Performance and Sociodemographic Determinants of Excess Outpatient Demand of Rural Residents in China: A Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Setting
2.2. Data Sources
2.3. Data Processing and Statistical Analysis
2.4. Ethical Approval and Consent to Participate
3. Results
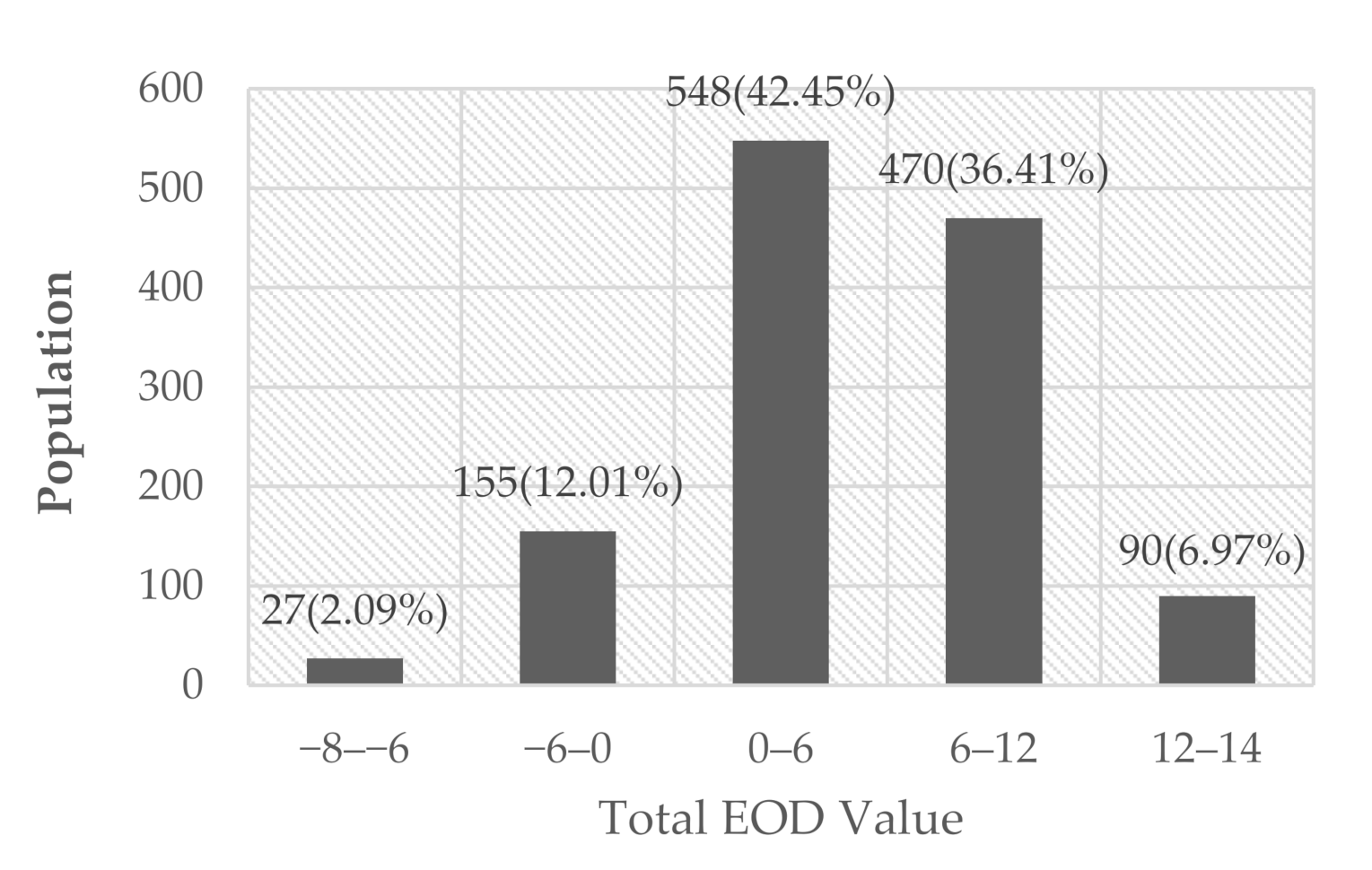
3.1. The Level and Characteristic Distribution of EOD
3.2. Excess Outpatient Demand of Symptoms, Diseases and Overall Situation
3.3. Samples’ Choice of Outpatient Institution in Five Symptoms and Seven Diseases
3.4. Sociodemographic Determinants of EOD according to Multilevel Analyses
4. Discussion
4.1. Excess Outpatient Demand Behavior Was Evident, but with Rare Extreme Conditions in Rural China
4.2. Excess Outpatient Demand Was More Evident When Residents Knew the Exact Disease rather than the Symptoms
4.3. Age, Educational Background and Distance to Hospital Were the Main Sociodemographic Determinants of EOD
4.4. Limitations of This Study
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Availability of Data and Materials
Abbreviations
| EOD | excess outpatient demand, outpatient preference for higher-level institution than reasonably needed |
Appendix A. Full Description of Five Symptoms
| A1 | Sore throat, cold, body temperature of 37.8 °C, swollen throat, perceiving pain when swallowing; |
| A2 | Pain in the middle and upper abdomen that can last for a few days, weeks or even longer; empty stomach pain or midnight pain; |
| A3 | Cough, expectoration and occasional breathing difficulty; cumulative incidence of 3 months annually, extending for 2; |
| A4 | Stomach pain (upper or lower right abdomen), body temperature of 37.8 °C, nausea and vomiting; |
