek, G.A.; Aitken, Z.; Simpson Jr, S.L.; Neate, S.L.; Taylor, K.L.; O’Kearney, E.; Bevens, W. Health outcomes and lifestyle in a sample of people with multiple sclerosis (holism): Longitudinal and validation cohorts. Front. Neurol. 2018, 9, 1074. [Google Scholar] [CrossRef]
- Jelinek, G. Overcoming Multiple Sclerosis: The Evidence-Based 7 Step Recovery Program, 2nd ed.; Allen and Unwin: Sydney, Australia, 2016. [Google Scholar]
- Hadgkiss, E.J.; Jelinek, G.A.; Taylor, K.L.; Marck, C.H.; van der Meer, D.M.; Pereira, N.G.; Weiland, T.J. Engagement in a program promoting lifestyle modification is associated with better patient-reported outcomes for people with ms. Neurol. Sci. 2015, 36, 845–852. [Google Scholar] [CrossRef] [Green Version]
- Hohol, M.; Orav, E.; Weiner, H. Disease steps in multiple sclerosis: A simple approach to evaluate disease progression. Neurology 1995, 45, 251–255. [Google Scholar] [CrossRef]
- Hohol, M.; Orav, E.; Weiner, H. Disease steps in multiple sclerosis: A longitudinal study comparing disease steps and edss to evaluate disease progression. Mult. Scler. J. 1999, 5, 349–354. [Google Scholar] [CrossRef] [PubMed]
- Krupp, L.B.; LaRocca, N.G.; Muir-Nash, J.; Steinberg, A.D. The fatigue severity scale. Application to patients with multiple sclerosis and systemic lupus erythematosus. Arch. Neurol. 1989, 46, 1121–1123. [Google Scholar] [CrossRef] [PubMed]
- WHO. Body Mass Index. Available online: Http://www.Euro.Who.Int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi (accessed on 19 April 2018).
- Jelinek, G.A. Overcoming Multiple Sclerosis: An Evidence-Based Guide to Recovery; Allen and Unwin: Sydney, Australia, 2010. [Google Scholar]
- McKellar, S.; Horsley, P.; Chambers, R.; Bauer, J.; Vendersee, P.; Clarke, C.; Callum, H.; Pullen, M. Development of the diet habits questionnaire for use in cardiac rehabilitation. Aust. J. Prim. Health 2008, 14, 43–47. [Google Scholar] [CrossRef]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef] [Green Version]
- Chwastiak, L.; Ehde, D.M.; Gibbons, L.E.; Sullivan, M.; Bowen, J.D.; Kraft, G.H. Depressive symptoms and severity of illness in multiple sclerosis: Epidemiologic study of a large community sample. Am. J. Psychiatry. 2002, 159, 1862–1868. [Google Scholar] [CrossRef]
- Vanner, E.A.; Block, P.; Christodoulou, C.C.; Horowitz, B.P.; Krupp, L.B. Pilot study exploring quality of life and barriers to leisure-time physical activity in persons with moderate to severe multiple sclerosis. Disabil. Health. J. 2008, 1, 58–65. [Google Scholar] [CrossRef]
- Tan-Kristanto, S.; Kiropoulos, L.A. Resilience, self-efficacy, coping styles and depressive and anxiety symptoms in those newly diagnosed with multiple sclerosis. Psychol. Health Med. 2015, 20, 635–645. [Google Scholar] [CrossRef]
- Tulloch, H.; Reida, R.; D’Angeloa, M.S.; Plotnikoff, R.C.; Morrina, L.; Beatona, L.; Papadakisa, S.; Pipe, A. Predicting short and long-term exercise intentions and behaviour in patients with coronary artery disease: A test of protection motivation theory. Psychol. Health 2009, 24, 255–269. [Google Scholar] [CrossRef]
