The Interactive Effects between Particulate Matter and Heat Waves on Circulatory Mortality in Fuzhou, China
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Statistical Analysis
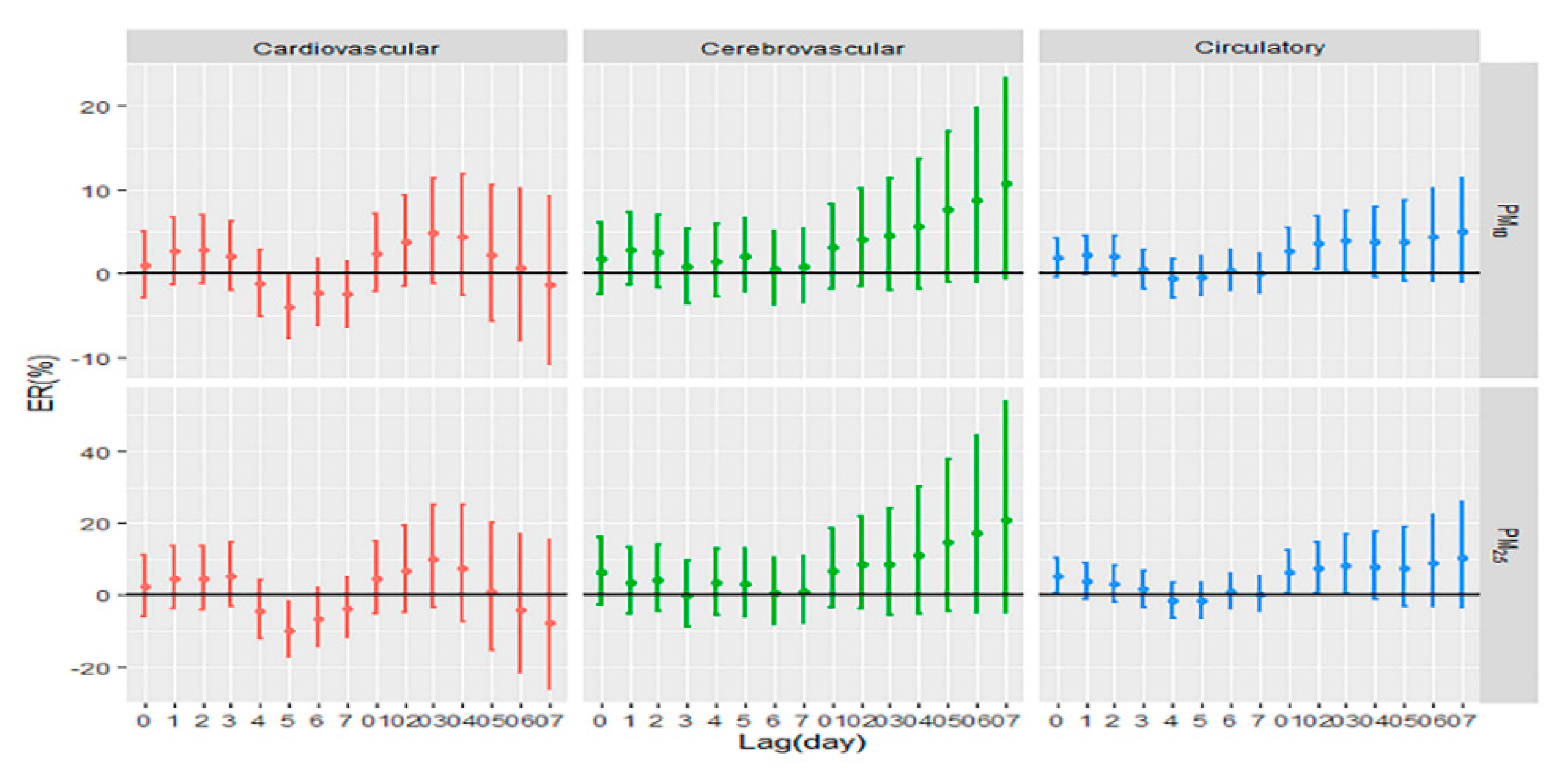
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Kinney, P.L. Interactions of climate change, air pollution, and human health. Curr. Environ. Health Rep. 2018, 5, 179–186. [Google Scholar] [CrossRef] [PubMed]
- Lelieveld, J.; Evans, J.S.; Fnais, M.; Giannadaki, D.; Pozzer, A. The contribution of outdoor air pollution sources to premature mortality on a global scale. Nature 2015, 525, 367–371. [Google Scholar] [CrossRef] [PubMed]
- Bind, M.A.; Peters, A.; Koutrakis, P.; Coull, B.; Vokonas, P.; Schwartz, J. Quantile regression analysis of the distributional effects of air pollution on blood pressure, heart rate variability, blood lipids, and biomarkers of inflammation in elderly American men: The normative aging study. Environ. Health Perspect. 2016, 124, 1189–1198. [Google Scholar] [CrossRef] [PubMed]
- Bouchama, A. The 2003 European heat wave. Intensiv. Care Med. 2004, 30, 1–3. [Google Scholar] [CrossRef]
- Watts, N.; Adger, W.N.; Agnolucci, P.; Blackstock, J.; Byass, P.; Cai, W.; Chaytor, S.; Colbourn, T.; Collins, M.; Cooper, A.; et al. Health and climate change: Policy responses to protect public health. Lancet 2015, 386, 1861–1914. [Google Scholar] [CrossRef]
- IPCC. Annex I Glossary. In Global Warming of 1.5 °C. An IPCC Special Report; Matthews, R., Babiker, M., Coninck, H.D., Weyer, N.M., Eds.; World Meteorological Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Gasparrini, A.; Guo, Y.; Hashizume, M.; Kinney, P.L.; Petkova, E.P.; Lavigne, E.; Zanobetti, A.; Schwartz, J.D.; Tobias, A.; Leone, M.; et al. Temporal variation in heat-mortality associations: A multicountry study. Environ. Health Perspect. 2015, 123, 1200–1207. [Google Scholar] [CrossRef]
- Li, J.; Xu, X.; Yang, J.; Liu, Z.; Xu, L.; Gao, J.; Liu, X.; Wu, H.; Wang, J.; Yu, J.; et al. Ambient high temperature and mortality in Jinan, China: A study of heat thresholds and vulnerable populations. Environ. Res. 2017, 156, 657–664. [Google Scholar] [CrossRef]