| A5 | Afraid of cold, body temperature of 39 °C, no strength, nausea, vomiting, diarrhea, tenesmus, watery stool with pus or blood in stool after 1–2 days and defecation 10 times per day with a small amount each time. |
References
- Zhang, Y.; Niu, Y.; Zhang, L. Determinants of patient choice for hospital readmission after township hospitalisation: A population-based retrospective study in China. BMJ Open 2018, 8, e021516. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, D.; Lam, T.P.; Lam, K.F.; Zhou, X.D.; Sun, K.S. Challenges to healthcare reform in China: Profit-oriented medical practices, patients’ choice of care and guanxi culture in Zhejiang province. Health Policy Plan 2017, 32, 1241–1247. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lei, S.-H.; Zhang, Y.; Li, H.-M.; Su, D.; Chang, J.-J.; Hu, X.-M.; Ye, Q.; Jiang, D.; Chen, Y.-C. Determinants of inappropriate admissions of children to county hospitals: A cross-sectional study from rural China. BMC Health Serv. Res. 2019, 19, 126. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gertman, P.M.; Restuccia, J.D. The appropriateness evaluation protocol: A technique for assessing unnecessary days of hospital care. Med. Care 1981, 19, 855–871. [Google Scholar] [CrossRef]
- Chen, Y. Rural Excessive Inpatient Services Demand: A Study on Measurement and Management of Inappropriate Admission; Science Press: Beijing, China, 2014. [Google Scholar]
- Henan Provincial Health Commission of the PRC: The Tiered Disease Directory of Township Hospitals in Henan Province. Available online: http://wsjkw.henan.gov.cn/2018/08-29/1278608.html (accessed on 9 June 2020).
- Henan Provincial Health Commission of the PRC: The Tiered Disease Directory of County Hospitals in Henan province. Available online: http://www.henanyz.com/index.gl?op=1&id=18090317072002251 (accessed on 9 June 2020).