- Smith, M.L.; Lee, S.; Towne, S.D., Jr.; Han, G.; Quinn, C.; Peña-Purcell, N.C.; Ory, M.G. Impact of a behavioral intervention on diet, eating patterns, self-efficacy, and social support. J. Nutr. Educ. Behav. 2020, 52, 180–186. [Google Scholar] [CrossRef]
- Carey, K.B.; Scott-Sheldon, L.A.; Elliott, J.C.; Garey, L.; Carey, M.P. Face-to-face versus computer-delivered alcohol interventions for college drinkers: A meta-analytic review, 1998 to 2010. Clin. Psychol. Rev. 2012, 32, 690–703. [Google Scholar] [CrossRef] [Green Version]
- Järvelä-Reijonen, E.; Karhunen, L.; Sairanen, E.; Muotka, J.; Lindroos, S.; Laitinen, J.; Puttonen, S.; Peuhkuri, K.; Hallikainen, M.; Pihlajamäki, J. The effects of acceptance and commitment therapy on eating behavior and diet delivered through face-to-face contact and a mobile app: A randomized controlled trial. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moss-Morris, R.; McCrone, P.; Yardley, L.; van Kessel, K.; Wills, G.; Dennison, L. A pilot randomised controlled trial of an internet-based cognitive behavioural therapy self-management programme (ms invigor8) for multiple sclerosis fatigue. Behav. Res. Ther. 2012, 50, 415–421. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Motl, R.W.; Hubbard, E.A.; Bollaert, R.E.; Adamson, B.C.; Kinnett-Hopkins, D.; Balto, J.M.; Sommer, S.K.; Pilutti, L.A.; McAuley, E. Randomized controlled trial of an e-learning designed behavioral intervention for increasing physical activity behavior in multiple sclerosis. Mult. Scler. J. Exp. Transl. Clin. 2017, 3, 2055217317734886. [Google Scholar] [CrossRef] [PubMed]
- Casey, B.; Coote, S.; Hayes, S.; Gallagehr, S. Changing physical activity behavior in people with multiple sclerosis: A systematic review and meta-analysis. Arch. Phys. Med. Rehabil. 2018, 99, 2059–2075. [Google Scholar] [CrossRef] [Green Version]
- Learmonth, Y.C.; Adamson, B.C.; Balto, J.M.; Chiu, C.y.; Molina-Guzman, I.; Finlayson, M.; Riskin, B.J.; Motl, R.W. Multiple sclerosis patients need and want information on exercise promotion from healthcare providers: A qualitative study. Health Expect. Int. J. Public Particip. Health Care Health Policy 2017, 20, 574–583. [Google Scholar] [CrossRef]
- Casey, B.; Hayes, S.; Browne, C.; Coote, S. What do people with ms want from a web-based resource to encourage increased physical activity behaviour? Disabil. Rehabil. 2016, 38, 1557–1566. [Google Scholar] [CrossRef]
- Silbermann, E.; Senders, A.; Wooliscroft, L.; Rice, J.; Cameron, M.; Waslo, C.; Orban, A.; Chase, E.; Yadav, V.; Bourdette, D.; et al. Cross-sectional survey of complementary and alternative medicine used in oregon and southwest washington to treat multiple sclerosis: A 17-year update. Mult. Scler. Relat. Disord. 2020, 41, 102041. [Google Scholar] [CrossRef]