- Hamanaka, R.B.; Mutlu, G.M. Particulate matter air pollution: Effects on the cardiovascular system. Front. Endocrinol. 2018, 9, 680. [Google Scholar] [CrossRef]
- Qin, R.X.; Xiao, C.; Zhu, Y.; Li, J.; Yang, J.; Gu, S.; Xia, J.; Su, B.; Liu, Q.; Woodward, A. The interactive effects between high temperature and air pollution on mortality: A time-series analysis in Hefei, China. Sci. Total Environ. 2017, 575, 1530–1537. [Google Scholar] [CrossRef]
- Zanobetti, A.; Peters, A. Disentangling interactions between atmospheric pollution and weather. J. Epidemiol. Commun. Health 2015, 69, 613–615. [Google Scholar] [CrossRef]
- Parry, M.; Green, D.; Zhang, Y.; Hayen, A. Does particulate matter modify the short-term association between heat waves and hospital admissions for cardiovascular diseases in greater Sydney, Australia? Int. J. Environ. Res. Public Health 2019, 16, 3270. [Google Scholar] [CrossRef]
- Li, G.; Zhou, M.; Cai, Y.; Zhang, Y.; Pan, X. Does temperature enhance acute mortality effects of ambient particle pollution in Tianjin City, China. Sci Total Environ. 2011, 409, 1811–1817. [Google Scholar] [CrossRef] [PubMed]
- Li, G.; Jiang, L.; Zhang, Y.; Cai, Y.; Pan, X.; Zhou, M. The impact of ambient particle pollution during extreme-temperature days in Guangzhou City, China. Asia Pac. J. Public Health 2014, 26, 614–621. [Google Scholar] [CrossRef]
- Breitner, S.; Wolf, K.; Devlin, R.B.; Diaz-Sanchez, D.; Peters, A.; Schneider, A. Short-term effects of air temperature on mortality and effect modification by air pollution in three cities of Bavaria, Germany: A time-series analysis. Sci. Total Environ. 2014, 485, 49–61. [Google Scholar] [CrossRef] [PubMed]
- Tian, L.; Liang, F.; Guo, Q.; Chen, S.; Xiao, S.; Wu, Z.; Jin, X.; Pan, X. The effects of interaction between particulate matter and temperature on mortality in Beijing, China. Environ. Sci. Process. Impacts 2018, 20, 395–405. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Moran, A.E.; Coxson, P.G.; Yang, X.; Liu, F.; Cao, J.; Chen, K.; Wang, M.; He, J.; Goldman, L.; et al. Potential cardiovascular and total mortality benefits of air pollution control in urban China. Circulation 2017, 136, 1575–1584. [Google Scholar] [CrossRef] [PubMed]