- Liu, W.; Yuan, S.; Wei, F.; Yang, J.; Zhu, C.; Yu, Y.; Ma, J. Inappropriate hospital days of a tertiary hospital in Shanghai, China. Int. J. Qual. Health. Care 2017, 29, 699–704. [Google Scholar] [CrossRef] [Green Version]
- Frey, R.; Liu, W.; Yuan, S.; Wei, F.; Yang, J.; Ma, J. Inappropriate admissions of the cardiology and orthopedics departments of a tertiary hospital in Shanghai, China. PLoS ONE 2018, 13, e0208146. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Y.; Chen, Y.; Zhang, X.; Zhang, L. Current level and determinants of inappropriate admissions to township hospitals under the new rural cooperative medical system in China: A cross-sectional study. BMC Health Serv. Res. 2014, 14, 649. [Google Scholar] [CrossRef] [Green Version]
- Chang, J.J.; Chen, Y.C.; Gao, H.X.; Zhang, Y.; Li, H.M.; Su, D.; Jiang, D.; Lei, S.H.; Hu, X.M.; Tan, M.; et al. Effect of inappropriate admissions on hospitalization performance in county hospitals: A cross-sectional study in rural China. Cost Eff. Resour. Alloc. 2019, 17, 8. [Google Scholar] [CrossRef]
- Center For Health Statistics And Information, N. 2019 China Statistics Yearbook of Health and Family Planning; China union medical university Press: Beijing, China, 2019. [Google Scholar]
- Reibling, N.; Wendt, C. Gatekeeping and provider choice in OECD healthcare systems. Curr. Sociol. 2012, 60, 489–505. [Google Scholar] [CrossRef]
- Dourgnon, P.; Naiditch, M. The preferred doctor scheme: A political reading of a French experiment of gate-keeping. Health Policy 2010, 94, 129–134. [Google Scholar] [CrossRef] [Green Version]
- Schlette, S.; Lisac, M.; Blum, K. Integrated primary care in Germany: The road ahead. Int. J. Integr. Care 2009, 9, e14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gerkens, S.; Merkur, S. Belgium: Health system review. Health Syst. Transit. 2010, 12, 1–266. [Google Scholar] [CrossRef]
- Groenewegen, P.P.; Dourgnon, P.; Gress, S.; Jurgutis, A.; Willems, S. Strengthening weak primary care systems: Steps towards stronger primary care in selected Western and Eastern European countries. Health Policy 2013, 113, 170–179. [Google Scholar] [CrossRef] [Green Version]
- Xu, J.; Mills, A. Challenges for gatekeeping: A qualitative systems analysis of a pilot in rural China. Int. J. Equity Health 2017, 16, 106. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kaneko, M.; Motomura, K.; Mori, H.; Ohta, R.; Matsuzawa, H.; Shimabukuro, A.; Matsushima, M. Gatekeeping function of primary care physicians under Japan’s free-access system: A prospective open cohort study involving 14 isolated islands. Fam. Pract. 2019, 36, 452–459. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tavakoli, N.; Kasnaviyeh, M.H.; Yasinzadeh, M.; Amini, M.; Nejad, M. Evaluation of appropriate and inappropriate admission and hospitalization days according to appropriateness evaluation protocol (AEP). Arch. Iran. Med. 2015, 18, 430–434. [Google Scholar]
- Sin, S.; Lee, S.-M.; Lee, J. Characteristics and outcomes of potentially inappropriate admissions to the intensive care unit. Acute Crit. Care 2019, 34, 46–52. [Google Scholar] [CrossRef] [Green Version]
- Mou, E.; Kwang, H.; Hom, J.; Shieh, L.; Kumar, A.; Richman, I.; Berube, C. Magnitude of potentially inappropriate thrombophilia testing in the inpatient hospital setting. J. Hosp. Med. 2017, 12, 735–738. [Google Scholar] [CrossRef] [Green Version]