- Ng, A.; Kennedy, P.; Hutchinson, B.; Ingram, A.; Vondrell, S.; Goodman, T.; Miller, D. Self-efficacy and health status improve after a wellness program in persons with multiple sclerosis. Disabil. Rehabil. 2013, 35, 1039–1044. [Google Scholar] [CrossRef]
- Marck, C.H.; De Livera, A.M.; Brown, C.R.; Neate, S.L.; Taylor, K.L.; Weiland, T.J.; Hadgkiss, E.J.; Jelinek, G.A. Health outcomes and adherence to a healthy lifestyle after a multimodal intervention in people with multiple sclerosis: Three year follow-up. PLoS ONE 2018, 13, e0197759. [Google Scholar] [CrossRef] [Green Version]
- Kinnett-Hopkins, D.; Adamson, B.; Rougeau, K.; Motl, R. People with ms are less physically active than healthy controls but as active as those with other chronic diseases: An updated meta-analysis. Mult. Scler. Relat. Disord. 2017, 13, 38–43. [Google Scholar] [CrossRef]
- Ploughman, M. Breaking down the barriers to physical activity among people with multiple sclerosis–a narrative review. Phys. Ther. Rev. 2017, 22, 124–132. [Google Scholar] [CrossRef]
- Richardson, E.V.; Barstow, E.A.; Motl, R.W. A narrative exploration of the evolving perception of exercise among people with multiple sclerosis. Qual. Res. Sport. Exerc. Health 2019, 11, 119–137. [Google Scholar] [CrossRef]
- Paul, L.; Coulter, E.H.; Miller, L.; McFadyen, A.; Dorfman, J.; Mattison, P.G.G. Web-based physiotherapy for people moderately affected with multiple sclerosis; quantitative and qualitative data from a randomized, controlled pilot study. Clin. Rehabil. 2014, 28, 924–935. [Google Scholar] [CrossRef] [PubMed]
- Tallner, A.; Pfeifer, K.; Mäurer, M. Web-based interventions in multiple sclerosis: The potential of tele-rehabilitation. Ther. Adv. Neurol. Disord. 2016, 9, 327–335. [Google Scholar] [CrossRef] [Green Version]
- Carvalho, F.A.; Morelhão, P.K.; Franco, M.R.; Maher, C.G.; Smeets, R.J.; Oliveira, C.B.; Júnior, I.F.F.; Pinto, R.Z. Reliability and validity of two multidimensional self-reported physical activity questionnaires in people with chronic low back pain. Musculoskelet. Sci. Pract. 2017, 27, 65–70. [Google Scholar] [CrossRef]
- Brenner, P.S.; DeLamater, J.D. Social desirability bias in self-reports of physical activity: Is an exercise identity the culprit? Soc. Indic. Res. 2014, 117, 489–504. [Google Scholar] [CrossRef]
- Steene-Johannessen, J.; Anderssen, S.A.; Van der Ploeg, H.P.; Hendriksen, I.J.; Donnelly, A.E.; Brage, S.; Ekelund, U. Are self-report measures able to define individuals as physically active or inactive? Med. Sci. Sports Exerc. 2016, 48, 235–244. [Google Scholar] [CrossRef] [Green Version]

| Adoption (Baseline to 5 Year) * | Maintenance (Baseline to 5 Year) * | |||
|---|---|---|---|---|
| Behaviour | Healthy | Unhealthy | Healthy | Unhealthy |
| Reference | No → No | Yes → Yes | Yes → No | No → Yes |
| Outcome | No → Yes | Yes → No | Yes → Yes | No → No |
| Baseline Resource Engagement | |||
|---|---|---|---|
| None | Medium | High | |
| n = 205 | n = 605 | n = 142 | |
| Frequency (percentage) | |||
| Sex | |||
| Male | 24 (11.7%) | 111 (18.3%) | 28 (19.7%) |
| Female | 181 (88.3%) | 494 (81.7%) † | 114 (80.3%) † |