- Crouse, D.L.; Peters, P.A.; van Donkelaar, A.; Goldberg, M.S.; Villeneuve, P.J.; Brion, O.; Khan, S.; Atari, D.O.; Jerrett, M.; Pope, C.A.; et al. Risk of nonaccidental and cardiovascular mortality in relation to long-term exposure to low concentrations of fine particulate matter: A Canadian national-level cohort study. Environ. Health Perspect. 2012, 120, 708–714. [Google Scholar] [CrossRef]
- Kan, H.; Chen, R.; Tong, S. Ambient air pollution, climate change, and population health in China. Environ. Int. 2012, 42, 10–19. [Google Scholar] [CrossRef]
- Zhang, S.; Li, G.; Tian, L.; Guo, Q.; Pan, X. Short-term exposure to air pollution and morbidity of COPD and asthma in East Asian area: A systematic review and meta-analysis. Environ. Res. 2016, 148, 15–23. [Google Scholar] [CrossRef]
- Zhan, D.; Kwan, M.-P.; Zhang, W.; Yu, X.; Meng, B.; Liu, Q. The driving factors of air quality index in China. J. Clean. Prod. 2018, 197, 1342–1351. [Google Scholar] [CrossRef]
- Bao, J.; Yang, X.; Zhao, Z.; Wang, Z.; Yu, C.; Li, X. The spatial-temporal characteristics of air pollution in China from 2001–2014. Int. J. Environ. Res. Public Health 2015, 12, 15875–15887. [Google Scholar] [CrossRef] [PubMed]
- Zeger, S.; Irizarry, R.; Peng, R. On time series analysis of public health and biomedical data. Ann. Rev. Public Health 2006, 27, 57–79. [Google Scholar] [CrossRef]
- Bell, M.L.; Samet, J.M.; Dominici, F. Time-series studies of particulate matter. Ann. Rev. Public Health 2004, 25, 247–280. [Google Scholar] [CrossRef]
- Peng, R.D.; Bobb, J.F.; Tebaldi, C.; McDaniel, L.; Bell, M.L.; Dominici, F. Toward a quantitative estimate of future heat wave mortality under global climate change. Environ. Health Perspect. 2011, 119, 701–706. [Google Scholar] [CrossRef]
- China Meteorological Administration. No Universal Definition of Heatwave. Available online: http://www.cma.gov.cn/2011xzt/kpbd/heatwave/2018050902/201807/t20180709_472858.html (accessed on 8 August 2018).