- Kim, A.M.; Cho, S.; Kim, H.J.; Jung, H.; Jo, M.W.; Lee, J.Y.; Eun, S.J. Primary care patients’ preference for hospitals over clinics in Korea. Int. J. Environ. Res. Public Health 2018, 15, 1119. [Google Scholar] [CrossRef] [Green Version]
- Rao, K.D.; Sheffel, A. Quality of clinical care and bypassing of primary health centers in India. Soc. Sci. Med. 2018, 207, 80–88. [Google Scholar] [CrossRef]
- Ramsay, R.; Baines, M.; Geeranavar, S. International primary care snapshots: New Zealand and Japan. InnovAiT Educ. Inspir. Gen. Pract. 2014, 8, 376–378. [Google Scholar] [CrossRef]
- Velasco Garrido, M.; Zentner, A.; Busse, R. The effects of gatekeeping: A systematic review of the literature. Scand. J. Prim. Health Care 2011, 29, 28–38. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sripa, P.; Hayhoe, B.; Garg, P.; Majeed, A.; Greenfield, G. Impact of GP gatekeeping on quality of care, and health outcomes, use, and expenditure: A systematic review. Br. J. Gen. Pract. 2019, 69, e294–e303. [Google Scholar] [CrossRef]
- Kulu-Glasgow, I.; Delnoij, D.; de Bakker, D. Self-referral in a gatekeeping system:patients’ reasons for skipping the general-practitioner. Health Policy 1998, 45, 221–238. [Google Scholar] [CrossRef] [Green Version]
- Aoki, T.; Yamamoto, Y.; Ikenoue, T.; Kaneko, M.; Kise, M.; Fujinuma, Y.; Fukuhara, S. Effect of patient experience on bypassing a primary care gatekeeper: A multicenter prospective cohort study in Japan. J. Gen. Intern. Med. 2018, 33, 722–728. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tabenkin, H.; Gross, R.; Brammli, S.; Shvartzman, P. Patients’ views of direct access to specialists: An Israeli experience. J. Am. Med Assoc. 1998, 279, 1943–1948. [Google Scholar] [CrossRef]
- Liu, J.J.; Bellamy, G.; Barnet, B.; Weng, S. Bypass of local primary care in rural counties: Effect of patient and community characteristics. Ann. Fam. Med. 2008, 6, 124–130. [Google Scholar] [CrossRef] [Green Version]
- Braun, B.L.; Fowles, J.B.; Forrest, C.B.; Kind, E.A.; Foldes, S.S.; Weiner, J.P. Which enrollees bypass their gatekeepers in a point-of-service plan? Med. Care 2003, 41, 836–841. [Google Scholar] [CrossRef]
- Pillay, I.; Mahomed, O.H. Prevalence and determinants of self referrals to a District-Regional Hospital in KwaZulu Natal, South Africa: A cross sectional study. Pan. Afr. Med. J. 2019, 33, 4. [Google Scholar] [CrossRef]
- Kahabuka, C.; Kvale, G.; Moland, K.M.; Hinderaker, S.G. Why caretakers bypass Primary Health Care facilities for child care—A case from rural Tanzania. BMC Health Serv. Res. 2011, 11, 315. [Google Scholar] [CrossRef] [Green Version]
- Liu, J.; Yin, H.; Zheng, T.; Ilia, B.; Wang, X.; Chen, R.; Hao, Y.; Sun, H.; Jiao, M.; Kang, Z.; et al. Primary health institutions preference by hypertensive patients: Effect of distance, trust and quality of management in the rural Heilongjiang province of China. BMC Health Serv. Res. 2019, 19, 852. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Wang, P.; Kong, X.; Liang, H.; Zhang, X.; Shi, L. Patient satisfaction between primary care providers and hospitals: A cross-sectional survey in Jilin province, China. Int. J. Qual. Health Care 2016, 28, 346–354. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brown, P.H.; Theoharides, C. Health-seeking behavior and hospital choice in China’s New Cooperative Medical System. Health Econ. 2009, 18, S47–S64. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McClain, J.O.; Riedel, D.C. Screening for utilization review: On the use of explicit criteria and non-physicians in case selection. Am. J. Public Health 1973, 63, 247–251. [Google Scholar] [CrossRef] [Green Version]
- Restuccia, J.D. The evolution of hospital utilization review methods in the United States. Int. J. Qual. Health Care 1995, 7, 253–260. [Google Scholar] [CrossRef]
- Payne, S.M. Identifying and managing inappropriate hospital utilization: A policy synthesis. Health Serv. Res. 1987, 22, 709–769. [Google Scholar]
- Morehead, M.A. The medical audit as an operational tool. Am. J. Public Health Nations Health 1967, 57, 1643–1656. [Google Scholar] [CrossRef] [Green Version]
- Payne, B.C. Use of the criteria approach to measurement of effectiveness of hospital utilization. J. Am. Med Assoc. 1966, 196, 1066–1068. [Google Scholar] [CrossRef]
- Forrest, C.B.; Weiner, J.P.; Fowles, J.; Vogeli, C.; Frick, K.D.; Lemke, K.W.; Starfield, B. Self-referral in point-of-service health plans. J. Am. Med Assoc. 2001, 285, 2223–2231. [Google Scholar] [CrossRef] [Green Version]
- Lavis, J.N.; Anderson, G.M. Appropriateness in health care delivery: Definitions, measurement and policy implications. Can. Med. Assoc. J. 1996, 154, 321–328. [Google Scholar] [CrossRef]
- Li, J.; Shi, L.; Liang, H.; Ding, G.; Xu, L. Urban-rural disparities in health care utilization among Chinese adults from 1993 to 2011. BMC Health Serv. Res. 2018, 18, 102. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Song, S.; Yuan, B.; Zhang, L.; Cheng, G.; Zhu, W.; Hou, Z.; He, L.; Ma, X.; Meng, Q. Increased inequalities in health resource and access to health care in rural China. Int. J. Environ. Res. Public Health 2018, 16, 49. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, Z.; Yang, J.; Wu, Y.; Pan, Z.; He, X.; Li, B.; Zhang, L. Challenges for the surgical capacity building of township hospitals among the Central China: A retrospective study. Int. J. Equity Health 2018, 17, 55. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, B.Y.; Zhang, L.; Zhang, Y. Discussion on the appropriate service scope of township hospitals in China. China Health Econ. 2016, 35, 58–60. [Google Scholar] [CrossRef]
- Sun, X.; Meng, H.; Ye, Z.; Conner, K.O.; Duan, Z.; Liu, D. Factors associated with the choice of primary care facilities for initial treatment among rural and urban residents in Southwestern China. PLoS ONE 2019, 14, e0211984. [Google Scholar] [CrossRef]
- Yadong, N.; Liang, Z.; Ting, Y.; Yan, Y.; Yan, Z. Can unsuccessful treatment in primary medical institutions influence patients’ choice? A retrospective cluster sample study from China. BMJ Open 2019, 9, e022304. [Google Scholar] [CrossRef] [Green Version]
- Hu, J.W.; Yin, W.Q.; Zhao, Y.K.; Guo, H.W.; Hu, S.L.; Sun, K. Analysis of residents’ willingness to hierarchical medical system and their intention of first visit hospitals. Chin. J. Hosp. Manag. 2017, 33, 404–407. [Google Scholar] [CrossRef]