| Education | |||
| No/basic schooling | 48 (23.6%) | 107 (17.8%) | 25 (17.6%) |
| Vocational training | 35 (17.2%) | 78 (13.0%) | 13 (9.2%) |
| University degree | 120 (59.1%) | 416 (69.2%) † | 104 (73.2%) |
| Employment | |||
| Unemployed | 94 (46.1%) | 338 (56.0%) | 58 (41.1%) |
| Paid employment | 47 (23.0%) | 143 (23.7%) | 57 (40.4%) † |
| Retired | 63 (30.9%) | 123 (20.4%) † | 26 (18.4%) |
| Marital status | |||
| Single | 23 (11.5%) | 81 (13.5%) | 13 (9.2%) |
| Married/partnered | 150 (75.0%) | 473 (78.8%) | 120 (85.1%) |
| Separated/divorced/widowed | 27 (13.5%) | 46 (7.7%) † | 8 (5.7%) |
| MS type | |||
| Benign/RRMS | 131 (75.7%) | 435 (81.6%) | 102 (81.0%) |
| SPMS/PPMS/PRMS | 42 (24.3%) | 98 (18.4%) | 24 (19.0%) |
| Disability (PDDS) | |||
| Normal/mild | 80 (45.7%) | 401 (66.3%) | 88 (62.0%) |
| Moderate | 79 (45.1%) | 168 (27.8%) ‡ | 46 (32.4%) † |
| Severe | 16 (9.1%) | 36 (6.0%) | 8 (5.6%) |
| Clinical fatigue (FSS>5) | |||
| No | 43 (27.0%) | 252 (43.8%) | 73 (54.1%) |
| Yes | 116 (73.0%) | 324 (56.3%) ‡ | 62 (45.9%) ‡ |
| BMI category | |||
| Underweight/normal | 96 (46.8%) | 416 (68.8%) | 95 (66.9%) |
| Overweight | 56 (27.3%) | 110 (18.2%) † | 34 (23.9%) |
| Obese | 53 (25.9%) | 79 (13.1%) ‡ | 13 (9.2%) ‡ |
| Mean (SD; range) | |||
| Age | 46.7 (9.7; 20.4–66.2) | 45.1 (10.4; 19.1–70.4) | 48.3 (10.8; 23.2–78.5) |
| Median (interquartile range) | |||
| Duration since onset (years) | 15.4 (8.5–25.4) | 10.4 (5.3–17.4) ‡ | 13.4 (6.5–22.4) |
| PDDS | 3 (1–4) | 1 (0–3) ‡ | 1 (0–3) † |
| Baseline Lifestyle | ||||||
|---|---|---|---|---|---|---|
| No at Baseline | Yes at Baseline | Unadjusted | Adjusted * | |||
| n/N (Percentage) | n/N (Percentage) | PR Est. | (95%CI) | PR Est. | (95%CI) | |
| Taking omega-3 supplement? | ||||||
| Engagement | ||||||
| None | 114/281 (40.6%) | 91/671 (13.6%) | Ref | Ref | ||
| Medium | 146/281 (52.0%) | 459/671 (68.4%) | 1.71 | (1.46, 2.01) | 1.42 | (1.21, 1.66) |
| High | 21/281 (7.5%) | 121/671 (18.0%) | 1.92 | (1.62, 2.27) | 1.56 | (1.32, 1.83) |
| PTREND | < 0.001 | PTREND | < 0.001 | |||
| Taking ≥ 5000 IU/d vitamin D supplement? | ||||||
| Engagement | ||||||
| None | 155/460 (33.7%) | 49/480 (10.2%) | Ref | Ref | ||
| Medium | 275/460 (59.8%) | 322/480 (67.1%) | 2.25 | (1.74, 2.90) | 1.85 | (1.44, 2.37) |
| High | 30/460 (6.5%) | 109/480 (22.7%) | 3.26 | (2.52, 4.23) | 2.70 | (2.09, 3.49) |
| PTREND | < 0.001 | PTREND | < 0.001 | |||
| Seeking sun exposure to raise vitamin D level? | ||||||
| Engagement | ||||||
| None | 86/262 (32.8%) | 86/653 (13.2%) | Ref | Ref | ||
| Medium | 149/262 (56.9%) | 454/653 (69.5%) | 1.51 | (1.29, 1.76) | 1.49 | (1.26, 1.76) |
| High | 27/262 (10.3%) | 113/653 (17.3%) | 1.61 | (1.36, 1.91) | 1.57 | (1.31, 1.89) |
| PTREND | < 0.001 | PTREND | < 0.001 | |||
| Meditating ≥ 10 min/week? | ||||||
| Engagement | ||||||
| None | 147/677 (21.7%) | 22/232 (9.5%) | Ref | Ref | ||
| Medium | 468/677 (69.1%) | 131/232 (56.5%) | 1.68 | (1.11, 2.55) | 1.65 | (1.09, 2.48) |