- Wu, Y.; Wang, X.; Wu, J.; Wang, R.; Yang, S. Performance of heat-health warning systems in Shanghai evaluated by using local heat-related illness data. Sci. Total Environ. 2020, 715, 136883. [Google Scholar] [CrossRef] [PubMed]
- Duan, Y.; Liao, Y.; Li, H.; Yan, S.; Zhao, Z.; Yu, S.; Fu, Y.; Wang, Z.; Yin, P.; Cheng, J.; et al. Effect of changes in season and temperature on cardiovascular mortality associated with nitrogen dioxide air pollution in Shenzhen, China. Sci. Total Environ. 2019, 697, 134051. [Google Scholar] [CrossRef] [PubMed]
- Gasparrini, A.; Armstrong, B.; Kenward, M.G. Distributed lag non-linear models. Stat. Med. 2010, 29, 2224–2234. [Google Scholar] [CrossRef] [PubMed]
- Hondula, D.M.; Georgescu, M.; Balling, R.C., Jr. Challenges associated with projecting urbanization-induced heat-related mortality. Sci. Total Environ. 2014, 490, 538–544. [Google Scholar] [CrossRef]
- Roberts, S. Interactions between particulate air pollution and temperature in air pollution mortality time series studies. Environ. Res. 2004, 96, 328–337. [Google Scholar] [CrossRef]
- Ren, C.; Williams, G.M.; Tong, S. Does particulate matter modify the association between temperature and cardiorespiratory diseases? Environ. Health Perspect. 2006, 114, 1690–1696. [Google Scholar] [CrossRef]
- Qian, Z.; He, Q.; Lin, H.M.; Kong, L.; Bentley, C.M.; Liu, W.; Zhou, D. High temperatures enhanced acute mortality effects of ambient particle pollution in the “oven” city of Wuhan, China. Environ. Health Perspect. 2008, 116, 1172–1178. [Google Scholar] [CrossRef] [PubMed]
- Stafoggia, M.; Schwartz, J.; Forastiere, F.; Perucci, C.A. Does temperature modify the association between air pollution and mortality? A multicity case-crossover analysis in Italy. Am. J. Epidemiol. 2008, 167, 1476–1485. [Google Scholar] [CrossRef] [PubMed]
- Gordon, C.J. Role of environmental stress in the physiological response to chemical toxicants. Environ. Res. 2003, 92, 1–7. [Google Scholar] [CrossRef]
- Cheng, Y.; Kan, H. Effect of the interaction between outdoor air pollution and extreme temperature on daily mortality in Shanghai, China. J. Epidemiol. 2012, 22, 28–36. [Google Scholar] [CrossRef]
- Guo, Y.; Gasparrini, A.; Armstrong, B.; Li, S.; Tawatsupa, B.; Tobias, A.; Lavigne, E.; de Sousa Zanotti Stagliorio Coelho, M.; Leone, M.; Pan, X.; et al. Global variation in the effects of ambient temperature on mortality: A systematic evaluation. Epidemiology 2014, 25, 781–789. [Google Scholar] [CrossRef]
- Karagulian, F.; Belis, C.A.; Dora, C.F.C.; Pruess-Ustuen, A.M.; Bonjour, S.; Adair-Rohani, H.; Amann, M. Contributions to cities’ ambient particulate matter (PM): A systematic review of local source contributions at global level. Atmos. Environ. 2015, 120, 475–483. [Google Scholar] [CrossRef]
- By, N.M.; Peterson, K.; Alston, L.; Allender, S. Australian Heart Disease Statistics 2014. Sexual Health 2014. Available online: https://www.heartfoundation.org.au/search/ (accessed on 10 August 2018).