- Yu, W.; Li, M.; Ye, F.; Xue, C.; Zhang, L. Patient preference and choice of healthcare providers in Shanghai, China: A cross-sectional study. BMJ Open 2017, 7, e016418. [Google Scholar] [CrossRef] [Green Version]
- Dong, X.; Liu, L.; Cao, S.; Yang, H.; Song, F.; Yang, C.; Xie, J. Focus on vulnerable populationsand promoting equityin health service utilization—Ananalysis of visitor characteristics and service utilization of the Chinese community health service. BMC Public Health 2014, 14, 503. [Google Scholar] [CrossRef] [Green Version]
- Zhang, L.; Wang, Z.; Qian, D.; Ni, J. Effects of changes in health insurance reimbursement level on outpatient service utilization of rural diabetics: Evidence from Jiangsu Province, China. BMC Health Serv. Res. 2014, 14, 185. [Google Scholar] [CrossRef] [Green Version]
- Wang, H.H.; Wang, J.J.; Wong, S.Y.; Wong, M.C.; Li, F.J.; Wang, P.X.; Mercer, S.W. Epidemiology of multimorbidity in China and implications for the healthcare system: Cross-sectional survey among 162,464 community household residents in southern China. BMC Med. 2014, 12, 188. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Chen, L.W.; Mueller, K.; Yu, Q.; Liu, J.; Lin, G. Tracking the effectiveness of health care reform in China: A case study of community health centers in a district of Beijing. Health Policy 2011, 100, 181–188. [Google Scholar] [CrossRef] [PubMed]

| Sociodemographic Factors | n (%) | Total EOD Value | t/F |
|---|---|---|---|
| All | 1290 (100) | 5.69 ± 4.97 | |
| County | |||
| Dingyuan | 256 (19.84) | 6.29 ± 4.27 | 32.277 ** |
| Xixian | 306 (23.72) | 3.39 ± 5.26 | |
| Xialu | 222 (17.22) | 7.00 ± 3.70 | |
| Renxian | 506 (39.22) | 6.21 ± 5.18 | |
| Sex | |||
| Male | 587 (45.50) | 5.57 ± 4.81 | 0.640 |
| Female | 703 (54.50) | 5.79 ± 5.11 | |
| Age 1 | |||
| 18–39 | 296 (22.95) | 7.38 ± 4.46 | 23.962 * |
| 40–59 | 542 (42.02) | 5.38 ± 5.01 | |
| ≥60 | 452 (35.04) | 4.95 ± 5.00 | |
| Education | |||
| Lower than PS 2 | 590 (45.74) | 4.39 ± 5.05 | 34.465 * |
| JHS 3 | 392 (30.39) | 6.10 ± 4.67 | |
| SHS 4 | 226 (17.52) | 7.26 ± 4.48 | |
| Above College | 82 (6.36) | 8.74 ± 4.30 | |
| Marital status | |||
| Married | 1166 (90.39) | 5.61 ± 4.97 | 8.572 * |
| Unmarried | 59 (4.57) | 8.17 ± 3.78 | |
| Divorced/widowed | 65 (5.04) | 4.82 ± 5.40 | |
| Economic burden | |||
| Severe | 88 (6.82) | 4.83 ± 4.48 | 1.467 |
| Moderate | 372 (28.84) | 5.68 ± 4.83 | |
| Not at all | 830 (64.34) | 5.78 ± 5.08 | |
| Time difference (min) 5 | |||
| <0 | 142 (11.01) | 8.49 ± 5.12 | 24.939 * |
| 0–15 | 267 (20.70) | 6.26 ± 4.57 | |
| 16–30 | 392 (30.39) | 5.62 ± 4.59 | |
| >30 | 489 (37.91) | 4.63 ± 5.09 |
| Total | Symptoms | Diseases | ||||
|---|---|---|---|---|---|---|
| EOD Value | EOD Risk (%) | EOD Value | EOD Risk (%) | EOD Value | EOD Risk (%) | |
| Mean ± SD | 5.69 ± 4.97 | 51.17 ± 22.20 | 1.69 ± 2.96 | 42.84 ± 30.59 | 4.00 ± 3.32 | 57.01 ± 24.56 |
| Min − Max | −8–24 | 0–100 | −3–12 | 0–100 | −5–17 | 0–100 |
| Median | 6 | 50 | 2 | 40 | 5 | 71 |
| Symptoms 1/Diseases | Village Clinics | Township Hospitals | County Hospitals | EOD Value |
|---|---|---|---|---|
| A1 Swollen and sore throat | 721 (55.89) | 466 (36.12) | 103 (7.98) | 0.52 ± 0.64 |
| A2 Long-time upper abdominal pain | 533 (41.32) | 418 (32.40) | 339 (26.28) | −0.14 ± 0.82 |