| High | 62/677 (9.2%) | 79/232 (34.1%) | 4.30 | (2.84, 6.53) | 3.94 | (2.60, 5.97) |
| PTREND | < 0.001 | PTREND | < 0.001 | |||
| Vigorous physical activity ≥ 30 min/d ≥ 3 times/week? | ||||||
| Engagement | ||||||
| None | 166/769 (21.6%) | 39/182 (21.4%) | Ref | Ref | ||
| Medium | 495/769 (64.4%) | 109/182 (59.9%) | 0.95 | (0.68, 1.32) | 0.58 | (0.42, 0.80) |
| High | 108/769 (14.0%) | 34/182 (18.7%) | 1.26 | (0.84, 1.89) | 0.76 | (0.51, 1.14) |
| PTREND | = 0.35 | PTREND | = 0.23 | |||
| Current smoker? | ||||||
| Engagement | ||||||
| None | 149/848 (17.6%) | 28/73 (38.4%) | Ref | Ref | ||
| Medium | 560/848 (66.0%) | 43/73 (58.9%) | 0.45 | (0.29, 0.70) | 0.53 | (0.32, 0.87) |
| High | 139/848 (16.4%) | 2/73 (2.7%) | 0.09 | (0.02, 0.37) | 0.12 | (0.03, 0.54) |
| PTREND | < 0.001 | PTREND | < 0.001 | |||
| Consuming dairy? | ||||||
| Engagement | ||||||
| None | 30/435 (6.9%) | 146/482 (30.3%) | Ref | Ref | ||
| Medium | 287/435 (66.0%) | 313/482 (64.9%) | 0.63 | (0.57, 0.70) | 0.69 | (0.62, 0.78) |
| High | 118/435 (27.1%) | 23/482 (4.8%) | 0.20 | (0.13, 0.29) | 0.20 | (0.13, 0.31) |
| PTREND | < 0.001 | PTREND | < 0.001 | |||
| Consuming meat? | ||||||
| Engagement | ||||||
| None | 19/405 (4.7%) | 158/519 (30.4%) | Ref | Ref | ||
| Medium | 267/405 (65.9%) | 338/519 (65.1%) | 0.63 | (0.57, 0.68) | 0.67 | (0.61, 0.74) |
| High | 119/405 (29.4%) | 23/519 (4.4%) | 0.18 | (0.12, 0.26) | 0.19 | (0.13, 0.28) |
| PTREND | < 0.001 | PTREND | < 0.001 | |||
| Lifestyle Adoption | ||||||
| No at Baseline and 5-yr | No at Baseline; Yes at 5-yr | Unadjusted | Adjusted * | |||
| n/N (Percentage) | n/N (Percentage) | RR Est. | (95%CI) | RR Est. | (95%CI) | |
| Taking omega-3 supplement? | ||||||
| Engagement | ||||||
| None | 80/188 (42.6%) | 34/93 (36.6%) | Ref | Ref | ||
| Medium | 97/188 (51.6%) | 49/93 (52.7%) | 1.13 | (0.78, 1.62) | 1.70 | (1.02, 2.84) |
| High | 11/188 (5.9%) | 10/93 (10.8%) | 1.60 | (0.94, 2.71) | 2.50 | (1.29, 4.85) |
| PTREND | = 0.16 | PTREND | = 0.005 | |||
| Taking ≥ 5000 IU/d vitamin D supplement? | ||||||
| Engagement | ||||||
| None | 86/248 (34.7%) | 66/205 (32.2%) | Ref | Ref | ||
| Medium | 144/248 (58.1%) | 128/205 (62.4%) | 1.08 | (0.87, 1.35) | 1.19 | (0.90, 1.57) |
| High | 18/248 (7.3%) | 11/205 (5.4%) | 0.87 | (0.53, 1.44) | 0.98 | (0.57, 1.67) |
| PTREND | = 0.91 | PTREND | = 0.55 | |||
| Seeking sun exposure to raise vitamin D level? | ||||||
| Engagement | ||||||
| None | 66/187 (35.3%) | 19/70 (27.1%) | Ref | Ref | ||
| Medium | 100/187 (53.5%) | 46/70 (65.7%) | 1.41 | (0.89, 2.24) | 1.19 | (0.73, 1.94) |
| High | 21/187 (11.2%) | 5/70 (7.1%) | 0.86 | (0.36, 2.08) | 1.04 | (0.44, 2.42) |
| PTREND | = 0.62 | PTREND | = 0.67 | |||
| Meditating ≥ 10 min/week? | ||||||
| Engagement | ||||||
| None | 116/529 (21.9%) | 19/93 (20.4%) | Ref | Ref | ||
| Medium | 368/529 (69.6%) | 67/93 (72.0%) | 1.09 | (0.68, 1.75) | 1.14 | (0.69, 1.89) |
| High | 45/529 (8.5%) | 7/93 (7.5%) | 0.96 | (0.43, 2.14) | 1.09 | (0.47, 2.50) |
| PTREND | = 0.93 | PTREND | = 0.72 | |||