- Guo, Y.; Gasparrini, A.; Armstrong, B.G.; Tawatsupa, B.; Tobias, A.; Lavigne, E.; Coelho, M.; Pan, X.; Kim, H.; Hashizume, M.; et al. Heat wave and mortality: A multicountry, multicommunity study. Environ. Health Perspect. 2017, 125, 087006. [Google Scholar] [CrossRef]
- Mercer, J.B. Cold—An underrated risk factor for health. Environ. Res. 2003, 92, 8–13. [Google Scholar] [CrossRef]
- Basu, R.; Dominici, F.; Samet, J.M. Temperature and mortality among the elderly in the United States: A comparison of epidemiologic methods. Epidemiology 2005, 16, 58–66. [Google Scholar] [CrossRef]
- Sacks, J.D.; Stanek, L.W.; Luben, T.J.; Johns, D.O.; Buckley, B.J.; Brown, J.S.; Ross, M. Particulate matter-induced health effects: Who is susceptible? Environ. Health Perspect. 2011, 119, 446–454. [Google Scholar] [CrossRef]
- McGeehin, M.A.; Mirabelli, M. The potential impacts of climate variability and change on temperature-related morbidity and mortality in the United States. Environ. Health Perspect. 2001, 109, 185–189. [Google Scholar] [CrossRef] [PubMed]
- Medina-Ramón, M.; Zanobetti, A.; Cavanagh, D.P.; Schwartz, J. Extreme temperatures and mortality: Assessing effect modification by personal characteristics and specific cause of death in a multi-city case-only analysis. Environ. Health Perspect. 2006, 114, 1331–1336. [Google Scholar] [CrossRef] [PubMed]
- Ma, Y.; Zhao, Y.; Yang, S.; Zhou, J.; Xin, J.; Wang, S.; Yang, D. Short-term effects of ambient air pollution on emergency room admissions due to cardiovascular causes in Beijing, China. Environ. Pollut 2017, 230, 974–980. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; Chen, K.; Chen, X.; Jing, Y.; Ma, Z.; Bi, J.; Kinney, P.L. Heat and mortality for ischemic and hemorrhagic stroke in 12 cities of Jiangsu Province, China. Sci. Total Environ. 2017, 601, 271–277. [Google Scholar] [CrossRef]
- Analitis, A.; Michelozzi, P.; D’Ippoliti, D.; De’Donato, F.; Menne, B.; Matthies, F.; Atkinson, R.W.; Iñiguez, C.; Basagaña, X.; Schneider, A.; et al. Effects of heat waves on mortality: Effect modification and confounding by air pollutants. Epidemiology 2014, 25, 15–22. [Google Scholar] [CrossRef]
- Ren, C.; O’Neill, M.S.; Park, S.K.; Sparrow, D.; Vokonas, P.; Schwartz, J. Ambient temperature, air pollution, and heart rate variability in an aging population. Am. J. Epidemiol. 2011, 173, 1013–1021. [Google Scholar] [CrossRef]
- Crandall, C.G.; González-Alonso, J. Cardiovascular function in the heat-stressed human. Acta Physiol. 2010, 199, 407–423. [Google Scholar] [CrossRef]
- Zeger, S.L.; Thomas, D.; Dominici, F.; Samet, J.M.; Schwartz, J.; Dockery, D.; Cohen, A. Exposure measurement error in time-series studies of air pollution: Concepts and consequences. Environ. Health Perspect. 2000, 108, 419–426. [Google Scholar] [CrossRef]
- Fang, X.; Li, R.; Kan, H.; Bottai, M.; Fang, F.; Cao, Y. Bayesian model averaging method for evaluating associations between air pollution and respiratory mortality: A time-series study. BMJ Open 2016, 6, e011487. [Google Scholar] [CrossRef]
| Heat Waves | Non-Heat Waves | |
|---|---|---|
| Days | 339 | 397 |
| Deaths (number of cases) | ||