| A3 Cough extending for 2 years | 492 (38.14) | 339 (26.28) | 459 (35.58) | 0.99 ± 0.88 |
| A4 Pain in the lower right abdomen | 579 (44.88) | 488 (37.83) | 223 (17.29) | −0.27 ± 0.75 |
| A5 Diarrhea, watery and blood in stool | 168 (13.02) | 288 (22.33) | 834 (64.65) | 0.60 ± 0.81 |
| B1 Childbirth | 1 (0.08) | 110 (8.53) | 1179 (91.39) | 1.08 ± 0.52 |
| B2 Mild pneumonia in adults | 241 (18.68) | 389 (30.16) | 660 (51.16) | 0.39 ± 0.87 |
| B3 Baby pneumonia | 102 (7.91) | 209 (16.20) | 979 (75.89) | −0.21 ± 0.75 |
| B4 Disc herniation | 121 (9.38) | 369 (28.60) | 800 (62.02) | 0.67 ± 0.86 |
| B5 Acute appendicitis | 39 (3.02) | 286 (22.17) | 965 (74.81) | 0.83 ± 0.67 |
| B6 Pesticide poisoning | 75 (5.81) | 364 (28.22) | 851 (65.97) | 0.73 ± 0.79 |
| B7 Tonsil inflammation | 710 (55.04) | 496 (38.45) | 84 (6.51) | 0.52 ± 0.62 |
| Sociodemographic Determinants | Coef. | p | 95% CI | OR |
|---|---|---|---|---|
| Fixed part: | ||||
| Intercept | 18.130 | <0.001 | 16.209, 20.052 | 74,775,436.5 |
| Sex | ||||
| Male | Ref. | |||
| Female | 0.219 | 0.163 | −0.089, 0.528 | 1.245 |
| Age 1 | ||||
| 18–39 | Ref. | |||
| 40–59 | −0.489 | 0.027 | −0.923, −0.054 | 0.613 |
| ≥60 | −0.715 | 0.005 ** | −1.212, −0.217 | 0.489 |
| Education | ||||
| Lower than PS 2 | Ref. | |||
| JHS 3 | 0.423 | 0.035 | 0.030, 0.815 | 1.527 |
| SHS 4 | 0.686 | 0.007 ** | 0.189, 1.183 | 1.986 |
| Above college | 1.183 | 0.001 * | 0.461, 1.906 | 0.489 |
| Marital status | ||||
| Married | Ref. | |||
| Unmarried | 0.632 | 0.105 | −0.133, 1.396 | 1.881 |
| Divorced/widowed | 0.251 | 0.486 | −0.456, 0.959 | 1.285 |
| Economic burden | ||||
| Severe | Ref. | |||
| Moderate | 0.357 | 0.272 | −0.280, 0.994 | 1.429 |
| Not at all | 0.412 | 0.181 | −0.192, 1.016 | 1.510 |
| Time difference (min) 5 | ||||
| <0 | Ref. | |||
| 0–15 | −0.678 | 0.018 | −1.238, −0.117 | 0.508 |
| 16–30 | −0.775 | 0.004 ** | −1.309, −0.243 | 0.461 |
| >30 | −1.351 | <0.001 * | −1.877, −0.826 | 0.259 |
| Random-effect Parameters: | ||||
| Township | – | – | 6.477, 19.086 | – |
| Residual | – | – | 19.324, 20.879 | – |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, Y.; Chen, Y.; Cheng, X.; Zhang, Y. Performance and Sociodemographic Determinants of Excess Outpatient Demand of Rural Residents in China: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2020, 17, 5963. https://doi.org/10.3390/ijerph17165963
Liu Y, Chen Y, Cheng X, Zhang Y. Performance and Sociodemographic Determinants of Excess Outpatient Demand of Rural Residents in China: A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2020; 17(16):5963. https://doi.org/10.3390/ijerph17165963
Chicago/Turabian StyleLiu, Yanchen, Yingchun Chen, Xueyan Cheng, and Yan Zhang. 2020. "Performance and Sociodemographic Determinants of Excess Outpatient Demand of Rural Residents in China: A Cross-Sectional Study" International Journal of Environmental Research and Public Health 17, no. 16: 5963. https://doi.org/10.3390/ijerph17165963
APA StyleLiu, Y., Chen, Y., Cheng, X., & Zhang, Y. (2020). Performance and Sociodemographic Determinants of Excess Outpatient Demand of Rural Residents in China: A Cross-Sectional Study. International Journal of Environmental Research and Public Health, 17(16), 5963. https://doi.org/10.3390/ijerph17165963