| Vigorous physical activity ≥ 30 min/d for ≥ 3 times/week? | ||||||
| Engagement | ||||||
| None | 152/651 (23.3%) | 14/117 (12.0%) | Ref | Ref | ||
| Medium | 412/651 (63.3%) | 83/117 (70.9%) | 1.99 | (1.16, 3.41) | 2.16 | (1.03, 4.55) |
| High | 87/651 (13.4%) | 20/117 (17.1%) | 2.22 | (1.17, 4.20) | 2.71 | (1.22, 6.01) |
| PTREND | = 0.006 | PTREND | = 0.007 | |||
| Lifestyle adoption | ||||||
| Yes at baseline and 5-yr | Yes at baseline; No at 5-yr | Unadjusted | Adjusted * | |||
| n/N (Percentage) | n/N (Percentage) | RR Est. | (95%CI) | RR Est. | (95%CI) | |
| Current smoker? | ||||||
| Engagement | ||||||
| None | 16/38 (42.1%) | 12/35 (34.3%) | Ref | Ref | ||
| Medium | 21/38 (55.3%) | 22/35 (62.9%) | 1.19 | (0.71, 2.01) | 1.46 | (0.83, 2.56) |
| High | 1/38 (2.6%) | 1/35 (2.9%) | 1.17 | (0.27, 5.03) | 2.29 | (0.58, 9.04) |
| PTREND | = 0.52 | PTREND | = 0.14 | |||
| Consuming dairy? | ||||||
| Engagement | ||||||
| None | 135/399 (33.8%) | 10/81 (12.4%) | Ref | Ref | ||
| Medium | 248/399 (62.2%) | 64/81 (79.0%) | 2.97 | (1.57, 5.63) | 3.98 | (1.85, 8.56) |
| High | 16/399 (4.0%) | 7/81 (8.6%) | 4.41 | (1.87, 10.44) | 4.94 | (1.90, 12.88) |
| PTREND | < 0.001 | PTREND | < 0.001 | |||
| Consuming meat? | ||||||
| Engagement | ||||||
| None | 150/453 (33.1%) | 7/64 (10.9%) | Ref | Ref | ||
| Medium | 283/453 (62.5%) | 54/64 (84.4%) | 3.59 | (1.67, 7.72) | 3.42 | (1.47, 7.91) |
| High | 20/453 (4.4%) | 3/64 (4.7%) | 2.93 | (0.81, 10.53) | 3.01 | (0.73, 12.40) |
| PTREND | < 0.001 | PTREND | = 0.002 | |||
| Lifestyle Maintenance | ||||||
| Yes at Baseline; No at 5-yr | Yes at Baseline & 5-yr | Unadjusted | Adjusted * | |||
| n/N (Percentage) | n/N (Percentage) | RR Est. | (95%CI) | RR Est. | (95%CI) | |
| Taking omega-3 supplement? | ||||||
| Engagement | ||||||
| None | 29/178 (16.3%) | 62/493 (12.6%) | Ref | Ref | ||
| Medium | 130/178 (73.0%) | 329/493 (66.7%) | 1.05 | (0.90, 1.22) | 1.08 | (0.92, 1.26) |
| High | 19/178 (10.7%) | 102/493 (20.7%) | 1.24 | (1.05, 1.45) | 1.26 | (1.06, 1.49) |
| PTREND | = 0.003 | PTREND | = 0.003 | |||
| Taking ≥ 5000 IU/d vitamin D supplement? | ||||||
| Engagement | ||||||
| None | 13/99 (13.1%) | 35/372 (9.4%) | Ref | Ref | ||
| Medium | 77/99 (77.8%) | 239/372 (64.2%) | 1.04 | (0.86, 1.25) | 1.05 | (0.86, 1.29) |
| High | 9/99 (9.1%) | 98/372 (26.3%) | 1.26 | (1.05, 1.51) | 1.26 | (1.04, 1.54) |
| PTREND | < 0.001 | PTREND | = 0.001 | |||
| Seeking sun exposure to raise vitamin D level? | ||||||
| Engagement | ||||||
| None | 22/168 (13.1%) | 63/470 (13.4%) | Ref | Ref | ||
| Medium | 121/168 (72.0%) | 323/470 (68.7%) | 0.98 | (0.85, 1.13) | 0.98 | (0.84, 1.13) |
| High | 25/168 (14.9%) | 84/470 (17.9%) | 1.04 | (0.88, 1.22) | 0.99 | (0.83, 1.18) |
| PTREND | = 0.58 | PTREND | = 0.97 | |||
| Meditating ≥ 10 min/week? | ||||||
| Engagement | ||||||
| None | 8/81 (9.9%) | 10/103 (9.7%) | Ref | Ref | ||
| Medium | 47/81 (58.0%) | 52/103 (50.5%) | 0.95 | (0.60, 1.49) | 0.97 | (0.61, 1.55) |