| Circulatory diseases | 10.26 ± 3.37 | 10.27 ± 3.47 |
| Cardiovascular diseases | 3.89 ± 2.24 | 3.66 ± 1.95 |
| Cerebrovascular diseases | 3.02 ± 1.78 | 3.22 ± 1.77 |
| Pollutants (ug/m3) | ||
| PM10 | 56.06 ± 19.23 | 51.72 ± 24.25 |
| PM2.5 | 21.69 ± 8.94 | 20.86 ± 9.63 |
| Meteorological factors | ||
| Daily maximum temperature (°C) | 35.11 ± 1.58 | 28.75 ± 3.25 |
| Mean pressure (hPa) | 1002.06 ± 4.35 | 1006.57 ± 6.02 |
| Mean relative humidity (%) | 69.75 ± 6.84 | 74.12 ± 12.05 |
| PM2.5 | PM10 | |||
|---|---|---|---|---|
| Heat Wave Days | Non-Heat Wave Days | Heat Wave Days | Non-Heat Wave Days | |
| Circulatory | 8.21 * | 4.24 | 3.84 * | 1.29 |
| (0.32, 16.72) | (−3.29, 12.37) | (0.28, 7.54) | (−1.98, 4.66) | |
| Cardiovascular | 9.89 | 1.36 | 4.90 | 1.11 |
| (−3.56, 25.22) | (−10.08, 14.26) | (−1.19, 11.37) | (−4.09, 6.60) | |
| Cerebrovascular | 8.29 | 2.19 | 4.49 | 1.63 |
| (−5.58, 24.20) | (−9.57, 15.48) | (−1.95, 11.35) | (−3.75, 7.31) | |
| Low PM2.5 | High PM2.5 | Low PM10 | High PM10 | ||
|---|---|---|---|---|---|
| Heat wave days | Total days | 155 | 184 | 146 | 193 |
| Circulatory | 16.68 | 13.09 | 3.74 | 0.96 | |
| (−23.59, 78.16) | (−7.16, 37.76) | (−20.01, 34.52) | (−8.21, 11.04) | ||
| Cardiovascular | −32.95 | 48.35 * | −23.6 | 14.73 | |
| (−68.97, 44.86) | (6.37, 106.89) | (−51.23, 19.68) | (−2.97, 35.66) | ||
| Cerebrovascular | 53.54 | 9.4 | 52.85 | −5.83 | |
| (−27.66, 225.87) | (−23.41, 56.25) | (−3.79, 142.85) | (−20.72, 11.85) | ||
| Non-heat wave days | Total days | 207 | 190 | 221 | 176 |
| Circulatory | −14.55 | 3.59 | −4.51 | −3.31 | |
| (−38.60, 18.91) | (−12.54, 22.69) | (−14.93, 7.19) | (−12.32, 6.63) | ||
| Cardiovascular | −36.24 | −12.84 | −6.44 | −0.68 | |
| (−62.69, 8.97) | (−32.81, 13.08) | (−22.90, 13.55) | (−15.07, 16.14) | ||
| Cerebrovascular | 3.58 | 29.94 | −6.25 | 12.79 | |
| (−38.73, 75.11) | (−3.67, 75.28) | (−22.72, 13.73) | (−4.60, 33.35) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ji, S.; Zhou, Q.; Jiang, Y.; He, C.; Chen, Y.; Wu, C.; Liu, B. The Interactive Effects between Particulate Matter and Heat Waves on Circulatory Mortality in Fuzhou, China. Int. J. Environ. Res. Public Health 2020, 17, 5979. https://doi.org/10.3390/ijerph17165979
Ji S, Zhou Q, Jiang Y, He C, Chen Y, Wu C, Liu B. The Interactive Effects between Particulate Matter and Heat Waves on Circulatory Mortality in Fuzhou, China. International Journal of Environmental Research and Public Health. 2020; 17(16):5979. https://doi.org/10.3390/ijerph17165979
Chicago/Turabian StyleJi, Shumi, Quan Zhou, Yu Jiang, Chenzhou He, Yu Chen, Chuancheng Wu, and Baoying Liu. 2020. "The Interactive Effects between Particulate Matter and Heat Waves on Circulatory Mortality in Fuzhou, China" International Journal of Environmental Research and Public Health 17, no. 16: 5979. https://doi.org/10.3390/ijerph17165979
APA StyleJi, S., Zhou, Q., Jiang, Y., He, C., Chen, Y., Wu, C., & Liu, B. (2020). The Interactive Effects between Particulate Matter and Heat Waves on Circulatory Mortality in Fuzhou, China. International Journal of Environmental Research and Public Health, 17(16), 5979. https://doi.org/10.3390/ijerph17165979