| High | 26/81 (32.1%) | 41/103 (39.8%) | 1.10 | (0.70, 1.74) | 1.10 | (0.69, 1.75) |
| PTREND | = 0.40 | PTREND | = 0.51 | |||
| Vigorous physical activity ≥ 30 min/d for ≥ 3 times/week? | ||||||
| Engagement | ||||||
| None | 18/83 (21.7%) | 21/99 (21.2%) | Ref | Ref | ||
| Medium | 46/83 (55.4%) | 63/99 (63.6%) | 1.08 | (0.78, 1.51) | 0.92 | (0.63, 1.34) |
| High | 19/83 (22.9%) | 15/99 (15.2%) | 0.82 | (0.51, 1.32) | 0.67 | (0.41, 1.10) |
| PTREND | = 0.45 | PTREND | = 0.10 | |||
| Lifestyle maintenance | ||||||
| No at baseline; Yes at 5-yr | No at baseline and 5-yr | Unadjusted | Adjusted * | |||
| n/N (Percentage) | n/N (Percentage) | RR Est. | (95%CI) | RR Est. | (95%CI) | |
| Current smoker? | ||||||
| Engagement | ||||||
| None | 6/16 (37.5%) | 142/831 (17.1%) | Ref | Ref | ||
| Medium | 9/16 (56.3%) | 551/831 (66.3%) | 1.03 | (0.99, 1.06) | 1.02 | (0.99, 1.06) |
| High | 1/16 (6.3%) | 138/831 (16.6%) | 1.03 | (1.00, 1.07) | 1.03 | (0.99, 1.07) |
| PTREND | = 0.062 | PTREND | = 0.13 | |||
| Consuming dairy? | ||||||
| Engagement | ||||||
| None | 13/92 (14.1%) | 17/339 (5.0%) | Ref | Ref | ||
| Medium | 59/92 (64.1%) | 225/339 (66.4%) | 1.40 | (1.02, 1.92) | 1.39 | (0.98, 1.97) |
| High | 20/92 (21.7%) | 97/339 (28.6%) | 1.46 | (1.06, 2.02) | 1.47 | (1.03, 2.10) |
| PTREND | = 0.019 | PTREND | = 0.023 | |||
| Consuming meat? | ||||||
| Engagement | ||||||
| None | 5/75 (6.7%) | 14/328 (4.3%) | Ref | Ref | ||
| Medium | 55/75 (73.3%) | 212/328 (64.6%) | 1.08 | (0.82, 1.42) | 1.04 | (0.79, 1.36) |
| High | 15/75 (20.0%) | 102/328 (31.1%) | 1.18 | (0.90, 1.56) | 1.13 | (0.86, 1.49) |
| PTREND | = 0.039 | PTREND | = 0.076 | |||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, X.; Yu, M.; Jelinek, G.A.; Simpson-Yap, S.; Neate, S.; Nag, N. Greater Engagement with Health Information Is Associated with Adoption and Maintenance of Healthy Lifestyle Behaviours in People with MS. Int. J. Environ. Res. Public Health 2020, 17, 5935. https://doi.org/10.3390/ijerph17165935
Lin X, Yu M, Jelinek GA, Simpson-Yap S, Neate S, Nag N. Greater Engagement with Health Information Is Associated with Adoption and Maintenance of Healthy Lifestyle Behaviours in People with MS. International Journal of Environmental Research and Public Health. 2020; 17(16):5935. https://doi.org/10.3390/ijerph17165935
Chicago/Turabian StyleLin, Xin, Maggie Yu, George A. Jelinek, Steve Simpson-Yap, Sandra Neate, and Nupur Nag. 2020. "Greater Engagement with Health Information Is Associated with Adoption and Maintenance of Healthy Lifestyle Behaviours in People with MS" International Journal of Environmental Research and Public Health 17, no. 16: 5935. https://doi.org/10.3390/ijerph17165935
APA StyleLin, X., Yu, M., Jelinek, G. A., Simpson-Yap, S., Neate, S., & Nag, N. (2020). Greater Engagement with Health Information Is Associated with Adoption and Maintenance of Healthy Lifestyle Behaviours in People with MS. International Journal of Environmental Research and Public Health, 17(16), 5935. https://doi.org/10.3390/ijerph17165935